Abstract
Introduction
Reducing readmissions has become a focus in efforts by Medicare to improve healthcare quality and reduce costs. This study aimed to determine whether causes for readmission differed between obese and non-obese patients, possibly allowing for targeted interventions.
Methods
A matched case-control study of Medicare patients admitted between 2002–2006 who were readmitted following hip or knee surgery, colectomy, or thoracotomy was performed. Patients were matched exactly for procedure, while also balancing on hospital, age and sex. Conditional logistic regression was used to study the odds of readmission for very obese cases (BMI > 35kg/m2) versus normal weight patients (BMI of 20–30kg/m2) after further controlling for race, transfer-in and emergency status, and comorbidities.
Results
Among 15,914 patient admissions we identified 1,380 readmitted patients and 2,760 controls. Risk of readmission was increased for obese vs. non-obese patients, before and after controlling for comorbidities (OR=1.35, P=0.003; OR=1.25, P=0.04). Reasons for readmission varied by procedure but were not different by BMI category.
Conclusions
Obese patients have an increased risk of readmission, yet reasons for readmission in obese patients appear similar to the non-obese, suggesting that improved post-discharge management for the obese cannot focus on a few specific causes of readmission, but must provide a broad range of interventions.
Keywords: readmissions, rehospitalization, obesity, surgery
Introduction
In an effort to improve quality of care and control healthcare costs, hospital readmissions have become the target of considerable discussion. The recently passed Patient Protection and Affordable Care Act gives the Centers for Medicare and Medicaid Services the authority to financially penalize hospitals for excessive readmissions, which will include surgical patients as early as 2015.1 The elderly accounted for 36% of healthcare expenditures in 2002 while making up only 13% of the United States population.2 As the population continues to age, the number of elderly patients undergoing surgery is also rising.3, 4 Surgical readmissions account for 22% of all readmissions.5
Obesity is a risk factor for surgical complications6–9 and as such, may affect rates of surgical readmission as well. Medicare and other administrative claims data do not collect body mass index (BMI) for patients, thus many of the large-scale studies examining predictors of readmission have not been able to include the effect of obesity.5, 10, 11 Studies that have included a measure of obesity have shown contradictory effects of obesity on readmission.12–14 The Obesity and Surgical Outcomes Study15, 16 database provides a unique dataset in which claims data are merged with chart abstracted data, allowing a detailed examination of readmissions and obesity in the elderly surgical patient.
In order to better understand why obese patients have elevated readmission rates and to prevent readmission in the obese, the aim of this study was to compare the causes of readmission for obese and non-obese elderly surgical patients.
We therefore sought to identify indications for readmission in a unique surgical cohort with a detailed evaluation of the impact of obesity on the likelihood for readmission. We hypothesized that obese patients would have an increased risk of readmission, even after controlling for other pre-operative patient comorbidities, and that the reasons for readmission would differ between obese and non-obese patients.
Methods
Study cohort and design
Approval for this study was obtained from the Institutional Review Board (IRB) of The Children’s Hospital of Philadelphia as well as hospital-specific IRBs when requested. This observational multi-institutional nested matched case-control study was conducted using the Obesity and Surgical Outcomes Study database. Details of the Obesity and Surgical Outcomes Study database data have been previously described. 9, 16 In brief, the dataset contains both administrative and chart-based information on Medicare patients undergoing surgical procedures at 47 hospitals located throughout Illinois, New York, and Texas. These three states were chosen to optimize population size, obtain varied geography, and minimize managed care enrollment of Medicare patients. The dataset combined Medicare claims data and supplemental data obtained from chart review, which was provided by the individual hospitals enrolled in the study. Supplemental chart-abstracted data included body mass index (BMI), admission vital signs and laboratory tests, and other perioperative information.
