Abstract
Background
The aim of this study was to revise the 2003 Fenton Preterm Growth Chart, specifically to: a) harmonize the preterm growth chart with the new World Health Organization (WHO) Growth Standard, b) smooth the data between the preterm and WHO estimates, informed by the Preterm Multicentre Growth (PreM Growth) study while maintaining data integrity from 22 to 36 and at 50 weeks, and to c) re-scale the chart x-axis to actual age (rather than completed weeks) to support growth monitoring.
Methods
Systematic review, meta-analysis, and growth chart development. We systematically searched published and unpublished literature to find population-based preterm size at birth measurement (weight, length, and/or head circumference) references, from developed countries with: Corrected gestational ages through infant assessment and/or statistical correction; Data percentiles as low as 24 weeks gestational age or lower; Sample with greater than 500 infants less than 30 weeks. Growth curves for males and females were produced using cubic splines to 50 weeks post menstrual age. LMS parameters (skew, median, and standard deviation) were calculated.
Results
Six large population-based surveys of size at preterm birth representing 3,986,456 births (34,639 births < 30 weeks) from countries Germany, United States, Italy, Australia, Scotland, and Canada were combined in meta-analyses. Smooth growth chart curves were developed, while ensuring close agreement with the data between 24 and 36 weeks and at 50 weeks.
Conclusions
The revised sex-specific actual-age growth charts are based on the recommended growth goal for preterm infants, the fetus, followed by the term infant. These preterm growth charts, with the disjunction between these datasets smoothing informed by the international PreM Growth study, may support an improved transition of preterm infant growth monitoring to the WHO growth charts.
Keywords: Infant, Premature; Infant, very low birth weight; Preterm infant; Growth; Weight; Head circumference; Length; Percentile
Background
The expected growth of the fetus describes the fastest human growth, increasing weight over six-fold between 22 and 40 weeks. Preterm infants, who are born during this rapid growth phase, rely on health professionals to assess their growth and provide appropriate nutrition and medical care.
In 2006, the World Health Organization (WHO) published their multicentre growth reference study, which is considered superior [1] to previous growth surveys since the measured infants were selected from communities in which economics were not likely to limit growth, among culturally diverse non-smoking mothers who planned to breastfeed [2]. Weekly longitudinal measures of the infants were made by trained data collection teams during the first 2 years of this study [3]. These WHO growth charts, although recommended for preterm infants after term age [4], begin at term and so do not inform preterm infant growth assessments younger than this age.
Optimum growth of preterm infants is considered to be equivalent to intrauterine rates [5-7] since a superior growth standard has not been defined. Perhaps the best estimate of fetal growth may be obtained from large population-based studies, conducted in developed countries [8], where constraints on fetal growth may be less frequent.
A recent multicentre study by our group (the Preterm Multicentre Growth (PreM Growth) Study) revealed that although the pattern of preterm infant growth was generally consistent with intrauterine growth, the biggest deviation in weight gain velocity between the preterm infants and the fetus and infant was just before term, between 37 and 40 weeks (Fenton TR, Nasser R, Eliasziw M, Kim JH, Bilan D, Sauve R: Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant, The Preterm Infant Multicentre Growth Study. Submitted BMC Ped 2012). Rather than demonstrating the slowing growth velocity of the term infant during the weeks just before term, the preterm infants had superior, close to linear, growth at this age. This finding has been observed by others as well [9-11]. Therefore, there is evidence to support a smooth transition on growth charts between late fetal and early infant ages.
Several previous growth charts based on size at birth presented their data as completed age, which affects the interpretation and use of a growth chart [12]. The use of completed weeks when plotting a growth chart requires all the measurements to be plotted on the whole week vertical axes. However, the use of completed weeks in a neonatal unit may not be intuitive, as nursery staff and parents think of infants as their exact age, and not age truncated to previous whole weeks. The advent of computers in health care, for clinical care and health recording, allow the use of the computer to plot growth charts, daily and with accuracy. It would make sense to support plotting daily measurements continuously by shifting the data collected as completed weeks to the midpoint of the next week to remove the truncation of the data collection as completed weeks.
The objectives of this study were to revise the 2003 Fenton Preterm Growth Chart, specifically to: a) use more recent data on size at birth based on an inclusion criteria, b) harmonize the preterm growth chart with the new WHO Growth Standard, c) to smooth the data between the preterm and WHO estimates while maintaining integrity with the data from 22 to 36 and at 50 weeks, d) to derive sex specific growth curves, and to e) re-scale the chart x-axis to actual age rather than completed weeks, to support growth monitoring.
Methods
To revise the growth chart, thorough literature searches were performed to find published and unpublished population-based preterm size at birth (weight, length, and/or head circumference) references. The inclusion criteria, defined a priori, designed to minimize bias by restriction [13], were to locate population-based studies of preterm fetal growth, from developed countries with:
a) Corrected gestational ages through fetal ultrasound and/or infant assessment and/or statistical correction;
b) Data percentiles at 24 weeks gestational age or lower;
c) Sample of at least 25,000 babies, with more than 500 infants aged less than 30 weeks;
d) Separate data on females and males;
e) Data available numerically in published form or from authors,
f) Data collected within the past 25 years (1987 to 2012) to account for any secular trends.
A. Data selection and combination
Major bibliographic databases were searched: MEDLINE (using PubMed) and CINHAL, by both authors back to year 1987 (given our 25 year limit), with no language restrictions, and foreign articles were translated. The following search terms as medical subject headings and textwords were used: (“Preterm infant” OR “Premature Birth”[Mesh]) OR (“Infant, Premature/classification”[Mesh] OR “Infant, Premature/growth and development”[Mesh] OR “Infant, Premature/statistics and numerical data”[Mesh] OR “Infant, very low birth weight”[Mesh]) AND (percentile OR *centile* OR weeks) AND (weight OR head circumference OR length). Grey literature sites including clinical trial websites and Google were searched in February 2012. Reference lists were reviewed for relevant studies.
All of the found data was reported as completed weeks except for the German Perinatal Statistics, which were reported as actual daily weights [14]. To combine the datasets, the German data was temporarily converted to completed weeks. A final step converted the meta-analyses to actual age.
B. Combine the data to produce weighted intrauterine growth curves for each sex
The located data (3rd, 10th, 50th, 90th, and 97th percentiles for weight, head circumference, and length) that met the inclusion criteria were extracted by copying and pasting into spreadsheets. The male and female percentile curves from each included data set for weight, head circumference and length were plotted together so they could be examined visually for heterogeneity (Figures 1, 2, and 3). The data for each gender were combined by using the weekly data for the percentiles: 3rd, 10th, 50th, 90th, and 97th, weighted by the sample sizes. The combined data was represented by relatively smooth curves.
