Abstract
Introduction:
The most common problem encountered in our day to day practice is exposed root surface or a tooth getting long. The main indication for root coverage procedures are esthetics and/or cosmetic demands followed by the management of root hypersensitivity, root caries or when it hampers proper plaque removal. Over the years, various techniques have been used to achieve root coverage.
Aim and Objectives:
The aim of this study was to compare the effectiveness of subpedicle acellular dermal matrix allograft (ADMA) with subepithelial connective tissue graft (SCTG) in the treatment of isolated marginal tissue recession.
Materials and Methods:
Twenty systemically healthy patients aged between 18 to 50 years (mean age29.7±4.35 years) with a recession defect on the labial and the buccal surfaces of any teeth were selected for the study. Ten patients received the test treatment (ADMA), ten patients received the control treatment (SCTG). Clinical recordings assessed at baseline, three months and six months post surgery, included Plaque index (PI), Papillary bleeding index (PBI), Gingival recession (REC), Probing pocket depth (PPD), Clinical attachment level (CAL) and Width of keratinized gingival (WKG).
Results:
Test group (ADMA) showed 86.93% mean root coverage while control group (SCTG) showed 84.72% at six months post surgery. Mean increase in the width of keratinized gingiva was significantly greater in the SCTG group (3.3±0.48mm) compared to ADMA group (2.4±0.51mm). Conclusion: Both the treatment produced a significant reduction in gingival recession and probing pocket depth and significant gain in clinical attachment level and width of keratinised gingiva.
Keywords: Acellular dermal matrix allograft, subepithelial connective tissue graft, gingival recession
INTRODUCTION
The most common problem encountered in our day to day practice is exposed root surface or a tooth getting long. The main indication for root coverage procedures are esthetics and/or cosmetic demands followed by the management of root hypersensitivity, root caries or when it hampers proper plaque removal. Over the years, various techniques have been used to achieve root coverage.
Langer and Langer[1] introduced subepithelial connective tissue graft in treating gingival recession, in which connective tissue graft combined with an overlaying pedicle graft were used. A coronally positioned pedicle graft has been shown to be effective with high percentage of root coverage, when combined with connective tissue graft. This technique offers a dual blood supply, improved esthetics and excellent predictability.
However, the disadvantages associated with subepithelial connective tissue graft procedure include the need for a second surgical site and morbidity linked with autogenous palatal donor mucosa.[2]
Recently, the use of an ADMG called as ALLODERM has become increasingly popular technique as a substitute for connective tissue graft.[3] Acellular dermal matrix is obtained from a human donor skin tissue, processed that removes its cell component while preserving the remaining bioactive components, which is subsequently freeze dried.[4] It is available in sheet form of various sizes such as 1×2 cm, 1×3 cm, 1×4 cm sizes. Multiple clinical studies have also documented predictable and esthetic results with an acellular dermal graft. This would simplify the surgery, eliminate the need for a second surgical site and permit treating an unlimited number of defects at one time.
MATERIALS AND METHODS
Study population
Twenty systemically healthy patients, aged between 18 to 50 years (mean age 29.7±4.35 years) with a recession defect on labial or buccal surface of any teeth were selected from the Outpatient Department of Periodontics.
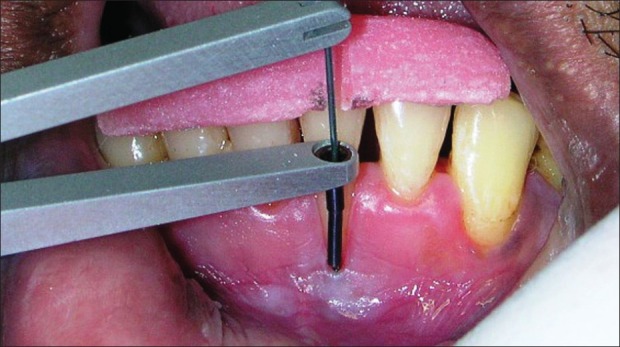
Patient selection criteria for this clinical study were: 1) presence of recession defect affecting labial/buccal surfaces of the teeth classified as either ‘Millers’ Class I or II, 2) Presence of ≥3 mm recession depth with the loss of clinical attachment level (CAL) ≥4 mm having equal amount of keratinized gingiva apical to the recession, 3) radiographic evidence of sufficient interdental bone (the distance between the crestal bone and cementoenamel junction as <2mm). Custom-made occlusal acrylic stents were used to standardize the probe angulation and position. Automated computerized 3rd generation Florida probe was used for measurement of clinical parameters [Figure 1].
