Abstract
Background
Total fat and omega-3 fatty acids in the diet may affect breast cancer risk by altering estrogen metabolism. The purpose of this study was to elucidate the effects of differing total fat and omega-3 fatty acid content of diets on a panel of urinary estrogens and metabolites.
Findings
A controlled, cross-over feeding trial was conducted in postmenopausal women using three test diets: high fat diet (HF; 40% energy from fat), low fat diet (LF; 20% of energy from fat) and low fat, high omega-3 diet (LFn3; 23% energy from fat; 3% omega-3 fatty acids) for 8 week periods. Urinary hormone concentrations for 16 women were compared among diets using a linear mixed model, and within diet comparisons were made using paired t-tests. Urinary excretion of estrone was greater after the LF and LFn3 compared to the HF (P = 0.004). Estrone excretion was increased from baseline within the LF only (P = 0.02). Total estrone + estradiol + estriol increased from baseline with LF (P = 0.02) and was greater than the other two diets at 8 weeks (P = 0.03). There were no effects on estrogen metabolites, including the 2-hydroxy estrone:16α-hydroxy estrone ratio.
Conclusions
The results of this study indicate that urinary sex hormone metabolism was modestly altered in postmenopausal women by a low fat dietary intervention.
Keywords: Dietary fat, Omega-3 fatty acids, Low fat diet, Urinary estrogens, Postmenopausal women
Finding
Introduction
High concentrations of estrogens in blood and urine are associated with increased risk of breast cancer in postmenopausal women [1], and one hypothesis is that this increased risk is mediated by sex hormone metabolism. Low fat diets resulted in significant reductions in circulating estrogens in some studies in postmenopausal women [2-4]. Dietary omega-3 fatty acids (n-3) may suppress tumorigenesis by inhibition of inflammatory eicosanoids, suppression of aromatase, and conversion of androgens to estrogens [5].
In addition to promoting growth via interaction with estrogen receptors, circulating estrogens are metabolized by hydroxylation reactions resulting in an array of metabolites with varying biological activity relative to the parent estrogens, with some having genotoxic activity [6]. Sixteen-α-hydroxy estrone (16αOH-E1) is a potent mitogen, tumor initiator, and tumor promoter in vitro[7]. 16α-hydroxylation of estrogens was enhanced in women with breast cancer relative to healthy controls [8,9]. A higher ratio of 2-hydroxy estrone (2OH-E1) to 16αOH-E1 (2:16αOH-E1 ratio) indicated decreased breast cancer risk in some studies [10,11]; however, other investigations do not support this association [12,13].
We have previously shown that a high fat diet elevates plasma estradiol [14]. The purpose of the present study was to determine the effects of diets with varying amounts of fat and n-3 on urinary estrogens and estrogen metabolites in healthy postmenopausal women. We hypothesized that compared to a high fat diet, diets low in fat or low in fat with high n-3 would decrease individual and total estrogens, 16αOH-E1, and the carcinogenic 4-hydroxy metabolites.
Subjects and methods
Experimental protocol
Complete details of the study design and treatments are described elsewhere [14]. The effects of controlled test diets: a high fat diet (HF; 40% energy as fat, 15% energy as protein, and 45% energy as carbohydrate), a low fat diet (LF; 20% energy as fat, 15% energy as protein, and 65% energy as carbohydrate) and a low fat diet with n-3 fatty acids (LFn3; 23% energy as fat [3% n-3], 15% energy as protein, and 62% energy as carbohydrate) on urinary estrogen metabolism were compared in a randomized, cross-over trial. All nutrient analysis was performed by a registered dietitian (SKR) using the Nutritionist V nutrient analysis program (Axxya Systems, Stafford, TX). Subjects consumed each diet in random order for 8 weeks with a 6–12 week washout between treatments. Reported dietary compliance was >99% for energy and >99.5% for omega-3 fatty acids [14].
The study was carried out from 2004–2008. The study was approved by the U.S. Army Medical Research and Materiel Command’s Human Subjects Research Review Board and the University of Minnesota Committee for the Use of Human Subjects in Research. Written informed consent was obtained from all subjects. The trial was retrospectively registered at http://www.clinicaltrials.gov as NCT01824498.
Subjects
Subject characteristics and recruitment are discussed elsewhere [14]. Participants were healthy postmenopausal women; age 45 – 70 years; had a body mass index of 19 – 32 kg/m2; had not lost or gained more than 5 pounds in the last 6 months; and had not used fish oil supplements or hormone replacement therapy for 2 months prior to the trial. Subjects were excluded if they had any active disease process, used prescription medications, or had both ovaries removed. None of the participants had prior a prior breast cancer diagnosis.
