Abstract
This study examined whether combining paclitaxel (taxol) with a novel epigenetic agent phenethyl isothiocyanate (PEITC) will yield a synergistic effect on inhibiting breast cancer cells. Two drug-resistant breast cancer cell lines, MCF7 and MDA-MB-231, were treated with PEITC and taxol. Cell growth, cell cycle, and apoptosis were examined. The combination of PEITC and taxol significantly decreased the IC50 of PEITC and taxol over each agent alone. The combination also increased apoptosis by more than two fold over each single agent in both cell lines. A significant increase of cells in the G2/M phases was detected. In conclusion, the combination of PEITC and taxol exhibits a synergistic effect on growth inhibition in breast cancer cells. This combination deserves further study in vivo.
Introduction
Two common epigenetic regulations are DNA methylation and histone acetylation, which modify DNA and histone interactions within chromatins and account for the increase or decrease in gene expression [1-3]. DNA hypermethylation has been shown to inhibit gene transcription, thus reducing gene expression [4-7]. Methylation and deacetylation have been found to play a key role in malignant disorders [8]. Inhibitors of these processes, such as methyltransferase inhibitors and histone deacetylase (HDAC) inhibitors, are novel anti-cancer agents. Two DNA methyltransferase inhibitors, azacitidine and decitabine, and a histone deacetylase inhibitor, vorinostat, have been licensed for clinical use [9-11]. Phenethyl isothiocyanate (PEITC) belongs to the family of natural isothiocyanates, which are found in a wide variety of cruciferous vegetables, and are released when the vegetables are cut or masticated. PEITC has been proven to be an effective HDAC inhibitor, and is able to induce growth arrest and apoptosis in cancer cells both in vitro and in vivo [12-15].
Breast cancer is the most commonly diagnosed cancer among women, accounting for more than 1 in 4 cancers [16]. After lung cancer, breast cancer is the leading cause of cancer death in women. Chemotherapy is a mainstay in breast cancer therapy. New agents are being actively sought [17-21]. Paclitaxel (taxol) is a widely used chemotherapy drug in the treatment of breast cancer [22], lung cancer [23], and ovarian cancer [24]. It was first discovered in 1967 [25], entered clinical trials in 1984 [26-28], and has been a leading chemotherapeutic agent ever since [23,26,27,29]. The mechanism of action of paclitaxel involves its interference with microtubule assembly [30]. Paclitaxel prevents the disassembly of microtubules during mitosis [31]. When taxol binds to tubulin, the microtubules become locked in polymerized state, and thus the cells are restricted from G2 to M phase transition [32-35]. The end result is that the cells are not able to replicate. Another effect of taxol is that it inhibits the anti-apoptosis protein Bcl-2, and induces apoptosis in cancer cells [36]. However, paclitaxel, like most other chemotherapy drugs, has a high level of toxicity as well as a multitude of side effects. The consequence of the toxicity of taxol at a higher dosage is neuropathy which limits its use in patients [23,26,27]. Furthermore, cancer cells develop resistance to taxol after prolonged use.
It has been shown in this laboratory that PEITC is a HDAC inhibitor and can suppress HDAC enzyme activity and decrease HDAC enzyme expression in prostate cancer, leukemia, and myeloma cells [12-14,37-40]. An interesting is that some isothionates have minimal toxicity to normal cells [40]. This project aimed to study the combined effect of PEITC and taxol on breast cancer.
Materials and methods
Chemicals and cell cultures
The PEITC (phenethyl isothiocyanate) was purchased from LKT Labs with 98% purity. The PEITC was in Paclitaxel (taxol) powder (Sigma Chemical Co.) was dissolved in DMSO to a stock concentration of 200 nM.
The MCF7 and MDA-MB-231 cell lines were obtained from American Type Cell Cultures. The cells were seeded at 0.4 × 106 per ml and 0.2 × 106 per ml, respectively, of PRMI-1640 medium supplemented with 10% heat-inactivated fetal bovine serum and maintained at 37 C in a humidified atmosphere containing 5% CO2. The cells in exponential growth were exposed to PEITC and taxol at various concentrations. The control cultures were supplemented with DMSO as the vehicle control. At the specified time points, the cells were harvested. Cell number and viability were determined from at least triplicate cultures by the trypan blue exclusion method.