Figure 1.
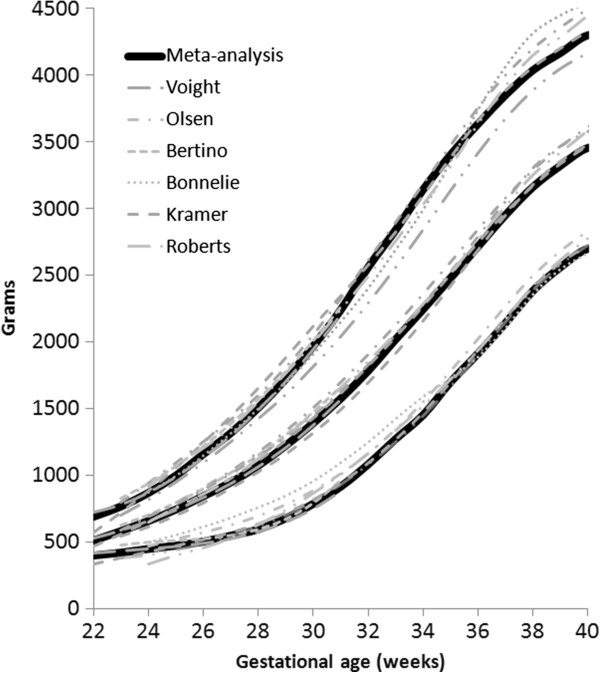
Boys birthweight centiles (3rd, 50th and 97th) from the six included studies, along with the boy’s meta-analysis curves (bold).
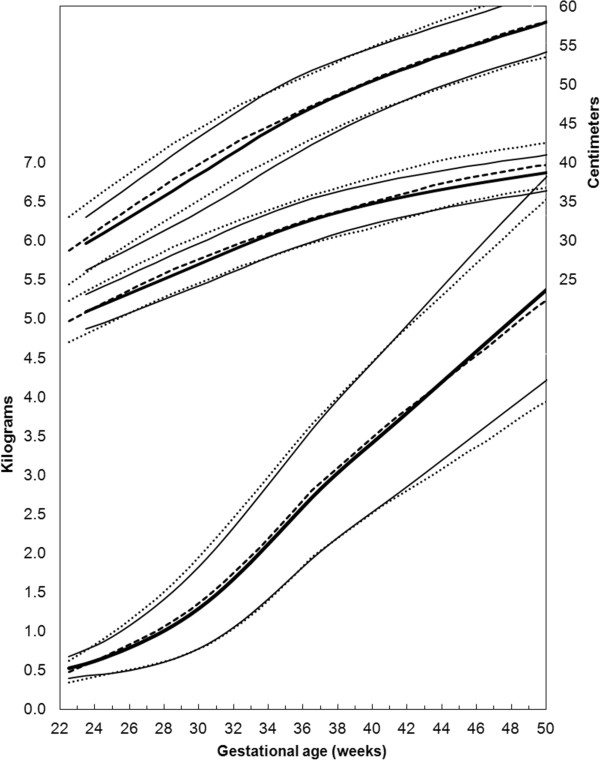
Figure 2.

Girls head circumference centiles (3rd, 50th and 97th) centiles from the included studies, along with the girl’s meta-analysis curves (dotted), and after 40 weeks, the World Health Organization centiles (dashed).
Figure 3.
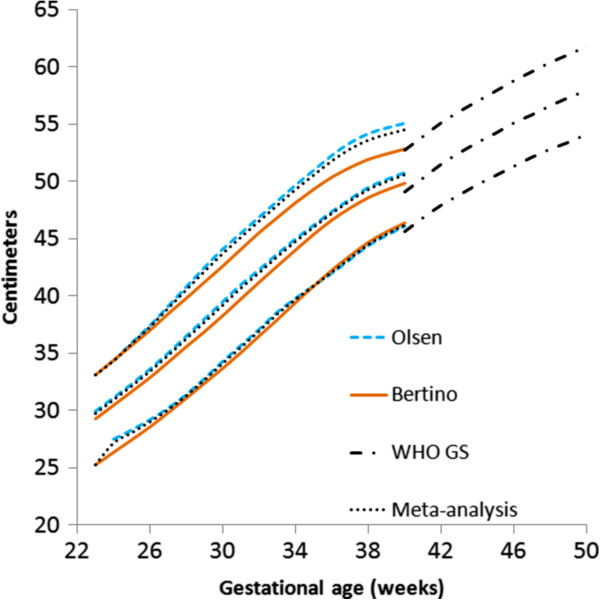
Girls length centiles (3rd, 50th and 97th) centiles from the included studies, along with the meta-analysis curves (dotted), and after 40 weeks, the World Health Organization centiles (dashed).
C. Develop growth monitoring curves
To develop the growth monitoring curves that joined the intrauterine meta-analysis data with the WHO Growth Standard (WHOGS) smoothly, the following cubic spline procedure was used to meet two objectives:
a) To maintain integrity with the meta-analysis curves from 22 to 36 weeks. Integrity of the fit was assumed to be agreement within 3% at each week.
b) To ensure fit of the data to the WHO values at 50 weeks, within 0.5%.
Procedure:
1) Cubic splines were used to interpolate smooth values between selected points (22, 25, 28, 32, 34, 36 and 50 weeks). Extra points were manually selected at 40, 43 and 46 weeks in order to produce acceptable fit through the underlying data. The PreM Growth study (Fenton TR, Nasser R, Eliasziw M, Kim JH, Bilan D, Sauve R: Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant, The Preterm Infant Multicentre Growth Study. Submitted BMC Ped 2012) conducted to inform the transition between the preterm and WHO data, was used to inform this step. The Prem Growth Study found that preterm infants growth in weight followed approximately a straight line between 37 and 45 weeks, as others have also noted [9-11].
2) LMS values (measures of skew, the median, and the standard deviation) [15] were computed from the interpolated cubic splines at weekly intervals. Cole’s procedures [15] and an iterative least squares method were used to derive the LMS parameters (L = Box-Cox power, M = median, S = coefficient of variation) from the multicentre meta-analyses for weight, head circumference and length. The LMS splines were smoothed slightly while maintaining data integrity as noted above.
3) The final percentile curves were produced from the smoothed LMS values.