All patients between the ages of 65 and 80 who underwent one of four specific surgical procedures between 2002 and 2006 were eligible for inclusion in this study if they were continuously enrolled in fee-for-service Medicare in the three months prior to and one month following the index admission. The four specific surgical procedures were identified as follows: (1) hip replacement or revision excluding fracture (ICD-9-CM Principal Procedure codes 81.51-81.53); (2) knee replacement or revision (ICD-9-CM Principal Procedure 81.54, 81.55); (3) colectomy for cancer (ICD-9-CM Principal Procedure codes 45.7-45.79, 45.8) (ICD-9-CM Principal Diagnosis codes 153-153.9, 154-154.8, 230.3-6) and colectomy not for cancer (ICD-9- CM Principle Procedure 45.7-45.79, 45.8) and (ICD-9-CM Principal Diagnosis codes 562.1- 562.13); and (4) thoracotomy (ICD-9-CM Principal Procedure codes 32-32.9). Throughout the manuscript, these procedure groups are referred to as orthopedic (hip or knee replacement), colorectal (colectomy for cancer or colectomy not for cancer), and thoracic (thoracotomy). Patients without an available BMI after chart abstraction and patients with height (≤48 or ≥84 inches), weight (≤80 or ≥600 lbs), or BMI (>100 kg/m2) outside a plausible range were excluded.
Available information on patients included comorbidities and APACHE score as identified and/or calculated using the merged dataset. Patient comorbidities included in this study are a history of congestive heart failure, stroke, seizure, dementia, alcohol use, drug use, electrolyte abnormalities, history of a myocardial infarction, history of arrhythmia, unstable angina, angina, hypertension, valvular disease, chronic lung disease, asthma, hepatic abnormalities, renal dysfunction, renal failure, paraplegia, collagen vascular disease, coagulation abnormality, thrombocytopenia, congenital coagulation disorder, history of smoking, pulmonary fibrosis, Cushing’s disease, Graves disease, cancer, hypothyroidism, chronic peptic ulcer disease, acquired immune deficiency syndrome (AIDS), weight loss, sleep apnea, and diabetes.9 Diabetes was determined using chart review, and was characterized into no diabetes, diabetes without medications, and diabetes with medications. Race was defined as black, white, or other as determined by Medicare claims. Index hospitalizations were defined as being an emergency if the patient’s source of admission was the emergency room. Patients who had a prior hospitalization in which the discharge date was the same as or the day prior to the day of admission for the hospitalization during which the procedure was performed were identified as having been transferred-in. The patient and hospital characteristics used in the risk adjustment were assigned at the time of the index hospitalization. Patient obesity status in the index admission was classified as normal weight if the calculated BMI was as 20–30 kg/m2 and obese if the calculated BMI was >35 kg/m2 (exactly as in our previous work9, 16, 17).
Readmission was defined as hospitalization (for reason other than rehabilitation) in an acute care facility after discharge from the index admission. Hospitals classified by Medicare as short term general/specialty hospitals or critical access hospitals (excluding psychiatric or rehabilitation specific sections) were considered acute care facilities. Admission for rehabilitation was identified by a diagnosis-related group (DRG) of 462. Transfers (defined as admission on the same day as or day after discharge from index admission, in which the discharge status or admission source indicated transfer) were not considered readmissions. Patients without 30 days of follow-up were also excluded.
Matching methodology
OBSOS patients who survived to discharge from their index hospitalization, but were readmitted or died within 30 days of discharge (without readmission) were matched in a 1:2 ratio to patients who survived to discharge from index hospitalization and also survived 30 days without requiring readmission. Patients who died within 30 days of discharge without being readmitted were identified as cases, under the presumption was that readmission would have been indicated if they had presented for medical care prior to death. Patients were matched with (i) exact matching for procedure, (ii) near-exact matching and near-fine balance for hospital18, 19, and (iii) balancing the means of age and sex17. Near-exact matching and near-fine balance are two forms of flexible matching that approximate exact matching and fine balance when these are not feasible.17–20 As a result of near-exact matching, patients are matched within hospitals as often as possible, whereas as a result of near-fine balance each hospital is approximately equally represented in the case and matched control groups. These forms of matching on the hospital allow the cases and controls to be identified and matched in such a way that differences across hospitals are less likely to bias the matched analyses. In so doing, we were able to minimize practice variation across institutions between cases and controls. This allowed us to study patient characteristics with minimal noise from the hospital processes of care.
Statistical Analysis
Balance on age and sex for patients in the match were examined using the Wilcoxon rank-sum test and the Fisher exact test. Conditional logistic regression was used to test the hypothesis that severely obese patients have equal odds of readmission compared to normal weight patients. The effect of controlling for race, emergency status, and transfer status, both with and without controlling for patient comorbidities, was examined using conditional logistic regression to determine if obesity remained an independent risk factor for readmission. These analyses were repeated after excluding cases in which the patients died prior to readmission to determine the influence of that subset of patients.