Figure 1.
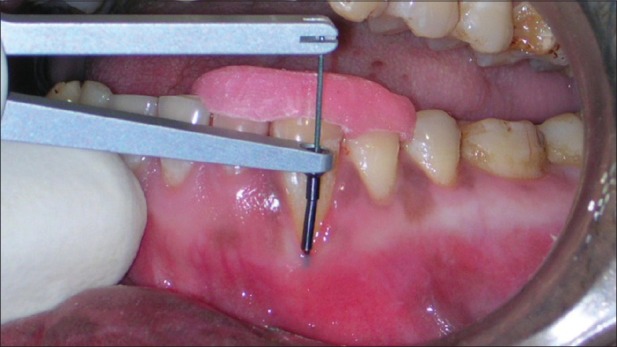
Preoperative assessment of recession with florida probe of test group
Surgical procedures
After induction of local Anesthesia (2% Lidocaine, epinephrine 1:100,000) the exposed root surfaces were carefully planned with curetts and ultrasonic instruments. The root surfaces were not subjected to any chemical conditioning.
Reciepient site preparation – Intra-Sulcular incision was made at the buccal aspect of the involved tooth. Two horizontal incisions were made at right angles to the adjacent interdental papillae, at the level of cemento-enamel junction without interfering with the gingival margin of the neighboring teeth. Two oblique vertical incisions were extended beyond the mucogingival junction and a trapezoidal mucoperiosteal flap was raised up to the mucogingival junction. After this point a split thickness flap was extended apically, releasing the tension and favoring the coronal positioning of the flap. The epithelium in the adjacent papillae was stripped away of its epithelium.
After the recipient site was completely prepared the selection of ADM (Alloderm) or CTG treatment was made by a coin toss. In cases of CTG donor palatal tissue was harvested by a ‘trap door approach’[5] from the area between the maxillary first molar and maxillary cuspid. An incision was made in the palate parallel to the maxillary premolar and first molar at a distance of approximately 3 mm apical to the gingival margin. Perpendicular incisions was then be made to establish width of the graft for covering the entire area of recession as well as the donor pedicle sites. A flap was reflected to expose the underlying connective tissue. The connective tissue graft was removed with a periosteal elevator. The graft was then placed on a sterile gauze pad and irrigated with saline. It can be modified as per the required dimensions after removal of excess fatty and glandular tissue. The primary flap was then returned to its original position and sutured with 4-0/5-0 Mersilk sutures to obtain primary closure, by using interrupted suturing technique or crossed horizontal suspension suturing technique [Figure 2].
Figure 2.

Suturing of the donor site in control group
Securing the connective tissue graft to the recipient site
Following the reflection of the flap at the recipient site, the connective tissue graft obtained from the donor site was placed in position on the recipient site at the level of cementoenamel junction and sutured with the interproximal papilla with 5-0 vicryl sutures.
The flap was then coronally postioned to completely cover the connective tissue graft and the deepithelialized portions of the papillae. The coronal margins of the flap was placed slightly coronal to the CEJ and stabilized with simple interrupted 5-0 vicryl.
In cases of ADM, it was hydrated in a sterile saline dish for 10 minutes according to the manufacturer's recommendation [Figure 3]. The graft was then trimmed to the shape and size designed to cover the exposed root surface, and extended about 3 mm on the bone surface. During the placement of the ADM one must be very careful that the connective tissue side (i.e., red side) should be placed on the exposed Root and Bone surface while the basement membrane side (i.e., white side) should be placed towards the pedicle soft tissue. The graft was secured to the wound bed with four interupted sutures using 5-0 vicryl material [Figure 4]. The flap was then coronally positioned to completely cover the ADM (ALLODERM) and the deepithelialized portions of papillae.
Figure 3.