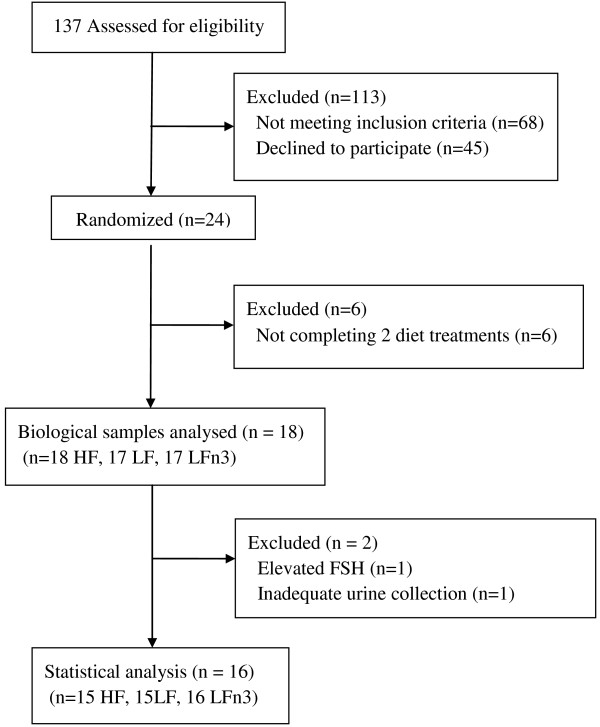
Seventeen subjects completed all three dietary treatments and one subject completed two treatments. One subject was excluded from the analysis because her follicle stimulating hormone concentration was intermittently in the premenopausal range. Another subject was excluded due to improperly collected urine specimens. One subject was missing urine samples for HF. In total, 15 subjects completed HF, 15 subjects completed LF, and 16 subjects completed LFn3 and are included in the final analysis. Figure 1 illustrates the flow of participants through the trial.
Figure 1.
Flow diagram of participants from screening to data analysis.
Urine collection
Subjects collected two consecutive 24-hour urine specimens at home on weeks 0 and 8 of each treatment period. Urine was pooled and sodium azide was added to 0.1%. Aliquots were immediately stored at −20°C until analysis.
Plasma phospholipid fatty acids
Plasma phospholipid fatty acids (PLFA) were analyzed by gas chromatography (Lipid Technologies, Austin, MN) as previously reported (14). Analysis was done to determine the effects of dietary treatments on PLFA content (μg/ml) of linoleic acid (LA, 18:2n6), α-linolenic acid (ALA, 18:3n3), arachidonic acid (AA, 20:4n6), eicosapentaenoic acid (EPA, 20:5n3) and docosahexaenoic acid (DHA, 22:6n3), total n3, total n6 and the n3/n6 ratio.
Estrogen metabolite assay by LC/MS-MS
LC-MS methods were used to determine urinary estrogens and estrogen metabolites [15,16]. Unless otherwise noted, all laboratory chemicals were obtained from Fisher Scientific (Pittsburg, PA). 10 μL of deuterated-estrogen metabolite internal standard solution (ISS; C/D/N Isotopes, Inc., Pointe-Claire, Quebec, Canada) containing representative analytes of each class of compounds were added to duplicate 1.0 ml urine aliquots, followed by 1.0 mL of freshly prepared enzymatic hydrolysis buffer containing 2 mg of L-ascorbic acid, 5 μL of β-glucuronidase/sulfatase (Type H-2; Sigma-Aldrich, St Louis, MO), and 1.0 mL of 0.15 M sodium acetate buffer (pH 4.1) and incubated overnight at 37°C.
Samples were extracted with ethyl ether and evaporated to dryness at 40°C under nitrogen. 25 μL of 0.1 M sodium bicarbonate buffer with 0.1% ascorbic acid (pH at 9.0) and 25 μL of dansyl chloride solution (3 mg/mL in acetone; Lancaster Synthesis, Inc., Pelham, NH) were added to each dried sample. Each sample was heated at 65°C for 6 minutes to form estrogen metabolite and deuterated estrogen metabolite dansyl derivatives. Calibration standards (Steraloids, Inc., Newport, RI) and quality control samples were similarly hydrolyzed, extracted, and derivatized.
