Abstract
Hierarchical models of psychopathology based on substantial numbers of lifetime diagnostic categories have not been sufficiently evaluated, even though such models have relevance for theories of disorder etiology, course, or prognosis. In this research, a hierarchical component model of 16 Axis I disorders is derived, and model elements are evaluated in terms of their ability to demonstrate distinct associations with several clinically–relevant variables. Participants were 816 randomly selected adolescents from the community who were repeatedly assessed for psychiatric disorders and associated risk and protective factors over a 14-year period. First-degree relatives were also interviewed to establish their lifetime psychiatric history. Patterns of lifetime comorbidity among 16 psychiatric disorders were described at five levels of organization. In addition to the broadest level that accounted for the most variance in disorder covariation, evidence was obtained at successive levels in the hierarchy for internalizing and externalizing broad–band domains that could be subdivided into more refined clusters. The validity and potential utility of the resultant hierarchical model was further supported by distinct associations that components at each level had with exposure to childhood adversities, psychiatric disorders among first–degree relatives, and psychosocial functioning at ~ age 30. A large number of DSM Axis I disorders can be described within broad–band internalizing and externalizing domains, and further differentiation within these domains is possible and likely useful for some purposes. Implications of this research for conceptualizing relations among psychiatric disorders are discussed.
Keywords: Internalizing disorders, externalizing disorders, hierarchical organization, familial risk, mental health care utilization, psychosocial functioning
Multivariate research on the organization of various indicators of psychopathology, including disorder symptoms [e.g., 1–2], diagnostic categories [e.g., 3–5], and genetic risk [6], has frequently identified two higher-order factors, internalizing and externalizing. Support for this basic organizing structure has been upheld when symptoms or diagnostic categories associated with Axis I and Axis II are jointly considered, although additional higher-order latent factors [7–8] or genetic risk factors [9] have also been identified. Other related research indicates that internalizing and externalizing domains are typically correlated when defined by phenotypic features [4, 10] or genetic risk factors [6, 9], with a substantial portion of the covariation between internalizing and externalizing spectrum disorders accounted for by neuroticism or negative emotion [4, 10].
Beyond the superordinate domains of neuroticism, internalizing, and externalizing, controversy persists as to the organization of psychiatric disorders at lower levels in the hierarchy. Internalizing psychopathology has been successfully modeled as a single factor [3, 11], or as a hierarchical domain with two lower-order factors, often labeled distress (major depression, dysthymia, generalized anxiety disorder) and fear (panic disorder, animal phobia, situational phobia) [4, 12]. Other research, however, indicates that single– and two–factor internalizing models fit the data about equally well [13], and that the fear/distress distinction may not be statistically optimal relative to alternative models [3, 13].
Similar controversy persists as to the most accurate model for representing hierarchical relations among externalizing psychiatric disorders. Several studies have successfully modeled a single externalizing latent factor not further subdivided [e.g., 14–15], while other research based on personality features, clinical symptoms, or psychiatric disorders has frequently produced outcomes that suggest multidimensionality within the externalizing domain [16–18]. There are, for example, indications that attention deficit/hyperactivity disorder and oppositional defiant disorder or their associated features are highly related and distinguishable from conduct disorder, antisocial behavior, and substance use disorders, which are also highly related [2, 19].
In separate reports with the Oregon Adolescent Depression Project (OADP) sample, we used confirmatory factor analytic methods to evaluate the validity of competing measurement models of internalizing [20] and externalizing [21] disorders. In the present report, we utilize lifetime diagnostic data from the OADP sample to examine the hierarchical structure of 16 common lifetime Axis I psychiatric disorders. Included among these are two disorders not well–researched with respect to internalizing or externalizing domain membership, bipolar spectrum disorders and bulimia nervosa. Cross-sectional and patient-based research has suggested that bipolar disorders demonstrate greater associations with the internalizing than externalizing domain [3, 12]. Anorexia and bulimia nervosa, when treated as observed indicators of a latent eating pathology factor, have been most accurately represented as an indicator of a higher-order internalizing factor [22].
The present study is an investigation of the hierarchical associations among 16 common lifetime psychiatric disorders. In contrast with similar studies that have used confirmatory methods to evaluate the feasibility of a hypothesized measurement model, we use a novel methodological approach, top-down exploratory principal components analysis, to reveal the component structures of these disorders within a single, integrated model that organizes disorder clusters from most broad to progressively more refined. To evaluate the discriminant validity and potential utility associated with the hierarchically arranged disorder clusters, we also comparatively evaluate correlates of component scores at each level in the hierarchy with several clinically relevant variables.
METHOD
Study procedures were reviewed and approved by an institutional review board before data were collected. Adults and youth younger than age 18 provided written consent or assent, respectively, after procedures had been fully explained.
Probands
The OADP is a community-based and multi-generational longitudinal study that has been thoroughly described in earlier publications [20, 23]. Briefly, four diagnostic assessments were conducted with randomly selected youth from 9 high schools at ~ ages 16 (T1) 17 (T2), 24 (T3), and 30 (T4). At T3, a stratified sampling procedure was implemented whereby all persons with a positive psychiatric history by T2 and a randomly selected subgroup of persons without any history of mental disorder by T2 were recruited. To enhance the ethnic diversity of the sample, all non-Caucasian T2 participants were recruited for T3 regardless of lifetime diagnostic history. From T1 to T2, T2 to T3, and T3 to T4, retention rates for eligible participants were 88%, 85%, and 87%, respectively. Although attrition over assessment waves was relatively small, it slightly but significantly favored individuals from lower socioeconomic groups or with externalizing disorders [24].
A total of 816 participants completed T4, and these persons constitute the reference sample for the present research. Most participants were women (59%), Caucasian (89%), and currently married (53%). A minority (41%) reported having earned a bachelor’s or higher degree.