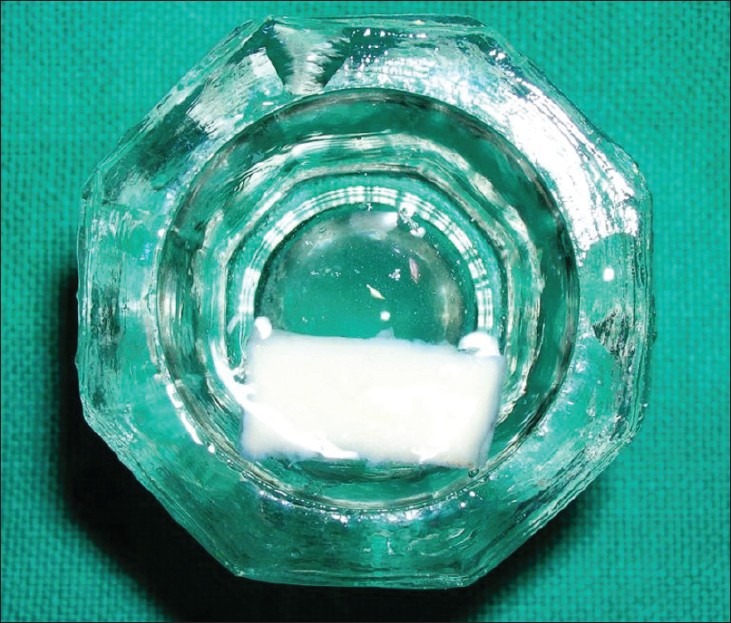
ADMA Hydration in normal saline
Figure 4.
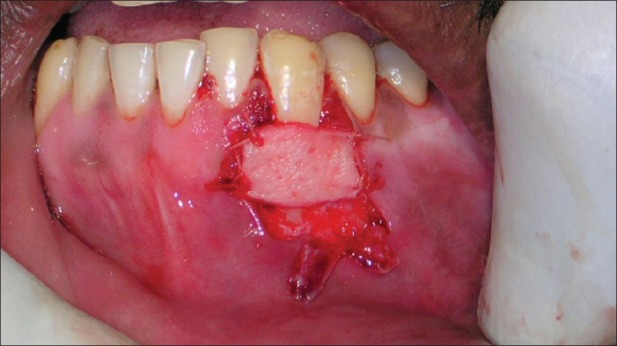
Suturing of ADMA at the recipient site
Post-operative care
Immediately after surgery periodontal dressing (COE-PAK™, GC America Inc., ALSIP, IL, U.S.A.) was placed. After surgery, a non-steroidal anti-inflammatory (Ibuprofen + Paracetamol, t.d.s for five days) and Systemic antibiotics (Amoxicillin 500 mg t.d.s.for seven days) were prescribed. All patients were placed on 0.2% chlorhexidine gluconate (Hexidine – ICPA) twice daily, for 4-6 weeks.
RESULTS
A total of twenty isolated gingival recession defects of Miller's class I in 20 systemically healthy patients (mean age 29.75±4.35) were selected for the study. The test group with 10 gingival recession defects were, treated with acellular dermal matrix allograft (ADMA) while the control group also with 10 gingival recession defects, were treated with connective tissue graft combined with coronally advanced flap.
Plaque index (PI), Papillary bleeding index (PBI), Gingival recession (REC), Probing pocket depth (PPD), Clinical attachment level (CAL), and Width of keratinized gingiva (WKG) were recorded at baseline, three months and six months post-surgery with the help of Florida probe [Figures 5–8].
Figure 5.
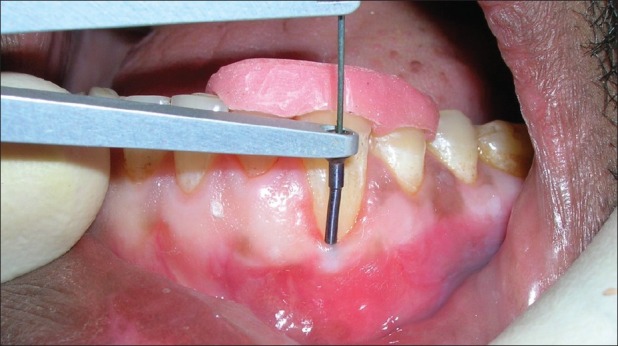
Post operative assessment of recession at 6 months with florida probe of test group
Figure 8.