Chromatographic separation was performed on a 100 × 0.5 mm (i.d.) Zorbax SB-C18 column 1.8μm particle size (Agilent Technologies, Santa Clara, CA). The mobile phase consisted of two eluents, solvent A (50 mL/L acetonitrile + 950 mL/L H2O containing 1 mL/L formic acid) and solvent B (475 mL/L acetonitrile + 475 mL/L methanol + 50 mL/L H2O containing 1 mL/L formic acid). LC/MS-MS analysis was performed on a Thermo Electron Quantum Discovery Max Triple Quadrupole Instrument. Quantitative analysis was performed using Thermo Electron Xcalibur proprietary software. All samples from a given subject were batch analyzed. Intra-batch coefficients of variation varied from 5.1 – 12.2%. Inter-batch coefficients of variation for quality control samples varied from 6.3 – 27.9% among hormones.
Statistical analysis
Data for urinary sex hormone metabolites were not normally distributed and are reported as geometric means and 95% confidence intervals. SAS Proc Mixed (SAS version 9.2, SAS Institute Inc., Cary, NC; 2002–2008) was used to fit a mixed effects linear model for each outcome with a random effect for subject to account for multiple correlated measurements within each subject. These effect models handled isolated missing values and were used to assess period and carryover effects. Least squares means generated from the mixed model were compared between treatments. Paired t-tests were applied to within diet differences. A P-value of < 0.05 was considered statistically significant.
Results
Study participants were slightly overweight (mean BMI 27 kg/m2, Table 1) mostly white (88%) middle-aged women (mean age 58 ± 6 years).
Table 1.
Characteristics of study subjects at baselinea
| Characteristic | Value |
|---|---|
| Age (years) |
58 ± 6 |
| Body weight (kg) |
74 ± 11 |
| Height (cm) |
165 ± 5 |
| BMI (kg/m2) |
27 ± 4 |
| Systolic blood pressure (mmHg) |
118 ± 15 |
| Diastolic blood pressure (mmHg) |
71 ± 8 |
| Follicle stimulating hormone (mIU/mL)b |
73 ± 22 |
| Ethnicity (n (%)) |
|
| White |
14 (88) |
| Hispanic |
1 (6) |
| African-American | 1 (6) |
aAll values are means ± standard deviations except ethnic groups, which are n (%); n = 16.
bBaseline follicle stimulating hormone values for all women ≤ 55 years old; n = 11.
Plasma phospholipid fatty acids
The results for n-3 and n-6 in PLFA are presented in Table 2. The LFn3 diet, which was low fat with supplemental n-3 promoted enhanced inclusion of total n-3, ALA, EPA and DHA into PLFA compared to the HF and LF diets (all p < 0.0001). The increases in n-3 were accompanied by a reduction in total n-6, LA, and ARA. In comparison to HF, LF promoted increased ARA and DHA (p=.02, p=.03, respectively).
Table 2.
Baseline, 8 weeks, and change from baseline to 8 weeks concentrations for n3 and n6 plasma phospholipid fatty acids in μg/ml1
|
High fat |
Low fat |
Low fat + n-3 |
|
|
|---|---|---|---|---|
| n = 17 | n = 16 | n = 17 | p-value2 | |
| 18:2n6 |
|
|
|
|
| Baseline |
280.69 ± 14.57 |
284.66 ± 14.76 |
293.95 ± 14.59 |
0.41 |
| 8 weeks |
285.49 ± 12.54a |
269.21 ± 12.86a |
233.08 ± 12.59b* |
0.0006 |
| Δ 8 weeks |
4.81 ± 10.90a |
−16.08 ± 11.29a |
−60.85 ± 10.95b |