The ICD9CM Principal Diagnosis code for the readmission hospitalization was determined for each patient who was readmitted. These were then grouped into similar clinical categories to determine the general reason for readmission (ie. infection, gastrointestinal complications, etc, Appendix B). The percent of readmissions due to each general reason were compared by BMI category for each procedure group. The distribution of the indications for readmission was compared between the obese and the non-obese using the Fisher exact test.
Results
Hospital Characteristics
The mean hospital size for hospitals included in this study was 423 beds (SD 285), with a mean nurse to bed ratio of 1.64 (0.44). Forty seven percent of hospitals were non-teaching (resident to bed ratio = 0) while 6% were “very major” teaching hospitals (resident to bed ratio >0.6, Table 1).
Table 1.
Study Hospital Characteristics
| Number of Hospitals | 47 |
|---|---|
| Size (Beds) Mean (sd) | 423 (285) |
| Size Distribution | |
| 0–200 (%) | 15% |
| 201–400 (%) | 40% |
| 401–600 (%) | 28% |
| 601–800 (%) | 11% |
| >800 (%) | 6% |
| Nurse to bed ratio * Mean (sd) | 1.64 (0.44) |
| Teaching Intensity based on Resident to Bed Ratio (%) | |
| Non-Teaching (RB ratio = 0) | 47% |
| Very Minor (0 < RB ≤ 0.05) | 15% |
| Minor (0.05 <RB≤ 0.25) | 19% |
| Major (0.25 <RB≤ 0.6) | 13% |
| Very Major (0.6 < RB ≤1.1) | 6% |
Full time equivalent registered nurses/number of beds
Characteristics of the study population
Of the 18,517 patients identified who met OBSOS study criteria and underwent chart abstraction, 2,481 (13%) were excluded for missing BMI, 65 for implausible height, weight, or BMI, and 57 for other significant data inconsistencies. From the remaining OBSOS study population of 15,914 patients, we identified 15,666 patients who survived to discharge from their index admission and had a full 30 days of follow-up. Fifteen percent of patients in this dataset had a BMI ≥ 35 kg/m2. There was an overall 8.9% rate of readmission or death: 13.9% in patients who underwent a colectomy, 6.0% in patients who underwent hip or knee procedure, and 12.8% in patients who underwent a thoracotomy. For the subset of patients with a BMI ≥ 35 kg/m2 8.7% of them were readmitted or died without readmission in the 30 days after discharge from index hospitalization.
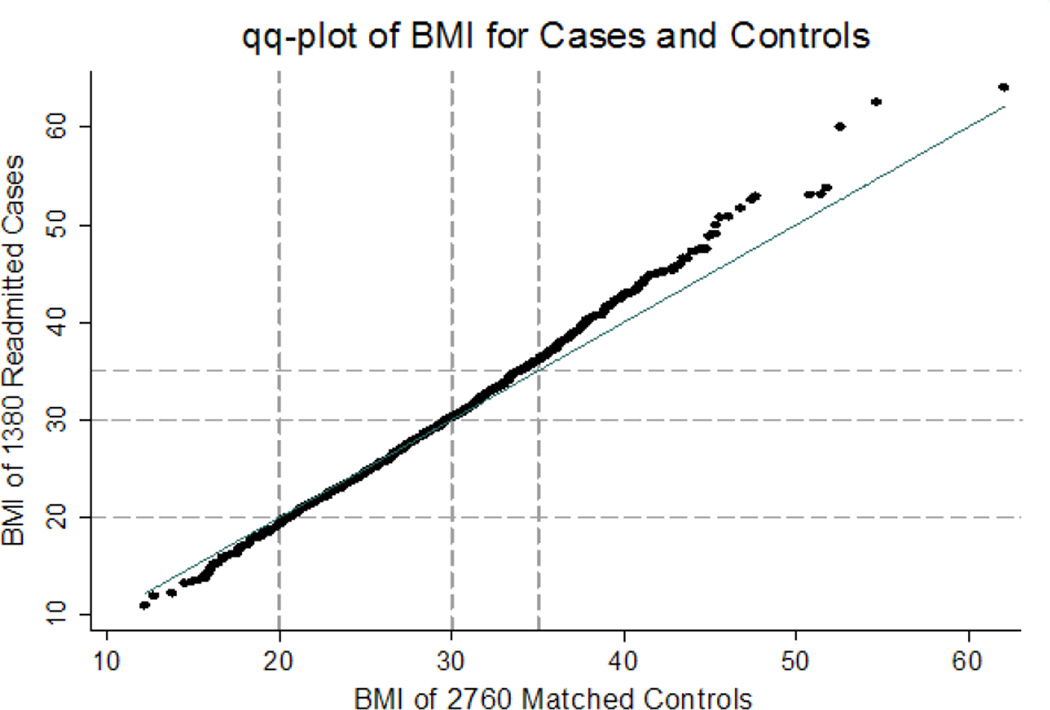