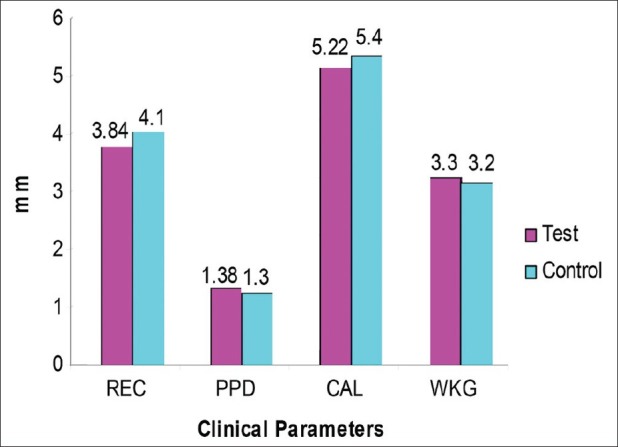
Baseline defect characteristics for the test and control groups
Figure 6.
Preoperative assessment of recession with florida probe of control group
Figure 7.
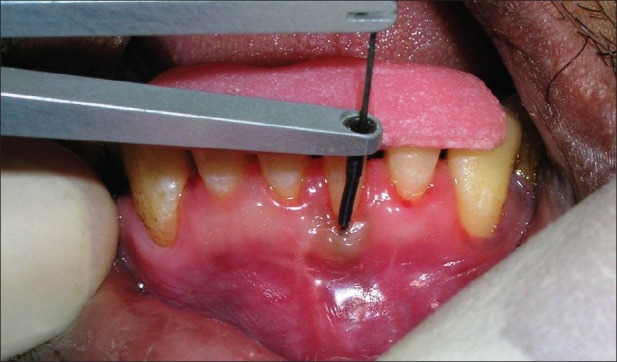
Post operative assessment of recession at 6 months with florida probe of control group (SCTG)
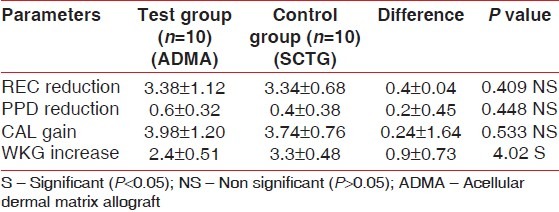
The mean PI and PBI scores decreased at three months and showed a statistically significant increase at six months after the surgery. The mean root coverage percent in ADMA group (86.93) was greater than the SCTG group (84.72). Probing pocket depth reduction in the ADMA group was 0.6±0.32 mm and 0.4±0.38 mm in SCTG group. Mean values of clinical attachment level gain was 3.98±1.20 mm in the ADMA group and 3.74±0.76 mm in the SCTG group. There was a statistically significant increase in the width of keratinized gingiva in the SCTG group (3.3±0.48 mm) compared to ADMA group (2.4±0.51 mm) [Table 1].
Table 1.
Comparison of clinical parameters between the test and control group at 6 months
DISCUSSION
The purpose of this present randomized controlled clinical trial was to compare the clinical outcomes of traditional SCTG versus ADMA in combination with coronally advanced flap for the treatment of isolated buccal/labial gingival recession. Six months results in the present study were obtained by comparing two well balanced experimental groups. There was no sign of allergy, infection or any other complication in any patients after the use of ADM graft, indicates that product ADM was well tolerated. A result obtained from this study indicates that both ADMA and SCTG can be successfully used to treat periodontal recession defects.
As outlined earlier, ADMA technique could offer several advantages over SCTG, including elimination of the need for a second surgical site(s) for harvesting graft and associated morbidity, less post surgery trauma and discomfort, reduction in operatory time, and an increase in acceptance of the procedure by patients. Our results suggest that this technique may eliminate the need for use of connective tissue in root coverage procedure.
In the present study, the SCTG group achieved 100% root coverage in 60% of cases were as only 40% of recession defect ADMA group were completely covered. Our findings might differ from Harris[6] and Aichelmann-Reidy[7] studies in which they reported similar complete root coverage between CT and ADM group treated gingival recession.
