Abstract
Disruptions in circadian and diurnal rhythms are associated with stress-related psychiatric disorders and stressor exposure can disrupt these rhythms. The controllability of the stressor can modulate various behavioral and neurochemical responses to stress. Uncontrollable, but not controllable, stress produces behaviors in rats that resemble symptoms of anxiety and depression. Whether acute stress-induced disruptions in physiological rhythms are sensitive to controllability of the stressor, however, remains unknown. To examine the role of controllability in diurnal rhythm disruption, adult male Sprague Dawley rats were implanted with Data Sciences International (DSI) biotelemetry devices. Real-time measurements were obtained before, during and after exposure to a controllable or yoked uncontrollable stressor. Controllable and uncontrollable stress equally disrupted diurnal rhythms of locomotor activity and body temperature but not heart rate. The diurnal heart rate the day following stressor exposure was flattened to a greater extent and was significantly higher in rats with control over stress suggesting a relationship between stressor controllability and the heart rate response. Our results are consistent with the conclusion that acute stress-induced disruptions in diurnal physiological rhythms likely contribute little to the behavioral and affective consequences of stress that are sensitive to stressor controllability.
Keywords: Controllability, Stress, Diurnal Rhythm, Heart Rate, Body Temperature, Locomotor Activity
1. Introduction
Disruptions in normal circadian and diurnal rhythms are associated with a number of stress-related psychiatric disorders including depression [1, 2, 3, 4], anxiety [5, 6, 7, 8] and post-traumatic stress disorder (PTSD) [9, 10, 11]. Depressed individuals, for example, have altered temperature rhythms [12, 13, 14, 15], and individuals with depression, anxiety, and PTSD have disrupted cortisol and sleep rhythms [5, 6, 9, 16, 17, 18]. Despite the clear association between stress-related psychiatric disorders and disruptions in these rhythms, it remains unclear whether disruptions in diurnal rhythms are a cause or a consequence of these disorders.
Consistent with a causal relationship between diurnal rhythm disruption and stress-related psychiatric disorders are numerous observations that exposure to stress can disrupt diurnal rhythms and that rhythm disruption precedes behavioral symptoms in pre-clinical models. Chronic social defeat, for example, can disrupt normal rhythms of activity, heart rate and body temperature as well as produce depression-like behavior in rodents [19, 20, 21, 22]. Importantly, treatment with antidepressants can reverse the disruption in rhythms produced by social defeat stress [19, 20, 23, 24]. Furthermore, manipulation of clock genes can alter diurnal rhythms and increase depression- and anxiety-like behavior [25, 26, 27, 28], suggesting that disruptions in normal rhythms are sufficient to produce behavioral symptoms observed in stress-related psychiatric disorders. Together these studies support the possibility that disruptions in diurnal rhythms are not simply a consequence of stressor exposure, but could be contributing to the pathology underlying the development of stress-related psychiatric disorders.
The ability to control stress through behavioral responses is a powerful modulator of future neurochemical and behavioral outcomes of stressor exposure. In humans, diminished perception of control has been related to greater PTSD symptom severity [29]. Similarly, rodents exposed to a stressor such as uncontrollable tail shock display hyperactivity of serotonergic systems [30, 31, 32, 33], as well as depression- and anxiety-like behaviors including enhanced fear conditioning [34], reduced social exploration [35, 36, 37] and a deficit in shuttle box escape learning [30, 36]. Importantly, none of these changes occur if animals are given the opportunity to learn to control the termination of the tail shocks. Uncontrollable stressors also disrupt regular diurnal rhythms. Both uncontrollable tail shock [38, 39] and social stress [40] disrupt activity patterns in rats, while those rats that fail to counter attack during social defeat (who may lack the perception of control) suffer the greatest disruption of diurnal rhythms of locomotor activity, heart rate, and body temperature [22, 41]. Although it is clear that uncontrollable stressors can disrupt rhythms, less work has investigated whether acute stress-induced rhythm disruption is sensitive to stressor controllability. If disruptions in mechanisms underlying diurnal physiological rhythms are a causal factor in the development of symptoms of stress-related disorders, then one would predict that uncontrollable stressors would produce greater physiological rhythm disruption than do stressors that are controllable.
The purpose of the current study was to determine whether acute stress-induced disruptions in diurnal rhythms of physiology are sensitive to the controllability of the stressor. Rats were implanted with Data Sciences International (DSI) biotelemetry devices and exposed to controllable or yoked uncontrollable tail shock stress. Locomotor activity, heart rate, blood pressure, and core body temperature were measured for 24 hours prior to, during, and 48 hours following stress. The results from this work may shed light on the role of diurnal rhythm disruption in stress-related psychiatric disorders.
2. Materials and Methods
2.1 Animals
Adult male Sprague-Dawley rats (n = 10, Harlan Laboratories) weighing 200g–230g; were housed with controlled temperature (22°C) and humidity. The animals were maintained on a 12:12 hour light/dark cycle (lights on 0700–1900 hours). All rats were housed in Nalgene Plexiglas cages (45 × 25.2 × 14.7 cm) and were allowed to acclimate to the housing conditions for one week before surgery. Rats had ad libitum access to food and water and were weighed weekly. All experimental procedures were performed during the inactive cycle and animals were handled during the 1 week acclimation period. Animal discomfort was minimized during all procedures. Experimental protocols for these studies were approved by the University of Colorado Animal Care and Use Committee.
2.2 Biotelemetry Surgeries
The C50-PXT biotelemetry transmitters (Data Sciences International, St. Paul, MN) were implanted into animals as previously described [42]. Briefly, animals were fully anesthetized and unresponsive following ketamine (i.p. 75.0 mg/kg), and medetomidine (i.p. 0.5 mg/kg). Animals were shaved and prepped for surgery. Body temperature was maintained on a heating pad and monitored throughout surgery. A midline incision was made approximately 5.0 cm in length on the ventral abdominal wall. Intestines were gently moved and the abdominal aorta isolated. The abdominal aorta was occluded rostral to the catheter entry site. Once occluded, the blood pressure catheter was inserted into the abdominal aorta and secured in place with a cellulose patch (Data Sciences International, St. Paul Minnesota) and glue (3M Vetbond Adhesive). The intestines were gently floated back into place with sterile saline and the C50-PXT transmitter was sutured into the ventral abdominal wall. Finally, the ECG leads were sutured into place to measure cardiac electrical activity. Animals were allowed to recover for 10 days before recording began.
2.3 Data Acquisition and Analysis
The C50-PXT transmitter allows real time measurement of locomotor activity (LA), heart rate (HR), QA Interval (QAI), blood pressure (SBP, MAP, DBP and PP), and core body temperature (CBT). The QAI is a measure of the time (milliseconds) between the Q-wave (Q) of the QRS complex and the onset of the aortic pulse (A) and can be used as an estimate of cardiac contractility as previously described [42]. There is an inverse relationship between the QAI and cardiac contractility such that a decrease in the QAI can be estimated as an increase in cardiac contractility [42, 43, 44]. Biotelemetry recordings were acquired/analyzed using Dataquest ART 4.3 Gold Acquisition and Analysis Software (Data Sciences International, St. Paul, MN). Locomotor activity, heart rate, and blood pressure were recorded at 500 Hz. A total of 10 rats were implanted with C50-PXT transmitters but one rat was dropped from the ES group due to technical difficulties with acquiring accurate readings from the transmitter.