0.0001 |
| p-value3 |
0.66 |
0.16 |
< 0.0001 |
|
| 18:3n3 |
|
|
|
|
| Baseline |
4.00 ± 0.86 |
4.51 ± 0.88 |
3.22 ± 0.86 |
0.34 |
| 8 weeks |
2.57 ± 0.45a |
3.12 ± 0.47a |
6.85 ± 0.45b* |
< 0.0001 |
| Δ 8 weeks |
−1.43 ± 0.79a |
−1.30 ± 0.82a |
3.62 ± 0.79b |
< 0.0001 |
| p-value3 |
0.08 |
0.12 |
< 0.0001 |
|
| 20:4n6 |
|
|
|
|
| Baseline |
120.62 ± 7.83 |
121.51 ± 7.94 |
126.04 ± 7.84 |
0.59 |
| 8 weeks |
107.89 ± 7.14a* |
135.62 ± 7.34b* |
100.12 ± 7.17a* |
0.0001 |
| Δ 8 weeks |
−12.72 ± 5.13a |
13.47 ± 5.33b |
−25.90 ± 5.16a |
< 0.0001 |
| p-value3 |
0.02 |
0.02 |
< 0.0001 |
|
| 20:5n-3 |
|
|
|
|
| Baseline |
11.43 ± 1.77 |
11.80 ± 1.82 |
9.69 ± 1.78 |
0.49 |
| 8 weeks |
6.89 ± 1.80a* |
9.99 ± 1.87a |
29.86 ± 1.81b* |
< 0.0001 |
| Δ 8 weeks |
−4.54 ± 1.94a |
−1.91 ± 2.02a |
20.17 ± 1.96b |
< 0.0001 |
| p-value3 |
0.02 |
0.35 |
< 0.0001 |
|
| 22:5n-3 |
|
|
|
|
| Baseline |
9.94 ± 0.78 |
10.56 ± 0.79 |
10.72 ± 0.78 |
0.49 |
| 8 weeks |
8.41 ± 0.88a* |
11.04 ± 0.91b |
13.45 ± 0.89c* |
< 0.0001 |
| Δ 8 weeks |
−1.52 ± 0.69a |
0.36 ± 0.72a |
2.73 ± 0.70b |
< 0.0001 |
| p-value3 |
0.03 |
0.62 |
0.0003 |
|
| 22:6n-3 |
|
|
|
|
| Baseline |
30.18 ± 2.82 |
28.90 ± 2.89 |
29.68 ± 2.83 |
0.89 |
| 8 weeks |
24.06 ± 3.77a* |
35.03 ± 3.90b* |
55.00 ± 3.78c* |
< 0.0001 |
| Δ 8 weeks |
−6.12 ± 2.56a |
5.95 ± 2.65b |
25.32 ± 2.57c |
< 0.0001 |
| p-value3 |
0.02 |
0.03 |
< 0.0001 |
|
| Total n-3 |
|
|
|
|
| Baseline |
59.71 ± 5.33 |
60.07 ± 5.42 |
56.75 ± 5.34 |
0.68 |
| 8 weeks |
44.50 ± 6.37a* |
62.86 ± 6.60b |
110.10 ± 6.41c* |
< 0.0001 |
| Δ 8 weeks |
−15.21 ± 4.95a |
2.55 ± 5.14b |
54.36 ± 4.98c |
< 0.0001 |
| p-value3 |
0.004 |
0.62 |
< 0.0001 |
|
| Total n-6 |
|
|
|
|
| Baseline |
452.87 ± 21.30 |
456.78 ± 21.57 |
468.55 ± 21.34 |
0.53 |
| 8 weeks |
432.99 ± 18.17a |
458.41 ± 18.74a |
370.63 ± 18.25b* |
0.0005 |
| Δ 8 weeks |
−19.85 ± 14.82a |
−0.58 ±15.34a |
−97.85 ± 14.89b |
< 0.0001 |
| p-value3 | 0.19 | 0.97 | < 0.0001 |
1All values are LS means ± standard error.
2p-value for effect of treatment across the three diets evaluated using a general linear mixed model. Values with differing letters as a superscript are significantly different at p < 0.05.
3p-value for paired t-test comparing baseline and 8 weeks means within each diet.
*8 week mean is significantly different from baseline mean.
Urinary sex hormones
Urinary estrone (E1) excretion was significantly greater after LF and LFn3 compared to HF (P = 0.004, Table 3), although E1 excretion was significantly increased from baseline with LF only (P = 0.02). Excretion of the sum of E1, estradiol (E2) and estriol (E3) was significantly greater with LF than HF at 8 weeks (P = 0.03) and E1+ E2 + E3 increased significantly from baseline to 8 weeks with LF (P = 0.02). Urinary excretion of 2OH-E1, 2-methoxy estrone (2-ME1), 2-methoxy estradiol (2-ME2), 4-hydroxy estrone (4OH-E1), 16αOH-E1, 2:16αOH-E1 ratio and total estrogens were not significantly different among test diets at 8 weeks. Urinary 2-hydroxy estradiol (2OH-E2), 4-hydroxy estradiol (4OH-E2), 4-methoxy estrone (4-ME1), and 4-methoxy estradiol (4-ME2) were undetectable in urine.
Table 3.