Assessment of Psychiatric Disorders among Probands and First-Degree Relatives
Disorder assessment of probands during the first three waves was performed with the Present Episode and Epidemiologic versions of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS) [25–26]. At T4, the Structured Clinical Interview for Axis I DSM-IV Disorders–Non-Patient Edition (SCID-NP) [27] was used for diagnostic assessments. These diagnostic interviews were supplemented with the Longitudinal Interval Follow-Up Evaluation [28] to assess disorder presence and course since the previous assessment. Symptom reports were evaluated in conjunction with DSM-III-R diagnostic criteria and decision rules at T1 and T2 and DSM-IV criteria and rules at T3 and T4.
Only disorders that had sufficient weighted lifetime prevalence rates through age 30.0 (> 1%) [14–15] were retained for analysis. These disorders, along with their associated unweighted and weighted lifetime prevalence rates through T4, respectively, were: major depressive disorder (MDD; 58.5, 50.8), dysthymia (DYS; 5.6, 4.1), bipolar spectrum disorders (BIP, inclusive of bipolar I, bipolar II, and cyclothymic disorders; 3.7, 3.1), post–traumatic stress disorder (PTSD; 8.6, 7.0), generalized anxiety disorder (GAD; 2.2, 2.0), specific phobia (PHOB; 4.3, 3.3), social phobia (SOC; 4.4, 3.6), panic disorder (PAN; 6.6, 5.6), separation anxiety disorder (SAD; 5.4, 3.9), bulimia nervosa (BN; 2.5, 1.8), attention deficit/hyperactivity disorder (ADHD; 3.2, 2.3), oppositional defiant disorder (ODD; 3.4, 2.6), conduct disorder (CD; 5.0, 3.8), alcohol use disorders (AUD, which includes alcohol abuse or dependence diagnoses; 37.0, 34.2), cannabis use disorders (CUD, which includes cannabis abuse or dependence diagnoses; 21.2, 19.1), and hard drug use disorders (DRG, which includes the abuse or dependence of substances other than cannabis and alcohol; 13.7, 11.0).
Randomly selected taped interviews from each wave were used to evaluate inter-rater reliability (T1 = 263, T2 = 162, T3 = 190, T4 = 124), with mean kappa (κ) coefficients computed for disorders diagnosed as present at least 10 times between the two raters within waves. For disorders that met this minimal threshold, agreement among raters was generally good to excellent (range of κ = .56 to .89 for 15 separate diagnostic categories; median κ = .77).
Around T3, first-degree relatives of probands were evaluated for current and lifetime psychiatric disorders, with all interviews conducted blind to proband diagnoses. At least two sources of diagnostic data were collected for each family member. Direct interviews were conducted with the SCID-NP for adult relatives and the K-SADS modified for DSM-IV for adolescent relatives aged 14–18 years. Informant interviews were conducted with other family members based on the Family Informant Schedule and Criteria modified for DSM-IV [29]. The best estimate method [30] was used for determining lifetime psychiatric diagnoses among family members.
For the 816 probands, diagnostic data were available for 732 (89.7%) proband families (730 biological mothers, 719 biological fathers, 476 female siblings, and 489 male siblings). Kappa coefficients for pairs of evaluators were excellent for all diagnostic categories that had a weighted family density > .01 in the sample: any anxiety disorder (κ = .93), mood disorder (κ = .91), substance use disorder (κ = .97), or disruptive behavior disorder (ADHD and CD only, κ = .87).
Proband Exposure to Childhood Adversities
Exposure to childhood adversities was retrospectively assessed by the Sexual Abuse subscale (α = .96) of the Childhood Trauma Questionnaire [31] and by two Assessing Environments III questionnaire scales [32] administered at T3: Negative Family Atmosphere (α = .78) and Physical Punishment/Abuse (α = .71).
Proband Psychosocial Functioning at T4
Several indicators of psychosocial functioning were assessed at T4. Topics included annual household income, number of weeks unemployed during the last year, history of divorce or separation, relationship quality with family (assessed by the Perceived Social Support from Family scale [33], α = .90), level of social adjustment (assessed by the Social Adjustment Scale [34], α = .70, higher scores indicate poorer adjustment), self-reported suicide attempt since T3, and the DSM-IV Global Assessment of Functioning scale.
Statistical Analyses
Participant weighting
Because of the stratified sampling procedure implemented at T3, Caucasian participants with no lifetime diagnosis by T2 were assigned a weight that reflected the probability of this subgroup being sampled during T3 and T4 assessments. Unless otherwise specified, all findings subsequently presented are based on weighted data.
“Top-down” component analyses
Goldberg [35] has outlined a procedure for revealing the hierarchical structure of a set of variables based on exploratory factor analytic (EFA) methods. In most applications of EFA, a “bottom-up” procedure is used whereby some number of lower-order factors is extracted based on covariation patterns among variables within a set. Rotating factors until some form of simple structure is achieved can, in turn, illuminate higher-order factors. In contrast to this traditional approach, Goldberg proposed a process that starts with the highest-order factor, followed by a series of sequential analyses that reveal successively lower-order factors in the hierarchy. This approach was used in the present study to reveal levels of the component hierarchy that characterize lifetime associations among common Axis I psychiatric disorders.
The first step in the “top-down” analyses involved the computation of the tetrachoric correlation matrix, which is the preferred correlation matrix when factoring dichotomous variables [36] and the commonly used input matrix in factor analyses of diagnostic categories [e.g., 37]. The next step was to extract the first unrotated principal component (FUPC), or the largest possible component, from the correlation matrix. To produce a two-component solution, the same correlation matrix used to derive the FUPC was inputted, and a two-component solution requested based on principal component extraction and varimax (orthogonal) rotation. This process of extraction and rotation was continued to reveal the structure for a number of components, with each successive analysis revealing lower-order components in the hierarchy. Given the emphasis in the present research on lifetime patterns of comorbidity, the stopping point for this process occurred at the level just before components began to be defined by single disorders.