Cell cycle analysis
The analysis of cell cycle phases was performed using a Becton-Dickinson FACScan flow cytometer according to the methods described previously [40]. The cells were stained with propidium iodide solution (50 μg/ml) on ice, and at least 10,000 cells were analyzed.
Apoptosis analysis
Apoptotic cells were determined by the terminal deoxynucleotidyl transferase-mediated biotinylated UTP nick-end labeling (TUNEL) assay. The TUNEL assay, according to the methods described previously [40], was performed in situ with a cell death detection kit (Roche Diagnostics). To enumerate the apoptotic cells, six different fields on each section were examined. At least 100 cells from each field were counted. The mean populations of apoptotic cells per section from the control group and experimental group were reported.
Statistical analysis
Results from 3 of more experiments were analyzed and expressed as the mean +/- SD. Results were evaluated by a two-sided paired Student’s t-test for statistical difference between treatments. P <0.05 was considered to be statistically significant. IC50, the concentration at which 50% of cell growth is inhibited, was calculated using the Calcusyn software (Biosoft, Inc). Synergism was assessed by the dose–effect curves of single versus combined drug treatment using the Calcusyn software [41].
Results
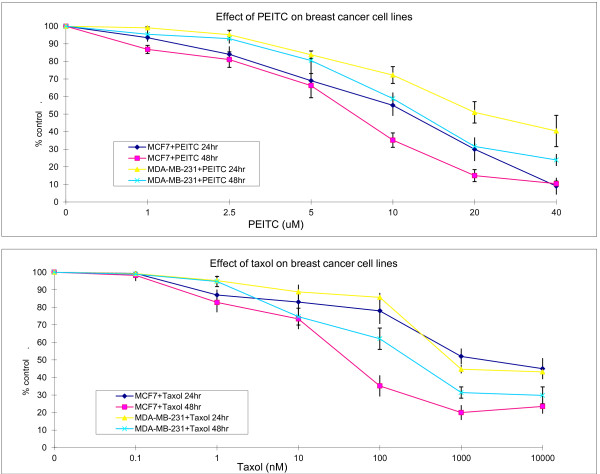
Effect of PEITC and taxol on breast cancer cells
To test the effect of PEITC and taxol on breast cancer cells, the agents were added to the MCF7 (MCF) and MDA-MB-231 (MB) cell cultures at serial dilutions for 24 and 48 hours, respectively. The PEITC concentration ranged from 1 to 40 μM (Figure 1), and taxol concentration ranged from 0.1 to 10,000 nM (Figure 1). PEITC suppressed cell growth in a time- and concentration-dependent manner. The IC50 (the concentration at which 50% of cell growth is inhibited) of PEITC for MCF cells at 48 hours is 5.6 μM, the IC50 of PEITC for MB cells at 48 hours is 15.6 μM. It appears that 5 μM and 10 μM are the concentrations that can cause growth suppression in a linear fashion for MCF and MB cells, respectively. These concentrations were therefore chosen for further combination studies. The IC50 of taxol for MCF and MB cells at 48 hours is 111 nM and 410 nM, respectively. The 10 nM and 100 nM concentrations of taxol were chosen for further combination studies for MCF and MB cells, respectively. It appears that MB cells are more resistant to PEITC (>2 x IC50) and taxol (4x IC50) than MCF cells, and higher concentrations of taxol did not further enhance the effect on growth inhibition.
Figure 1.