Baseline and 8 week values for urinary estrogens and metabolites for the HF, LF and LFn3a
| Analyte |
HF |
LF |
LFn3 |
P-valued |
|---|---|---|---|---|
| n = 15b | n = 15c | n = 16 | ||
| Estrone (E1) (nmol/day) |
|
|
|
|
| Baseline |
6.7 (4.8, 9.5) |
7.2 (5.1, 10.1) |
8.1 (5.8, 11.5) |
0.36 |
| 8 weeks |
6.3 (4.4, 9.1) § |
9.9 (6.9, 14.2) †** |
8.5 (5.9, 12.1) † |
0.004 |
| P-valuee |
0.39 |
0.02 |
0.92 |
|
| Estradiol (E2) (nmol/day) |
|
|
|
|
| Baseline |
2.0 (1.0, 3.8) |
2.2 (1.2, 4.3) |
1.4 (0.7, 2.6) |
0.36 |
| 8 weeks |
1.0 (0.5, 2.1) |
2.1 (1.0, 4.4) |
1.7 (0.8, 3.4) |
0.12 |
| P-valuee |
0.37 |
0.47 |
0.83 |
|
| Estriol (E3) (nmol/day) |
|
|
|
|
| Baseline |
7.2 (3.1, 16.8) |
8.5 (3.6, 19.9) |
10.8 (4.7, 25.0) |
0.62 |
| 8 weeks |
11.8 (6.3, 22.0) |
14.3 (7.7, 26.7) |
11.7 (6.3, 21.5) |
0.79 |
| P-valuee |
0.84 |
0.12 |
0.64 |
|
| E1 + E2 + E3 (nmol/day) |
|
|
|
|
| Baseline |
22.9 (15.3, 34.4) |
24.8 (16.6, 37.1) |
23.0 (15.4, 34.2) |
0.77 |
| 8 weeks |
21.5 (14.3, 32.2)§ |
35.7 (23.9, 53.4)†** |
26.8 (18.1, 39.8)§† |
0.03 |
| P-valuee |
0.51 |
0.02 |
0.60 |
|
| 2-hydroxyestrone (2OH-E1) (nmol/day) |
|
|
|
|
| Baseline |
22.7 (16.5, 31.2)§† |
25.0 (18.2, 34.4)§ |
18.5 (13.5, 25.3)† |
0.02 |
| 8 weeksf |
17.6 (13.7, 22.7) |
20.4 (15.8, 26.3) |
24.1 (18.8, 30.9) |
0.23 |
| P-valuee |
0.19 |
0.81 |
0.29 |
|
| 2-methoxyestrone (2-ME1)(nmol/day) |
|
|
|
|
| Baseline |
1.6 (0.7, 3.8) |
3.4 (1.5, 7.8) |
3.1 (1.4, 7.1) |
0.21 |
| 8 weeks |
1.4 (0.7, 3.1) |
2.1 (0.9, 4.5) |
3.3 (1.5, 7.1) |
0.23 |
| P-valuee |
0.98 |
0.48 |
0.91 |
|
| 2-methoxyestradiol (2-ME2) (nmol/day) |
|
|
|
|
| Baseline |
1.3 (0.6, 3.3) |
3.9 (1.6, 9.4) |
1.7 (0.7, 3.9) |
0.09 |
| 8 weeks |
0.9 (0.4, 2.1) |
1.0 (0.4, 2.3) |
1.7 (0.8, 4.0) |
0.39 |
| P-valuee |
0.84 |
0.08 |
0.57 |
|
| 4-hydroxyestrone (4OH-E1) (nmol/day) |
|
|
|
|
| Baseline |
0.78 (0.51, 1.21) |
1.08 (0.70, 1.68) |
1.17 (0.76, 1.80) |
0.21 |
| 8 weeks |
0.92 (0.66, 1.27) |
1.05 (0.76, 1.45) |
1.28 (0.93, 1.75) |
0.25 |
| P-valuee |
0.64 |
0.93 |
0.50 |
|
| 16α-hydroxyestrone (16αOH-E1) (nmol/day) |
|
|
|
|
| Baseline |
2.03 (1.10, 3.75) |
2.39 (1.29, 4.44) |
1.70 (0.93, 3.11) |
0.62 |
| 8 weeks |
1.50 (0.82, 2.74) |
2.34 (1.27, 4.29) |
2.03 (1.12, 3.65) |
0.52 |
| P-valuee |
0.47 |
0.22 |
0.32 |
|
| Total Estrogens (nmol/day) |
|
|
|
|
| Baseline |
73.7 (52.7, 100.1) |
83.7 (60.9, 115.0) |
72.8 (53.1, 99.6) |
0.38 |
| 8 weeks |
65.5 (45.8, 93.8) |
86.4 (60.7, 123.0) |
80.6 (57.0, 113.9) |
0.27 |
| P-valuee |
0.78 |
0.54 |
0.40 |
|
| 2:16αOH-E1 ratio (nmol/day) |
|
|
|
|
| Baseline |
11.3 (5.4, 23.6) |
10.5 (5.0, 21.9) |
10.8 (5.3, 22.4) |
0.98 |
| 8 weeks |
11.9 (5.7, 25.2) |
10.0 (4.7, 21.3) |
10.4 (5.0, 21.7) |
0.90 |
| P-valuee | 0.90 | 0.12 | 0.72 | |
HF: high fat diet; LF: low fat diet; LFn3: low fat + omega-3 fatty acids diet; E1: estrone;
2:16αOH-E1 ratio: 2-hydroxy estrone:16α-hydroxy estrone ratio.
aAll values are geometric means (95% confidence interval).
bOne subject was missing urines for HF diet, thus n = 15 for HF.
cOne subject was missing urines for LF diet, thus n = 15 for LF.
dP-value for effect of treatment across the three diets; values with differing symbols (§,†) as a superscript are significantly different.
eP-value for paired t-test comparing baseline and 8 weeks means within each diet.