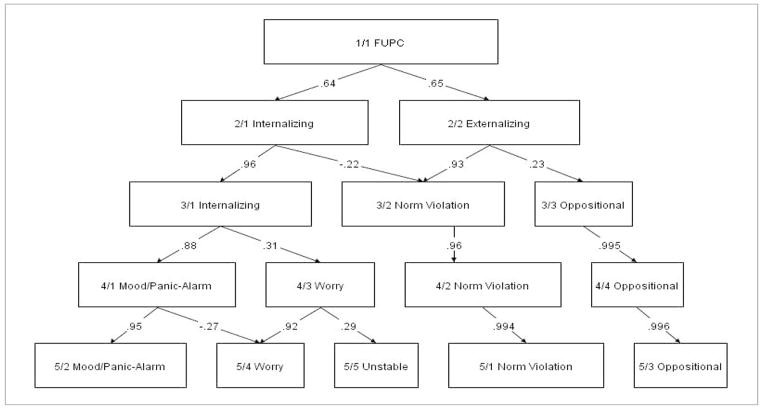
During each component analysis, component scores were computed and saved. To compute principal component scores, standardized diagnostic variables were multiplied by their corresponding principal component score coefficients with the resulting products summed. To display the hierarchical representation of psychopathology at successive levels (Figure 1), component scores derived at each level were correlated with those at the level immediately below, with the resulting correlations serving as a type of path coefficient used to index associations among components at adjoining levels in the hierarchy. Components are illustrated as rectangular boxes and sized according to the proportion of variance they accounted for at each level.
Figure 1.
Hierarchical Structure of 16 Lifetime Axis I Psychiatric Disorders
Notes: FUPC = First unrotated principal component. Rectangular boxes along rows (horizontal organization) are sized according to the proportion of variance each component explains among variables included within the same level of analysis. When correlations between component scores at adjoining levels (vertical organization) equaled or exceeded ± .20, pathways and their corresponding correlations are displayed, with each significant at p < .001.
Component scores were also used in the computation of correlations with clinically relevant variables not included in component analysis. In these analyses, participants’ positions on a given component, as indexed by their individual component scores, were correlated with scores on these additional variables so as to evaluate the discriminant validity and potential utility of the various levels of the resultant hierarchical model. Fisher r-to-z procedures were used to evaluate the statistical significance of magnitude differences among pairs of correlations.
RESULTS
Hierarchical Associations of 16 Lifetime Psychiatric Disorders
Component loadings associated with the extraction and rotation process for the first 5 levels from the “top–down” EFA are presented in Table 1, and a corresponding diagram of the hierarchical associations among components is presented in Figure 1. The first 5 component extractions are emphasized because beginning with Level 6, components began to be defined by single disorders. Eigenvalues for the first 5 components (and corresponding percentage of variance explained by each component) are: 4.53 (28.3), 2.58 (16.1), 1.43 (8.9), 1.38 (8.6), and 1.13 (7.1).
Table 1.
Top-Down Principal Component Analysis: Psychiatric Disorder Component Loadings for Each Level in the Hierarchy
| Level in hierarchy | Component loadings | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDD | DYS | BIP | PTSD | PAN | SAD | GAD | SOC | PHOB | BN | AUD | CUD | DRG | CD | ODD | ADHD | |
| Level 1: | ||||||||||||||||
| 1/1 | .67 | .48 | .50 | .56 | .57 | .39 | .45 | .59 | .47 | .53 | .58 | .62 | .72 | .42 | .43 | .38 |
| Level 2: | ||||||||||||||||
| 2/1 | .74 | .67 | .40 | .69 | .74 | .63 | .35 | .49 | .57 | .46 | .08 | .06 | .20 | −.20 | .15 | .13 |
| 2/2 | .20 | −.01 | .31 | .08 | .04 | −.09 | .28 | .34 | .08 | .28 | .76 | .84 | .84 | .83 | .47 | .41 |
| Level 3: | ||||||||||||||||
| 3/1 | .76 | .69 | .39 | .73 | .74 | .59 | .40 | .45 | .42 | .46 | .15 | .13 | .23 | −.20 | .04 | −.03 |
| 3/2 | .18 | −.02 | .26 | .10 | .01 | −.17 | .31 | .23 | −.15 | .23 | .80 | .87 | .81 | .79 | .27 | .15 |
| 3/3 | .08 | −.01 | .18 | −.06 | .08 | .20 | −.04 | .34 | .67 | .18 | .01 | .05 | .22 | .26 | .64 | .82 |
| Level 4: | ||||||||||||||||
| 4/1 | .74 | .87 | .19 | .66 | .68 | .64 | .10 | .13 | .35 | .39 | .07 | .10 | .19 | −.14 | .11 | −.04 |
| 4/2 | .19 | .10 | .16 | .07 | −.01 | −.13 | .15 | .07 | −.17 | .21 | .77 | .87 | .81 | .83 | .33 | .16 |
| 4/3 | .23 | −.21 | .55 | .32 | .29 | .03 | .73 | .82 | .28 | .27 | .26 | .15 | .21 | −.09 | −.06 | .10 |
| 4/4 | .06 | .02 | .12 | −.09 | .06 | .21 | −.12 | .26 | .65 | .15 | −.02 | .02 | .19 | .25 | .65 | .81 |
| Level 5: | ||||||||||||||||
| 5/1 | .21 | .07 | .13 | .07 | .00 | −.08 | .19 | .10 | −.18 | .15 | .77 | .87 | .82 | .82 | .32 | .17 |
| 5/2 | .77 | .77 | .07 | .64 | .68 | .75 | .19 | .17 | .30 | .23 | .08 | .10 | .21 | −.17 | .09 | −.03 |
| 5/3 | .08 | .01 | .09 | −.08 | .07 | .25 | −.09 | .27 | .64 | .11 | −.01 | .03 | .21 | .25 | .65 | .82 |
| 5/4 | .19 | −.39 | .32 | .20 | .21 | .12 | .75 | .77 | .16 | −.02 | .22 | .10 | .18 | −.14 | −.10 | .10 |
| 5/5 | .06 | .34 | .69 | .30 | .22 | −.31 | .05 | .24 | .34 | .76 | .11 | .10 | .05 | .07 | .05 | −.01 |
Notes: The highest loading at each level of analysis is bolded for each disorder category. MDD = major depressive disorder, DYS = dysthymia, BIP = bipolar spectrum disorders (i.e., bipolar I, bipolar II, or cyclothymia), PTSD = post–traumatic stress disorder, PAN = panic disorder, SAD = separation anxiety disorder, GAD = generalized anxiety disorder, SOC = social phobia, PHOB = specific phobia, BN = bulimia nervosa, AUD = alcohol use disorder, CUD = cannabis use disorder, DRG = hard drug use disorder, CD = conduct disorder, ODD = oppositional defiant disorder, ADHD = attention deficit/hyperactivity disorder.
