Abstract
Objectives
To identify a standard physical performance test that can predict 3-year incident mobility disability (IMD) independent of demographics
Design
Longitudinal cohort study
Setting
Population-based older cohort
Participants
Community-living middle-aged and older persons (age: 50–85 years) without baseline mobility disability (n=622).
Measurements
Mobility disability was ascertained at baseline and at 3-year follow-up using an established self-report method: self-reported inability to walk a quarter mile without resting or inability to walk up a flight of stairs unsupported. Physical performance tests included self-selected usual gait speed, time required to complete 5 times sit-to-stand (5tSTS) and 400 m brisk walking. Demographic variables age, sex, height and weight were recorded.
Results
Overall, 13.5% participants reported 3-year IMD. Usual gait speed <1.2 m/s, requiring >13.6 seconds to complete 5tSTS and completing 400 m at <1.19m/s walking speed were highly predictive of future mobility disability independent of demographics.
Conclusions
Inability to complete 5tSTS in < 13.7 seconds can be a clinically convenient guideline for monitoring and for further assessment of middle-aged and older persons, in order to prevent or delay future mobility disability.
Keywords: mobility, disability, aging
The performance on standard physical tests has been used to predict several adverse health outcomes, including frank disability, in older persons. However, whether the initial process of disablement, which is mobility disability1, can be predicted using known standard physical tests is not clear. The performance on Short Physical Performance Battery can predict 4-year incident mobility disability (IMD)2. However, the authors did not adjust their analysis for participants’ height or weight. These demographic characteristics can significantly impact physical performance measures such as walking speed, a component of Short Physical Performance Battery. The 400 m brisk walking test has also been shown to predict ~5-year IMD in older persons. However, only those between the narrow age range of 70–79 years were included in this study limiting the generalizability3. Furthermore, no comparative studies could be found that identified a test that is the best predictor of IMD. Since mobility disability denotes the earliest stage of disablement1, detecting mobility disability during an early or preclinical stage may provide an important opportunity for implementing preventative measures. Therefore, the purpose of this study was to test the ability of 3 physical performance tests to predict 3-year IMD in middle aged and older adults.
METHODS
Participants
Six hundred seventy-seven In CHIANTI study4 participants aged 50–85 years and who did not report mobility disability were initially included. Follow-up data were collected after 3 years. The study protocol was approved by the ethical committee of the Italian National Institute of Research and Care of Aging and complies with the Declaration of Helsinki. All participants signed an informed consent.
Outcome measures
Mobility disability assessed traditionally as self-reported inability to walk a quarter mile without resting or inability to walk up a flight of stairs unsupported5 was ascertained at baseline and at the 3-year follow-up. Demographic variables included age, sex, height and weight.
Standard physical measures
Usual gait speed
Participants were asked to walk at a self-selected normal pace. The time to complete the 7 m path was recorded in seconds and was converted to gait speed (m/s). The gait speed performance was categorized into 4 groups using the known cut-off points (0 = < 0.80 m/s, 1 = 0.80 – 0.99 m/s, 2 = 1.00 – 1.19 m/s and ≥ = 1.2 m/s)6–8. The gait speed < 0.80 m/s is an indicator of prevalent mobility limitations, <1.0 m/s is associated with adverse health outcomes in well-functioning older adults and <1.2 m/s is associated with difficulty in crossing streets in community.
5 times sit-to-stand test (5tSTS)
Participants were asked to stand up from a sitting position in a standard chair (height 46 cm) 5 times consecutively as quickly as possible without using hand support. The time to complete the test was recorded in seconds. The performance was categorized using quartile cut-off points derived from a large series of longitudinal studies that were conducted using small town population and have been used by aging studies as norms9: 0= inability to complete the test, 1= test completed in >16.6 s, 2= 13.7–16.6 s to complete, 3= 11.2–13.6 s to complete and 4= test completed in <11.2 sec.
400 m brisk walking test
Participants were asked to walk briskly to complete 20 laps on a 20 m path10. The performance was dichotomized as 0= unable to complete the test and 1= completed the test. Further, the average walking speed of those who completed the test was categorized into study quartiles as no known cut-off points are available in literature. Thus, the final 5 categories included: 0= unable to complete, 1= < 1.19 m/s, 2= 1.19–1.32m/s, 3= 1.33–1.46 m/s and 4= >1.46 m/s.
Covariates
Age and sex were recorded from birth records. The height was recorded in centimetres and weight was recorded in kilograms.