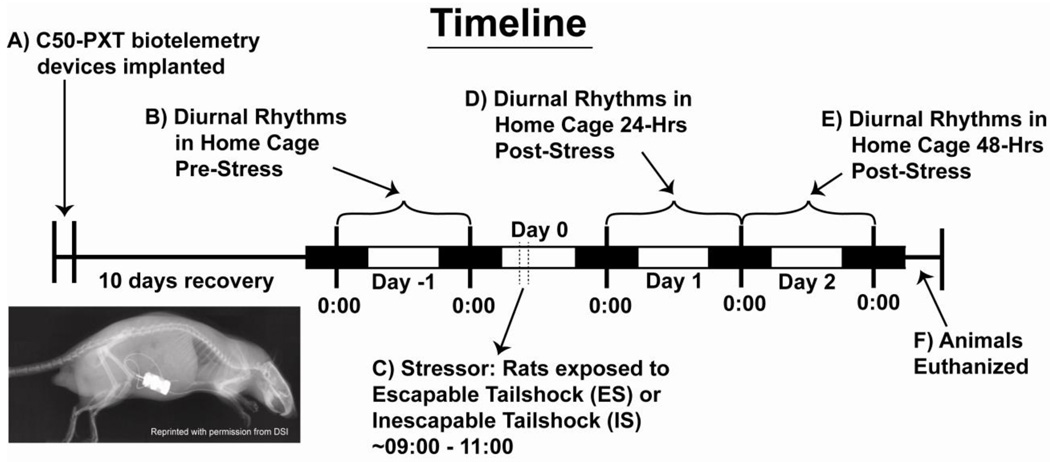
2.4 Experimental Design (Figure 1)
Figure 1.
A) Rats were implanted with the C50-PXT biotelemetry devices and allowed 10 days to recover before recording began. B) Diurnal rhythms were measured uninterrupted in the home cage for twenty-four hours from midnight to midnight (Day -1) before stressor exposure. C) The following day (Day 0) rats were exposed to either escapable stress (ES) or yoked inescapable stress (IS). Diurnal rhythms were again measured uninterrupted in the home cage for D) twenty-four hours (Day 1) and E) forty-eight hours (Day 2) from midnight to midnight.
Stabilization of normal diurnal rhythms after surgery takes around 10 days [42, 45]. Therefore following 10 days of recovery, biotelemetry recordings were obtained for twenty-four hours from 0000h to 0000h (midnight to midnight) before stressor exposure (Day -1) in order to obtain accurate pre-stress diurnal variations. The following light cycle (Day 0), rats were exposed to either controllable/escapable tail shock (ES) or uncontrollable/inescapable tail shock (IS) from 0900hrs to 1100hrs. Stress during this time period is consistent with previous publications examining behavioral control over stressors [30, 33, 46] and induces greater responses in several physiological parameters, such as adrenal and body weights [47, 48]. Following stressor exposure, biotelemetry recordings were measured in the home cage immediately after, on Day 1, and on Day 2 in order to compare whether behavioral control over stressor exposure impacted subsequent diurnal physiological rhythms. Since previous studies have demonstrated altered diurnal rhythms the day following stressor exposure [22, 41, 49] and due to limited equipment availability, a non-stressed control group was not included in this experiment. Importantly, the main focus of this manuscript was whether having behavioral control over the stressful experience would alter this response, not whether stressor exposure, per sedisrupts diurnal physiological rhythms.
2.5 Stressor Controllability Procedure
As previously described [30, 35], rats were placed in clear Plexiglas boxes (11 × 14 × 17 cm) containing a wheel at the front, which were placed in sound-attenuating chambers. The tail was taped to a Plexiglass rod that extended from the back of the box, and two copper electrodes were attached to the tail with cloth tape and augmented with electrolyte paste. Tail shock was delivered by a Precision Regulated Animal Shocker operated by a computer and Graphic State 3.0 software (Coulbourn Instruments, Allentown, PA). Each rat received 100 trials of tail shock (33 trials × 1.0 mA, 33 trials × 1.3 mA, and 34 trials × 1.6 mA) on a variable interval schedule (average 60 sec; range = 20–140 sec). Tail shocks were given to yoked rat pairs (ES and IS) such that the shock terminated for both the ES and IS rats when the ES rats turned the wheel. The contingency required for the ES rats at the beginning of the stressor was a one-quarter turn of the wheel. The response requirement doubled on the subsequent trial if the response was made within 5 s of shock onset. The maximum response was 4 wheel turns. If the response was made between 6 and 20 s the requirement stayed the same. If no response was made after 30 s the shock was terminated by the computer and the escape requirement was reset to a one-quarter wheel turn. This procedure was used to insure that the ES subjects learned an operant escape response. Rats in the IS condition were placed in identical chambers but the wheel was locked in place.
2.6 Statistical Analysis
In order to examine the acute effects of controllable and uncontrollable stress on physiology, repeated measures ANOVA with time and controllability as the factors were performed on 20 minute blocks of biotelemetry data both prior to (60 min), during (120 min), and following (180 min) stressor exposure. These data were additionally collapsed into pre, during, and post-stress values and compared with repeated measures ANOVA. In order to capture the effects of stressor controllability on diurnal (i.e. day/night) differences in physiology, 12-hour averaged night values were subtracted from 12-hour averaged day values collected the day prior to, and two days following, stressor exposure (Day -1, Day 1, and Day 2). Repeated measures ANOVA were performed on the difference scores with time and controllability as factors. Finally, in order to examine in greater temporal detail how control over the stressor affected biotelemetric measures of physiology, data collected the day prior to stress and on day 1 following stress, were collapsed into 1-hour blocks. Area under the curve was calculated and groups were compared with ANOVA. Repeated measures ANOVA were also performed on the 1-hour blocks with control as a factor. When appropriate, post hoc analyses were performed using Fisher’s protected least significant differences (PLSD). Alpha was set to p < 0.05.
3. Results
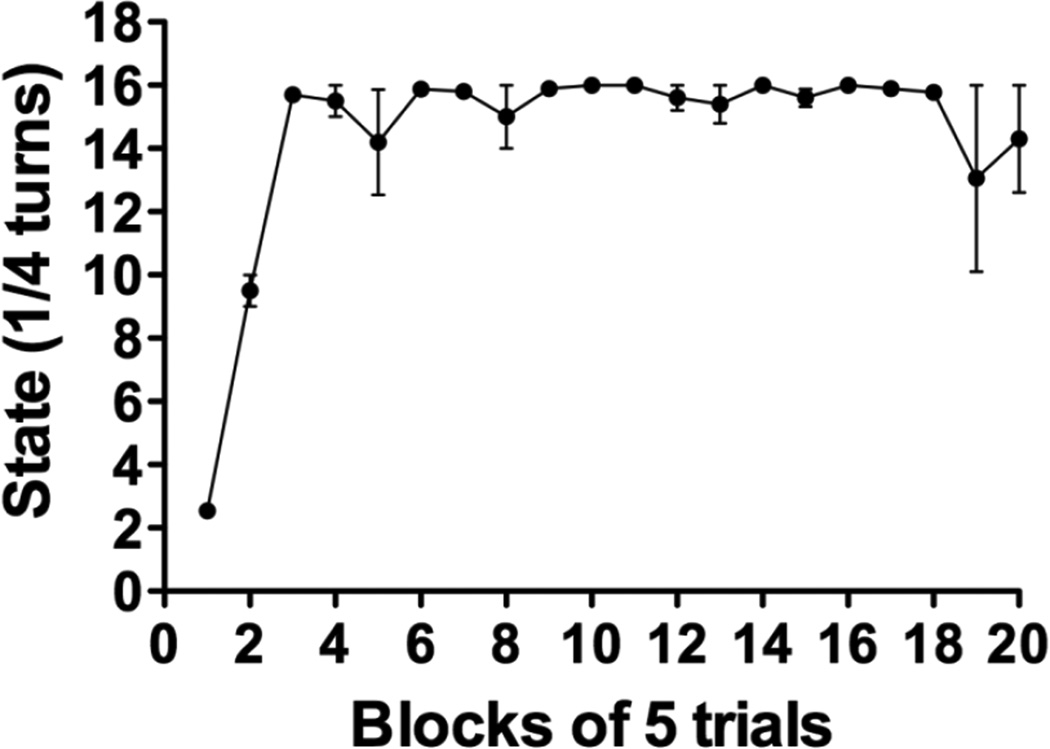
3.1 Wheel rotations (Figure 2)
Figure 2.