Common level
Level 1/1 in Table 1 and Figure 1 corresponds to the FUPC, which represents common variance shared among the disorders included in this analysis. Component loadings indicate that the lifetime histories of each disorder contributed positively and at least moderately to the definition of the FUPC.
Broad–band level
The two-component solution (Level 2) corresponds to the familiar internalizing (2/1) and externalizing (2/2) domains of psychopathology. The disorders that contributed the most to the definition of the internalizing component, as evident in component loadings ≥ .60, were MDD, PAN, PTSD, DYS, and SAD. For the externalizing component, the corresponding disorders with the highest loadings were CUD, DRG, CD, and AUD.
Narrow–band levels
Lower levels in the hierarchy (Levels 3–5) represent successive refinements of the two broad–band domains. At Level 3, the internalizing domain is largely preserved and the externalizing domain is split into two clusters, social norm violation disorders (3/2: CD, AUD, CUD, DRG) and oppositional behavior disorders (3/3: ADHD, ODD) together with PHOB. PHOB also demonstrated a moderate cross–loading with the internalizing component at this level. Although we use the term “oppositional” in Figure 1 and elsewhere as a descriptive label for the lower-level components to which ADHD, ODD, and PHOB are the most significant contributors, we do so in recognition that this label might more accurately apply to ADHD and ODD and have less relevance for PHOB.
The broad-band internalizing domain splits at Level 4 into two clusters, mood/panic-alarm disorders (4/1: MDD, DYS, PTSD, PAN, BN, SAD) and disorders commonly characterized by excessive worry (4/3: GAD, SOC) together with BIP. The mood/panic-alarm component, subsequently abbreviated as mood/alarm, is defined by disorders where depressed mood is a core feature (MDD, DYS) as well as other disorders where panic or alarm responses are triggered by specific cues (e.g., interoceptive cues in the case of PAN, trauma-related cues in PTSD, separation events from caretakers in SAD, feelings of fullness in BN) that, in turn, increase the likelihood of accompanying avoidance or escape behavior. The worry component is defined by disorders characterized by excessive worry and rumination (related to performance or social situations in the case of SOC and apprehensive expectations associated with several events or activities in the case of GAD).
At Level 5, the mood/alarm component is preserved (5/2), excepting BN, which combines with BIP to form a new component, unstable self-regulation (5/5). Both disorder categories that contribute to this component include features associated with shifting mood states and episodic loss of self-control. GAD and SOC (5/4) continue to define a component primarily characterized by worry.
Associations of Component Loadings with Clinically-Relevant Variables
Childhood adversities
Table 2 presents correlations for component scores at each level in the hierarchy with various forms of childhood adversity. The FUPC (1/1) was significantly and positively associated with each form of childhood adversity. At Levels 2 and 3, childhood sexual abuse was significantly and more strongly associated with internalizing disorders (2/1, 3/1) than externalizing disorders (2/2, 3/2, 3/3). At Levels 4 and 5, physical abuse was more strongly associated with norm violation externalizing clusters (4/2, 5/1) when compared to several internalizing clusters (4/1, 5/2, 5/4, 5/5).
Table 2.
Correlations of Component Scores at Each Level in the Hierarchy with Childhood Adversity Exposure
| Level in hierarchy | Childhood Adversities
|
||
|---|---|---|---|
| Negative Family Atmosphere | Physical Punishment/Abuse | Sexual Abuse | |
| Level 1: | |||
| 1/1 (FUPC) | .33** | .26** | .32** |
| Level 2: | |||
| 2/1 (INT) | .22**a | .13*a | .28**a |
| 2/2 (EXT) | .22**a | .22**a | .14**b |
| Level 3: | |||
| 3/1 (INT) | .22**a | .14**ab | .29**a |
| 3/2 (EXT NV) | .19**a | .21**a | .13**b |
| 3/3 (EXT Opp) | .08b | .04b | .03b |
| Level 4: | |||
| 4/1 (INT M/P-A) | .20**a | .10*a | .25**a |
| 4/2 (EXT NV) | .19**ac | .20**bc | .12*b |
| 4/3 (INT Worry) | .09bc | .10*ac | .11*b |
| 4/4 (EXT Opp) | .07b | .02a | .02b |
| Level 5: | |||
| 5/1 (EXT NV) | .19**a | .20**a | .12*ac |
| 5/2 (INT M/P-A) | .17**a | .09b | .22**b |
| 5/3 (EXT Opp) | .06b | .03b | .02c |
| 5/4 (INT Worry) | .03b | .07b | .05ac |
| 5/5 (INT Unstable) | .12*ab | .07b | .13*ab |
Notes: Because of the number of computations associated with this and subsequent tables, only correlations significantly different from zero at p < .01 are denoted. Correlations that significantly differ (p < .05) from one another at the same level in the hierarchy for a given column variable are distinguished with different superscripts. FUPC = First unrotated principal component; INT = Internalizing; EXT = Externalizing; NV = Norm Violation; Opp = Oppositional; M/P-A = Mood/Panic-Alarm.
p < .01,
p < .001.