Single agent phenethyl isothiocyanate (PEITC) and paclitaxel (taxol)-induced growth inhibition of MCF7 and MDA-MB-231 breast cancer cells. The cells were treated with PEITC or taxol at various concentrations. The viable cells were enumerated at 24 and 48 hours, respectively. Vertical bars represent the means +/- SD of 3 or more independent experiments
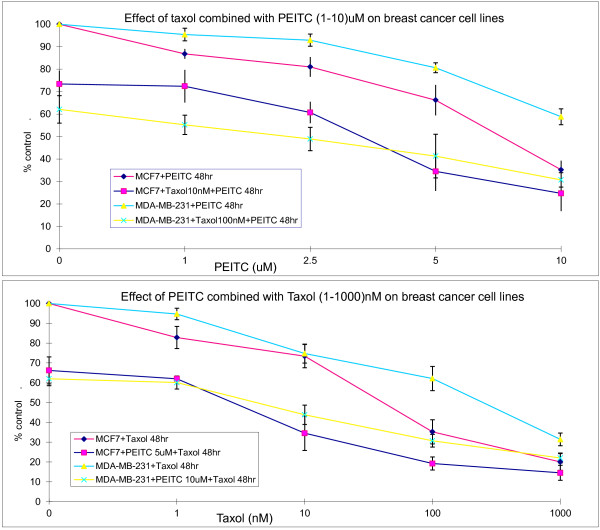
Effect of PEITC and taxol in combination on breast cancer cell growth
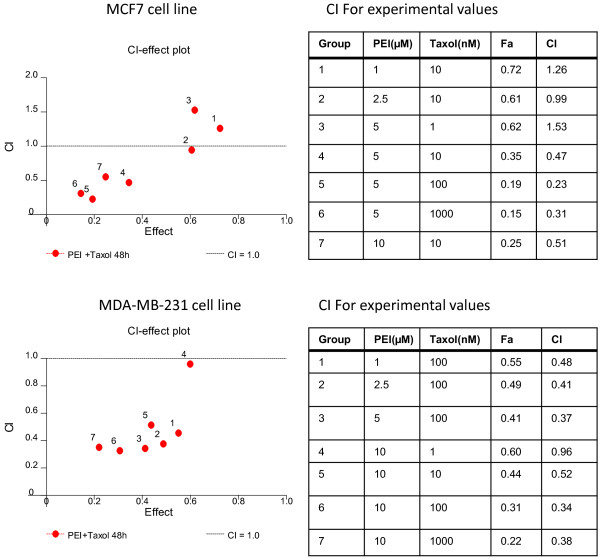
We further tested the effect of the combination of the two agents on breast cancer cell growth at 48 hours. To search for the optimal concentrations of the two agents, various concentrations were tested. When cells were treated with a fixed concentration of taxol, IC50 of PEITC for MCF and MB cells decreased by more than 2.6 folds and 7.3 folds, respectively (Figure 2). When the cells were treated with a fixed concentration of PEITC, the taxol IC50 for MCF and MB cells decreased by more than 37 folds and 50 folds, respectively (Figure 2). This effect was further analyzed for synergism using computer modeling. For both MCF and MB cells, there is a clear synergistic effect when PEITC and taxol are combined, although antagonistic effects were seen in certain combinations (Figure 3).
Figure 2.
Effect of combination of PEITC and taxol on growth inhibition of MCF7 and MDA-MB-231 breast cancer cells. The cells were treated with fixed concentration of PEITC and various concentrations of taxol or vice versa for 48 hours. The viable cells were enumerated at the end of the treatment. Vertical bars represent the means +/- SD of 3 or more independent experiments
Figure 3.