Efficiency of wheel-turn behavior during stressor exposure in rats that had control (ES) over tail shock and learned to escape. Rats in the IS group had locked wheels and were yoked to ES rats, receiving the same amount of stress but were unable to turn the wheels. Data represents the mean number (± s.e.m.) of ¼ wheel turns in order to escape on each trial. Sixteen ¼ turns equaled 4 full revolutions of the wheel, which was the criterion to terminate the tail shock by the third block of trials.
Rats exposed to ES quickly learned to escape such that average trial lengths were approximately 3–5 s (Figure 2). The rats in the ES group learned to terminate shock by trial block 3 (F(19, 57) = 15.163; p < 0.0001) which required a full 4 turns or 16 quarter turns. No differences in body weights were observed between the ES and IS groups prior to stress exposure (F(1,7) = 0.00011; p = 0.99) or after stressor exposure (F(1,7) = 0.002; p = 0.96)(data not shown).
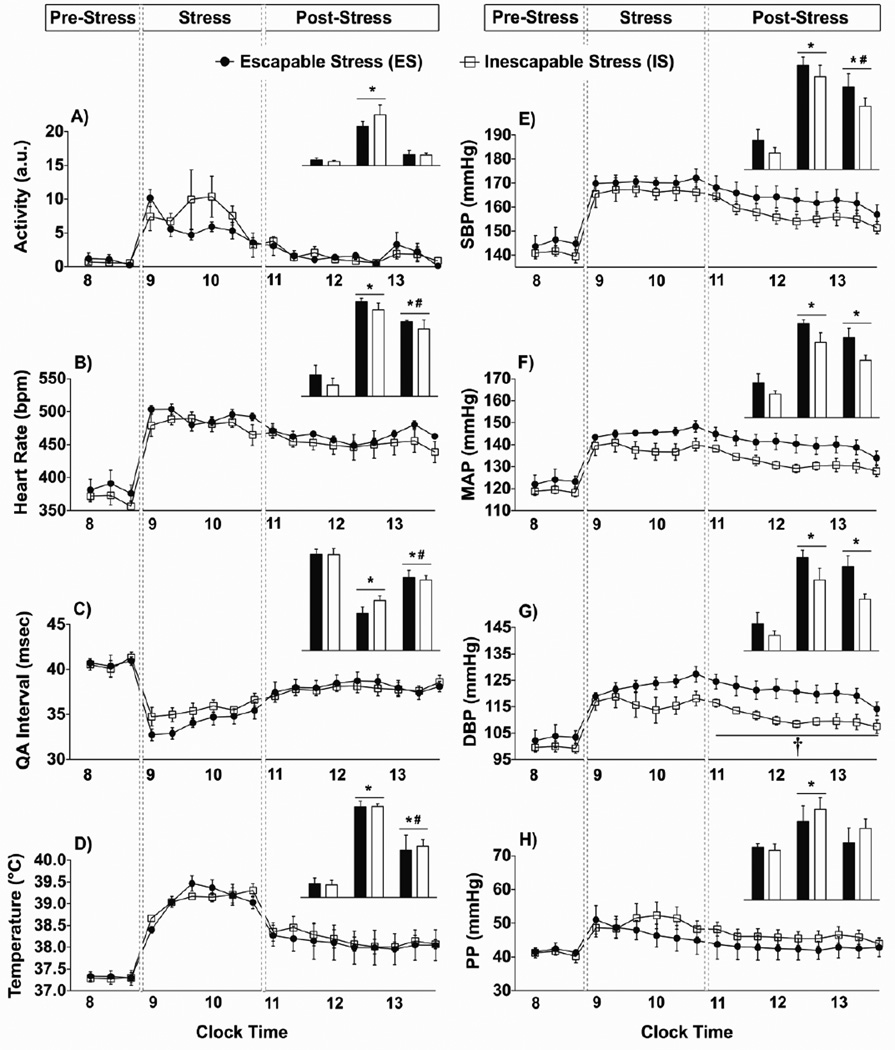
3.2 Telemetric measures the day of stressor exposure (Figure 3)
Figure 3.
Data are graphed in 20-minute blocks (or averaged, insets) before stress in the home cage, during stress, and immediately after stress upon return to the home cage. A) Locomotor activity was significantly increased during stress, but not after. B) Heart rate was significantly increased during stress and remained elevated after stressor exposure. C) QA interval was decreased during stress and remained decreased after stressor exposure. D) Core body temperature was significantly increased during stress and remained elevated after exposure. E-H) Systolic blood pressure (SBP), mean arterial pressure (MAP), diastolic blood pressure (DBP) and pulse pressure (PP) were significantly increased during stress. G) A higher DBP in the ES group developed during stress and remained significantly higher relative to the IS group in the home cage after exposure. (* p < 0.05 compared to pre-stress values; # p < 0.05 compared to during stress values; † p < 0.05 ES compared to IS)
Twenty-minute blocks of telemetry data obtained in the home cage immediately prior to stressor exposure (pre-stress), during exposure to stress, and upon return to the home cage (post-stress) are shown in Figure 3. The averaged values of each time point (pre, during, and post-stress) are shown in the graph insets. There were no differences between groups prior to stressor exposure and, in general, exposure to ES and IS produced similar stress responses. Locomotor activity increased during stressor exposure regardless of controllability (F(2,14) = 31.632; p < 0.0001), but returned to pre-stress levels rapidly upon return to the home cage following stress (Figure 3A). Heart rate (Figure 3B) increased during stress regardless of controllability (F(2,14) = 72.509; p < 0.0001). Heart rate remained elevated above pre-stress levels upon return to the home cage (p < 0.05); though heart rate following stress wasn’t as high as levels during stressor exposure (p < 0.05). Similar patterns were also observed for QA Interval (F(2,14) =123.178 ; p < 0.0001; Figure 3C), core body temperature (F(2,14) = 103.885; p < 0.0001; Figure 3D), and systolic blood pressure (F(2,14) = 158.858; p < 0.0001). Stress, regardless of controllability, increased mean arterial pressure both during stress and for several hours upon return to the home cage (F(2,14) = 82.697; p < 0.0001; Figure 3F). In contrast, diastolic blood pressure was elevated in both groups during stressor exposure (F(2,14) = 46.432; p < 0.0001), but rats exposed to ES had higher diastolic blood pressure both during (F(5,35) = 3.025; p = 0.02) and after (F(1,7) = 8.508; p = 0.02) stress compared to rats exposed to IS (Figure 3G). Finally, pulse pressure was increased by stress regardless of controllability (F(2,14) = 20.476; p < 0.0001), but returned to pre-stress levels within 2 hours after return to the home cage after stress (Figure 3H).
