Abstract
The findings of a case study assessing the design and implementation of an electronic health record (EHR) in the public health system of Colima, Mexico, its perceived benefits and limitations, and recommendations for improving the implementation process are presented. In-depth interviews and focus group discussions were used to examine the experience of the actors and stakeholders participating in the design and implementation of EHRs. Results indicate that the main driving force behind the use of EHRs was to improve reporting to the two of the main government health and social development programs. Significant challenges to the success of the EHR include resistance by physicians to use the ICD-10 to code diagnoses, insufficient attention to recurrent resources needed to maintain the system, and pressure from federal programs to establish parallel information systems. Operating funds and more importantly political commitment are required to ensure sustainability of the EHRs in Colimaima.
Keywords: Electronic Health Records, Mexico, Public Health, Ambulatory Care Information Systems, Health Informatics
Introduction
The electronic health record (EHR) is a tool with the potential to improve the quality, safety, and efficiency of health services.1–9 It can also provide data for assessing the health status of the population and the performance of the health system itself.10 11 Many countries in the developing world are considering EHR adoption.12
In Mexico, different public and private healthcare institutions have adopted EHRs, including Mexico's Social Security Institute,13 the Institute for Social Security and Services for Government Employees, and the health services of several states and many private hospitals. As part of the national strategy for monitoring and improving the quality, functionality, and interoperability of EHRs in Mexico, in 2010 the General Directorate of Health Information published the Official Mexican Standard NOM-024-SSA3-2010.14 However, the way in which EHRs have been introduced and their specific functionality have varied between institutions and states, mainly because they were developed and implemented before publication of the official standard.13 15 16
Mexico's health system consists of public institutions and private providers, all of which are under the governance of the Ministry of Health. The public social security institutions provide services to the employees of the formal economic sector and civil servants, as well as other public sector specific institutions (eg, the federal oil company PEMEX and the Armed Forces). Together these account for approximately 44% of the population.17 The rest of the population is served either by the System for Social Protection in Health (SSPH), also known as Seguro Popular, or by private providers. The SSPH is a health insurance program for the poor and other vulnerable individuals and has become one of the main funding agencies for the health system in Mexico. Its beneficiaries receive healthcare services through the Ministry of Health and the 32 decentralized State Health Services (SHS). Colima's SHS provide health care to approximately 42% of the state's population including the beneficiaries of the SSPH and the Oportunidades Program, a conditional cash transfer program designed to address health and poverty.18 These two programs are important sources of funds for the operation of the SHS and demand detailed and systematic information about their affiliates, most often by imposing specialized parallel systems.
The state of Colima demonstrated leadership and foresight with the development and implementation of an EHR beginning in 2005, called SAECCOL. Other states, such as Coahuila, Aguascalientes, and Yucatán, have expressed interest in adopting SAECCOL.19 In fact, the state of Coahuila has already started to implement it in several hospitals. As they have improved and developed new modules, they have shared back these improvements with Colima, in the spirit of open source software development.
Given the potential benefits of SAECCOL in Colima and the possibility that other states in Mexico may adopt the system, our purpose was to assess the design and implementation of SAECCOL, its perceived benefits and limitations, and to make recommendations to improve the system and implementation process. Despite the number of states implementing EHRs, there are no studies that document the design and implementation process or assess the effectiveness of EHRs in improving the quality and efficiency of care delivered in Mexico's public healthcare facilities, and few in low and middle income countries. We explored the technical, organizational, and behavioral issues that may have affected EHR adoption and use, and their possible implications for other states and countries. Our results have implications that can guide other states in Mexico and other countries in the design and implementation of an EHR in the public health system.