Descriptive variable
Presence of comorbidities (listed in the results section) was used to describe the population and was recorded from participants’ self-report and medical records.
Statistical analysis
Binary logistic regression analyses were performed to examine the likelihood of developing mobility disability associated with the aforementioned performance categories of each of the 3 physical tests, independent of demographics. Data were analyzed using IBM-SPSS version19. A p < 0.05 was considered statistically significant.
RESULTS
Six hundred twenty-two participants attended the follow-up and were included in the final analysis. Eighty-two participants were between the ages of 50–64 years, 320 participants were between 65–74 years and 220 participants were 75–85 years old. A total of 3.5% had a history of stroke, 2.9% had myocardial infarction, 4.5% reported angina pectoris, 47.7% had hypertension, 11.4% had diabetes and 2.5% had peripheral arterial disease, 1.7% reported hip replacement, 21.5% had either hip or knee pain requiring medication.
Eighty-four participants reported mobility disability at the 3-year follow-up (total 13.5%, men 8.7%, women 17.6%).
Poor performance on the physical tests at baseline was strongly associated with 3-year IMD, independent of demographic variables. The odds of developing IMD increased consistently as the baseline gait speed decreased below 1.2m/s. Participants who could not complete 5tSTS were five times as likely, whereas, those who required >13.7 s to complete this test were almost four times as likely to report incident mobility disability compared to those who completed 5tSTS in <11.2 s. Compared to the highest quartile of the average walking speed during 400 m brisk walking test (>1.47 m/s) participants who could not complete the test as well as those who completed but with the average walking speed <1.19 m/s were almost 20 times as likely to report incident mobility disability (Table 1).
Table 1.
The odds for 3-year incident mobility disability associated with performance on standard physical performance tests.
| variable | B(SE) | p | OR(CI) |
|---|---|---|---|
| 1. UG speed | |||
| UW speed | <0.001 | ||
| < 0.80 m/s | 3.217(0.724) | <0.001 | 24.957(6.039–103.135) |
| 0.80 –0.99 m/s | 1.970(0.408) | <0.001 | 7.171(3.222–15.958) |
| 1.0–1.19 m/s | 1.260(0.316) | <0.001 | 3.526(1.898–6.550) |
| ≥ 1.2 m/s | Comparison group | ||
| 2. 5tSTS | |||
| 5tSTS | <0.001 | ||
| not completed | 1.591(0.697) | 0.022 | 4.907(1.252–19.228) |
| >16.6 s | 1.380(0.391) | <0.001 | 3.976(1.849–8.553) |
| 13.7 – 16.6 s | 1.474(0.342) | <0.001 | 4.376(2.234–8.531) |
| 11.2 – 13.6 s | −0.667(0.424) | 0.116 | 0.513(0.224–1.178) |
| < 11.2 s | Comparison group | ||
| 3. 400 BW completed | |||
| 400 BW not completed | 1.068 (0.207) | <0.001 | 2.909 (1.711–4.945) |
| 400 BW completed | Comparison group | ||
| 4. 400 BW speed | |||
| 400 BW speed | <0.001 | ||
| not completed | 3.129(1.051) | 0.003 | 22.859(2.915–179.255) |
| < 1.19 m/s | 3.142(1.056) | 0.003 | 23.145(2.924–183–198) |
| 1.19 – 1.32 m/s | 1.862(1.074) | 0.083 | 6.434(0.784–52.767) |
| 1.33 – 1.46 m/s | 1.307(1.114) | 0.241 | 3.696(0.416–32.806) |
| > 1.46 m/s | Comparison group | ||
UG speed: usual gait speed, 5tSTS: 5 times sit to stand, 400 BW completed: 400 m brisk walking completed, 400 BW speed: average speed of 400 m brisk walking. The analyses were adjusted for age, sex, weight and height.
DISCUSSION
Using the population-based data this longitudinal study demonstrated that the performance on all the three physical tests was able to predict IMD. The gradient effect of decline in usual walking speed on the likelihood of developing mobility disability suggests that the possibility of IMD consistently increases with decrease in usual gait speed. However, the time to complete 5tSTS and average walking speed for 400 m brisk walking test provided a more clear demarcation point (Figure 1). The confidence intervals of the odds ratios associated with average walking speed < 1.19 i.e. > 5 minutes 36 seconds to complete 400 m and inability to complete the 400 m brisk walking test were large, demonstrating significant variability. Further, compared to 400 m brisk walking test, considering time and space requirements, 5tSTS is a more convenient test to administer in clinical environments. The results of the 5tSTS suggested that those requiring >13.6 s to complete this task were at least 4 times as likely to report incident mobility disability. Additionally, these results did not change significantly when further adjusted for number of comorbid conditions. For the first time the results indicate that this cut-off point can provide a simpler clinical guideline to determine which middle-aged or older persons should be monitored and assessed further for possible modifiable factors that may contribute to mobility disability in near future.
