Abstract
Objective
To determine if automated screening and just in time delivery of testing and referral materials at the point of care promotes universal screening referral rates for maternal depression.
Methods
The Child Health Improvement through Computer Automation (CHICA) system is a decision support and electronic medical record system used in our pediatric clinics. All families of patients up to 15 months of age seen between October 2007 and July 2009 were randomized to one of three groups: (1) screening questions printed on prescreener forms (PSF) completed by mothers in the waiting room with physician alerts for positive screens, (2) everything in (1) plus ‘just in time’ (JIT) printed materials to aid physicians, and (3) a control group where physicians were simply reminded to screen on printed physician worksheets.
Results
The main outcome of interest was whether physicians suspected a diagnosis of maternal depression and referred a mother for assistance. This occurred significantly more often in both the PSF (2.4%) and JIT groups (2.4%) than in the control group (1.2%) (OR 2.06, 95% CI 1.08 to 3.93). Compared to the control group, more mothers were noted to have depressed mood in the PSF (OR 7.93, 95% CI 4.51 to 13.96) and JIT groups (OR 8.10, 95% CI 4.61 to 14.25). Similarly, compared to the control group, more mothers had signs of anhedonia in the PSF (OR 12.58, 95% CI 5.03 to 31.46) and JIT groups (OR 13.03, 95% CI 5.21 to 32.54).
Conclusions
Clinical decision support systems like CHICA can improve the screening of maternal depression.
Keywords: Maternal depression, CHICA, screening, computer decision support system, visualization of data and knowledge, data models, software engineering: architecture, agents, distributed systems, pediatrics
Background
Depression occurring in the postpartum period is the most common medical problem affecting new mothers.1–3 A comprehensive summary of studies of maternal depression found that the average prevalence is 13%.4 5 Maternal depression is concerning to pediatricians because it affects not only the mother but also her family and immediate interaction with her child; this can result in decreased use of car seats, electrical socket covers, smoke detectors, and correct infant sleep position, and in long-term health effects for the child, including poorer performance on developmental tests, school problems, conflicts with peers, and increased rates of psychiatric problems.6–9 Unfortunately, screening and diagnosis of maternal depression is suboptimal, leaving many mothers and newborns at increased risk for negative consequences.10
A number of studies have identified contacts in pediatric offices as potential opportunities for the diagnosis of and referral for maternal depression.3 In general, however, pediatricians are not prepared for this responsibility. Without specific instruction, most clinicians depend on a general impression of the mother, which is imprecise and may miss many cases.11 12 In response, some have called for more standardized screening in the pediatric clinical environment.10 11
How best to carry out such screening has been debated. A delicate balance must be found between a comprehensive instrument, that might be specific but time-intensive, and an easily implemented tool which might be sensitive but not specific.13 A growing body of evidence points to the fact that asking as few as three questions2 and even just two that look for feelings of depression and anhedonia may be enough to screen for maternal depression.10 14 Even if a two-question screening tool is sufficient, finding a way to integrate universal screening into the pediatric clinical environment is not straightforward.
As with many sensitive issues, clinicians may also be hesitant to screen for maternal depression because they are uncertain how to respond when the problem is detected.15 They need help with appropriate diagnostic and educational materials as well as information about local resources to share with the mother.
Clinical decision support systems that are integrated with electronic medical records offer a good opportunity to introduce such screening in an unobtrusive manner. Further, they can provide appropriate testing and educational materials at the point of care when needed. We have developed a novel system that supports such screening and evaluation in a way that minimizes obstructions to normal processes of care. We hypothesized that (1) automated screening for maternal depression and (2) just in time delivery of testing and referral materials at the point of care would promote universal screening of new mothers and thereby increase referrals for maternal depression.