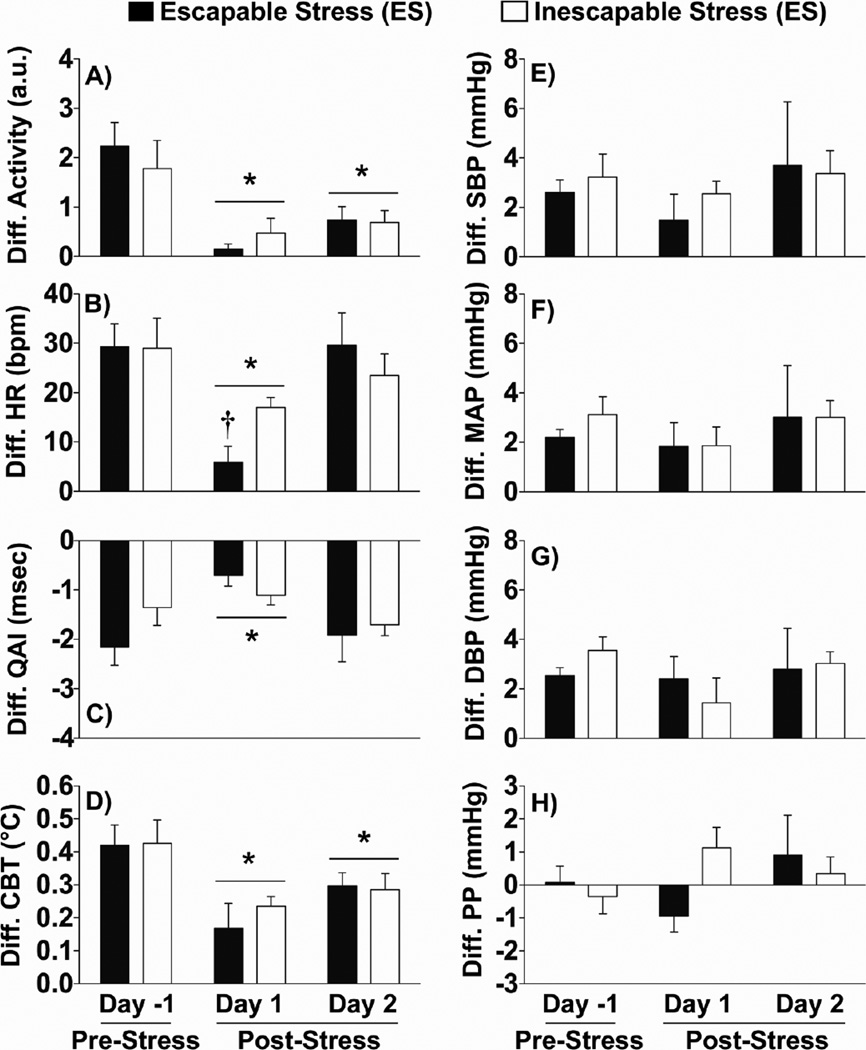
3.3 Effect of controllable and uncontrollable stress on diurnal rhythms of physiology. (Figure 4)
Figure 4.
Data are graphed as the difference between the 12-hour night and the 12-hour day averaged values to reveal how controllability affected the diurnal rhythms following stressor exposure. A) The diurnal rhythm in locomotor activity, regardless of control, was reduced after stressor exposure on day 1 and day 2. B) The diurnal rhythm in heart rate was reduced after stressor exposure, but ES rats had a greater reduction than IS rats and by day 2 both effects were gone. C) The diurnal rhythm in the QA Interval, regardless of control, was also reduced only on day 1 after stressor exposure. D) The diurnal rhythm of temperature, regardless of controllability, was reduced following stress on both day 1 and day 2. E–F) There were no effects of stressor exposure on diurnal rhythms of blood pressure. Abbreviations are as follows: arbitrary units (a.u.), systolic blood pressure (SBP), mean arterial pressure (MAP), diastolic blood pressure (DBP), and pulse pressure (PP). (* p < 0.05 when compared to pre-stress values; † p < 0.05 ES compared to IS)
Stress, regardless of controllability, flattened the diurnal rhythm of locomotor activity (F(2,14) = 30.433; p < 0.0001; Figure 4A) and core body temperature (F(2,14) = 10.321; p = 0.0018; Figure 4D) for at least 2 days following stressor exposure. Stress flattened the diurnal rhythm of heart rate (F(2,14) = 18.534; p = 0.0001; Figure 4B). Surprisingly, ES, relative to IS, produced a greater flattening of the diurnal rhythm of heart rate on day 1 following stress (F(2,14) = 4.149; p = 0.0401). The normal rhythm of heart rate was restored in both ES and IS groups by day 2. Stress, regardless of controllability, produced a transient flattening of the QA Interval (F(2,14) = 9.974; p = 0.002), such that there was a significant flattening on day 1, but not day 2, when compared to pre-stress values (Figure 4C). Although there were trends for time by controllability interactions for QA Interval (F(2,14) = 3.726; p = 0.0604) and pulse pressure (F(2,14) = 3.047; p = 0.0797; Figure 4H), these differences were not significant. Diurnal rhythms of systolic blood pressure (Figure 4E), mean arterial pressure (Figure 4F), and diastolic blood pressure (Figure 4G) were not impacted by either ES or IS. Results of post hoc analyses are denoted in Figure 4.
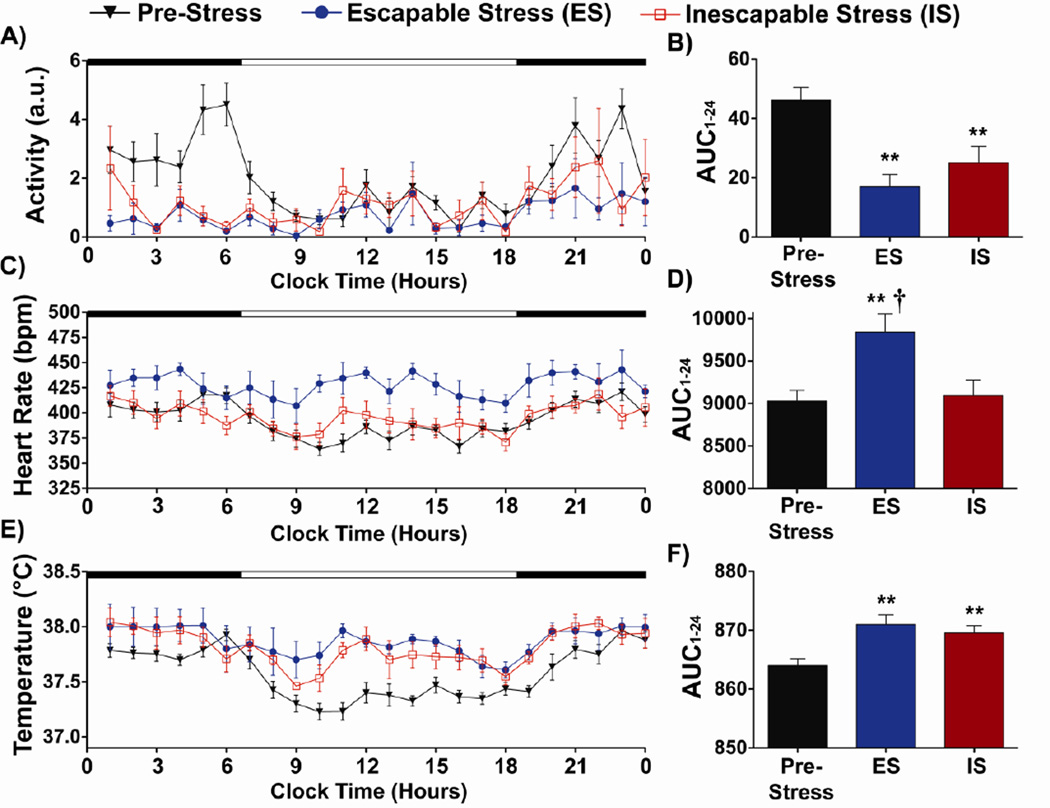
3.4 Real-time telemetric measures in the home cage on Day 1 following stressor exposure (Figure 5)
Figure 5.