Figure 1.
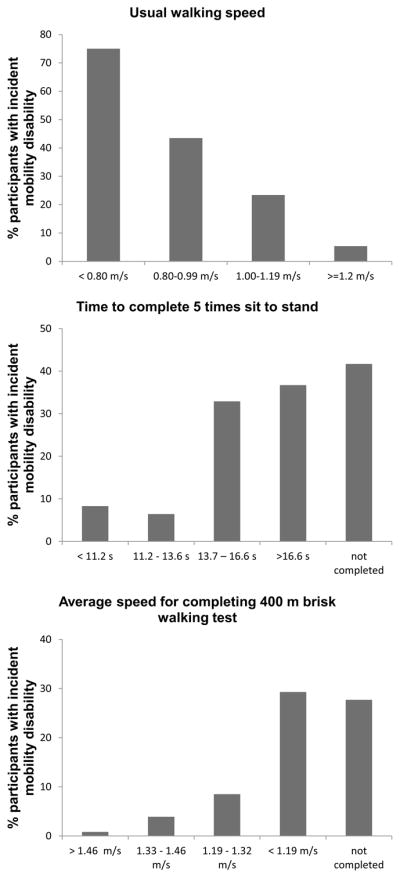
The % distribution of participants with the 3-year incident mobility disability according to the performance on usual walking speed, 5 times sit to stand and average speed for completing 400 m brisk walking test categories.
Study limitations
The study population was primarily Caucasian adults living in small towns which may not represent a racially mixed older cohort living in larger cities. Further, the assessment of mobility disability was completed using a dichotomized self-report rather than using a continuous measure. However, the method used is the most commonly used process of ascertaining mobility disability.
CONCLUSIONS
In conclusion, independent of the demographics, inability to complete 5tSTS in < 13.7 seconds can be a clinically convenient guideline for monitoring and further assessment of middle-aged and older persons, in order to prevent or delay mobility disability in near future.
Acknowledgments
The In CHIANTI study was supported as a “targeted project” (ICS 110.1\RS97.71) by the Italian Ministry of Health and in part, by National Institute on Aging Contracts N01-AG-916413, N01-AG-821336, N01-AG-5-0002, and NIA Grant R01 AG 027012 and the Intramural Research Program, National Institute on Aging, NIH. We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
Abbreviations
- IMD
Incident mobility disability
- ADL
Activities of daily living
- IADL
Instrumental activities of daily living
- 5tSTS
5 times sit to stand
Footnotes
Potential financial conflicts of interest: none
Reprints: Reprints will not be available from the authors
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci. 2000;55(1):M43–52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295(17):2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 4.Ferrucci L, Bandinelli S, Benvenuti E, Di Iorio A, Macchi C, Harris TB, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the In CHIANTI study. J Am Geriatr Soc. 2000;48:1618–25. doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]
- 5.Gill TM, Allore HG, Hardy SE, Guo Z, et al. The dynamic nature of mobility disability in older persons. J Am Geriatr Soc. 2006;54(2):248–54. doi: 10.1111/j.1532-5415.2005.00586.x. [DOI] [PubMed] [Google Scholar]
- 6.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675–80. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 7.Shumway-Cook A, Patla AE, Stewart A, Ferrucci L, Ciol MA, Guralnik JM. Environmental demands associated with community mobility in older adults with and without mobility disabilities. Phys Ther. 2002;82(7):670–81. [PubMed] [Google Scholar]
- 8.Langlois JA, Keyl PM, Guralnik JM, Foley DJ, Marottoli RA, Wallace RB. Characteristics of older pedestrians who have difficulty crossing the street. Am J Public Health. 1997;87(3):393–7. doi: 10.2105/ajph.87.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994 Mar;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 10.McDermott MM, Guralnik JM, Albay M, Bandinelli S, Miniati B, Ferrucci L. Impairments of muscles and nerves associated with peripheral arterial disease and their relationship with lower extremity functioning: the In CHIANTI Study. J Am Geriatr Soc. doi: 10.1111/j.1532-5415.2004.52113.x. [DOI] [PubMed] [Google Scholar]