Methods
The CHICA system
CHICA (Child Health Improvement through Computer Automation) is a decision support and electronic medical record system for pediatric health surveillance and disease management. CHICA also serves as a portal for data exchange with the Regenstrief Medical Record System (RMRS).16 It can work as a standalone application or be coupled with any other clinical information system. CHICA's primary user interface consists of two sheets of paper that collect handwritten responses to dynamically generated questions and clinical reminders while easily integrating into clinic workflows.17 18 These forms are created by CHICA and tailored to the individual patient. The forms, called adaptive turnaround documents (ATDs), are scanned, and data are read by optical character recognition and optical mark recognition software. CHICA uses a library of Arden Syntax rules19 that utilize data from the RMRS and CHICA medical records to determine what information should be printed on each ATD. CHICA also uses a global prioritization scheme to determine the most relevant information to be printed. This effectively constrains the number of topics that CHICA recommends for any given patient encounter.
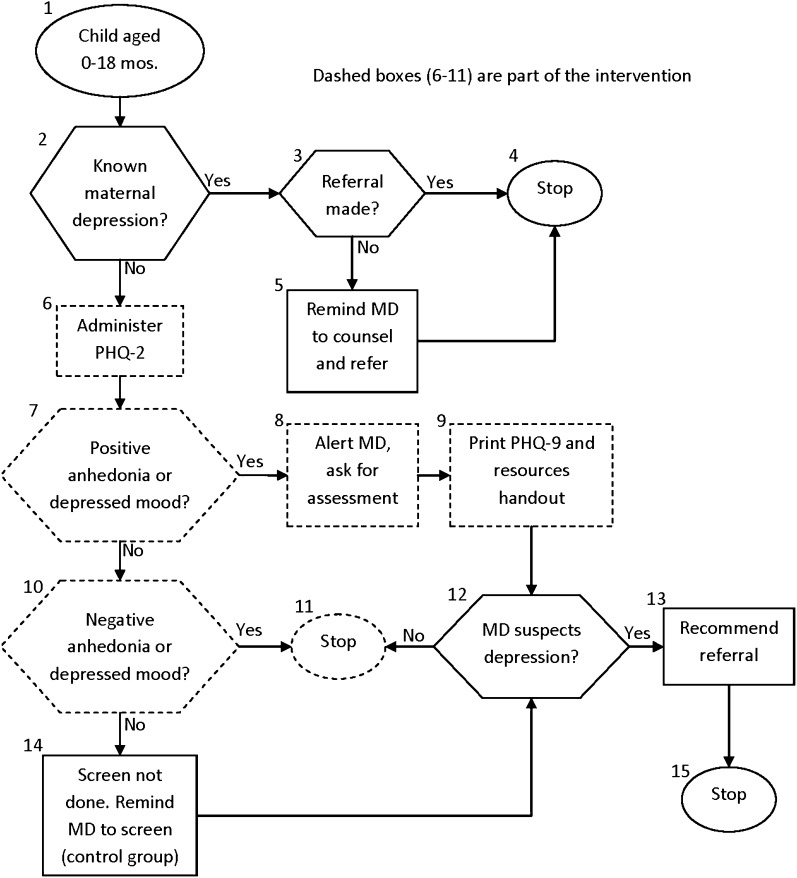
CHICA's functionality in a given domain is first conceptualized as a clinical algorithm (figure 1). The algorithm is segmented and the segments are converted into Arden Syntax rules (also called medical logic modules or MLMs). For example, the segment indicated by the dotted line in figure 1 was converted into a rule whose ‘Action slot’ says:
write (**ATTENTION** <First Name>'s parent identified symptoms of depressed mood on <Date>. Symptoms of sadness, anhedonia, sleep disturbance or appetite disturbance may indicate depression.)
Figure 1.
CHICA's maternal depression screening algorithm. CHICA, The Child Health Improvement through Computer Automation system; MD, medical doctor; PHQ-9, nine-item Patient Health Questionnaire.