Locomotor activity, heart rate, and core body temperature data are expressed as 1-hour blocks and as area-under the curve (AUC), obtained pre-stress and day 1 following stressor exposure. A,B) Locomotor activity was significantly reduced after stressor exposure regardless of controllability. C,D) Escapable stress (ES), but not iescapable stress, increased heart rate the day following stressor exposure. E,F) Core body temperature was significantly higher than pre-stress values following both ES and IS. Abbreviations are as follows: arbitrary units (a.u.), area under the curve for 24-hours (AUC1–24). (** p < 0.01 compared to pre-stress values. † p < 0.01 ES compared to IS group)
Diurnal analysis (Figure 4) revealed the greatest flattening of activity, heart rate, and body temperature rhythms following stress, so these parameters were examined in greater temporal resolution during day 1 following stress. Although pre-stress values were not included in the analyses, pre-stress values are included in the graphs for ease of interpretation. Neither locomotor activity (Figure 5A) nor core body temperature (Figure 5E) were impacted differentially by stressor controllability. Controllable stress, however, produced a significantly higher heart rate compared to uncontrollable stress (F(1,7) = 7.046; p = 0.032; Figure 5C). For comparison with pre-stress values, area under the curve analysis was performed. Stressor exposure significantly altered the area under the curve for locomotor activity (F(2,15) = 10.103; p = 0.0017; Figure 5B), heart rate (F(2,15) = 6.215; p = 0.0108; Figure 5D) and core body temperature (F(2,15) = 7.858; p = 0.0046; Figure 5F). Post hoc analyses are denoted in Figure 5.
4. Discussion
The current study investigated whether stress-induced disruptions in diurnal physiological and behavioral rhythms are sensitive to controllability, and specifically, if exposure to an acute uncontrollable stressor would produce greater physiological rhythm disruption than exposure to a controllable one. Here we report that both uncontrollable and controllable stressor exposure disrupted diurnal rhythms. Consistent with prior reports [22, 41], diurnal rhythms were disrupted for at least 24–48 hours after stressor termination. Specifically, locomotor activity was substantially reduced during the night (active) cycle and core body temperature was substantially higher during the day (inactive) cycle compared to pre-stress levels, which is in agreement with previous studies [49]. In addition, uncontrollable stress failed to disrupt diurnal rhythms more than did controllable stress. In fact, the rhythm disruption of heart rate was greater in rats with control over tail shock than in uncontrollably stressed rats. Interestingly, there was not just a disrupted diurnal heart rate but rather a sustained elevation across both the day and night in rats with control over stress. These results suggest that the ability to control stress has little influence on the mechanisms underlying stress-induced disruptions in locomotor activity and core body temperature rhythms, but that heart rate may be differentially influenced by stressor controllability.
Although stress-induced disruptions in diurnal locomotor activity and body temperature rhythms are not sensitive to controllability, the mechanisms for their disruption may depend on a variety of factors. These factors could include stress-induced disruptions in central circuits controlling diurnal rhythms such as the suprachiasmatic nucleus (SCN) or central clock genes, and/or peripheral clock genes themselves. Interactions of these systems with glucocorticoids could also be an important factor contributing to stress-induced rhythm disruption. Per1for example, is a particularly stress-responsive clock gene, both in the periphery [50] and brain [51], and the expression of Per1 is related to circulating glucocorticoids [52]. In fact, glucocorticoids can entrain Per1 expression in the periphery [53]. Tail shock exposure increases basal circulating glucocorticoids, specifically elevating trough corticosterone levels, for at least 48 hours after exposure [54]. This increase is not sensitive to the controllability of the stressor [55]. Together, these data suggest that stress, regardless of control, could influence diurnal rhythms via a mechanism involving glucocorticoid modulation of the clock gene Per1.
In contrast to other physiological rhythms, the ability to control stress did lead to a higher sustained heart rate the day following stressor exposure. Although the difference in HR between rats exposed to ES and IS could also depend on either peripheral or central mechanisms, the ability to control stress is a psychological factor; thus implicating a central mechanism. The medial prefrontal cortex (mPFC) is critical for the differential effects of ES and IS on neurochemistry and behavior [30, 35, 56]. It is therefore possible that the mPFC mediates the differential effects of controllability on the diurnal HR response to stress. Consistent with this idea, the mPFC has been reported to be involved in stress-evoked heart rate responses [57, 58, 59, 60] and the baroreflex parasympathetic component of the cardiac response to stressor exposure [61, 62, 63]. The mPFC can be subdivided into several distinct regions including the prelimbic (PL) and the infralimbic (IL) cortex comprising the ventral mPFC [64, 65, 66], which when stimulated produces greater cardiovascular effects than other areas of the mPFC [64, 67]. Both the PL cortex and the IL cortex project extensively throughout the brain with one key difference being that only the IL cortex projects to the nucleus tractus solitarius or NTS [66, 68], which is the site of the first synapse of baroreceptor afferent projections [69]. Furthermore, the IL cortex receives strong afferent input from the SCN [70] and there are diurnal differences in structural plasticity of pyramidal cells within the IL cortex which are reduced by stressor exposure [71]. One explanation, therefore, could be that having control over the stressor transiently alters neurotransmission within the mPFC leading to the higher sustained heart rate the day following stressor exposure.
Regardless of the mechanism, it is of interest to speculate whether a sustained elevation in heart rate following exposure to a controllable versus an uncontrollable stressor is somehow adaptive or beneficial. Although chronic elevations in HR can contribute to stress-related illness such as cardiovascular disease [72, 73], the elevation in heart rate in rats exposed to controllable stress was temporary since within 48 hours after stress the heart rate in rats with control had almost returned to pre-stress levels (Figure 4B, Day 2). It is possible that the temporary elevation in HR following ES reflects an adaptive, preparatory response to facilitate fighting or fleeing from subsequent challenges. Future studies could examine whether a sustained elevation in heart rate after a controllable stressor depends on mPFC involvement.