4) A grid similar to the 2003 growth chart was used, but the growth curves were re-scaled along the x-axis from completed weeks to allow clinicians to plot infant growth by actual age in weeks, and a slight modification (scaled to 60 centimeters instead of 65) was made to the y-axis.
D. Compared the revised charts with the 2003 version
The revised growth charts were compared graphically with the original 2003 Fenton preterm growth chart. To make the differences in chart values more apparent, the 2003 chart data was also shifted to actual weeks for these comparison figures.
Results
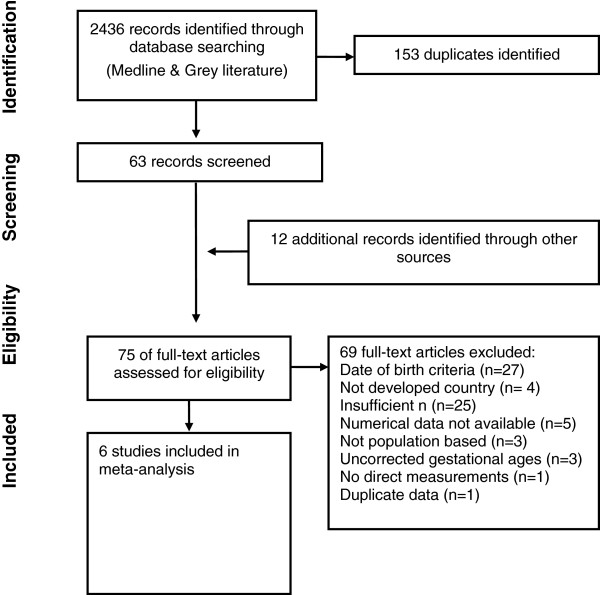
Six large population based surveys [14,16-20] of size at preterm birth from countries Germany, United States, Italy, Australia, Scotland, and Canada were located that met the inclusion criteria (Table 1). The literature search identified 2436 papers, of which 2373 were discarded as being not relevant or duplicates based on the titles (Figure 4). Reviewing reference lists identified another 12 studies. Seventy-five studies were examined in detail, however 27 of these did not meet the date criteria. Among the 48 studies that met the date of birth criteria, some did not meet the other inclusion criteria for the following reasons: Did not meet the criterion for more than 25,000 babies [21-35], no low gestational age infants less than 25 weeks [31,36-41], insufficient number less than 30 weeks [34,42-45], no statistical correction for inaccurate gestational ages [46-48], numerical data not available [49-51], number of infants each week were not available [52], number of infants in the subgroups each week were not available [53], was not population based [54-56], no direct measurements [27], some of the data [57] was also in one of the larger included studies [17].
Table 1.
Details of the data sources
| Voight, 2010 | Olsen, 2010 | Kramer, 2001 | Roberts, 1999 | Bonellie, 2008 | Bertino, 2010 | WHO, 2006 | |
|---|---|---|---|---|---|---|---|
| Data source |
German Perinatal Survey |
Pediatrix Medical Group hospitals |
Canadian national file |
Australian National Perinatal Statistics Unit |
Scottish maternity data collection |
Italian Neonatal Study |
WHO multicentre growth reference study |
| Sample size |
2,300,000 |
130,111 |
676,605 |
734,145 |
100,133 |
45,462 |
882 |
| n < 30 weeks |
14146 |
11377 |
3247 |
3193 |
2053 |
623 |
N/A |
| Lowest gestational age |
22 |
23 |
22 |
20 |
24 |
23 |
term |
| Dates |
1995 to 2000 |
1998 to 2006 |
1994 to 1996 |
1991 to 1994 |
1998 to 2003 |
2005 to 2007 |
1997-2003 |
| Data |
Weight |
Weight, head, length |
Weight |
Weight |
Weight |
Weight, head, length |
Weight, head, length |
| Exclusion criteria |
None stated, included both live and stillborn |
Multiple births, congenital anomalies, death before discharge, outlier measures (> 2 x interquartile range below the first and 3rd quartile). |
Ontario province was excluded due to problems with data quality. |
Omitted multiple and still births (births < 400 grams did not need to be recorded) |
Multiple births, lethal anomalies, weights < 250 grams, and outlier measures (> 2 x interquartile range outside the first and 3rd quartile). |
Multiple births, stillbirths, major congenital anomalies, and fetal hydrops |
Maternal smoking, not breastfeeding, solids before 4 months. Screened for environmental or economic constraints. |
| Method to assess gestational age |
Ultrasound assessment 8–14 weeks and Naegle’s rule. |
Neonatologist assessment |
“early ultrasound has increasingly been the basis for gestational age assessments in recent years” |
Dates, prenatal, or postnatal assessment |
Clinician assessment based on ultrasound, maternal dates, and clinical estimates |
Ultrasound assessment first trimester |
Not stated |
| Outliers/smoothing method | Cubic regression, LOESS smoothing, LMS parameter smoothing | LMS methods, with the skew set to one and further manual smoothing | Assumed a log normal distribution of birthweight at each gestational age and compared the probabilities of accurate versus misclassification of infant’s gestational age | Omitted outlier measures (> 2 x interquartile range below the first and 3rd quartile). | Cubic spline fitting | Generalized logistic functions | Omitted outliers > 3 SD, LMS parameter smoothing, skew set to one for weight, cubic spline fitting. |
Figure 4.
Flow diagram of studies identified, excluded and included in the systematic review.
Included in the meta-analyses were almost four million (3,986,456) infants at birth (34,639 less than 30 weeks) from six studies for weight (Table 2), and 173,612 infants for head circumference, and 151,527 for length [16,18]. The World Health Organization data measurements were made longitudinally on 882 infants.
Table 2.