From the 15,666 patients, we identified 1,380 patients who were readmitted or died within 30 days after discharge from index admission. Fifty-nine of the 1,380 patients died within 30 days after discharge without being readmitted. The 1,380 patients were matched to 2,760 patients who were discharged alive and did not die and did not require readmission within 30 days. The matching algorithm successfully balanced age, sex, procedures and hospital between patients who were readmitted or died and those who did not die and did not get readmitted (see Table 2). Of the patients who were readmitted or died, 15% were obese while only 12% of the non-readmitted controls were obese. Patients with a BMI greater than 35 kg/m2 were overrepresented among cases of readmission as compared to controls, as seen in the quantile-quantile plot (Figure 1).
Table 2.
PatientCharacteristics
| Patient Characteristics | Cases (readmitted or died) N=1380 |
Controls N=2760 |
P-value |
|---|---|---|---|
| Age (years) mean | 73.25 | 73.25 | 0.94* |
| Sex | 0.97† | ||
| Female | 51% | 51% | |
| Male | 49% | 49% | |
| BMI category | |||
| BMI<20 | 6% | 5% | 0.01† |
| 20≤BMI <30 | 59% | 63% | |
| 30≤BMI<35 | 19% | 20% | |
| BMI≥35 | 15% | 12% | |
| Race | 0.17† | ||
| White | 91% | 91% | |
| Black | 6% | 5% | |
| Other | 3% | 3% | |
| Transfer Status | 0.01† | ||
| Nottransferred | 99% | 99% | |
| Transferred | 1% | 1% | |
| Emergent Status | <0.0001† | ||
| Elective | 86% | 91% | |
| Emergent | 14% | 9% | |
| APACHE Score | |||
| Mean (standard deviation) | 26.8 (8.6) | 25.4 (7.7) | <0.0001* |
| Colectomy with cancer (all) | 24% | 24% | -- |
| Left Colectomy | 7% | 7% | |
| Right Colectomy | 15% | 15% | |
| Total/Other | 2% | 2% | |
| Colectomy with out cancer (all) | 11% | 11% | -- |
| Left | 9% | 9% | |
| Right | 1% | 1% | |
| Total/Other | 1% | 1% | |
| Hip with out fracture (all) | 19% | 19% | -- |
| Total hip replacement | 14% | 14% | |
| Partial hip replacement | 2% | 2% | |
| Revision of hip replacement | 3% | 3% | |
| Knee (all) | 24% | 24% | -- |
| Total knee replacement | 22% | 22% | |
| Revision of knee replacement | 2% | 2% | |
| Thoractomy (all) | 22% | 22% | -- |
| Lobectomy | 13% | 13% | |
| Pneumonectomy | 1% | 1% | |
| Wed geresection | 8% | 8% | |
| Other‡ | 0% | 0% |
P-values compare non-obese to obese,
Wilcoxon’s rank sum,
Fisher exact test,
two cases and one control underwent other thoracotomy. Patients were matched with (i) exact matching for procedure, (ii) near-exact matching and near-fine balance for hospital, and (iii) balancing the means of age and sex
Figure 1. Quantile-quantile plot of body mass index for cases and controls.
The solid line indicates x = y, and dashed lines indicate BMI = 20, BMI = 30 and BMI = 35. After ordering the cases and controls, adjacent pairs of controls were averaged to allow a one-to-one plot of cases versus controls. As can be seen, patients with a BMI greater than 35 kg/m2 were overrepresented among cases of readmission as compared to controls.