**8 weeks mean is significantly different from baseline mean.
f8 weeks means were adjusted for baseline 2OH-E1.
Discussion
Estrone excretion was significantly greater with LF and LFn3 compared to HF, although there was little overall change in urinary hormone metabolites. The sum of all estrogens and metabolites assayed in this study (Total Estrogens) did not differ among diets at 8 weeks. We previously reported the effects of the test diets on plasma sex hormones [14]. In blood, E2 concentration increased significantly with HF (P = 0.03) and decreased slightly, but non-significantly with LF (P = 0.10) [14]. Therefore, we anticipated changes in sex hormone metabolism measured in urine. We saw no change in urinary sex hormone metabolite excretion even though changes in the parent hormones E1 and E2 were observed. Limiting factors include the high variability (wide confidence intervals) of urinary hormones and our small sample size.
We anticipated that LF and LFn3 would reduce excretion of estrogens and metabolites in accordance with the hypothesis that a low fat diet alters profiles of sex hormones in a direction of reduced breast cancer risk. Increased excretion of urinary estrogens (defined as E1 + E2 + E3 or E1 + E2) was associated with increased risk of breast cancer in another study of postmenopausal women [1]. Decreased excretion of estrogens was observed in postmenopausal women from Asian nations with relatively low breast cancer incidence and concomitantly low intake of dietary fat [17-19].
In addition to total dietary fat, n-3 may play a role in breast cancer prevention. Greenland Eskimos, with high n-3 intake [20], have historically had a low incidence of breast cancer [21,22]. However, this risk has increased as Westernized and nontraditional foods have become more prevalent in their diets [23]. Few studies have investigated the relationship of n-3 and urinary sex hormone metabolism in humans. Urinary 16αOH-E1 was reduced in the n-3 fatty acid supplement arm in a pilot trial of high-risk women [24]. In a study by Wu et al. [25] postmenopausal vegetarian women consuming 2.14 g/day of n-3 docosahexaenoic acid had no significant change in urinary 2:16αOH-E1 ratio following intervention. In our study, 2:16αOH-E1 ratio was not altered following 8 weeks of dietary intervention.
Conclusion
In conclusion, urinary sex hormone metabolism was modestly altered in healthy postmenopausal women by LF alone or with additional n-3.
Abbreviations
2OH-E1: 2-hydroxy estrone; 2OH-E2: 2-hydroxy estradiol; 2-ME1: 2-methoxy-estrone; 2-ME2: 2-methoxy estradiol; 2:16αOH-E1 ratio: 2-hydroxy estrone:16α-hydroxy estrone ratio; 4OH-E1: 4-hyrdroxy estrone; 4OH-E2: 4-hydroxy estradiol; 4-ME1: 4-methoxy estrone; 4-ME2: 4-methoxy estradiol; 16αOH-E1: 16-alpha-hydroxy estrone; E1: Estrone; E2: Estradiol; E3: Estriol; HF: High fat diet; LF: Low fat diet; LFn3: Low fat + omega-3 fatty acids diet; n3: Omega-3; n6: Omega 6; ALA: α-linolenic acid; EPA: Eicosapentaenoic acid; DHA: Docosahexaenoic acid; LA: Linolenic acid; ARA: Arachidonic acid.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
The authors’ responsibilities were as follows - SKR and MSK designed the research; SKR, LRY and JBR conducted the research; WT, LRY and SKR analyzed the data; LRY, SKR and MSK wrote the manuscript; all authors had responsibility for final content. All authors read and approved the final manuscript.
Contributor Information
Lindsay R Young, Email: lryoung@umn.edu.
Susan K Raatz, Email: susan.raatz@ars.usda.gov.
William Thomas, Email: thoma003@umn.edu.
J Bruce Redmon, Email: redmo001@umn.edu.
Mindy S Kurzer, Email: mkurzer@umn.edu.