Within the internalizing clusters at lower level in the hierarchy, mood/alarm disorders (4/1, 5/2) were more strongly associated with negative family atmosphere and sexual abuse than the worry components (4/3, 5/4). Within lower level externalizing clusters, physical abuse was more strongly associated with the norm violation components (4/2, 5/1) than the oppositional components (4/4, 5/3).
Psychiatric disorders among first-degree relatives
Table 3 displays correlations of component scores with family densities of psychiatric disorders. The FUPC (1/1) was significantly associated with both broad–band (i.e., all internalizing or externalizing disorders) and domain specific representations (anxiety, mood, substance use, disruptive behavior disorder categories) of family disorder densities. At lower levels in the hierarchy, homotypic disorder associations between probands and first-degree relatives are of particular interest, and are evident when a class of related disorders (e.g., mood disorders) among probands constitutes an increased risk for the same class of disorders among first–degree relatives.
Table 3.
Correlations of Component Scores at Each Level in the Hierarchy with Psychiatric Disorder Densities among First-Degree Relatives
| Level in Hierarchy | Psychiatric Disorder Densities among First-Degree Relatives
|
|||||
|---|---|---|---|---|---|---|
| Anxiety disorders | Mood disorders | All Internalizing | Substance use disorders | Disruptive behavior disorders | All Externalizing | |
| Level 1: | ||||||
| 1/1 (FUPC) | .16** | .24** | .24** | .25** | .14** | .25** |
| Level 2: | ||||||
| 2/1 (INT) | .17**a | .20**a | .21**a | .11*a | .07a | .13**a |
| 2/2 (EXT) | .04b | .11*a | .11**a | .21**a | .11*a | .20**a |
| Level 3: | ||||||
| 3/1 (INT) | .15**a | .19**a | .20**a | .13*ab | .05a | .14**ab |
| 3/2 (EXT NV) | .01b | .09ab | .08ab | .20**b | .08a | .19**b |
| 3/3 (EXT Opp) | .09ab | .07b | .06b | .04a | .10*a | .04a |
| Level 4: | ||||||
| 4/1 (INT M/P-A) | .11*a | .16**a | .18**a | .13**ab | .03a | .13**ab |
| 4/2 (EXT NV) | −.01b | .08a | .08a | .20**a | .07a | .19**a |
| 4/3 (INT Worry) | .11*a | .09a | .08a | .04b | .07a | .05b |
| 4/4 (EXT Opp) | .08ab | .06a | .05a | .03b | .09a | .04b |
| Level 5: | ||||||
| 5/1 (EXT NV) | .00a | .08a | .08a | .21**a | .07a | .20**a |
| 5/2 (INT M/P-A) | .11*b | .14**a | .16**a | .13*ab | .04a | .13**ab |
| 5/3 (EXT Opp) | .08ab | .06a | .05a | .04bc | .09a | .04bc |
| 5/4 (INT Worry) | .09ab | .04a | .04a | .03bc | .07a | .04bc |
| 5/5 (INT Unstable) | .04ab | .10*a | .09a | −.01c | .00a | .00c |
Notes: Correlations that significantly differ at p < .05 at the same level in the hierarchy for a given column variable are denoted by different superscripts. “All Internalizing” and “All Externalizing,” respectively, denote family density values for all lifetime DSM-defined anxiety and mood disorders and all substance use and disruptive behavior disorders assessed among family members. FUPC = First unrotated principal component; INT = Internalizing; EXT = Externalizing; NV = Norm Violation; Opp = Oppositional; M/P-A = Mood/Panic-Alarm.
p < .01,
p < .001.
In Levels 2–5, the broad proband internalizing component (2/1, 3/1) and the more refined mood/alarm component at lower levels (4/1, 5/2) demonstrated the largest absolute associations with family densities of anxiety, mood, and all internalizing disorders. Because of large confidence intervals around these correlations, however, statistical contrasts of correlation values within the same levels of the hierarchy revealed no statistically significant differences between these and other refined internalizing components (worry, unstable self-regulation) at lower levels of the hierarchy, and only a limited number of significant contrasts with externalizing components across the full range of the hierarchy. When statistically significant differences in correlations were noted at lower levels of the hierarchy, these occurred for contrasts that involved the mood/alarm internalizing components (4/1, 5/2) and the norm violation externalizing components (4/2, 5/1) for anxiety disorder densities in first-degree relatives.
In the right half of Table 3, component score correlations with family densities of substance use, disruptive behavior, and all externalizing disorders are presented. For proband Levels 2–5, the broad externalizing component (2/2) or more refined externalizing components lower in the hierarchy demonstrated the largest absolute correlations with family densities of these disorder categories. Many of the statistical contrasts conducted within the same level of the hierarchy, however, did not reach statistical significance. When significant differences were noted, these generally occurred for family substance use disorder densities. In these instances, correlations that indexed associations between family substance use disorders and proband norm violation externalizing components (3/2, 4/2, 5/1) were significantly larger than those associated with the oppositional behavior externalizing components (3/3, 4/4, 5/3).
Psychosocial functioning at T4
Component score correlations with psychosocial functioning indicators are displayed in Table 4. The FUPC (1/1) was significantly associated with each of the impairment indicators in the direction of greater impairment. Beginning with Level 2, externalizing psychopathology (2/2) when compared to internalizing psychopathology (2/1) was significantly and more strongly associated with decreased income and impaired relationship quality. Conversely, social adjustment was comparatively poorer for those with internalizing psychopathology (2/1), particularly with the mood/alarm internalizing components at lower levels in the hierarchy (4/1, 5/2).
Table 4.