The overall mean time to readmission (or death) for cases was 11.3 days (SD 8.3 days). By procedure specialty, the overall mean time to readmission was: colorectal 9.6 days (1.6 days), hip or knee 12.6 days (8.7 days), and thoracotomy 11.6 days (8.4 days). Patients who were readmitted or died had a mean length of stay of 8.7 days (8.9) for their index admission while those who were discharged alive and survived 30 days without requiring readmission had a mean length of stay of 6.6 days (5.4). Overall, 11% of patients in the matched pair cohort underwent an emergent procedure: 23% of colectomies were emergent, 6% of thoracotomies, and 3% of orthopedic procedures. Patients were most commonly readmitted through the emergency department (64%), followed by physician referral (31%) and transfer from an acute care facility (2%). Readmission to the same hospital as the index procedure was most common (80% of readmissions), while 20% of readmitted patients were readmitted to a different facility.
Effect of obesity on readmission
Obese patients had a 36% increased risk of readmission before controlling for other factors (95% CI 1.12-1.66, P-value = 0.002, Table 3). After controlling for race, emergency status, and transfer status during the index admission, obese patients had 35% increased odds of 30-day readmission or death (95% CI 1.10-1.65, P-value = 0.003). After controlling for all other patient comorbidities, including the APACHE score upon the index admission, obese patients remained at 25% increased odds of readmission (95% CI 1.01-1.55, P-value = 0.04). After excluding the 59 patients who died prior to readmission and their controls, the findings were unchanged (Table 3).
Table 3.
The relationship between obesity and readmission controlling for differing covariates in conditional logistic models
| Variables controlled for in model or match |
Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Procedure | Yes | Yes | Yes |
| Age | Yes | Yes | Yes |
| Sex | Yes | Yes | Yes |
| Hospital | Yes | Yes | Yes |
| Race | -- | Yes | Yes |
| Emergency status | -- | Yes | Yes |
| Transfer status | -- | Yes | Yes |
| Comorbidities | -- | -- | Yes |
| Odds Ratio for readmission or death | |||
| Obese:Nonobese | 1.36 | 1.35 | 1.25 |
| 95% Confidence Interval | (1.12–1.66) | (1.10–1.65) | (1.01–1.55) |
| P-value | 0.002 | 0.003 | 0.04 |
| Odds Ratio for readmission (deaths before readmission excluded) | |||
| Obese:Nonobese | 1.35 | 1.34 | 1.23 |
| 95% Confidence Interval | (1.10–1.64) | (1.10–1.64) | (1.00–1.53) |
| P-value | 0.004 | 0.005 | 0.05 |
Causes of readmission and association with obesity
The most common cause of readmission differed substantially by procedure specialty (Table 4). For patients undergoing colectomy, the most common causes of readmission were gastrointestinal complications and infection. After thoracotomy, patients were readmitted most often for pulmonary and cardiac complications. Orthopedic patients were most likely to be readmitted for orthopedic complications, cardiac reasons, or infection. The reasons for readmission were not significantly different between the obese and non-obese patients.
Table 4.