We have implemented a limited Arden Syntax interpreter in CHICA, using ANTLR open source parsing software (http://www.antlr.org/). The MLM is converted to executable JAVA code that runs the MLM against the patient data to produce information in an XML format. The XML is accessed by a third party scannable forms producing software (Automerge Publisher, Cardiff Software, Vista, California, USA, http://www.cardiff.com/) to make a printable form (ATD).
In the first step in our clinical workflow, our clinic appointment system sends a registration message (HL7 Admission Discharge Transfer message) to alert CHICA to generate the first of two ATDs. CHICA has a socket listener and HL7 interpreter that parses the Admission Discharge Transfer message, populating the CHICA database and triggering the production of the two ATDs. This first form, called the ‘pre-screening’ form (PSF), captures data from both clinic staff and parents before the patient is seen by a physician. This form has a section for nurses to enter morphometrics, vital signs, and other data, and also contains the 20 most important questions selected by CHICA to ask a child's family. Each question corresponds to an Arden MLM. The form is placed on a clipboard and given to the family by the clinic's front desk staff. The family completes the form in the waiting room. When they are called back, the nurse or medical assistant weighs and measures the child and enters the data in the top portion of the form. The form is then placed by the nurse or medical assistant into a high volume scanner. The scanner captures an image of the form from which CHICA extracts the coded data.
Data obtained through the PSF are merged with previously existing data and analyzed to generate a second ATD, also known as the ‘provider worksheet’ (PWS). The scanning of the PSF triggers the printing of the PWS. This PWS contains up to six reminders, each generated by an Arden MLM, which are tailored to the individual patient based on the merged data of the PSF and existing records. Each reminder contains a ‘stem,’ introducing the reason for the prompt to the clinician, and between one and six ‘leaves’ which consist of check boxes, allowing the physician to document his or her responses to the reminder. We recognize that some questions are sensitive in nature, and that answers may be affected by whether parents are alone or feel safe. Such questions, like those that address intimate partner violence, instruct the physician to make sure that