Correlations of Component Scores at Each Level in the Hierarchy with Psychosocial Functioning Indicators Assessed at T4
| Level in hierarchy | T4 (~ Age 30) Psychosocial Functioning Indicators
|
||||||
|---|---|---|---|---|---|---|---|
| Unemployment | Household income | Divorced/ separated | Relationship quality | Suicide attempt since T3 | Social adjustment | Global functioning | |
| Level 1: | |||||||
| 1/1 (FUPC) | .20** | −.28** | .20** | −.20** | .33** | .29** | −.43** |
| Level 2: | |||||||
| 2/1 (INT) | .18**a | −.11*a | .16**a | −.07a | .25**a | .25**a | −.27**a |
| 2/2 (EXT) | .08a | −.24**b | .10*a | −.19**b | .18**a | .13**b | −.29**a |
| Level 3: | |||||||
| 3/1 (INT) | .17**a | −.12*a | .16**a | −.06a | .24**a | .24**a | −.28**a |
| 3/2 (EXT NV) | .06b | −.23**b | .09*ab | −.16**a | .16**ab | .10*b | −.27**a |
| 3/3 (EXT Opp) | .06b | −.04a | .02b | −.08a | .08b | .07b | −.05b |
| Level 4: | |||||||
| 4/1 (INT M/P-A) | .16**a | −.15**a | .12*a | −.05a | .18**a | .23**a | −.20**a |
| 4/2 (EXT NV) | .07ab | −.25**b | .08ab | −.16**b | .14**ab | .11**b | −.24**a |
| 4/3 (INT Worry) | .05b | .02c | .10*ab | −.05a | .15**ab | .06b | −.22**a |
| 4/4 (EXT Opp) | .05b | −.04c | .01b | −.08ab | .06b | .07b | −.03b |
| Level 5: | |||||||
| 5/1 (EXT NV) | .06ab | −.25**a | .08ab | −.15**a | .14**ab | .10*a | −.24**a |
| 5/2 (INT M/P-A) | .13**a | −.14**b | .12*a | −.02bc | .17**a | .21**b | −.19**ac |
| 5/3 (EXT Opp) | .05ab | −.04bc | .01b | −.07abc | .06b | .07a | −.03b |
| 5/4 (INT Worry) | .00b | .03c | .07ab | .00c | .11*ab | .02a | −.16**ac |
| 5/5 (INT Unstable) | .10*ab | −.02c | .07ab | −.12*ab | .10*ab | .09a | −.12**bc |
Notes: Correlations that significantly differ at p < .05 at the same level in the hierarchy for a given column variable are denoted by different superscripts. FUPC = First unrotated principal component; INT = Internalizing; EXT = Externalizing; NV = Norm Violation; Opp = Oppositional; M/P-A = Mood/Panic-Alarm.
p < .01,
p < .001.
DISCUSSION
The main objective of this research was to evaluate the hierarchical associations of 16 lifetime psychiatric disorders in a prospective sample, and to investigate the discriminant validity of the resultant components at different levels in the hierarchy by evaluations of their associations with several clinically relevant variables. In conjunction with these aims, hierarchical associations among disorder constructs were described at (a) a common level, within which all 16 disorder concepts demonstrated significant shared variability; (b) a broad-band level, which corresponded to the distinction between internalizing and externalizing forms of psychopathology; and (c) three narrow-band levels that involved further refinement of internalizing and externalizing broad-band domains. Component correlations with childhood adversities and family densities of psychiatric disorder domains within various levels of the hierarchy frequently indicated different patterns of associations with these external variables, providing support for the discriminant validity of more refined elements within the hierarchical model. Overall, findings from the present research suggest that an exclusive focus on one level of the hierarchy may negate important information or distinctions that emerge at successively lower levels, a consequence of which may be an incomplete or limited conceptualization of the underlying structure of common lifetime Axis I disorders.
In addition to these general observations, several specific findings warrant comment. At broad- and narrow-band levels, and consistent with findings previously noted in the literature [e.g., 3, 22], both BIP and BN were primarily aligned the internalizing domain. Within the internalizing domain, however, we did not find evidence for the “distress” and “fear” clusters that are sometimes observed when confirmatory factor analytic methods are used [4,12]. In our earlier research restricted to the structural organization of internalizing disorders with this data set [20], we reported that the distress/fear two-factor hierarchical model fit the data well when subjected to confirmatory factor analytic methods, but did not perform significantly better than two alternative models. The distress and fear internalizing subdomains have received inconsistent support other research [3, 13], a likely consequence of the substantial comorbidity among internalizing disorders [13]. In the present research, there was evidence for three distinct clusters at lower levels in the internalizing hierarchy: mood/alarm, worry, and unstable self-regulation. The robustness of the smaller internalizing clusters at lower levels, however, needs further investigation. Although worry has emerged as a dominant feature among people with bipolar spectrum disorders [38–39], for example, the reliability of the covariation of BIP with GAD and SOC observed at Level 4 in the present research requires replication.
With respect to the externalizing domain, the externalizing cluster beginning at Level 3 split into two clusters. Whereas the norm violation cluster (3/2) was strongly associated with the higher-level externalizing component (2/2), the oppositional behavior disorder cluster (3/3) demonstrated a comparatively weak association with the broad externalizing component. This finding, in need of replication, is partially consistent with recent formulations by Achenbach and colleagues [1], who place “attention problems” outside of the internalizing and externalizing domains. Additionally, and consistent with prior research [40], ADHD and ODD were more strongly related to internalizing disorders than was a component defined, in part, by CD. In the present research, ADHD and ODD associations with internalizing psychopathology were limited to their lifetime comorbidity with PHOB. ADHD and ODD covariations with PHOB but not anxiety disorders associated with panic and alarm (PAN, PTSD, SAD) or worry (GAD, SOC) warrants further investigation. Gray and McNaughton [41], for example, have argued that PHOB should not be regarded as an anxiety disorder. In support, they refer to research that indicates that PHOB is not associated with the activation of brain regions typically observed with other anxiety disorders, and note that anxiolytics have little effect in altering avoidance of feared objects related to the phobia. Other research indicates that PHOB, although generally related to other anxiety disorders in the literature, also demonstrate significant comorbidity and covariation with ADHD and ODD [37, 42, 43]. Further research is necessary to determine the extent to which the associations observed among ADHD, ODD, and PHOB at lower levels of the hierarchy in the present research are generalizable to other samples.