Combination dose-effect of PEITC and taxol on MCF7 and MDA-MB-231 breast cancer cells. Cells were cultured in the presence of PEITC and taxol at various concentrations as indicated in the tables for 48 hours. The number of cells were then enumerated. The dose-effect plot is done using Calcusyn software. CI: combination index. Fa: fraction affected; Index >1.0 indicates antagonism, index <1.0 indicates synergism
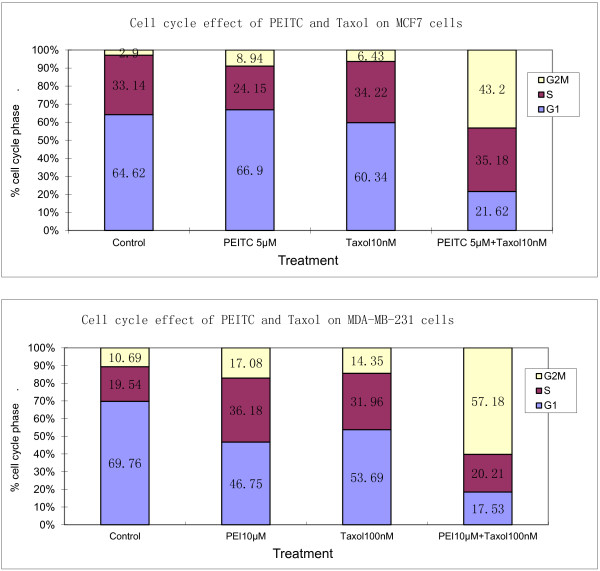
Effect of combination of PEITC and taxol on cell cycle in breast cancer cells
It is known that taxol can suppress cell growth through blocking cell cycle arrest at G2M phases. We therefore examined the effect of combining both agents on cell cycle progression. Taxol and PEITC as single agent at low concentrations caused an accumulation of cells in G2M (PEITC: 8.94% and 17.08%; taxol: 6.43% and 14.35%, for MCF and MB, respectively) (Figure 4). When PEITC and taxol were added concurrently in the cell culture for 48 hours , there was a significant increase (43.2% and 57.1% for MCF and MB, respectively) in the number of cells arrested in the G2M phases (P < 0.001) and a corresponding decrease of cells in the G1 phases (P < 0.001).
Figure 4.
PEI and taxol combination increases G2M cell cycle arrest in MCF7 and MDA-MB-231 breast cancer cells. The MCF7 cells were treated with 5 μM of PEITC and 10 nM of taxol alone or in combination. Due to higher resistance of MDA-MB-231 cells, PEITC at 10 μM and taxol at 100 nM were used. The DNA content was by flow cytometry to determine the distribution of cells in each phases
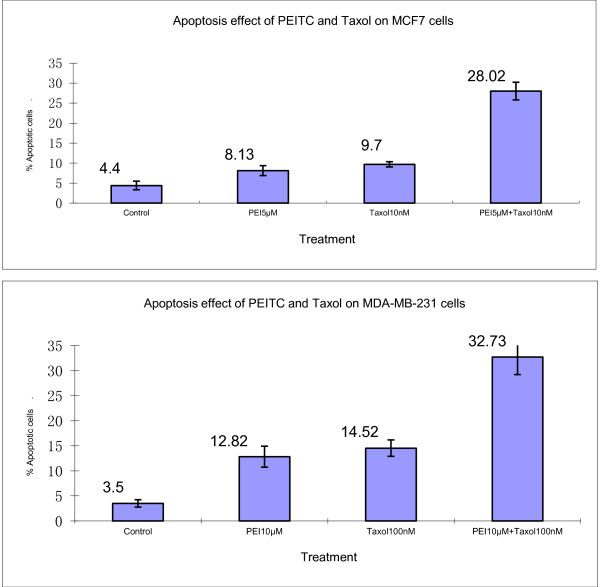
Effect of combination of PEITC and taxol on apoptosis of breast cancer cells
Using TUNEL assay, the effect of PEITC and taxol on cell apoptosis was examined. Compared with either agent alone, the combination of PEITC and taxol increased apoptosis by 3.4- and 2.8- folds, respectively, in MCF cells, and by more than two folds in MB cells (Figure 5).
Figure 5.
PEI and taxol combination increases apoptosis of MCF7 and MDA-MB-231 breast cancer cells. The MCF7 cells were treated with 5 μM of PEITC and 10 nM of taxol alone or in combination. Due to higher resistance of MDA-MB-231 cells, PEITC at 10 μM and taxol at 100 nM were used. Apoptosis was determined using TUNEL assay as described in Materials and Methods. Vertical bars represent the means +/- SD of 3 independent experiments
Discussion
Paclitaxel has been a major chemotherapeutic agent for breast cancer and a variety of solid tumors [22-24]. Its major clinical limitations are neurotoxicity and cellular resistance after prolonged treatment. PEITC is a novel epigenetic agent with a dual effect of histone deacetylation and DNA methylation [13,14]. This study found that the two agents have a profound synergistic inhibitory effect on the growth of two different breast cancer cell lines, MCF and MDA-MB-231. The IC50 of PEITC and taxol decrease dramatically when the two chemicals are used in combination. These results suggest that it is highly possible to significantly reduce side effects of taxol while maintaining or enhancing clinical efficacy by combining the two drugs.