Acknowledgements
Funding for this work was provided by grants from the Department of Defense (W81XWH-04-1-0448 and W81XWH-06-1-0778) and the National Center for Research Resources, National Institutes of Health (MO1-RR00400). This study was carried out at the General Clinical Research Center, University of Minnesota Medical School, Minneapolis, MN, USA.
References
- Thomas HV, Reeves GK, Key TJ. Endogenous estrogen and postmenopausal breast cancer: a quantitative review. Cancer Causes Control. 1997;8:922–928. doi: 10.1023/A:1018476631561. [DOI] [PubMed] [Google Scholar]
- Heber D, Ashley JM, Leaf DA, Barnard RJ. Reduction of serum estradiol in postmenopausal women given free access to low-fat high-carbohydrate diet. Nutrition. 1991;7:137–9. discussion 139–40. [PubMed] [Google Scholar]
- Prentice R, Thompson D, Clifford C, Gorbach S, Goldin B, Byar D. Dietary fat reduction and plasma estradiol concentration in healthy postmenopausal women. The Women's Health Trial Study Group. J Natl Cancer Inst. 1990;82:129–134. doi: 10.1093/jnci/82.2.129. [DOI] [PubMed] [Google Scholar]
- Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK, Margolis KL, Limacher MC, Manson JE, Parker LM, Paskett E, Phillips L, Robbins J, Rossouw JE, Sarto GE, Shikany JM, Stefanick ML, Thomson CA, Van Horn L, Vitolins MZ, Wactawski-Wende J, Wallace RB, Wassertheil-Smoller S, Whitlock E, Yano K, Adams-Campbell L, Anderson GL, Assaf AR, Beresford SA, Black HR, Brunner RL, Brzyski RG, Ford L, Gass M, Hays J, Heber D, Heiss G, Hendrix SL, Hsia J, Hubbell FA, Jackson RD, Johnson KC, Kotchen JM, LaCroix AZ, Lane DS, Langer RD, Lasser NL, Henderson MM. Low-fat dietary pattern and risk of invasive breast cancer: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:629–642. doi: 10.1001/jama.295.6.629. [DOI] [PubMed] [Google Scholar]
- Noble LS, Takayama K, Zeitoun KM, Putman JM, Johns DA, Hinshelwood MM, Agarwal VR, Zhao Y, Carr BR, Bulun SE. Prostaglandin E2 stimulates aromatase expression in endometriosis-derived stromal cells. J Clin Endocrinol Metab. 1997;82:600–606. doi: 10.1210/jc.82.2.600. [DOI] [PubMed] [Google Scholar]
- Zhu BT, Conney AH. Functional role of estrogen metabolism in target cells: review and perspectives. Carcinogenesis. 1998;19:1–27. doi: 10.1093/carcin/19.1.1. [DOI] [PubMed] [Google Scholar]
- Telang NT, Suto A, Wong GY, Osborne MP, Bradlow HL. Induction by estrogen metabolite 16 alpha-hydroxyestrone of genotoxic damage and aberrant proliferation in mouse mammary epithelial cells. J Natl Cancer Inst. 1992;84:634–638. doi: 10.1093/jnci/84.8.634. [DOI] [PubMed] [Google Scholar]
- Schneider J, Kinne D, Fracchia A, Pierce V, Anderson KE, Bradlow HL, Fishman J. Abnormal oxidative metabolism of estradiol in women with breast cancer. Proc Natl Acad Sci USA. 1982;79:3047–3051. doi: 10.1073/pnas.79.9.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishman J, Schneider J, Hershcope RJ, Bradlow HL. Increased estrogen-16 alpha-hydroxylase activity in women with breast and endometrial cancer. J Steroid Biochem. 1984;20:1077–1081. doi: 10.1016/0022-4731(84)90021-9. [DOI] [PubMed] [Google Scholar]
- Kabat GC, Chang CJ, Sparano JA, Sepkovie DW, Hu XP, Khalil A, Rosenblatt R, Bradlow HL. Urinary estrogen metabolites and breast cancer: a case–control study. Cancer Epidemiol Biomarkers Prev. 1997;6:505–509. [PubMed] [Google Scholar]
- Ho GH, Luo XW, Ji CY, Foo SC, Ng EH. Urinary 2/16 alpha-hydroxyestrone ratio: correlation with serum insulin-like growth factor binding protein-3 and a potential biomarker of breast cancer risk. Ann Acad Med Singapore. 1998;27:294–299. [PubMed] [Google Scholar]