Number of infants each week from each study
| Gestational age | Voight, 2010 | Olsen, 2010 | Bertino, 2010 | Kramer, 2001 | Roberts, 1999 | Bonellie, 2008 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
Females |
Males |
Females |
Males |
Females |
Males |
Females |
Males |
Females |
Males |
Females |
Males |
| 22 |
188 |
321 |
- |
- |
- |
- |
80 |
82 |
71 |
74 |
- |
- |
| 23 |
431 |
560 |
133 |
153 |
3 |
8 |
106 |
114 |
79 |
95 |
- |
- |
| 24 |
575 |
704 |
438 |
451 |
20 |
24 |
148 |
156 |
115 |
135 |
120 |
126 |
| 25 |
713 |
846 |
603 |
722 |
40 |
38 |
184 |
202 |
136 |
180 |
115 |
118 |
| 26 |
812 |
968 |
773 |
881 |
35 |
58 |
191 |
234 |
188 |
235 |
179 |
172 |
| 27 |
1073 |
1203 |
966 |
1030 |
52 |
61 |
188 |
254 |
231 |
284 |
174 |
177 |
| 28 |
1276 |
1536 |
1187 |
1281 |
79 |
63 |
287 |
330 |
287 |
361 |
246 |
239 |
| 29 |
1516 |
1838 |
1254 |
1505 |
70 |
72 |
299 |
392 |
325 |
397 |
245 |
265 |
| 30 |
1853 |
2212 |
1606 |
1992 |
107 |
114 |
390 |
467 |
440 |
571 |
317 |
313 |
| 31 |
2283 |
2956 |
2044 |
2460 |
126 |
140 |
461 |
584 |
548 |
743 |
136 |
148 |
| 32 |
* |
* |
3007 |
3677 |
165 |
183 |
795 |
997 |
877 |
1117 |
193 |
205 |
| 33 |
* |
* |
4186 |
5014 |
211 |
240 |
1055 |
1368 |
1200 |
1471 |
239 |
256 |
| 34 |
* |
* |
5936 |
7291 |
263 |
349 |
2018 |
2553 |
2086 |
2657 |
374 |
422 |
| 35 |
* |
* |
5082 |
6952 |
366 |
418 |
3391 |
4314 |
3418 |
4092 |
644 |
653 |
| 36 |
* |
* |
4690 |
7011 |
562 |
665 |
8203 |
9648 |
7320 |
8788 |
1048 |
1265 |
| 37 |
* |
* |
4372 |
6692 |
1291 |
1492 |
17308 |
19965 |
16105 |
18660 |
2006 |
2499 |
| 38 |
* |
* |
5755 |
8786 |
3524 |
3976 |
47516 |
51947 |
47809 |
51404 |
4630 |
6387 |
| 39 |
* |
* |
5978 |
8324 |
5295 |
5452 |
75068 |
77623 |
68846 |
72871 |
8699 |
10706 |
| 40 | * | * | 5529 | 7235 | 5672 | 5653 | 110738 | 112737 | 137570 | 141553 | 12644 | 14230 |
* Not reported.
The individual datasets from the literature showed good agreement with each other, especially along the 50th and lower centiles (Figures 1, 2, and 3) and the meta-analysis curves had a close fit with the individual datasets up to 36 weeks and at 50 weeks (Figures 5, 6, 7). The final splined weight curves were within 3% of the meta-analysis curves for 24 through 36 weeks for both genders, except for a 3.8% difference for girls at 32 weeks along the 90th centile. None of the length measurements differed by more than 1.8% percent between the meta-analysis and the splined curves; all weeks of the head circumference curves were within 1.5%. The meta-analyses for head circumference and length for girls and boys were close enough to normal distributions that normal distributions were used to summarize the data. The measures at 50 weeks were within 0.5% of the WHOGS values.
Figure 5.
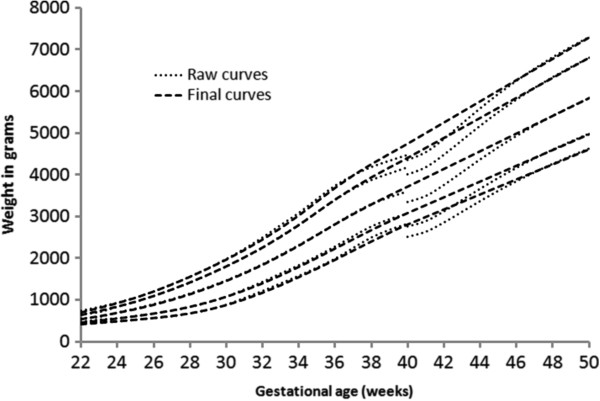
Boys meta-analysis weight curves (dotted) with the final smoothed growth chart curves (dashed).
Figure 6.
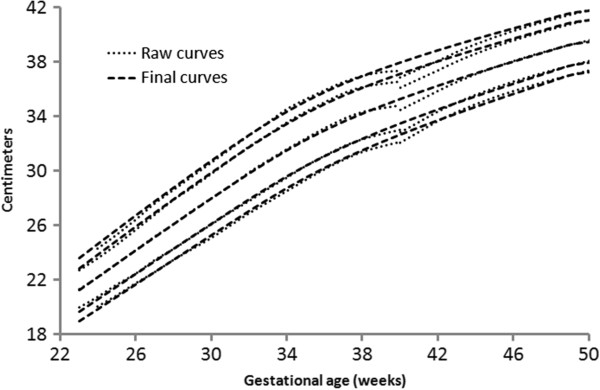
Boys meta-analysis head circumference curves (dotted) with the final smoothed growth chart curves (dashed).
Figure 7.
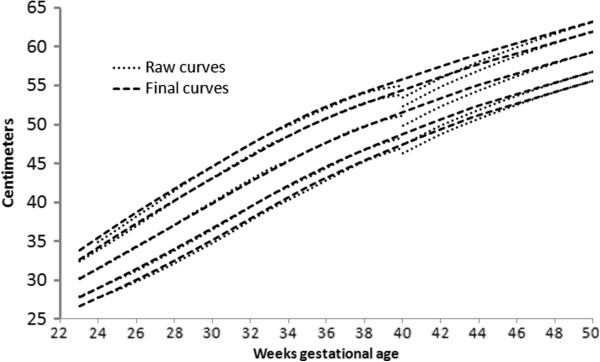
Boys meta-analysis length curves (dotted) with the final smoothed growth chart curves (dashed).
Girl and boy charts were prepared (Figure 8 and 9), by shifting the age by 0.5 weeks to allow plotting by exact age instead of completed weeks. The LMS Parameters [15] were used to develop the exact z-score and percentile calculators for the new growth chart.