With regard to psychosocial functioning at T4, areas of impairment generally differed between internalizing (e.g., social adjustment) and externalizing (e.g., employment, income, relationship quality) domains. At lower levels in the hierarchy, the externalizing oppositional disorder subcomponent was unrelated to any functioning indicator, and was associated with better functioning on 6 of 7 indicators when compared with the externalizing norm violation subcomponent. Within the internalizing subcomponents, functioning in the areas of income and social adjustment was significantly more impaired for the mood/alarm cluster than the worry and unstable self-regulation clusters. Across all lower level component domains (Levels 3 through 5), the externalizing norm violation domain was characterized by the lowest household income.
A limitation of this research is that many of the disorders specified in DSM are defined by symptom sets that are multidimensional [12]. When analyses are focused at the disorder level, the multidimensionality associated with diagnostic criteria for specific disorders is ignored. More precise models of phenotypic covariations are likely to result from studies based at the symptom– rather than disorder–level of analysis.
Another potential limitation is that diagnostic decisions in the present study followed DSM hierarchical rules. Diagnostic criteria for many psychiatric disorders specified in DSM, for example, include qualifying statements such as “the disturbance is not better accounted for by another mental disorder.” For some diagnostic categories, the co-occurrence of another indicated disorder takes precedence when making differential diagnoses (e.g., an ODD diagnosis would not be made if the person also meets diagnostic criteria for CD). Similarly, within the mood disorders domain, a lifetime history of a manic, hypomanic, or mixed episode would negate a diagnosis of MDD or DYS, and instead direct consideration to the bipolar disorders. Adherence to these decision rules in the present research most certainly altered lifetime disorder comorbidity patterns among some disorder pairs, particularly within relatively short timeframes. Any such biasing effects, however, were likely offset to some degree given our emphasis on lifetime disorders as determined by multiple diagnostic assessments spanning a broad age range. To illustrate, DSM hierarchical decision rules indicate that a diagnosis of GAD should not be made if the GAD-related disturbance occurs exclusively during a mood disorder. In such instances, adherence to this rule within an episode-defined timeframe would likely result in substantially lower rates of disorder comorbidity than would be observed if this differential diagnostic rule were ignored. When lifetime disorders are considered, however, there are greater opportunities for disorders subject to such decision rules to demonstrate distinct courses with asynchronous onsets and offsets (e.g., GAD had a lifetime correlation of .49 with MDD in this study). In other instances, however, hierarchical decision rules might have a more pronounced effect that extends beyond the duration of a single episode, such as in the lifetime comorbidity rates of unipolar mood disorders (MDD, DYS) with bipolar disorders (BIP). Strict adherence to DSM decision rules would only permit lifetime comorbidity among unipolar and bipolar mood disorders when unipolar mood disorder onsets precede and are distinct from the onsets of bipolar disorders, but not vice versa. Our adherence to diagnostic decision rules, although consistent with the practice of making diagnoses within the DSM framework, likely resulted in lower rates of comorbidity for most disorder pairs (and for some pairs more so than others) than would have been observed if diagnoses were made independently of these rules. Replication of the present study’s findings is therefore necessary with a representative sample based on hierarchy-free lifetime diagnoses.
Debates concerning the modeling of psychiatric disorders have often emphasized the optimal number or representation of disorder categories. The analyses undertaken here suggest that multiple levels of breadth in the representation of the hierarchical organization of psychopathology may be valid and useful depending on the purpose for which the organizational system is used. As suggested by Lahey and colleagues [2] and supported by findings reported here, there is likely more than one valid level in the hierarchy of disorder associations, and that the utility of splitting higher-order levels into narrower-band clusters should be evaluated with reference to pertinent external validity criteria.
Acknowledgments
This research was supported by National Institute of Mental Health Grants MH40501 and MH50522 and National Institute on Drug Abuse Grant DA12951 to Peter M. Lewinsohn. The authors thank Lewis R. Goldberg for his valuable input and guidance.