the parent is alone and in a private place before discussing them further. A physician reminder may also be associated with a ‘just in time’ handout (JIT) that is printed with the PWS. These JITs are produced by a function call in the Arden MLM and can provide targeted additional advice to the physician (eg, a depression screening tool) or to the patient (eg, an educational handout about mental health resources). The JIT prints at the same time as the PWS and is placed on the chart for the physician's use during the encounter. The PWS is scanned by clinic staff at the end of the clinic session. After being scanned, the PSF and PWS are placed in our paper charts. However, TIFF images of the form as well as the coded data collected from them are also stored and accessible through our electronic health record.
Intervention: maternal depression module
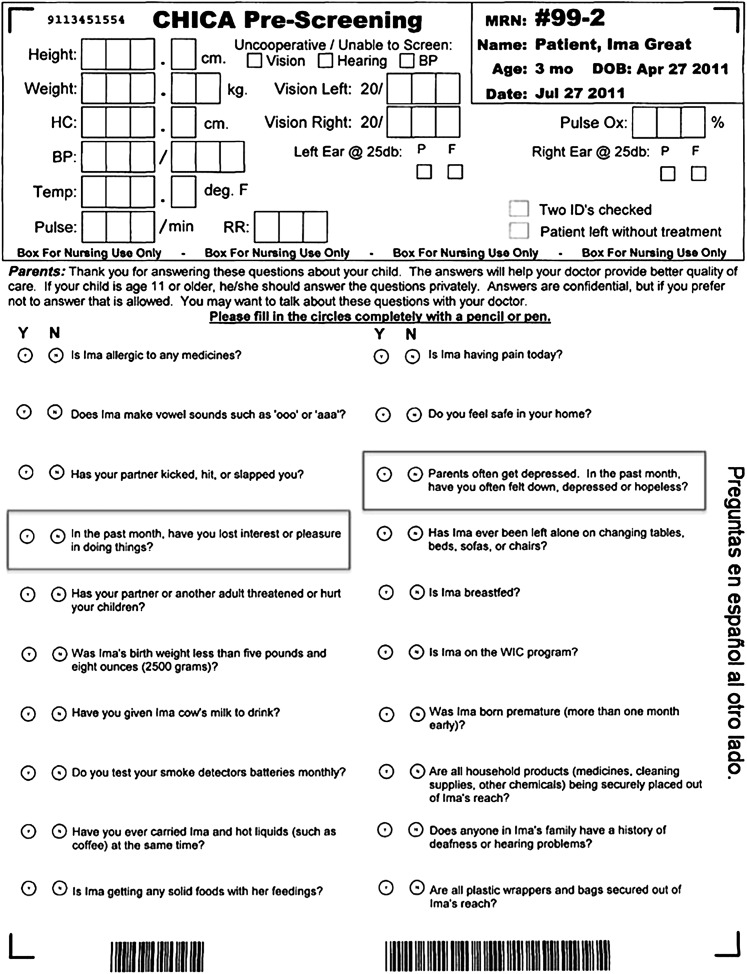
A specific rule set was created for the CHICA system to screen, diagnose, and recommend care for maternal depression. We adapted a validated two question screening tool into PSF questions that parents completed in the waiting room when they arrived for clinic visits10 14 (figure 2). These questions were targeted at mothers of children aged 0–15 months, and appeared on the PSF every 3 months.
Figure 2.
Example of a pre-screening form with maternal depression questions.
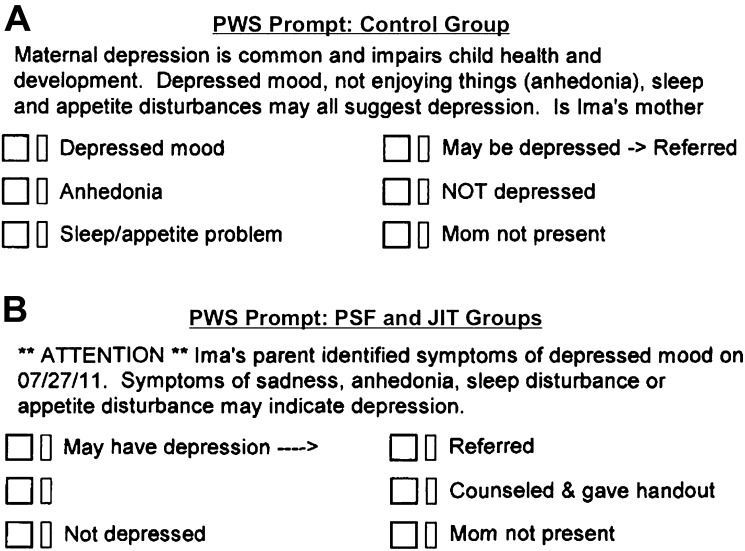
We also created three sets of PWS prompts. Which prompt was presented to the physician on the PWS depended on which of the three study groups a patient was randomly assigned to. The first PWS prompt was generic, and would fire if no information about maternal depression were gathered from the PSF (figure 3A). The second PWS prompt was tailored, and would fire if either of the PSF screening questions were answered ‘yes’ (figure 3B). The final PWS prompt was also tailored, but also included two JIT handouts. The first JIT walked the physician through the diagnosis of maternal depression with the help of the nine-item Patient Health Questionnaire (PHQ-9). The second JIT was an educational handout with information about maternal depression and community resources for treatment of depression.
Figure 3.
(A) Example of the provider worksheet with maternal depression prompts for the control group. (B) Example of the provider worksheet with maternal depression prompts for the PSF and JIT groups (note that in the PSF group, the fourth box read ‘Counseled’ and made no mention of a handout).