Reasons for readmission by procedure type
| Normal Weight | Obese | ||||||
|---|---|---|---|---|---|---|---|
| BMI 20–30 | BMI ≥ 35 | ||||||
| N = 819 readmissions | N = 209 readmissions | ||||||
| COLECTOMY p = 0.67† | |||||||
| N = 322 | N = 49 | ||||||
| GI Complications (33%) | GI Complications (36%) | ||||||
| Infection (19%) | Infection (19%) | ||||||
| Cardiac (9%) | Electrolyte/renal abnormality (8%) | ||||||
| Pulmonary (7%) | Cardiac (6%) | ||||||
| Electrolye/renal abnormality (7%) | Pulmonary (3%) | ||||||
| Bleeding (4%) | Bleeding (3%) | ||||||
| Urinary (3%) | Neurologic (3%) | ||||||
| Vascular (3%) | Ortho (3%) | ||||||
| Neurologic (3%) | Pain (3%) | ||||||
| Pain (2%) | Urinary (0%) | ||||||
| Psychiatric (0%) | Vascular (0%) | ||||||
| Ortho (0%) | Psychiatric (0%) | ||||||
| Other (11%) | Other (17%) | ||||||
| THORACOTOMY p = 0.82† | |||||||
| N = 203 | N = 31 | ||||||
| Pulmonary (37%) | Pulmonary (44%) | ||||||
| Cardiac (13%) | Cardiac (22%) | ||||||
| GI complications (8%) | Infection (7%) | ||||||
| Infection (6%) | Neurologic (7%) | ||||||
| Bleeding (4%) | GI complications (4%) | ||||||
| Neurologic (3%) | Ortho (4%) | ||||||
| Electrolyte/renal abnormality (3%) | Bleeding (0%) | ||||||
| Pain (3%) | Electrolyte/renal abnormality (0%) | ||||||
| Psychiatric (2%) | Pain (0%) | ||||||
| Urinary (1%) | Psychiatric (0%) | ||||||
| Vascular (1%) | Urinary (0%) | ||||||
| Ortho (1%) | Vascular (0%) | ||||||
| Other (17%) | Other (11%) | ||||||
| ORTHOPEDIC PROCEDURE p = 0.91† | |||||||
| N = 294 | N=129 | ||||||
| Ortho (23%) | Ortho (27%) | ||||||
| Cardiac (16%) | Infection (16%) | ||||||
| Infection (14%) | Cardiac (12%) | ||||||
| Bleeding (9%) | GI complications (12%) | ||||||
| GI complications (7%) | Bleeding (10%) | ||||||
| Neurologic (5%) | Neurologic (4%) | ||||||
| Vascular (5%) | Pulmonary (4%) | ||||||
| Pulmonary (3%) | Vascular (3%) | ||||||
| Pain (3%) | Pain (3%) | ||||||
| Urinary (2%) | Electrolyte/renal abnormalities (2%) | ||||||
| Electrolyte/renal abnormalities (2%) | Urinary (1%) | ||||||
| Psychiatric (1%) | Psychiatric (0%) | ||||||
| Other (10%) | Other (9%) | ||||||
Fisher exact test to compare the distribution of reasons for readmission between the obese and normal weight patients. See online appendix for ICD-9 principal diagnosis codes associated with each reason for readmission.
Discussion
We report that obesity increases the risk of 30-day readmission or death following surgical procedures from a variety of surgical specialties. After controlling for age, sex, procedure, hospital, emergency status, transfer status, and patient characteristics including APACHE score and comorbidities, the risk of readmission remains elevated in obese patients when compared to the non-obese. We also found that the most common causes of readmission differ by surgical procedure, indicating that readmissions after surgical procedures are likely related to the procedures rather than acute exacerbations of the patients’ chronic conditions. Furthermore, the most common indications for readmission did not differ significantly by obesity status but did differ by procedure specialty. Therefore successful speciality-specific interventions would likely result in reduced readmission rates regardless of obesity status.
Previous studies have reported that rehospitalizations in elderly surgical patients are frequently related to the initial indication for the surgical procedure.21 And, more recently, infectious reasons, such as surgical site infections, have been found to be a leading cause of readmission in vascular surgical patients.22 One of the largest studies to date by Jencks et. al. emphasized the frequent role of heart failure and pneumonia (suggesting need for closer medical outpatient follow-up) in the need for readmission in the post-operative period5. However, when broken down by procedure type, variation in reasons for readmissions by procedure type, similar to our findings, were seen.5 By examining patterns of readmission in three distinct surgical populations in our study, we were able to extend previous findings to demonstrate that the indications for readmission were most commonly related to the surgical procedure.
Our results highlight the importance of accurate risk stratification for complications, including readmissions. The presentation of complications often occurs in the outpatient setting in current medical care paradigms,23 and we suggest that the new interest in surgical readmissions likely represents a persistent interest in post-operative occurrences. Occurrences that previously would have happened during the index admission now occur in the outpatient setting, and when severe enough or impossible to evaluate in a timely fashion in the outpatient setting, mandate re-admission for timely management. It appears that obesity, a well-described risk factor for post-operative infectious complications,6–8 is also an independent risk factor for readmission. Using the unique characteristics of the OBSOS dataset, we were able to tease out the relationship between surgical readmissions and obesity independent of other obesity-related comorbidities in a multi-institutional study. Given our finding of increased risk of readmission in obese patients, we believe that future risk adjustment algorithms used to determine reimbursement for readmissions must incorporate BMI when possible.