- Muti P, Bradlow HL, Micheli A, Krogh V, Freudenheim JL, Schunemann HJ, Stanulla M, Yang J, Sepkovic DW, Trevisan M, Berrino F. Estrogen metabolism and risk of breast cancer: a prospective study of the 2:16alpha-hydroxyestrone ratio in premenopausal and postmenopausal women. Epidemiology. 2000;11:635–640. doi: 10.1097/00001648-200011000-00004. [DOI] [PubMed] [Google Scholar]
- Cauley JA, Zmuda JM, Danielson ME, Ljung BM, Bauer DC, Cummings SR, Kuller LH. Estrogen metabolites and the risk of breast cancer in older women. Epidemiology. 2003;14:740–744. doi: 10.1097/01.ede.0000091607.77374.74. [DOI] [PubMed] [Google Scholar]
- Young LR, Kurzer MS, Thomas W, Redmon JB, Raatz SK. Effect of dietary fat and omega-3 fatty acids on urinary eicosanoids and sex hormone concentrations in postmenopausal women: a randomized controlled feeding trial. Nutr Cancer. 2011;63:930–939. doi: 10.1080/01635581.2011.589957. [DOI] [PubMed] [Google Scholar]
- Nelson RE, Grebe SK, OKane DJ, Singh RJ. Liquid chromatography-tandem mass spectrometry assay for simultaneous measurement of estradiol and estrone in human plasma. Clin Chem. 2004;50:373–384. doi: 10.1373/clinchem.2003.025478. [DOI] [PubMed] [Google Scholar]
- Xu X, Veenstra TD, Fox SD, Roman JM, Issaq HJ, Falk R, Saavedra JE, Keefer LK, Ziegler RG. Measuring fifteen endogenous estrogens simultaneously in human urine by high-performance liquid chromatography-mass spectrometry. Anal Chem. 2005;77:6646–6654. doi: 10.1021/ac050697c. [DOI] [PubMed] [Google Scholar]
- Goldin BR, Adlercreutz H, Gorbach SL, Woods MN, Dwyer JT, Conlon T, Bohn E, Gershoff SN. The relationship between estrogen levels and diets of Caucasian American and Oriental immigrant women. Am J Clin Nutr. 1986;44:945–953. doi: 10.1093/ajcn/44.6.945. [DOI] [PubMed] [Google Scholar]
- Adlercreutz H, Gorbach SL, Goldin BR, Woods MN, Dwyer JT, Hamalainen E. Estrogen metabolism and excretion in Oriental and Caucasian women. J Natl Cancer Inst. 1994;86:1076–1082. doi: 10.1093/jnci/86.14.1076. [DOI] [PubMed] [Google Scholar]
- Ursin G, Wilson M, Henderson BE, Kolonel LN, Monroe K, Lee HP, Seow A, Yu MC, Stanczyk FZ, Gentzschein E. Do urinary estrogen metabolites reflect the differences in breast cancer risk between Singapore Chinese and United States African-American and white women? Cancer Res. 2001;61:3326–3329. [PubMed] [Google Scholar]
- Bang HO, Dyerberg J, Sinclair HM. The composition of the Eskimo food in north western Greenland. Am J Clin Nutr. 1980;33:2657–2661. doi: 10.1093/ajcn/33.12.2657. [DOI] [PubMed] [Google Scholar]
- Schaefer O, Hildes JA, Medd LM, Cameron DG. The changing pattern of neoplastic disease in Canadian Eskimos. Can Med Assoc J. 1975;112:1399–1404. [PMC free article] [PubMed] [Google Scholar]
- Nielsen NH, Hansen JP. Breast cancer in Greenland–selected epidemiological, clinical, and histological features. J Cancer Res Clin Oncol. 1980;98:287–299. doi: 10.1007/BF00410791. [DOI] [PubMed] [Google Scholar]
- Deutch B, Dyerberg J, Pedersen HS, Aschlund E, Hansen JC. Traditional and modern Greenlandic food - dietary composition, nutrients and contaminants. Sci Total Environ. 2007;384:106–119. doi: 10.1016/j.scitotenv.2007.05.042. [DOI] [PubMed] [Google Scholar]
- Osborne MP, Karmali RA, Hershcopf RJ, Bradlow HL, Kourides IA, Williams WR, Rosen PP, Fishman J. Omega-3 fatty acids - Modulation of estrogen metabolism and potential for breast-cancer prevention. Cancer Invest. 1988;6:629-630–631. [Google Scholar]
- Wu WH, Lu SC, Wang TF, Jou HJ, Wang TA. Effects of docosahexaenoic acid supplementation on blood lipids, estrogen metabolism, and in vivo oxidative stress in postmenopausal vegetarian women. Eur J Clin Nutr. 2006;60:386–392. doi: 10.1038/sj.ejcn.1602328. [DOI] [PubMed] [Google Scholar]