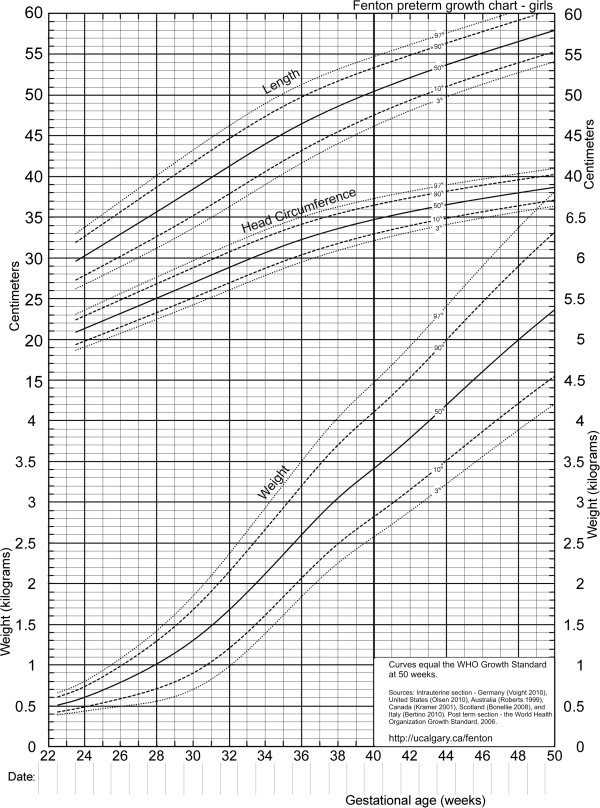
Figure 8.
Revised growth chart for girls.
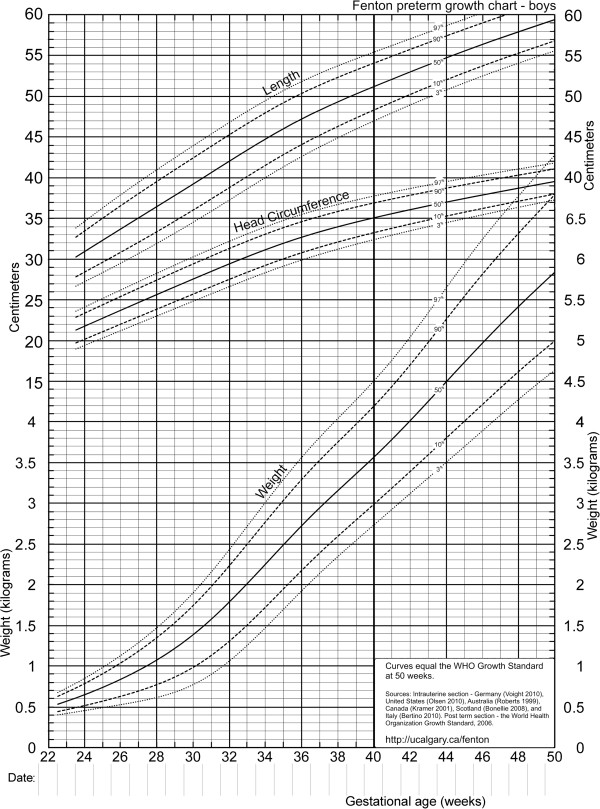
Figure 9.
Revised growth chart for boys.
In the two graphical comparisons between the revised growth charts, one for each sex, with the 2003 Fenton preterm growth chart revealed that the curves were quite similar (Figures 10 and 11). Generally the new girls’ curves were slightly lower (Figure 10) and the new boys’ slightly higher (Figure 11) for all 3 parameters (weight, head circumference, and length) than the 2003 curves. The most dramatic visual and numerical difference between the new charts and the 2003 chart was the higher shift of the boys’ weight curves after 40 weeks compared to the 2003 chart, reaching a maximum difference at 50 weeks of 650, 580, and 740 grams at the 3rd, 50th, and 97th percentiles, respectively. The second biggest visual difference was the lower pattern of the girls’ length curves below 37 weeks; the difference in length reached a maximum numerical value of 1.7 centimeters at 24 weeks along the 97th percentile.
Figure 10.
Comparison of the revised growth chart for girls (solid curves) and the 2003 Fenton growth chart (dashed curves) 3rd, 50th, and 97th percentile curves for length, head circumference, and weight). Both the 2003 and the revised growth curves are shown shifted to actual weeks.
Figure 11.

Comparison of the revised growth chart for boys (solid curves) and the 2003 Fenton growth chart (dashed curves) 3rd, 50th, and 97th percentile curves for length, head circumference, and weight). Both the 2003 and the revised growth curves are shown shifted to actual weeks.
Discussion
We used a strict set of inclusion criteria to include only the best data available to convert fetal and infant size data into fetal-infant growth charts for preterm infants. The revised sex-specific actual-age (versus completed weeks) growth charts (Figure 9 and 10), are based on birth size information of almost four million births with confirmed or corrected gestational ages, born in developed countries (See Features of the new growth chart). The revised charts are based on the recommended growth goal for preterm infants, the fetus and the term infant, with smoothing of the disjunction between these datasets, based on the findings of our international multicentre validation study (Fenton TR, Nasser R, Eliasziw M, Kim JH, Bilan D, Sauve R: Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant, The Preterm Infant Multicentre Growth Study. Submitted BMC Ped 2012). These charts are consistent with the meta-analysis data up to and including 36 weeks, thus they can be used for the assessment of size for gestational age for preterm infants under 37 weeks of gestational age. This growth chart is likely applicable to preterm infants in both developed and developing countries since the data was selected from developed countries to minimize the influence from circumstances that may not have been ideal to support growth.
Features of the new growth chart
•Based on the recommended growth goal for preterm infants: The fetus and the term infant
•Girl and boy specific charts
•Equivalent to the WHO growth charts at 50 weeks gestational age (10 weeks post term age).
•Large preterm birth sample size of 4 million infants;
•Recent population based surveys collected between 1991 to 2007
•Data from developed countries including Germany, Italy, United States, Australia, Scotland, and Canada
•Curves are consistent with the data to 36 weeks, thus can be used to assign size for gestational age up to and including 36 weeks.
•Chart is designed to enable plotting as infants are measured, not as completed weeks. The x axis was adjusted for this chart so that infant size data can be plotted without age adjustment, i.e. Babies should be plotted as exact ages, that is a baby at 25 3/7 weeks should be plotted along the x axis between 25 and 26 weeks.
•Exact z-score and percentile calculator available for download from http://ucalgary.ca/fenton. Data is available for research upon request.
It may be more intuitive to plot on growth charts using exact ages rather than on the basis of complete weeks. Several years ago, the WHO used completed age for growth chart development [12]. This recommendation was likely due to the way data had been collected in the past, that is all 26 0/7 through 26 6/7 week infants were included in the 26 week completed week category. However, with the use of computers to plot on growth charts comes the potential to more accurately plot measurements to the exact day of data collection. Thus the time scale of the horizontal axes of these new growth charts were re-scaled to actual age, for ease of use and understanding. For example, a baby at 25 3/7 can be intuitively plotted between 25 and 26 weeks.