In conclusion, the current results are largely in agreement with previous studies reporting that acute stressor exposure produces disruptions in physiological diurnal rhythms. We add to this literature by demonstrating that behavioral control over stress modulated the effect of stress-induced HR rhythm disruption, but had little impact on stress-induced rhythm disruption in core body temperature and locomotor activity. Our results are consistent with the interpretation that acute stress-induced disruptions in diurnal physiological rhythms are a consequence of stressor exposure and likely do not directly contribute to the behavioral and affective consequences of stress that are sensitive to stressor controllability.
Highlights.
Rhythm disruption is linked to stress-related disorders and stress disrupts rhythms.
Control over stress modulates various behavioral/neurochemical responses to stress.
Uncontrollable stress produces behaviors resembling symptoms of anxiety/depression.
Stress-induced rhythm disruption may be sensitive to controllability of the stressor.
Diurnal heart rate, but not activity or temperature, is sensitive to control.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Robert S. Thompson, Email: robert.s.thompson@colorado.edu.
John P. Christianson, Email: john.christianson@colorado.edu.
Thomas M. Maslanik, Email: thomas.maslanik@colorado.edu.
Steve F. Maier, Email: steve.maier@colorado.edu.
Benjamin N. Greenwood, Email: ben.greenwood@colorado.edu.
References
- 1.Cole RJ, Loving RT, Kripke DF. Psychiatric aspects of shiftwork. Occupational medicine. 1990;5:301–314. [PubMed] [Google Scholar]
- 2.Scott AJ, Monk TH, Brink LL. Shiftwork as a Risk Factor for Depression: A Pilot Study. International journal of occupational and environmental health. 1997;3:S2–S9. [PubMed] [Google Scholar]
- 3.Hasler BP, Buysse DJ, Kupfer DJ, Germain A. Phase relationships between core body temperature, melatonin, and sleep are associated with depression severity: further evidence for circadian misalignment in non-seasonal depression. Psychiatry research. 2010;178:205–207. doi: 10.1016/j.psychres.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emens J, Lewy A, Kinzie JM, Arntz D, Rough J. Circadian misalignment in major depressive disorder. Psychiatry research. 2009;168:259–261. doi: 10.1016/j.psychres.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Kyung Lee E, Douglass AB. Sleep in psychiatric disorders: where are we now? Canadian journal of psychiatry Revue canadienne de psychiatrie. 2010;55:403–412. doi: 10.1177/070674371005500703. [DOI] [PubMed] [Google Scholar]
- 6.Pervanidou P, Bastaki D, Chouliaras G, Papanikolaou K, Laios E, et al. Circadian cortisol profiles, anxiety and depressive symptomatology, and body mass index in a clinical population of obese children. Stress. 2012 doi: 10.3109/10253890.2012.689040. [DOI] [PubMed] [Google Scholar]
- 7.Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders. A meta-analysis. Archives of general psychiatry. 1992;49:651–668. doi: 10.1001/archpsyc.1992.01820080059010. discussion 669–670. [DOI] [PubMed] [Google Scholar]
- 8.Ohayon MM, Roth T. What are the contributing factors for insomnia in the general population? Journal of psychosomatic research. 2001;51:745–755. doi: 10.1016/s0022-3999(01)00285-9. [DOI] [PubMed] [Google Scholar]
- 9.Morris MC, Compas BE, Garber J. Relations among posttraumatic stress disorder, comorbid major depression, and HPA function: a systematic review and meta-analysis. Clinical psychology review. 2012;32:301–315. doi: 10.1016/j.cpr.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Germain A, Nielsen TA. Sleep pathophysiology in posttraumatic stress disorder and idiopathic nightmare sufferers. Biological psychiatry. 2003;54:1092–1098. doi: 10.1016/s0006-3223(03)00071-4. [DOI] [PubMed] [Google Scholar]
- 11.Breslau N, Roth T, Burduvali E, Kapke A, Schultz L, et al. Sleep in lifetime posttraumatic stress disorder: a community-based polysomnographic study. Archives of general psychiatry. 2004;61:508–516. doi: 10.1001/archpsyc.61.5.508. [DOI] [PubMed] [Google Scholar]
- 12.Avery DH, Wildschiodtz G, Rafaelsen OJ. Nocturnal temperature in affective disorder. Journal of affective disorders. 1982;4:61–71. doi: 10.1016/0165-0327(82)90020-9. [DOI] [PubMed] [Google Scholar]
- 13.Monk TH, Buysse DJ, Frank E, Kupfer DJ, Dettling J, et al. Nocturnal and circadian body temperatures of depressed outpatients during symptomatic and recovered states. Psychiatry research. 1994;51:297–311. doi: 10.1016/0165-1781(94)90016-7. [DOI] [PubMed] [Google Scholar]
- 14.Posener JA, DeBattista C, Williams GH, Chmura Kraemer H, Kalehzan BM, et al. 24-Hour monitoring of cortisol and corticotropin secretion in psychotic and nonpsychotic major depression. Archives of general psychiatry. 2000;57:755–760. doi: 10.1001/archpsyc.57.8.755. [DOI] [PubMed] [Google Scholar]
- 15.Souetre E, Salvati E, Belugou JL, Pringuey D, Candito M, et al. Circadian rhythms in depression and recovery: evidence for blunted amplitude as the main chronobiological abnormality. Psychiatry research. 1989;28:263–278. doi: 10.1016/0165-1781(89)90207-2. [DOI] [PubMed] [Google Scholar]
- 16.Meewisse ML, Reitsma JB, de Vries GJ, Gersons BP, Olff M. Cortisol and post-traumatic stress disorder in adults: systematic review and meta-analysis. The British journal of psychiatry : the journal of mental science. 2007;191:387–392. doi: 10.1192/bjp.bp.106.024877. [DOI] [PubMed] [Google Scholar]
- 17.Laudenslager ML, Noonan C, Jacobsen C, Goldberg J, Buchwald D, et al. Salivary cortisol among American Indians with and without posttraumatic stress disorder (PTSD): gender and alcohol influences. Brain, behavior, and immunity. 2009;23:658–662. doi: 10.1016/j.bbi.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sachar EJ, Hellman L, Fukushima DK, Gallagher TF. Cortisol production in depressive illness. A clinical and biochemical clarification. Archives of general psychiatry. 1970;23:289–298. doi: 10.1001/archpsyc.1970.01750040001001. [DOI] [PubMed] [Google Scholar]
- 19.Fuchs E. Social stress in tree shrews as an animal model of depression: an example of a behavioral model of a CNS disorder. CNS spectrums. 2005;10:182–190. doi: 10.1017/s1092852900010038. [DOI] [PubMed] [Google Scholar]
- 20.Corbach S, Schmelting B, Fuchs E, Mocaer E. Comparison of agomelatine and melatonin for effects in chronically stressed tree shrews, an animal model of depression. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2007;Volume 17:S364–S365. [Google Scholar]
- 21.Krishnan V, Han MH, Graham DL, Berton O, Renthal W, et al. Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell. 2007;131:391–404. doi: 10.1016/j.cell.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 22.Meerlo P, Sgoifo A, De Boer SF, Koolhaas JM. Long-lasting consequences of a social conflict in rats: behavior during the interaction predicts subsequent changes in daily rhythms of heart rate, temperature, and activity. Behavioral neuroscience. 1999;113:1283–1290. doi: 10.1037//0735-7044.113.6.1283. [DOI] [PubMed] [Google Scholar]