We hypothesize that by combining PEITC and taxol, it is possible to significantly reduce toxicity in vivo by reducing the dosage of taxol needed while maintaining clinical efficacy for breast cancer and other solid tumors. This hypothesis appears to be supported by this in vitro study, and can be tested further in mouse model carrying breast cancer xenografts.
Novel agents targeting different molecular pathways are being actively studied for targeted cancer therapy [18,21,42-46]. A recent study has shown that the HDAC inhibitor vorinostat can up-regulate estrogen receptors and make breast cancer cells more sensitive to tamoxifen [47]. A preliminary report from a recent clinical study seems to corroborate this laboratory finding, where patients with hormone-refractory breast cancer showed responses to tamoxifen again after vorinostat treatment [48]. Since PEITC is a HDAC inhibitor as well as a tubulin-targeting agent, it would be worthwhile to test the combination of PEITC and tamoxifen for therapy of hormone-refractory breast cancer.
Similar to previous reports, we also observed that very high concentrations of taxol did not further increase growth inhibition and apoptosis. This may be due to the fact that higher concentrations of taxol have the opposite effect on cell growth as reported earlier [49]. The exact mechanism remains unclear.
In conclusion, this is the first study to show that the combination of the epigenetic agent PEITC with the chemotherapeutic agent taxol exhibits a synergistic effect on growth inhibition, cell cycle arrest, and apoptosis in breast cancer cells. This novel strategy deserves further study in vivo.
Competing interests
The authors have no relevant conflicts of interests.
Authors’ contributions
KL, SC and YM performed laboratory studies. All authors have contributed to data preparation, drafting and revising the manuscripts. All authors have read and approved the final manuscript.
Contributor Information
Katherine Liu, Email: kathylab2010@gmail.com.
Shundong Cang, Email: cangshundong@163.com.
Yuehua Ma, Email: HAL19831116@yahoo.com.cn.
Jen Wei Chiao, Email: jen-wei_chiao@nymc.edu.
References
- Wolffe AP, Matzke MA. Epigenetics: regulation through repression. Science. 1999;286(5439):481–486. doi: 10.1126/science.286.5439.481. [DOI] [PubMed] [Google Scholar]
- Ura K, Kurumizaka H, Dimitrov S, Almouzni G, Wolffe AP. Histone acetylation: influence on transcription, nucleosome mobility and positioning, and linker histone-dependent transcriptional repression. EMBO J. 1997;16(8):2096–2107. doi: 10.1093/emboj/16.8.2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Workman JL, Kingston RE. Alteration of nucleosome structure as a mechanism of transcriptional regulation. Annu Rev Biochem. 1998;67:545–579. doi: 10.1146/annurev.biochem.67.1.545. [DOI] [PubMed] [Google Scholar]
- Bird AP, Wolffe AP. Methylation-induced repression–belts, braces, and chromatin. Cell. 1999;99(5):451–454. doi: 10.1016/S0092-8674(00)81532-9. [DOI] [PubMed] [Google Scholar]
- Hendrich B, Bird A. Mammalian methyltransferases and methyl-CpG-binding domains: proteins involved in DNA methylation. Curr Top Microbiol Immunol. 2000;249:55–74. doi: 10.1007/978-3-642-59696-4_4. [DOI] [PubMed] [Google Scholar]
- Tyler JK, Kadonaga JT. The “dark side” of chromatin remodeling: repressive effects on transcription. Cell. 1999;99(5):443–446. doi: 10.1016/S0092-8674(00)81530-5. [DOI] [PubMed] [Google Scholar]