Footnotes
Conflicts of interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Achenbach TM, Bernstein A, Dumenci L. DSM-oriented scales and statistically based syndromes for ages 18 to 59: Linking taxonomic paradigms to facilitate multitaxonomic approaches. J Pers Assess. 2005;84:49–63. doi: 10.1207/s15327752jpa8401_10. [DOI] [PubMed] [Google Scholar]
- 2.Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Applegate B, Garriock HA, Chapman DA, Waldman ID. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. J Abnorm Child Psychol. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Stein DJ, Zaslavsky AM, Aguilar-Gaxiola S, Alonso J, Andrade L, Benjet C, de Girolamo G, de Graaf R, Demyttenaere K, Fayyad J, Haro JM, Hu CY, Karam A, Lee S, Lepine J-P, Matchsinger H, Mihaescu-Pintia C, Posada-Villa J, Sagar R, Ustun TB. Development of lifetime comorbidity in the World Health Organization World Mental Health Surveys. Arch Gen Psychiat. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slade T, Watson D. The structure of common DSM–IV and ICD–10 mental disorders in the Australian general population. Psychol Med. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- 6.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiat. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 7.Markon KE. Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psychol Med. 2010;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- 8.Røysamb E, Kendler KS, Tambs K, Orstavik RE, Neale MC, Aggen SH, Torgersen S, Reichborn-Kjennerud T. The joint structure of DSM-IV Axis I and Axis II disorders. J Abn Psychol. 2011;120:198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. Amer J Psychiat. 2011;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. Brit J Psychiat. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- 11.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders. J Abn Psychol. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 12.Watson D. Rethinking mood and anxiety disorders: A quantitative hierarchical model for DSM-V. J Abn Psychol. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- 13.Beesdo-Baum K, Hofler M, Gloster AT, Klotsche J, Lieb R, Beauducel A, Buhner M, Kessler RC, Wittchen H-U. The structure of common mental disorders: A replication study in a community sample of adolescents and young adults. Int J Methods Psychiatr Res. 2009;18:204–220. doi: 10.1002/mpr.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krueger RF. The structure of common mental disorders. Arch Gen Psychiat. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 15.Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: The NEMESIS study. Arch Gen Psychiat. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 16.Bezdjian S, Krueger RF, Derringer J, Malone S, McGue M, Iacono WG. The structure of DSM-IV ADHD, ODD, and CD criteria in adolescent boys: a hierarchical approach. Psychiat Res. 2011;188:411–421. doi: 10.1016/j.psychres.2011.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castellanos-Ryan N, Conrod PJ. Personality correlates of the common and unique variance across conduct disorder and substance misuse symptoms in adolescence. J Abnorm Child Psychol. 2011;39:563–576. doi: 10.1007/s10802-010-9481-3. [DOI] [PubMed] [Google Scholar]
- 18.Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. J Abn Psychol. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fergusson DM, Horwood LJ, Lynskey MT. Structure of DSM-III-R criteria for disruptive childhood behaviors: Confirmatory factor models. J Amer Acad Child Adoles Psychiat. 1994;33:1145–1155. doi: 10.1097/00004583-199410000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Seeley JR, Kosty DB, Farmer RF, Lewinsohn PM. The modeling of internalizing disorders on the basis of patterns of lifetime comorbidity: Associations with psychosocial impairment and psychiatric disorders among first–degree relatives. J Abn Psychol. 2011;120:308–321. doi: 10.1037/a0022621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farmer RF, Seeley JR, Kosty DB, Lewinsohn PM. Refinements of the hierarchical structure of externalizing psychiatric disorders: Patterns of lifetime liability from mid-adolescence through early adulthood. J Abn Psychol. 2009;118:699–710. doi: 10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forbush KT, South SC, Krueger RF, Iacono WG, Clark LA, Keel PK, Legrand LN, Watson D. Locating eating pathology within an empirical diagnostic taxonomy: Evidence from a community-based sample. J Abn Psychol. 2010;119:282–292. doi: 10.1037/a0019189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abn Psychol. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 24.Rohde P, Lewinsohn PM, Seeley JR, Klein DN, Andrews JA, Small JW. Psychosocial functioning of adults who experienced substance use disorders as adolescents. Psychol Add Behav. 2007;21:155–164. doi: 10.1037/0893-164X.21.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview: Test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, present episode version. Arch Gen Psychiat. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- 26.Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J Amer Acad Child Psychiat. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- 27.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for Axis I DSM-IV disorders, Non-patient Edition. Biometrics Research Department; New York: 1994. [Google Scholar]
- 28.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott PA. The Longitudinal Interval Follow-up Evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiat. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 29.Mannuzza S, Fyer AJ. Anxiety Disorders Clinic. New York State Psychiatric Institute; New York: 1990. Family informant schedule and criteria (FISC), July 1990 revision. [Google Scholar]
- 30.Klein DN, Lewinsohn PM, Seeley JR, Rohde P. Family study of major depressive disorder in a community sample of adolescents. Arch Gen Psychiat. 2001;58:13–20. doi: 10.1001/archpsyc.58.1.13. [DOI] [PubMed] [Google Scholar]
- 31.Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report: Manual. The Psychological Corporation; San Antonio, TX: 1998. [Google Scholar]
- 32.Berger AM, Knutson JF, Mehm JG, Perkins KA. The self-report of punitive childhood experiences of young adults and adolescents. Child Ab Negl. 1988;12:251–262. doi: 10.1016/0145-2134(88)90033-6. [DOI] [PubMed] [Google Scholar]
- 33.Procidano ME, Heller K. Measures of perceived social support from friends and from family: Three validation studies. Amer J Community Psychol. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- 34.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiat. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 35.Goldberg LR. Doing is all bass-ackwards: The development of hierarchical factor structures from the top down. J Res Pers. 2006;40:347–358. [Google Scholar]
- 36.Panter AT, Swygert KA, Dahlstrom WG, Tanaka JS. Factor analytic approaches to personality item-level data. J Pers Assess. 1997;68:561–589. doi: 10.1207/s15327752jpa6803_6. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiat. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gruber J, Eidelman P, Harvey AG. Transdiagnostic emotion regulation processes in bipolar disorder and insomnia. Behav Res Ther. 2008;46:1096–1100. doi: 10.1016/j.brat.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 39.Thomas J, Knowles R, Tai S, Bentall RP. Response styles to depressed mood in bipolar affective disorder. J Affect Dis. 2006;100:249–252. doi: 10.1016/j.jad.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 40.Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. J Abn Psychol. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- 41.Gray JA, McNaughton N. The neuropsychology of anxiety. Oxford University Press; London: 2000. [Google Scholar]
- 42.Fayyad J, de Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, de Girolamo G, Haro JM, Karam EG, Lara C, Lépine J-P, Ormel J, Posada-Villa J, Zaslavsky AM, Jin R. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Brit J Psychiat. 2007;190:402–409. doi: 10.1192/bjp.bp.106.034389. [DOI] [PubMed] [Google Scholar]
- 43.Kim S-J, Kim B-N, Cho S-C, Kim J-W, Shin M-S, Yoo H-J, Kim HW. The prevalence of specific phobia and associated co-morbid features in children and adolescents (2010) J Anxiety Dis. 2010;24:629–634. doi: 10.1016/j.janxdis.2010.04.004. [DOI] [PubMed] [Google Scholar]