- 23.Friedman A, Shaldubina A, Flaumenhaft Y, Weizman A, Yadid G. Monitoring of circadian rhythms of heart rate, locomotor activity, and temperature for diagnosis and evaluation of response to treatment in an animal model of depression. Journal of molecular neuroscience : MN. 2011;43:303–308. doi: 10.1007/s12031-010-9441-y. [DOI] [PubMed] [Google Scholar]
- 24.Overstreet DH, Friedman E, Mathe AA, Yadid G. The Flinders Sensitive Line rat: a selectively bred putative animal model of depression. Neuroscience and biobehavioral reviews. 2005;29:739–759. doi: 10.1016/j.neubiorev.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 25.Keers R, Pedroso I, Breen G, Aitchison KJ, Nolan PM, et al. Reduced anxiety and depression-like behaviours in the circadian period mutant mouse afterhours. PloS one. 2012;7:e38263. doi: 10.1371/journal.pone.0038263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li JD, Hu WP, Zhou QY. Disruption of the circadian output molecule prokineticin 2 results in anxiolytic and antidepressant-like effects in mice. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2009;34:367–373. doi: 10.1038/npp.2008.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roybal K, Theobold D, Graham A, DiNieri JA, Russo SJ, et al. Mania-like behavior induced by disruption of CLOCK. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:6406–6411. doi: 10.1073/pnas.0609625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curtis AM, Cheng Y, Kapoor S, Reilly D, Price TS, et al. Circadian variation of blood pressure and the vascular response to asynchronous stress. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:3450–3455. doi: 10.1073/pnas.0611680104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bolstad BR, Zinbarg RE. Sexual victimization, generalized perception of control, and posttraumatic stress disorder symptom severity. Journal of Anxiety Disorders. 1997;11:523–540. doi: 10.1016/s0887-6185(97)00028-5. [DOI] [PubMed] [Google Scholar]
- 30.Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, et al. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus. Nature neuroscience. 2005;8:365–371. doi: 10.1038/nn1399. [DOI] [PubMed] [Google Scholar]
- 31.Christianson JP, Ragole T, Amat J, Greenwood BN, Strong PV, et al. 5-hydroxytryptamine 2C receptors in the basolateral amygdala are involved in the expression of anxiety after uncontrollable traumatic stress. Biological psychiatry. 2010;67:339–345. doi: 10.1016/j.biopsych.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grahn RE, Will MJ, Hammack SE, Maswood S, McQueen MB, et al. Activation of serotonin-immunoreactive cells in the dorsal raphe nucleus in rats exposed to an uncontrollable stressor. Brain research. 1999;826:35–43. doi: 10.1016/s0006-8993(99)01208-1. [DOI] [PubMed] [Google Scholar]
- 33.Maswood S, Barter JE, Watkins LR, Maier SF. Exposure to inescapable but not escapable shock increases extracellular levels of 5-HT in the dorsal raphe nucleus of the rat. Brain research. 1998;783:115–120. doi: 10.1016/s0006-8993(97)01313-9. [DOI] [PubMed] [Google Scholar]
- 34.Baratta MV, Christianson JP, Gomez DM, Zarza CM, Amat J, et al. Controllable versus uncontrollable stressors bi-directionally modulate conditioned but not innate fear. Neuroscience. 2007;146:1495–1503. doi: 10.1016/j.neuroscience.2007.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Christianson JP, Thompson BM, Watkins LR, Maier SF. Medial prefrontal cortical activation modulates the impact of controllable and uncontrollable stressor exposure on a social exploration test of anxiety in the rat. Stress. 2009;12:445–450. doi: 10.1080/10253890802510302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Christianson JP, Paul ED, Irani M, Thompson BM, Kubala KH, et al. The role of prior stressor controllability and the dorsal raphe nucleus in sucrose preference and social exploration. Behavioural brain research. 2008;193:87–93. doi: 10.1016/j.bbr.2008.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Short KR, Maier SF. Stressor controllability, social interaction, and benzodiazepine systems. Pharmacology, biochemistry, and behavior. 1993;45:827–835. doi: 10.1016/0091-3057(93)90128-g. [DOI] [PubMed] [Google Scholar]
- 38.Desan PH, Silbert LH, Maier SF. Long-term effects of inescapable stress on daily running activity and antagonism by desipramine. Pharmacology, biochemistry, and behavior. 1988;30:21–29. doi: 10.1016/0091-3057(88)90420-0. [DOI] [PubMed] [Google Scholar]
- 39.Woodmansee WW, Silbert LH, Maier SF. Factors that modulate inescapable shock-induced reductions in daily activity in the rat. Pharmacology, biochemistry, and behavior. 1993;45:553–559. doi: 10.1016/0091-3057(93)90505-n. [DOI] [PubMed] [Google Scholar]
- 40.Slattery DA, Uschold N, Magoni M, Bar J, Popoli M, et al. Behavioural consequences of two chronic psychosocial stress paradigms: anxiety without depression. Psychoneuroendocrinology. 2012;37:702–714. doi: 10.1016/j.psyneuen.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 41.Meerlo P, Sgoifo A, Turek FW. The effects of social defeat and other stressors on the expression of circadian rhythms. Stress. 2002;5:15–22. doi: 10.1080/102538902900012323. [DOI] [PubMed] [Google Scholar]
- 42.Thompson RS, Strong PV, Fleshner M. Physiological Consequences of Repeated Exposures to Conditioned Fear. Behavioral Sciences. 2012;2(2):57–78. doi: 10.3390/bs2020057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cambridge D, Whiting MV. Evaluation of the QA interval as an index of cardiac contractility in anaesthetised dogs: responses to changes in cardiac loading and heart rate. Cardiovascular research. 1986;20:444–450. doi: 10.1093/cvr/20.6.444. [DOI] [PubMed] [Google Scholar]
- 44.Chang CC, Hwang JS, Chan CC, Wang PY, Hu TH, et al. Effects of concentrated ambient particles on heart rate, blood pressure, and cardiac contractility in spontaneously hypertensive rats. Inhalation toxicology. 2004;16:421–429. doi: 10.1080/08958370490439579. [DOI] [PubMed] [Google Scholar]
- 45.Harper DG, Tornatzky W, Miczek KA. Stress induced disorganization of circadian and ultradian rhythms: comparisons of effects of surgery and social stress. Physiology & behavior. 1996;59:409–419. doi: 10.1016/0031-9384(95)02012-8. [DOI] [PubMed] [Google Scholar]
- 46.Amat J, Matus-Amat P, Watkins LR, Maier SF. Escapable and inescapable stress differentially alter extracellular levels of 5-HT in the basolateral amygdala of the rat. Brain research. 1998;812:113–120. doi: 10.1016/s0006-8993(98)00960-3. [DOI] [PubMed] [Google Scholar]
- 47.Bartlang MS, Neumann ID, Slattery DA, Uschold-Schmidt N, Kraus D, et al. Time matters: pathological effects of repeated psychosocial stress during the active, but not inactive, phase of male mice. The Journal of endocrinology. 2012;215:425–437. doi: 10.1530/JOE-12-0267. [DOI] [PubMed] [Google Scholar]