Randomization
We performed this study as a non-blinded, interventional, randomized controlled trial. All families with at least one child between the ages of 0 and 15 months seen in our main primary clinic between October 2007 and July 2009 were eligible to take part in this trial. Each year, this clinic sees about 2000 children in that age group. The CHICA system was programmed to assign a child to a study group randomly upon patient registration for a clinic appointment. Specifically, the CHICA system generates a random number for that child and then assigns them to a study group based upon that randomly generated number. However, not every child who attended a clinic was eligible for the study. Moreover, we did not use any block randomization. Therefore, under random conditions, the study groups may have had different numbers of children. The Arden MLMs were programmed to conclude TRUE only if the child was in the appropriate study arm. This means that the MLM's action slot is executed and that output (relevant forms or questions thereon) is generated.
In the control group, no screening questions were asked of mothers on the PSF in the waiting room and physicians received the generic PWS prompt recommending that the mother be screened for depression (figure 3A). In the tailored prompt group (PSF group), mothers were screened with the two questions on the PSF. If either of these questions was answered in the affirmative, the physician received the tailored prompt (figure 3B) alerting him or her to the risk and recommending assessment for depression. The physician was not required to provide a response to the prompt. In the JIT group, mothers were once again screened in the waiting room using the two questions on the PSF. If either of these questions was answered in the affirmative, the physician received both the tailored prompt (figure 3B) and the two JIT handouts, which were available in Spanish and English.
For all mothers answering ‘Yes’ to either of the two screening questions on the PSF in the PSF and JIT groups, the pediatrician was given the opportunity to indicate if he or she suspected maternal depression and provide the mothers with information on how to obtain further assistance. However, the pediatrician was not required to provide a response to the tailored prompt. For mothers in the control group, the physician was reminded to screen for depression and indicate whether he or she suspected depression. It was our hypothesis that the use of screening questions on the PSF would increase the screening rate for maternal depression above a simple reminder to physicians to screen. It was also our hypothesis that the use of a JIT would increase referral rates for suspected maternal depression by guiding the pediatrician through the next steps. Generic forms were available in clinics should physicians wish to distribute them on their own if patients were not in a study group where they were automatically provided.
Data collection
Data were extracted from the CHICA database for use in this analysis. When forms are scanned into CHICA, TIFF images are created. These are then optically read by our software in order to convert responses into data variables that are stored within the database of the CHICA system. Only checked boxes on the PSF are recorded as answered data points. Questions that are ignored will fire at the next visit. Physicians were not required to provide a response to the prompt. An unanswered screening question is not assumed to be a negative response. The same holds true on the PWS. A prompt left unanswered by a physician is not assumed to be negative.
Analysis
We used χ2 analysis to test for differences between groups after randomization. We used logistic regression to determine how the use of the prescreener questions and JIT affected the screening of maternal depression and referral for suspected maternal depression. The unit of analysis was the patient's mother. A family with a child aged between 0 and 15 months could, and should, have more than one visit over the first year of life, and so there were multiple opportunities to detect or diagnose maternal depression. We only counted positives once, however, so that multiple reports of anhedonia or other symptoms were not considered independently.
Based on pilot data collected through the system prior to this study, we concluded that the intervention alone would not bring the maternal depression detection rate up to the 7% prevalence that has been reported nationally. We estimated that if the baseline percentage of suspected maternal depression was 3%, and we wished to detect a 2% difference with an α error level of 5% and a β error level of 20%, we would need about 1200 participants per group. All calculations were performed using the STATA V.9.0 statistical package.
All methods for this study were approved by the Indiana University School of Medicine Institutional Review Board. A waiver of the informed consent process was granted by the Institutional Review Board. Physicians caring for patients in the clinic were also not notified about the study, as doing so explicitly might have changed their practices.
Results
For this study, we analyzed data from our largest clinic, which is an academic pediatric setting that involved 48 attending physicians over the course of the study. During this study, 3520 children between the ages of 0 and 15 months were randomized to one of the three treatment groups.
The control group had 1186 children assigned to it, and each of the two intervention (PSF and JIT) groups had 1167 children assigned. Children were about equally split between males and females, and were mostly Hispanic (40%) or African–American (35%). No significant differences were seen between groups with respect to race, sex, or number of visits (table 1).