Exact z-score and centile calculators for the revised charts are available for download: http://ucalgary.ca/fenton. Data is available for research upon request.
The data revealed that between 22 weeks to 50 weeks post menstrual age, the fetus/infant multiplies its weight tenfold, for example, the girls’ median weight increased from a median of 520 to 5360 grams. Using a fetal-infant growth chart allows clinicians to compare preterm infants’ growth to an estimated reference of the fetus and the term infant.
There was a remarkably close fit of the included preterm surveys for weight, head circumference and length from the 6 countries, especially at the 50th percentile, even though the data came from different countries.
The splining procedures we used have produced a chart that has integrity and good agreement with the original data. Smoothing of the LMS parameters is recommended since minor fluctuations are more likely due to sampling errors rather than physiological events [15]. Experts recommend that growth charts be developed based on smoothed L, M and S, to constrain the adjacent curves so that they relate to each other smoothly [15]. The World Health Organization set their L parameter to 1 for head circumference and length, while they maintained the exact L values for infants’ weights [58]. The data under study here revealed the same effect as the WHO data; we found that both head circumference and length were close enough to normal distributions that normal distributions could summarize the data, while the exact L’s were needed to retain the nuances of the weight curves.
The differences between the revised growth charts and the 2003 Fenton preterm growth chart may reflect improvements since the selected preterm growth references for the new versions are more likely globally representative of fetal and infant growth. Some of the differences between the current charts and the 2003 version are likely due to the separation into girl and boy charts, since the shifts of the girls’ curves tend to be downward and the boys’ curves upward. The weight shifts after 40 weeks were upward for both sexes, due to the higher values for the WHOGS compared to the CDC growth reference [59] at 10 weeks post term.
The ideal growth pattern of preterm infants remains undefined. These revised growth charts were developed based on the growth patterns of the fetus (as has been determined by size at birth in the large population studies) and the term infant (based on the WHO Growth Standard) [2]. Ultrasound studies and comparison of subgroups of prematurely born infants suggest that the fetal studies, such as those used in this development, may be biased by the premature birth since fetuses who remain in utero likely differ in important ways from babies who are born early [60,61]. However, fetal size from these imperfect studies may be the best data available at this point in time for comparing the growth of preterm infants since the alternative, to compare to in utero infants requires extrapolation from ultrasound measurements. To use other premature infants as the growth reference for preterm infants may not be ideal since the ideal growth of preterm infants has not been defined, has been changing over time [62], and is influenced by the nutrition and medical care received after birth [63,64].
Although the WHOGS is considered to be a growth standard, the infants in the population-based surveys of size at birth are more likely representative of the reference populations and were not selected to be healthy. Thus these growth charts are growth references and are not a growth standard. The INTERGROWTH study, currently underway, will rectify this problem, since their purpose is to develop prescriptive standards for fetal and preterm growth [65].
Conclusion
The inclusion of data from a number of developed countries increases the generalizability of the growth chart. The revised preterm growth chart, harmonized with the World Health Organization Growth Standard at 50 weeks, may support an improved transition of preterm infant growth monitoring to the WHO charts.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
The author’s responsibilities were as follows: JHK suggested the study, TRF & JHK designed the study and conducted independent literature searches, TRF extracted the data, performed the statistical analysis, and wrote the manuscript. Both of the authors contributed to interpret the findings and writing the manuscript, and both authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Tanis R Fenton, Email: tfenton@ucalgary.ca.
Jae H Kim, Email: neojae@ucsd.edu.
Acknowledgements
Many thanks to Patrick Fenton and Misha Eliasziw for statistical assistance, Roseann Nasser, Reg Sauve, Debbie O’Connor, and Sharon Unger for encouragement and advice, and Jayne Thirsk for editing advice.
References
- Secker D. Promoting optimal monitoring of child growth in Canada: using the new WHO growth charts. Can J Diet Pract Res. 2010;71:e1–e3. doi: 10.3148/71.1.2010.54. [DOI] [PubMed] [Google Scholar]
- De Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull. 2004;25:S15–S26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- Borghi E, De Onis M, Garza C, den BJ V, Frongillo EA, Grummer-Strawn L, Van Buuren S, Pan H, Molinari L, Martorell R, Onyango AW, Martines JC. Construction of the World Health Organization child growth standards: selection of methods for attained growth curves. Stat Med. 2006;25:247–265. doi: 10.1002/sim.2227. [DOI] [PubMed] [Google Scholar]
- Dietitians of Canada, Canadian Pediatric Society, College of Family Physicians of Canada, Community Health Nurses of Canada. Promoting Optimal Monitoring of Child Growth in Canada: Using the New WHO Growth Charts. Can J Diet Pract Res. 2010;71:1–22. doi: 10.3148/71.1.2010.54. [DOI] [PubMed] [Google Scholar]
- Committee on Nutrition American Academy Pediatrics. Nutritional Needs of Preterm Infants. 6. Elk Grove Village Il: American Academy Pediatrics; 2009. (Pediatric Nutrition Handbook). [Google Scholar]
- Agostoni C, Buonocore G, Carnielli VP, De CM, Darmaun D, Decsi T. Enteral nutrient supply for preterm infants. A comment of the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91. doi: 10.1097/MPG.0b013e3181adaee0. [DOI] [PubMed] [Google Scholar]
- Nutrition Committee, Canadian Paediatric Society. Nutrient needs and feeding of premature infants. CMAJ. 1995;152:1765–1785. [PMC free article] [PubMed] [Google Scholar]
- United Nations Statistics Division: Composition of macro geographical (continental) regions, geographical sub-regions, and selected economic and other groupings. http://unstats.un.org/unsd/methods/m49/m49regin.htm#developed.