- Tse C, Sera T, Wolffe AP, Hansen JC. Disruption of higher-order folding by core histone acetylation dramatically enhances transcription of nucleosomal arrays by RNA polymerase III. Mol Cell Biol. 1998;18(8):4629–4638. doi: 10.1128/mcb.18.8.4629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade PA. Transcriptional control at regulatory checkpoints by histone deacetylases: molecular connections between cancer and chromatin. Hum Mol Genet. 2001;10(7):693–698. doi: 10.1093/hmg/10.7.693. [DOI] [PubMed] [Google Scholar]
- Momparler RL. Epigenetic therapy of cancer with 5-aza-2’-deoxycytidine (decitabine) Semin Oncol. 2005;32(5):443–451. doi: 10.1053/j.seminoncol.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Kaminskas E, Farrell A, Abraham S, Baird A, Hsieh LS, Lee SL, Leighton JK, Patel H, Rahman A, Sridhara R. Approval summary: azacitidine for treatment of myelodysplastic syndrome subtypes. Clin Cancer Res. 2005;11(10):3604–3608. doi: 10.1158/1078-0432.CCR-04-2135. [DOI] [PubMed] [Google Scholar]
- Kelly WK, Richon VM, O’Connor O, Curley T, Gregor-Curtelli B, Tong W, Klang M, Schwartz L, Richardson S, Rosa E. Phase I clinical trial of histone deacetylase inhibitor: suberoylanilide hydroxamic acid administered intravenously. Clin Cancer Res. 2003;9(10 Pt 1):3578–3588. [PubMed] [Google Scholar]
- Beklemisheva AA, Fang Y, Feng J, Ma X, Dai W, Chiao JW. Epigenetic mechanism of growth inhibition induced by phenylhexyl isothiocyanate in prostate cancer cells. Anticancer Res. 2006;26(2A):1225–1230. [PubMed] [Google Scholar]
- Wang LG, Liu XM, Fang Y, Dai W, Chiao FB, Puccio GM, Feng J, Liu D, Chiao JW. De-repression of the p21 promoter in prostate cancer cells by an isothiocyanate via inhibition of HDACs and c-Myc. Int J Oncol. 2008;33(2):375–380. [PubMed] [Google Scholar]
- Wang LG, Beklemisheva A, Liu XM, Ferrari AC, Feng J, Chiao JW. Dual action on promoter demethylation and chromatin by an isothiocyanate restored GSTP1 silenced in prostate cancer. Mol Carcinog. 2007;46(1):24–31. doi: 10.1002/mc.20258. [DOI] [PubMed] [Google Scholar]
- Zou Y, Ma X, Huang Y, Hong L, Chiao J-w. Effect of phenylhexyl isothiocyanate on aberrant histone H3 methylation in primary human acute leukemia. J Hematol Oncol. 2012;5(1):36. doi: 10.1186/1756-8722-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feuer EJ, Wun LM, Boring CC, Flanders WD, Timmel MJ, Tong T. The lifetime risk of developing breast cancer. J Natl Cancer Inst. 1993;85(11):892–897. doi: 10.1093/jnci/85.11.892. [DOI] [PubMed] [Google Scholar]
- Xu B, Wu Y, Shen L, Ye D, Jappe A, Cherfi A, Wang H, Yuan R. Two-dose-level confirmatory study of the pharmacokinetics and tolerability of everolimus in Chinese patients with advanced solid tumors. J Hematol Oncol. 2011;4(1):3. doi: 10.1186/1756-8722-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan Y, Liao Y-M, Hsueh C-T, Mirshahidi H. Novel targeted therapeutics: inhibitors of MDM2, ALK and PARP. J Hematol Oncol. 2011;4(1):16. doi: 10.1186/1756-8722-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafiyath S, Rasul M, Lee B, Wei G, Lamba G, Liu D. Comparison of safety and toxicity of liposomal doxorubicin vs. conventional anthracyclines: a meta-analysis. Exp Hematol Oncol. 2012;1(1):10. doi: 10.1186/2162-3619-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbaz H, Stueckle T, Tse W, Rojanasakul Y, Dinu C. Digitoxin and its analogs as novel cancer therapeutics. Exp Hematol Oncol. 2012;1(1):4. doi: 10.1186/2162-3619-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WeiSZ L, Efferth T. Polo-like kinase 1 as target for cancer therapy. Exp Hematol Oncol. 2012;1(1):38. doi: 10.1186/2162-3619-1-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes FA, Walters RS, Theriault RL, Forman AD, Newton LK, Raber MN, Buzdar AU, Frye DK, Hortobagyi GN. Phase II trial of taxol, an active drug in the treatment of metastatic breast cancer. J Natl Cancer Inst. 1991;83(24):1797–1805. doi: 10.1093/jnci/83.24.1797-a. [DOI] [PubMed] [Google Scholar]