Table 1.
Demographic data on study population
| Control | JIT | PSF | |
| Race | |||
| American Indian | 4 (0.35) | 4 (0.4%) | 2 (0.2%) |
| Asian Pacific | 41 (3.5%) | 37 (3.2%) | 37 (3.2%) |
| Black | 407 (34.6%) | 398 (34.4%) | 427 (36.9%) |
| Hispanic | 484 (41.1%) | 452 (39.0%) | 465 (40.2%) |
| Other | 34 (2.9%) | 29 (2.5%) | 29 (2.5%) |
| White | 207 (17.6%) | 238 (20.65) | 198 (17.1%) |
| Sex | |||
| Female | 611 (51.5%) | 565 (48.1%) | 590 (50.6%) |
| Male | 575 (48.5%) | 602 (51.6%) | 577 (49.4%) |
| Patients with this many visits | |||
| 1 | 1186 | 1167 | 1167 |
| 2 | 764 | 742 | 736 |
| 3 | 550 | 542 | 568 |
| 4 | 411 | 408 | 417 |
| 5 | 306 | 300 | 309 |
| >5 | 220 | 217 | 210 |
JIT, just-in-time document group; PSF, prescreener form group.
The main outcome of interest was whether the physician suspected that a diagnosis of maternal depression was warranted and therefore referred a mother for assistance by providing her with information about why help is needed and how to obtain the necessary help. In the control group, 14 (1.2%) of the mothers had suspected depression and were therefore referred, but significantly more (28) mothers in both the PSF and JIT groups (2.4%, OR 2.06, 95% CI 1.08 to 3.93) presented with this finding (table 2). Moreover, significantly more mothers were also found to have concerning symptoms in the intervention groups. Compared to the control group, where 14 mothers were noted to have depressed mood, 103 answered this question affirmatively in the PSF group (OR 7.93, 95% CI 4.51 to 13.96) and 101 in the JIT group (OR 8.10, 95% CI 4.61 to 14.25). Similarly, compared to the control group, where five were noted to have signs of anhedonia, 59 answered this question affirmatively in the PSF group (OR 12.58, 95% CI 5.03 to 31.46) and 61 in the JIT group (OR 13.03, 95% CI 5.21 to 32.54).
Table 2.
Differences in screening and diagnosis rates among the control group, the PSF only group, and the JIT group
| Control | JIT | PSF | |
| Total number of patients | 1186 | 1167 | 1167 |
| Screened positive for depressed mood | 14 (1.2%) | 101 (8.7%) | 103 (8.8%) |
| Screened positive for anhedonia | 5 (0.4%) | 61 (5.2%) | 59 (5.1%) |
| Referred for depression | 14 (1.2%) | 28 (2.4%) | 28 (2.4%) |
JIT, just-in-time document group; PSF, prescreener form group.
In general, the use of the JIT only slightly increased the numbers of mothers screened for or ultimately referred on for assistance with maternal depression. The use of the JIT did, however, result in significantly more mothers being referred for assistance earlier. Of the 28 mothers referred for maternal depression in the PSF group, five were referred in the first week of their child's life. In the JIT group, 12 of the 28 were referred in the child's first week of life (OR 3.45, 95% CI 1.004 to 11.85).
An interesting anecdotal observation was that, because randomization was by patient, physicians began complaining that CHICA was malfunctioning when they were alerted to depression risk among patients in the PSF group, because they were not receiving the JIT handouts. In response, the clinicians began photocopying and using the handouts from patients in the JIT group for patients in the PSF group.
Discussion
By automating the process of maternal depression screening and alerting the pediatrician to those who screened positive with our decision support system, we significantly increased the identification of suspected depression among mothers in our clinic. We found that the use of our PSF, where questions were asked directly of parents, resulted in a dramatic increase in the detection of depressed mood and/or anhedonia among mothers in the clinic. We also found that the percentage of mothers who were suspected of having maternal depression and were therefore referred on for further care or support doubled.