We add to the growing body of literature that encourages the federal government to consider the potential unintended consequences of penalizing providers without consideration of the patient’s excessive risk due to obesity. Previous studies demonstrated an increased risk of SSI for obese patients and raised concerns about unfairly penalizing surgeons and having negative effects on obese patients’ access to surgery.24, 25 Readmission penalties are at risk for similar negative effects on providers and healthcare access for obese patients if not appropriately risk adjusted. Many studies that examine readmissions use Medicare or SEER databases because of the ability to accurately track rates of readmission to any hospital. However, studies that have used these national databases have not had the ability to study the effect of BMI due to the lack of this information in the dataset.5, 10, 11 Two studies using cardiac surgery databases, one for the state of New York14 and one in London,12 found that BMI or body surface area was associated with risk of readmission, while a smaller hospital-specific study found that BMI was not associated with readmission.13 Our study extends the results of these previous studies by using a large claims database supplemented with chart information including BMI and other physiologic data and by studying BMI as the primary predictor variable after controlling for other factors known to the surgeon and hospital at the time of preoperative evaluation.
Our findings must be placed in context. In examining a Medicare population we report only on the association between readmissions and obesity in the elderly. It is not clear that our findings will generalize to younger patients who might be more easily managed and evaluated in the outpatient setting or to other surgical procedures. However, obesity in the elderly population has increased over the last three decades, and between 2003–2006 almost one third of the population over the age of 60 was obese.26 Similarly, the elderly population is expected to increase to nearly 20% of the overall population by the year 2030.26 Therefore, given the increasing proportion of health care costs likely to be consumed by the elderly obese patient, it is important to understand the outcomes and risk factors for this population.
A limitation of our study is the focus on three main procedure groups: thoracotomy, colectomy (with and without cancer) and orthopedic procedures (hip and knee replacements, without fracture). These procedures were chosen for study because they are common in the Medicare population, but there may be variations in other types of procedures we were not able to identify. Additionally, the obese patients included in this study may be healthier than other Medicare patients in that they were able to find a surgeon who felt that the benefit of surgical intervention outweighed the risks of surgery. Thus, they may represent a less risky population of obese patients than the entire population of obese patients presenting for surgical evaluation, which would bias our results towards the null.
Obesity appears to be an independent risk factor for readmission after surgery for the elderly patient. The inability to include BMI in current risk-adjustment for readmission has the potential to unfairly penalize hospitals that treat a large number of obese patients, providing disincentives for providers to care for obese patients. As the body mass index is used routinely in the process of patient care, it is easily available and should be added to the list of elements abstracted for billing purposes to allow for reasonable risk adjustment in this challenging patient population. Further study is needed to determine how best to decrease the risk of readmission for obese patients as they seem to have similar reasons for readmission.
Supplementary Material
Acknowledgments
Sources of Financial Support:
This research was funded through grants from the National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK R01 DK 073671 and 3R01 DK 073671-0451) and the National Science Foundation Grant No. SES-0849370.
Abbreviations used
- BMI
body mass index
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- FFS
Fee-for-service
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflict of interest.