- Brown T, Havlin K, Weiss G, Cagnola J, Koeller J, Kuhn J, Rizzo J, Craig J, Phillips J, Von HD. A phase I trial of taxol given by a 6-hour intravenous infusion. J Clin Oncol. 1991;9(7):1261–1267. doi: 10.1200/JCO.1991.9.7.1261. [DOI] [PubMed] [Google Scholar]
- McGuire WP, Rowinsky EK, Rosenshein NB, Grumbine FC, Ettinger DS, Armstrong DK, Donehower RC. Taxol: a unique antineoplastic agent with significant activity in advanced ovarian epithelial neoplasms. Ann Intern Med. 1989;111(4):273–279. doi: 10.7326/0003-4819-111-4-273. [DOI] [PubMed] [Google Scholar]
- Wani MC, Taylor HL, Wall ME, Coggon P, McPhail AT. Plant antitumor agents. VI. The isolation and structure of taxol, a novel antileukemic and antitumor agent from Taxus brevifolia. JAm Chem Soc. 1971;93(9):2325–2327. doi: 10.1021/ja00738a045. [DOI] [PubMed] [Google Scholar]
- Wiernik PH, Schwartz EL, Strauman JJ, Dutcher JP, Lipton RB, Paietta E. Phase I clinical and pharmacokinetic study of taxol. Cancer Res. 1987;47(9):2486–2493. [PubMed] [Google Scholar]
- Wiernik PH, Schwartz EL, Einzig A, Strauman JJ, Lipton RB, Dutcher JP. Phase I trial of taxol given as a 24-hour infusion every 21 days: responses observed in metastatic melanoma. J Clin Oncol. 1987;5(8):1232–1239. doi: 10.1200/JCO.1987.5.8.1232. [DOI] [PubMed] [Google Scholar]
- Grem JL, Tutsch KD, Simon KJ, Alberti DB, Willson JK, Tormey DC, Swaminathan S, Trump DL. Phase I study of taxol administered as a short i.v. infusion daily for 5 days. Cancer Treat Rep. 1987;71(12):1179–1184. [PubMed] [Google Scholar]
- Donehower RC, Rowinsky EK, Grochow LB, Longnecker SM, Ettinger DS. Phase I trial of taxol in patients with advanced cancer. Cancer Treat Rep. 1987;71(12):1171–1177. [PubMed] [Google Scholar]
- Jordan MA, Kamath K. How do microtubule-targeted drugs work? An overview. Curr Cancer Drug Targets. 2007;7(8):730–742. doi: 10.2174/156800907783220417. [DOI] [PubMed] [Google Scholar]
- Kumar N. Taxol-induced polymerization of purified tubulin. Mechanism of action. J Biol Chem. 1981;256(20):10435–10441. [PubMed] [Google Scholar]
- Fuchs DA, Johnson RK. Cytologic evidence that taxol, an antineoplastic agent from Taxus brevifolia, acts as a mitotic spindle poison. Cancer Treat Rep. 1978;62(8):1219–1222. [PubMed] [Google Scholar]
- Schiff PB, Horwitz SB. Taxol stabilizes microtubules in mouse fibroblast cells. Proc Natl Acad Sci U S A. 1980;77(3):1561–1565. doi: 10.1073/pnas.77.3.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiff PB, Horwitz SB. Taxol assembles tubulin in the absence of exogenous guanosine 5’-triphosphate or microtubule-associated proteins. Biochemistry. 1981;20(11):3247–3252. doi: 10.1021/bi00514a041. [DOI] [PubMed] [Google Scholar]
- Schiff PB, Fant J, Horwitz SB. Promotion of microtubule assembly in vitro by taxol. Nature. 1979;277(5698):665–667. doi: 10.1038/277665a0. [DOI] [PubMed] [Google Scholar]