We found that providing the two JIT (eg, the PHQ-9 and the educational and referral form) handouts to the pediatrician had a more subtle effect on the care of mothers with postpartum depression. Although there was no increase in the rate of referral for maternal depression over the PSF alone, more mothers were referred earlier in a newborn's life when the JIT handouts were provided. This may be because the use of the JIT handouts made pediatricians more comfortable in making the decision to refer sooner. The JITs were apparently valued by the clinicians who began using the forms among patients in the PSF arm of the study. The resulting contamination would create a bias toward the null and may mean the study underestimated the effect of the JIT. Further work, using a different unit of randomization, would need to be done to confirm this supposition.
This study, like all research, has limitations that warrant consideration. The overall numbers of mothers who were suspected of maternal depression still falls well below the prevalence we might expect given the literature on the topic. This may be because even with help, pediatricians are still reluctant to engage in this issue. It may also be that referrals were made, but not recorded on the CHICA worksheet as physicians were not required to respond to the prompt. We have no reason to believe, however, that there would be a differential recording of referrals made across our study groups. Such research is also somewhat limited in its generalizability. Additionally, it is possible that different factors, such as seeing adoptive mothers or foster mothers, might change the overall prevalence. The randomized nature of the study, though, should ensure that these differences were evenly distributed among the study groups. Our CHICA system has benefits and flaws that differ from other such systems, and the fact that our system performed well in this study does not necessarily mean another would perform better or worse. We are, however, explicit about the features in our system so that individuals can make comparisons and decide how our findings might be translated across environments. Further, CHICA is built on an open-source platform, and it is our goal to make it available to other clinic settings that would like to use it for pediatric care. We can also only report on what happened in the clinic; we do not know how many mothers actually made use of resources provided to them or in how many mothers maternal depression was eventually diagnosed.
Other studies have investigated the use of electronic reminders to encourage providers to screen for maternal depression.20 21 Those, however, have relied primarily on the physician as the first line for screening, and have therefore tried to limit the number of screenings to one visit in a child's first year. Studies that screened mothers directly relied on clinic staff, creating challenges to sustainability.3 The CHICA system, on the other hand, potentially relieves physicians and staff of the need to carry out primary screening by automating the process, and thus makes multiple screening less of a burden on clinic staff and workflow. We believe that this has great potential in a number of domains, and may also make screening more cost-effective.22
Maternal depression is an important and prevalent condition that necessitates wider screening and treatment. Clinical decision support systems such as CHICA can be used to improve the recognition and management of this disorder by combining automated screening in the waiting room, physician alerts, and just in time support materials. More work is needed to identify how we can further improve CHICA in this, and other domains, to improve the ability of clinicians to care for conditions for which they might not feel completely comfortable and prepared.
Footnotes
Contributors: All authors participated in the conception and design, or analysis and interpretation of data; helped to draft the article or revise it critically for important intellectual content; and gave final approval of the version to be published. The views expressed in this article are those of the authors and do not necessarily represent those of Indiana University.
Funding: This project was supported by grant number K22LM009160 from the National Library of Medicine.
Competing interests: All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: one author (PGB) had financial support from the NIH/NLM for the submitted work, and no other authors had relationships or activities that could appear to have influenced the submitted work.