- Niklasson A, Engstrom E, Hard AL, Wikland KA, Hellstrom A. Growth in very preterm children: a longitudinal study. Pediatr Res. 2003;54:899–905. doi: 10.1203/01.PDR.0000091287.38691.EF. [DOI] [PubMed] [Google Scholar]
- Bertino E, Coscia A, Mombro M, Boni L, Rossetti G, Fabris C, Spada E, Milani S. Postnatal weight increase and growth velocity of very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 2006;91:F349–F356. doi: 10.1136/adc.2005.090993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krauel VX, Figueras AJ, Natal PA, Iglesias PI, Moro SM, Fernandez PC, Martin-Ancel A. Reduced postnatal growth in very low birth weight newborns with GE < or = 32 weeks in Spain. An Pediatr (Barc) 2008;68:206–212. doi: 10.1157/13116698. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- Hennekens CH, Buring JE. In: Epidemiology in Medicine. Mayrent SL, Little B, editor. Boston; 1987. Analysis of epidemiologic studies: Evaluating the role of confounding; pp. 287–323. [Google Scholar]
- Voigt M, Zels K, Guthmann F, Hesse V, Gorlich Y, Straube S. Somatic classification of neonates based on birth weight, length, and head circumference: quantification of the effects of maternal BMI and smoking. J Perinat Med. 2011;39:291–297. doi: 10.1515/jpm.2011.017. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med. 1992;11:1305–1319. doi: 10.1002/sim.4780111005. [DOI] [PubMed] [Google Scholar]
- Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–e224. doi: 10.1542/peds.2009-0913. [DOI] [PubMed] [Google Scholar]
- Roberts CL, Lancaster PA. Australian national birthweight percentiles by gestational age. Med J Aust. 1999;170:114–118. doi: 10.5694/j.1326-5377.1999.tb127678.x. [DOI] [PubMed] [Google Scholar]
- Bertino E, Spada E, Occhi L, Coscia A, Giuliani F, Gagliardi L, Gilli G, Bona G, Fabris C, De CM, Milani S. Neonatal anthropometric charts: the Italian neonatal study compared with other European studies. J Pediatr Gastroenterol Nutr. 2010;51:353–361. doi: 10.1097/MPG.0b013e3181da213e. [DOI] [PubMed] [Google Scholar]
- Bonellie S, Chalmers J, Gray R, Greer I, Jarvis S, Williams C. Centile charts for birthweight for gestational age for Scottish singleton births. BMC Pregnancy Childbirth. 2008;8:5. doi: 10.1186/1471-2393-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, Blondel B, Breart G. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35. doi: 10.1542/peds.108.2.e35. [DOI] [PubMed] [Google Scholar]
- Karna P, Brooks K, Muttineni J, Karmaus W. Anthropometric measurements for neonates, 23 to 29 weeks gestation, in the 1990s. Paediatr Perinat Epidemiol. 2005;19:215–226. doi: 10.1111/j.1365-3016.2005.00641.x. [DOI] [PubMed] [Google Scholar]
- Kwan AL, Verloove-Vanhorick SP, Verwey RA, Brand R. Ruys JH: [Birth weight percentiles of premature infants needs to be updated] Ned Tijdschr Geneeskd. 1994;138:519–522. [PubMed] [Google Scholar]
- Riddle WR, DonLevy SC, Lafleur BJ, Rosenbloom ST, Shenai JP. Equations describing percentiles for birth weight, head circumference, and length of preterm infants. J Perinatol. 2006;26:556–561. doi: 10.1038/sj.jp.7211572. [DOI] [PubMed] [Google Scholar]
- Figueras F, Figueras J, Meler E, Eixarch E, Coll O, Gratacos E, Gardosi J, Carbonell X. Customised birthweight standards accurately predict perinatal morbidity. Arch Dis Child Fetal Neonatal Ed. 2007;92:F277–F280. doi: 10.1136/adc.2006.108621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fok TF, So HK, Wong E, Ng PC, Chang A, Lau J, Chow CB, Lee WH. Updated gestational age specific birth weight, crown-heel length, and head circumference of Chinese newborns. Arch Dis Child Fetal Neonatal Ed. 2003;88:F229–F236. doi: 10.1136/fn.88.3.F229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole TJ, Williams AF, Wright CM. Revised birth centiles for weight, length and head circumference in the UK-WHO growth charts. Ann Hum Biol. 2011;38:7–11. doi: 10.3109/03014460.2011.544139. [DOI] [PubMed] [Google Scholar]
- Salomon LJ, Bernard JP, Ville Y. Estimation of fetal weight: reference range at 20–36 weeks’ gestation and comparison with actual birth-weight reference range. Ultrasound Obstet Gynecol. 2007;29:550–555. doi: 10.1002/uog.4019. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Freeman JV, Preece MA. British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Stat Med. 1998;17:407–429. doi: 10.1002/(SICI)1097-0258(19980228)17:4<407::AID-SIM742>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Gibbons K, Chang A, Flenady V, Mahomed K, Gardener G, Gray PH. Validation and refinement of an Australian customised birthweight model using routinely collected data. Aust N Z J Obstet Gynaecol. 2010;50:506–511. doi: 10.1111/j.1479-828X.2010.01219.x. [DOI] [PubMed] [Google Scholar]
- Ogawa Y, Iwamura T, Kuriya N, Nishida H, Takeuchi H, Takada M. Birth size standards by gestational age for Japanese neonates. Acta Neonat Jpn. 1998;34:624–632. [Google Scholar]
- Storms MR, Van Howe RS. Birthweight by gestational age and sex at a rural referral center. J Perinatol. 2004;24:236–240. doi: 10.1038/sj.jp.7211065. [DOI] [PubMed] [Google Scholar]
- Romano-Zelekha O, Freedman L, Olmer L, Green MS, Shohat T. Should fetal weight growth curves be population specific? Prenat Diagn. 2005;25:709–714. doi: 10.1002/pd.1194. [DOI] [PubMed] [Google Scholar]
- Ooki S, Yokoyama Y. Reference birth weight, length, chest circumference, and head circumference by gestational age in Japanese twins. J Epidemiol. 2003;13:333–341. doi: 10.2188/jea.13.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergara G, Carpentieri M, Colavita C. Birthweight centiles in preterm infants. A new approach. Minerva Pediatr. 2002;54:221–225. [PubMed] [Google Scholar]
- Bernstein IM, Mohs G, Rucquoi M, Badger GJ. Case for hybrid “fetal growth curves”: a population-based estimation of normal fetal size across gestational age. J Matern Fetal Med. 1996;5:124–127. doi: 10.1002/(SICI)1520-6661(199605/06)5:3<124::AID-MFM5>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Ramos F, Perez G, Jane M, Prats R. Construction of the birth weight by gestational age population reference curves of Catalonia (Spain): Methods and development. Gac Sanit. 2009;23:76–81. doi: 10.1016/j.gaceta.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Visser GH, Eilers PH, Elferink-Stinkens PM, Merkus HM, Wit JM. New Dutch reference curves for birthweight by gestational age. Early Hum Dev. 2009;85:737–744. doi: 10.1016/j.earlhumdev.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Roberts C, Mueller L, Hadler J. Birth-weight percentiles by gestational age, Connecticut 1988–1993. Conn Med. 1996;60:131–140. [PubMed] [Google Scholar]