In the present study SCTG group showed significant greater increase in width of keratinize gingiva (3.3 mm), as compared to ADMA group (2.4 mm). A similar result was obtained by Harris[8] in a clinical trial comparing connective tissue and acellular dermal matrix grafts in association with a coronally positioned flap. In comparative study on the effectiveness of ADM to increase attach gingiva, Wei et al.,[9] reported that ADM free grafts produced a lesser extent attached gingiva in comparison to CT free grafts. They believed that the difference could be attributed due to considerable shrinkage of ADM during the healing phase.
ADM acts as a scaffold for cells from the surrounding tissues, and the original non vital graft is degraded and completely replaced by host cell. Considering that only the cells from the PDL and gingival connective tissue are capable of inducing the development of keratinized epithelium,[10] the inductive properties of ADM graft will depend on the percent of colonization of non vital graft by the host cells deriving from these tissues capable of inducing keratinization. Conversely, connective tissue grafts are entirely made up of tissue that is able to induce keratization of epithelium.
CONCLUSION
Both the treatment resulted in significant reduction in gingival recession and probing pocket depth; and significant gains in clinical attachment level and width of keratinized gingiva
ADMA group showed 86.93% mean root coverage while SCTG 84.72% at six months post surgery
Mean CAL gains and mean root coverage obtained in ADMA group was greater than SCTG group but the difference was not statistically significant
Mean increase in width of keratinized gingiva was significantly greater in SCTG group (3.3±0.48 mm) compared to ADMA group (2.4±0.51 -mm).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715–20. doi: 10.1902/jop.1985.56.12.715. [DOI] [PubMed] [Google Scholar]
- 2.Harris RJ. Root coverage with a connective tissue with partial thickness double pedicle graft and an acellular dermal matrix graft: A clinical and histological evaluation of a case report. J Periodontol. 1998;68:1305–11. doi: 10.1902/jop.1998.69.11.1305. [DOI] [PubMed] [Google Scholar]
- 3.Dodge JR, Henderson R, Greenwell H. Root coverage without a palatal donor site, using an acellular dermal graft. Periodontal Insights. 1998;5:5–9. [Google Scholar]
- 4.Batista EL, Jr, Batista FC, Novaes AB., Jr Management of soft tissue ridge deformities with acellular dermal matrix. Clinical approach and outcome after 6 months of treatment. J Periodontol. 2001;72:265–73. doi: 10.1902/jop.2001.72.2.265. [DOI] [PubMed] [Google Scholar]
- 5.Langer B, Calangna LJ. The subepithelial connective tissue graft. J Prosthet Dent. 1980;44:363–71. doi: 10.1016/0022-3913(80)90090-6. [DOI] [PubMed] [Google Scholar]
- 6.Harris RJ. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: Result of 107 recession defect in 50 consecutively treated patients. Int J Periodontics Restorative Dent. 2000;20:51–9. [PubMed] [Google Scholar]
- 7.Aichelmann-Reidy ME, Yukna RA, Evans GH, Nasr HF, Mayer ET. Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. J Periodontol. 2001;72:998–1005. doi: 10.1902/jop.2001.72.8.998. [DOI] [PubMed] [Google Scholar]
- 8.Harris RJ. A short term and long term comparison of root coverage with an acellular dermal matrix and a subepithelial graft. J Periodontol. 2004;75:734–43. doi: 10.1902/jop.2004.75.5.734. [DOI] [PubMed] [Google Scholar]
- 9.Wei PC, Laurell L, Geivelis M, Lingen MW, Maddalozzo D. Acellular dermal matrix allograft to achieve increased attach gingival. Part 1. A clinical study. J Periodontol. 2001;71:1297–305. doi: 10.1902/jop.2000.71.8.1297. [DOI] [PubMed] [Google Scholar]
- 10.Karring T, Lang NP, Loe H. The role of gingival connective tissue in determining epithelial differentiation. J Periodontol Res. 1974;10:1–11. doi: 10.1111/j.1600-0765.1975.tb00001.x. [DOI] [PubMed] [Google Scholar]