Ethics approval: Ethics approval was provided by Indiana University School of Medicine Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Chaudron LH. Postpartum depression: what pediatricians need to know. Pediatr Rev 2003;24:154–61 [DOI] [PubMed] [Google Scholar]
- 2. Kabir K, Sheeder J, Kelly LS. Identifying postpartum depression: are 3 questions as good as 10? Pediatrics 2008;122:e696–702 [DOI] [PubMed] [Google Scholar]
- 3. Olson AL, Dietrich AJ, Prazar G, et al. Brief maternal depression screening at well-child visits. Pediatrics 2006;118:207–16 [DOI] [PubMed] [Google Scholar]
- 4. O'hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. Int Rev Psychiatry 1996;8:37–54 [Google Scholar]
- 5. Gibson J, McKenzie-McHarg K, Shakespeare J, et al. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand 2009;119:350–64 [DOI] [PubMed] [Google Scholar]
- 6. Boath EH, Pryce AJ, Cox JL. Postnatal depression: the impact on the family. J Reprod Infant Psychol 1998;16:199–203 [Google Scholar]
- 7. Murray L, Cooper P. Editorial: postpartum depression and child development. Psychol Med 1997;27:253–60 [DOI] [PubMed] [Google Scholar]
- 8. Caplan H, Cogill S, Alexandra H, et al. Maternal depression and the emotional development of the child. Br J Psychiatry 1989;154:818–22 [DOI] [PubMed] [Google Scholar]
- 9. Murray L, Sinclair D, Cooper P, et al. The socioemotional development of 5-year-old children of postnatally depressed mothers. J Child Psychol Psychiatry 1999;40:1259–71 [PubMed] [Google Scholar]
- 10. Cutler CB, Legano LA, Dreyer BP, et al. Screening for maternal depression in a low education population using a two item questionnaire. Arch Womens Ment Health 2007;10:277–83 [DOI] [PubMed] [Google Scholar]
- 11. Mishina H, Takayama JI. Screening for maternal depression in primary care pediatrics. Curr Opin Pediatr 2009;21:789–93 [DOI] [PubMed] [Google Scholar]
- 12. Olson AL, Kemper KJ, Kelleher KJ, et al. Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics 2002;110:1169–76 [DOI] [PubMed] [Google Scholar]
- 13. Chaudron LH, Szilagyi PG, Tang W, et al. Accuracy of depression screening tools for identifying postpartum depression among urban mothers. Pediatrics 2010;125:e609–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gjerdingen D, Crow S, McGovern P, et al. Postpartum depression screening at well-child visits: validity of a 2-question screen and the PHQ-9. Ann Fam Med 2009;7:63–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sugg NK, Inui T. Primary care physicians' response to domestic violence. Opening Pandora's box. JAMA 1992;267:3157–60 [PubMed] [Google Scholar]
- 16. McDonald CJ, Overhage JM, Tierney WM, et al. The Regenstrief Medical Record System: a quarter century experience. Int J Med Inform 1999;54:225–53 [DOI] [PubMed] [Google Scholar]
- 17. Biondich PG, Downs SM, Anand V, et al. Automating the recognition and prioritization of needed preventive services: early results from the CHICA system. AMIA Annu Symp Proc 2005:51–5 [PMC free article] [PubMed] [Google Scholar]
- 18. Biondich PG, Overhage JM, Dexter PR, et al. A modern optical character recognition system in a real world clinical setting: some accuracy and feasibility observations. Proc AMIA Symp 2002:56–60 [PMC free article] [PubMed] [Google Scholar]
- 19. Jenders RA, Hripcsak G, Sideli RV, et al. Medical decision support: experience with implementing the Arden Syntax at the Columbia-Presbyterian Medical Center. Proc Annu Symp Comput Appl Med Care 1995:169–73 [PMC free article] [PubMed] [Google Scholar]
- 20. Sheeder J, Kabir K, Stafford B. Screening for postpartum depression at well-child visits: is once enough during the first 6 months of life? Pediatrics 2009;123:e982–8 [DOI] [PubMed] [Google Scholar]
- 21. Bogen D. Electronic reminder systems increase screening for postpartum depression. J Pediatr 2009;155:758–9 [DOI] [PubMed] [Google Scholar]
- 22. Hewitt CE, Gilbody SM. Is it clinically and cost effective to screen for postnatal depression: a systematic review of controlled clinical trials and economic evidence. BJOG 2009;116:1019–27 [DOI] [PubMed] [Google Scholar]