- Zhang X, Platt RW, Cnattingius S, Joseph KS, Kramer MS. The use of customised versus population-based birthweight standards in predicting perinatal mortality. BJOG. 2007;114:474–477. doi: 10.1111/j.1471-0528.2007.01273.x. [DOI] [PubMed] [Google Scholar]
- Gielen M, Lindsey PJ, Derom C, Loos RJ, Souren NY, Paulussen AD, Zeegers MP, Derom R, Vlietinck R, Nijhuis JG. Twin-specific intrauterine ‘growth’ charts based on cross-sectional birthweight data. Twin Res Hum Genet. 2008;11:224–235. doi: 10.1375/twin.11.2.224. [DOI] [PubMed] [Google Scholar]
- Monroy-Torres R, Ramirez-Hernandez SF, Guzman-Barcenas J, Naves-Sanchez J. [Comparison between five growth curves used in a public hospital] Rev Invest Clin. 2010;62:121–127. [PubMed] [Google Scholar]
- Blair EM, Liu Y, de Klerk NH, Lawrence DM. Optimal fetal growth for the Caucasian singleton and assessment of appropriateness of fetal growth: an analysis of a total population perinatal database. BMC Pediatr. 2005;5:13. doi: 10.1186/1471-2431-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrascosa A, Yeste D, Copil A, Almar J, Salcedo S, Gussinye M. [Anthropometric growth patterns of preterm and full-term newborns (24–42 weeks’ gestational age) at the Hospital Materno-Infantil Vall d’Hebron (Barcelona)(1997–2002] An Pediatr (Barc) 2004;60:406–416. doi: 10.1016/s1695-4033(04)78299-5. [DOI] [PubMed] [Google Scholar]
- Rousseau T, Ferdynus C, Quantin C, Gouyon JB, Sagot P. [Liveborn birth-weight of single and uncomplicated pregnancies between 28 and 42 weeks of gestation from Burgundy perinatal network] J Gynecol Obstet Biol Reprod (Paris) 2008;37:589–596. doi: 10.1016/j.jgyn.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Polo A, Pezzotti P, Spinelli A, Di LD. Comparison of two methods for constructing birth weight charts in an Italian region. Years 2000–2003. Epidemiol Prev. 2007;31:261–269. [PubMed] [Google Scholar]
- Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montoya-Restrepo NE, Correa-Morales JC. [Birth-weight curves] Rev Salud Publica (Bogota) 2007;9:1–10. doi: 10.1590/s0124-00642007000100002. [DOI] [PubMed] [Google Scholar]
- Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon ES. Birth weight standards in the live-born population in Israel. Isr Med Assoc J. 2005;7:311–314. [PubMed] [Google Scholar]
- Kierans WJ, Kendall PRW, Foster LT, Liston RM, Tuk T. New birth weight and gestational age charts for the British Columbia population. BC Medical J. 2006;48:28–32. [Google Scholar]
- Uehara R, Miura F, Itabashi K, Fujimura M, Nakamura Y. Distribution of birth weight for gestational age in Japanese infants delivered by cesarean section. J Epidemiol. 2011;21:217–222. doi: 10.2188/jea.JE20100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsky S, Easterling TR, Holt VL, Critchlow CW. Detecting small for gestational age infants: the development of a population-based reference for Washington state. Am J Perinatol. 2005;22:405–412. doi: 10.1055/s-2005-872595. [DOI] [PubMed] [Google Scholar]
- Niklasson A, Albertsson-Wikland K. Continuous growth reference from 24th week of gestation to 24 months by gender. BMC Pediatr. 2008;8:8. doi: 10.1186/1471-2431-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GR, Kogan MD, Himes JH. 1994–1996 U.S. singleton birth weight percentiles for gestational age by race, Hispanic origin, and gender. Matern Child Health J. 1999;3:225–231. doi: 10.1023/A:1022381506823. [DOI] [PubMed] [Google Scholar]
- Davidson S, Sokolover N, Erlich A, Litwin A, Linder N, Sirota L. New and improved Israeli reference of birth weight, birth length, and head circumference by gestational age: a hospital-based study. Isr Med Assoc J. 2008;10:130–134. [PubMed] [Google Scholar]
- Kato N, A. [Reference birthweight for multiple births in Japan] Nihon Koshu Eisei Zasshi. 2002;49:361–370. [PubMed] [Google Scholar]
- Braun L, Flynn D, Ko CW, Yoder B, Greenwald JR, Curley BB, Williams R, Thompson MW. Gestational age-specific growth parameters for infants born at US military hospitals. Ambul Pediatr. 2004;4:461–467. doi: 10.1367/A03-022R.1. [DOI] [PubMed] [Google Scholar]
- Thomas P, Peabody J, Turnier V, Clark RH. A new look at intrauterine growth and the impact of race, altitude, and gender. Pediatrics. 2000;106:E21. doi: 10.1542/peds.106.2.e21. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The WHO Child Growth Standards. http://www.who.int/childgrowth/standards/en/
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- Hutcheon JA, Platt RW. The missing data problem in birth weight percentiles and thresholds for “small-for-gestational-age”. Am J Epidemiol. 2008;167:786–792. doi: 10.1093/aje/kwm327. [DOI] [PubMed] [Google Scholar]
- Sauer PJ. Can extrauterine growth approximate intrauterine growth? Should it? Am J Clin Nutr. 2007;85:608S–613S. doi: 10.1093/ajcn/85.2.608S. [DOI] [PubMed] [Google Scholar]
- Christensen RD, Henry E, Kiehn TI, Street JL. Pattern of daily weights among low birth weight neonates in the neonatal intensive care unit: data from a multihospital health-care system. J Perinatol. 2006;26:37–43. doi: 10.1038/sj.jp.7211431. [DOI] [PubMed] [Google Scholar]
- Valentine CJ, Fernandez S, Rogers LK, Gulati P, Hayes J, Lore P, Puthoff T, Dumm M, Jones A, Collins K, Curtiss J, Hutson K, Clark K, Welty SE. Early amino-acid administration improves preterm infant weight. J Perinatol. 2009;29:428–432. doi: 10.1038/jp.2009.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senterre T, Rigo J. Reduction in postnatal cumulative nutritional deficit and improvement of growth in extremely preterm infants. Acta Paediatr. 2012;101:e64–e70. doi: 10.1111/j.1651-2227.2011.02443.x. [DOI] [PubMed] [Google Scholar]
- Study Coordinating Unit. INTERGROWTH-21st. http://intergrowth21.org.uk/