- Haldar S, Jena N, Croce CM. Inactivation of Bcl-2 by phosphorylation. Proc Natl Acad Sci U S A. 1995;92(10):4507–4511. doi: 10.1073/pnas.92.10.4507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cang S, Feng J, Konno S, Han L, Liu K, Sharma SC, Choudhury M, Chiao JW. Deficient histone acetylation and excessive deacetylase activity as epigenomic marks of prostate cancer cells. Int J Oncol. 2009;35:1417–1422. doi: 10.3892/ijo_00000459. [DOI] [PubMed] [Google Scholar]
- Lu L, Liu D, Ma X, Beklemishev A, Seiter K, Ahmed T, Chiao JW. The phenylhexyl isothiocyanate induces apoptosis and inhibits leukemia cell growth in vivo. Oncol Rep. 2006;16(6):1363–1367. [PubMed] [Google Scholar]
- Lu Q, Lin X, Feng J, Zhao X, Gallagher R, Lee MY, Chiao JW, Liu D. Phenylhexyl isothiocyanate has dual function as histone deacetylase inhibitor and hypomethylating agent and can inhibit myeloma cell growth by targeting critical pathways. J Hematol Oncol. 2008;1:6. doi: 10.1186/1756-8722-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma X, Fang Y, Beklemisheva A, Dai W, Feng J, Ahmed T, Liu D, Chiao JW. Phenylhexyl isothiocyanate inhibits histone deacetylases and remodels chromatins to induce growth arrest in human leukemia cells. Int J Oncol. 2006;28(5):1287–1293. [PubMed] [Google Scholar]
- Chou TC, Talalay P. Generalized equations for the analysis of inhibitions of Michaelis-Menten and higher-order kinetic systems with two or more mutually exclusive and nonexclusive inhibitors. Eur J Biochem. 1981;115(1):207–216. doi: 10.1111/j.1432-1033.1981.tb06218.x. [DOI] [PubMed] [Google Scholar]
- Trachootham D, Zhou Y, Zhang H, Demizu Y, Chen Z, Pelicano H, Chiao PJ, Achanta G, Arlinghaus RB, Liu J. Selective killing of oncogenically transformed cells through a ROS-mediated mechanism by beta-phenylethyl isothiocyanate. Cancer Cell. 2006;10(3):241–252. doi: 10.1016/j.ccr.2006.08.009. [DOI] [PubMed] [Google Scholar]
- Lamba G, Gupta R, Lee B, Ambrale S, Liu D. Current management and prognostic features for gastrointestinal stromal tumor (GIST) Exp Hematol Oncol. 2012;1(1):14. doi: 10.1186/2162-3619-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firer M, Gellerman G. Targeted drug delivery for cancer therapy: the other side of antibodies. J Hematol Oncol. 2012;5(1):70. doi: 10.1186/1756-8722-5-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Chen Y, Xu X, Fu X, Zhao Z. SU11652 Inhibits tyrosine kinase activity of FLT3 and growth of MV-4-11 cells. J Hematol Oncol. 2012;5(1):72. doi: 10.1186/1756-8722-5-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K, Wei G, Liu D. CD19: a biomarker for B cell development, lymphoma diagnosis and therapy. Exp Hematol Oncol. 2012;1(1):36. doi: 10.1186/2162-3619-1-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badia E, Oliva J, Balaguer P, Cavailles V. Tamoxifen resistance and epigenetic modifications in breast cancer cell lines. Curr Med Chem. 2007;14(28):3035–3045. doi: 10.2174/092986707782794023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster PN, Lacevic M, Schmitt M, Bicaku E, Marchion D, Stephens A, Sullivan L, Minton S. Phase II trial of vorinostat, a histone deacetylase inhibitor to restore the hormone sensitivity to the anti-estrogen tamoxifen in patients with advanced breast cancer having failed prior aromatase inhibitor therapy. J Clin Oncol. 2008;26:abs#3501. [Google Scholar]
- Liebmann JE, Cook JA, Lipschultz C, Teague D, Fisher J, Mitchell JB. Cytotoxic studies of paclitaxel (Taxol) in human tumour cell lines. Br J Cancer. 1993;68(6):1104–1109. doi: 10.1038/bjc.1993.488. [DOI] [PMC free article] [PubMed] [Google Scholar]