- 48.Rybkin II, Zhou Y, Volaufova J, Smagin GN, Ryan DH, et al. Effect of restraint stress on food intake and body weight is determined by time of day. The American journal of physiology. 1997;273:R1612–R1622. doi: 10.1152/ajpregu.1997.273.5.R1612. [DOI] [PubMed] [Google Scholar]
- 49.Deak T, Meriwether JL, Fleshner M, Spencer RL, Abouhamze A, et al. Evidence that brief stress may induce the acute phase response in rats. The American journal of physiology. 1997;273:R1998–R2004. doi: 10.1152/ajpregu.1997.273.6.R1998. [DOI] [PubMed] [Google Scholar]
- 50.Yamamoto T, Nakahata Y, Tanaka M, Yoshida M, Soma H, et al. Acute physical stress elevates mouse period1 mRNA expression in mouse peripheral tissues via a glucocorticoid-responsive element. The Journal of biological chemistry. 2005;280:42036–42043. doi: 10.1074/jbc.M509600200. [DOI] [PubMed] [Google Scholar]
- 51.Takahashi S, Yokota S, Hara R, Kobayashi T, Akiyama M, et al. Physical and inflammatory stressors elevate circadian clock gene mPer1 mRNA levels in the paraventricular nucleus of the mouse. Endocrinology. 2001;142:4910–4917. doi: 10.1210/endo.142.11.8487. [DOI] [PubMed] [Google Scholar]
- 52.Balsalobre A, Brown SA, Marcacci L, Tronche F, Kellendonk C, et al. Resetting of circadian time in peripheral tissues by glucocorticoid signaling. Science. 2000;289:2344–2347. doi: 10.1126/science.289.5488.2344. [DOI] [PubMed] [Google Scholar]
- 53.Pezuk P, Mohawk JA, Wang LA, Menaker M. Glucocorticoids as entraining signals for peripheral circadian oscillators. Endocrinology. 2012;153:4775–4783. doi: 10.1210/en.2012-1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kennedy SL, Nickerson M, Campisi J, Johnson JD, Smith TP, et al. Splenic norepinephrine depletion following acute stress suppresses in vivo antibody response. Journal of neuroimmunology. 2005;165:150–160. doi: 10.1016/j.jneuroim.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 55.Helmreich DL, Watkins LR, Deak T, Maier SF, Akil H, et al. The effect of stressor controllability on stress-induced neuropeptide mRNA expression within the paraventricular nucleus of the hypothalamus. Journal of neuroendocrinology. 1999;11:121–128. doi: 10.1046/j.1365-2826.1999.00300.x. [DOI] [PubMed] [Google Scholar]
- 56.Amat J, Paul E, Watkins LR, Maier SF. Activation of the ventral medial prefrontal cortex during an uncontrollable stressor reproduces both the immediate and long-term protective effects of behavioral control. Neuroscience. 2008;154:1178–1186. doi: 10.1016/j.neuroscience.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wager TD, Waugh CE, Lindquist M, Noll DC, Fredrickson BL, et al. Brain mediators of cardiovascular responses to social threat: part I: Reciprocal dorsal and ventral sub-regions of the medial prefrontal cortex and heart-rate reactivity. NeuroImage. 2009;47:821–835. doi: 10.1016/j.neuroimage.2009.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buchanan TW, Driscoll D, Mowrer SM, Sollers JJ, 3rd, Thayer JF, et al. Medial prefrontal cortex damage affects physiological and psychological stress responses differently in men and women. Psychoneuroendocrinology. 2010;35:56–66. doi: 10.1016/j.psyneuen.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Muller Ribeiro FC, Zaretsky DV, Zaretskaia MV, Santos RA, Dimicco JA, et al. Contribution of infralimbic cortex in the cardiovascular response to acute stress. American journal of physiology Regulatory, integrative and comparative physiology. 2012 doi: 10.1152/ajpregu.00573.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tavares RF, Correa FM, Resstel LB. Opposite role of infralimbic and prelimbic cortex in the tachycardiac response evoked by acute restraint stress in rats. Journal of neuroscience research. 2009;87:2601–2607. doi: 10.1002/jnr.22070. [DOI] [PubMed] [Google Scholar]
- 61.Hilton SM. The defence-arousal system and its relevance for circulatory and respiratory control. The Journal of experimental biology. 1982;100:159–174. doi: 10.1242/jeb.100.1.159. [DOI] [PubMed] [Google Scholar]
- 62.Nosaka S. Modifications of arterial baroreflexes: obligatory roles in cardiovascular regulation in stress and poststress recovery. Jpn J Physiol. 1996;46:271–288. doi: 10.2170/jjphysiol.46.271. [DOI] [PubMed] [Google Scholar]
- 63.Resstel LB, Fernandes KB, Correa FM. Medial prefrontal cortex modulation of the baroreflex parasympathetic component in the rat. Brain research. 2004;1015:136–144. doi: 10.1016/j.brainres.2004.04.065. [DOI] [PubMed] [Google Scholar]
- 64.Ongur D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cerebral cortex. 2000;10:206–219. doi: 10.1093/cercor/10.3.206. [DOI] [PubMed] [Google Scholar]
- 65.Ray JP, Price JL. The organization of the thalamocortical connections of the mediodorsal thalamic nucleus in the rat, related to the ventral forebrain-prefrontal cortex topography. The Journal of comparative neurology. 1992;323:167–197. doi: 10.1002/cne.903230204. [DOI] [PubMed] [Google Scholar]
- 66.Vertes RP. Differential projections of the infralimbic and prelimbic cortex in the rat. Synapse. 2004;51:32–58. doi: 10.1002/syn.10279. [DOI] [PubMed] [Google Scholar]
- 67.Fisk GD, Wyss JM. Pressor and depressor sites are intermingled in the cingulate cortex of the rat. Brain research. 1997;754:204–212. doi: 10.1016/s0006-8993(97)00076-0. [DOI] [PubMed] [Google Scholar]
- 68.van der Kooy D, McGinty JF, Koda LY, Gerfen CR, Bloom FE. Visceral cortex: a direct connection from prefrontal cortex to the solitary nucleus in rat. Neuroscience letters. 1982;33:123–127. doi: 10.1016/0304-3940(82)90238-5. [DOI] [PubMed] [Google Scholar]
- 69.Palkovits M, Zaborszky L. Neuroanatomy of central cardiovascular control. Nucleus tractus solitarii: afferent and efferent neuronal connections in relation to the baroreceptor reflex arc. Progress in brain research. 1977;47:9–34. doi: 10.1016/S0079-6123(08)62709-0. [DOI] [PubMed] [Google Scholar]
- 70.Sylvester CM, Krout KE, Loewy AD. Suprachiasmatic nucleus projection to the medial prefrontal cortex: a viral transneuronal tracing study. Neuroscience. 2002;114:1071–1080. doi: 10.1016/s0306-4522(02)00361-5. [DOI] [PubMed] [Google Scholar]
- 71.Perez-Cruz C, Simon M, Flugge G, Fuchs E, Czeh B. Diurnal rhythm and stress regulate dendritic architecture and spine density of pyramidal neurons in the rat infralimbic cortex. Behavioural brain research. 2009;205:406–413. doi: 10.1016/j.bbr.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 72.Cooney MT, Vartiainen E, Laatikainen T, Juolevi A, Dudina A, et al. Elevated resting heart rate is an independent risk factor for cardiovascular disease in healthy men and women. American heart journal. 2010;159:612–619. e613. doi: 10.1016/j.ahj.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 73.Heusch G. Heart rate and heart failure. Not a simple relationship. Circulation journal : official journal of the Japanese Circulation Society. 2011;75:229–236. doi: 10.1253/circj.cj-10-0925. [DOI] [PubMed] [Google Scholar]