References
- 1.Foster D, Harkness G. Healthcare Reform: Pending Changes to Reimbursement for 30-day Readmissions. 2010 [Google Scholar]
- 2.Stanton M, MK R. The High Concentration of U.S. Health Care Expenditures. Agency for Healthcare Research and Quality: Research in Action Issue 19. 2006 AHRQ Pub. No. 06-0060. [Google Scholar]
- 3.Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg. 2007;205(6):729–734. doi: 10.1016/j.jamcollsurg.2007.06.307. [DOI] [PubMed] [Google Scholar]
- 4.Etzioni DA, Liu JH, O'Connell JB, et al. Elderly patients in surgical workloads: a population-based analysis. Am Surg. 2003;69(11):961–965. [PubMed] [Google Scholar]
- 5.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 6.Gendall KA, Raniga S, Kennedy R, Frizelle FA. The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum. 2007;50(12):2223–2237. doi: 10.1007/s10350-007-9051-0. [DOI] [PubMed] [Google Scholar]
- 7.Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20(7) Suppl 3:46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 8.Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg. 2009;250(1):166–172. doi: 10.1097/SLA.0b013e3181ad8935. [DOI] [PubMed] [Google Scholar]
- 9.Silber JH, Rosenbuam PR, Kelz RR, et al. Medical and Financial Risks Associated with Surgery in the Elderly Obese. Ann Surg. 2012 doi: 10.1097/SLA.0b013e31825375ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greenblatt DY, Weber SM, O'Connor ES, et al. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 251(4):659–669. doi: 10.1097/SLA.0b013e3181d3d27c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tuggle CT, Park LS, Roman S, et al. Rehospitalization among Elderly Patients with Thyroid Cancer after Thyroidectomy are Prevalent and Costly. Ann Surg Oncol. doi: 10.1245/s10434-010-1144-7. [DOI] [PubMed] [Google Scholar]
- 12.Rockx MA, Fox SA, Stitt LW, et al. Is obesity a predictor of mortality, morbidity and readmission after cardiac surgery? Can J Surg. 2004;47(1):34–38. [PMC free article] [PubMed] [Google Scholar]
- 13.Kariv Y, Wang W, Senagore AJ, et al. Multivariable analysis of factors associated with hospital readmission after intestinal surgery. Am J Surg. 2006;191(3):364–371. doi: 10.1016/j.amjsurg.2005.10.038. [DOI] [PubMed] [Google Scholar]
- 14.Hannan EL, Racz MJ, Walford G, et al. Predictors of readmission for complications of coronary artery bypass graft surgery. JAMA. 2003;290(6):773–780. doi: 10.1001/jama.290.6.773. [DOI] [PubMed] [Google Scholar]
- 15.Silber JH, Rosenbuam PR, Kelz RR, et al. Medical and Financial Risks Associated with Surgery in the Elderly Obese. Ann Surg in press. doi: 10.1097/SLA.0b013e31825375ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silber JH, Rosenbaum PR, Even-Shoshan O, et al. Estimating anesthesia time using the medicare claim: a validation study. Anesthesiology. 115(2):322–333. doi: 10.1097/ALN.0b013e31821d6c81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zubizarreta JR, Reinke CE, Kelz RR, et al. Matching for several sparse nominal variables in a case-control study of readmission following surgery. The American Statistician. 2012 doi: 10.1198/tas.2011.11072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenbuam PR, Ross RN, Silber JH. Minimum distance matched sampling with fine balance in an observational study of treatment for ovarian cancer. J Am Stat Assoc. 2007;102:75–83. [Google Scholar]
- 19.Yang D, Small DS, Silber JH, Rosenbaum PR. Optimal Matching with Minimal Deviation from Fine Balance in a Study of Obesity and Surgical Outcomes. Biometrics. doi: 10.1111/j.1541-0420.2011.01691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenbuam PR. Design of Observational Studies. New York: Springer; 2010. [Google Scholar]
- 21.Riley G, Lubitz J. Outcomes of surgery in the Medicare aged population: rehospitalization after surgery. Health Care Financ Rev. 1986;8(1):23–34. [PMC free article] [PubMed] [Google Scholar]
- 22.Jackson BM, Nathan DP, Doctor L, et al. Low rehospitalization rate for vascular surgery patients. J Vasc Surg. 54(3):767–772. doi: 10.1016/j.jvs.2011.03.255. [DOI] [PubMed] [Google Scholar]
- 23.Bilimoria KY, Cohen ME, Ingraham AM, et al. Effect of postdischarge morbidity and mortality on comparisons of hospital surgical quality. Ann Surg. 252(1):183–190. doi: 10.1097/SLA.0b013e3181e4846e. [DOI] [PubMed] [Google Scholar]
- 24.Wick EC, Hirose K, Shore AD, et al. Surgical site infections and cost in obese patients undergoing colorectal surgery. Arch Surg. 146(9):1068–1072. doi: 10.1001/archsurg.2011.117. [DOI] [PubMed] [Google Scholar]
- 25.Hirose K, Shore AD, Wick EC, et al. Pay for obesity? Pay-for-performance metrics neglect increased complication rates and cost for obese patients. J Gastrointest Surg. 15(7):1128–1135. doi: 10.1007/s11605-011-1529-3. [DOI] [PubMed] [Google Scholar]
- 26.Sommers A. Obesity Among Older Americans. Congressional Research Service. 2009 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.