Materials and methods
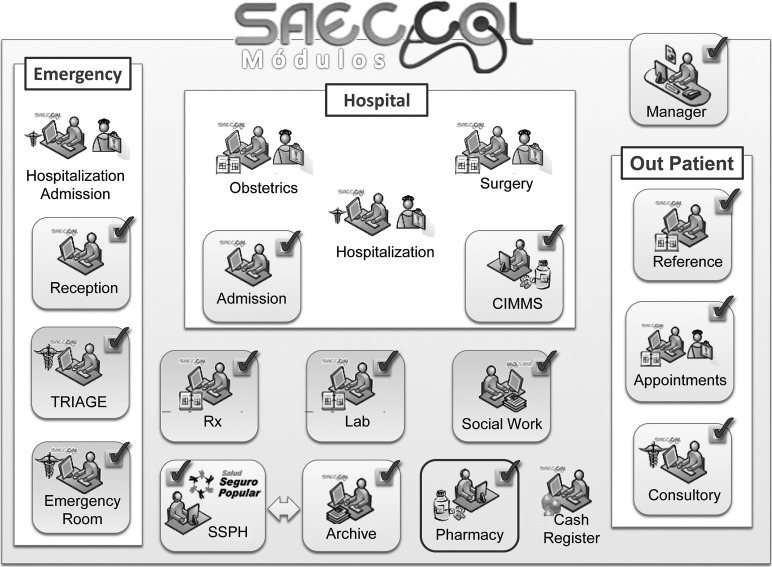
SAECCOL is an EHR developed and implemented by Colima's SHS. It is based on the MS-SQL Server database management system and Visual Basic was used for the development of the main application and specific modules. It is a modular system (figure 1) that at the time of the study operated mainly in the outpatient and emergency departments, offering support services such as laboratory, imagery, pharmacy, social work and archive modules, the last of which is linked to SSPH's databases. The system allows physicians to record and retrieve the clinical history of patients, as well as all consultation data including drug prescriptions and laboratory studies requested. The system had not been fully implemented in the hospital environment at the time of the study, with working sub-modules only operating in admissions and the pharmacy department. The archive module also transfers administrative data for the management of the SSPH.
Figure 1.
SAECCOL home-grown modular electronic health record (EHR). SSPH, System for Social Protection in Health.
Framework analysis, a method developed specifically for applied research where there are particular questions to be answered, a limited time frame, and a pre-designed sample,20 21 was used and included in-depth interviews and focus group discussions to examine the experiences of the actors and stakeholders who participated in the design and implementation of EHRs in the state of Colima.21 Key informants were selected using purposive sampling to ensure that all SHS officials and IT experts in Colima who were involved in the development, implementation, and operation of SAECCOL were included. In addition, four officials of the SSPH and the Oportunidades Program at the federal level were also interviewed so that the perspectives of the financing agencies would be represented (table 1).
Table 1.
Types of actors and their respective roles in the design, implementation, and operation of SAECCOL
| Type of actor | Roll/functions | N |
|---|---|---|
| Federal level officials | Federal health system governance Financing state health services (SHS) through the System for Social Protection in Health and/or Oportunidades ProgramDeveloping and publishing official norms |
4 |
| State level officials | State level governance Operate SHSState public policy to establish the conditions for SAECCOL development, implementation, and operationParticipation in the design and implementation of SAECCOL |
7 |
| Hospital and health center managers | Directing health center/hospitals Administrative tasks using of information generated by SAECCOL |
10 |
| IT staff | Participation in the design of SAECCOL Development of SAECCOL's softwareImplementation of SAECCOL in health centers and hospitals including installation and training of physicians |
6 |
| Physicians in outpatient departments | Use SAECCOL as a tool to improve doctor/patient interaction through the use of data recorded in SAECCOL | 35 |
| Total | 62 |
In total, 27 in-depth interviews were held (table 2). Four focus groups were conducted with physicians at two health centers and two hospitals who were categorized as either pioneer users of the system or as new users (table 3). The views were obtained of 35 physicians or about 10% of all general physicians working in outpatient departments using SAECCOL: (1) doctors working in facilities that adopted the system relatively early (Centro de Salud Gustavo Vázquez Montes); (2) doctors working in facilities that adopted the system relatively recently (Centro de Salud Colima); (3) doctors working in hospitals that adopted the system relatively early (Hospital de Tecoman); and (4) doctors working in hospitals that adopted the system relatively recently (Hospital de Manzanillo).
Table 2.
Demographic characteristics of in-depth interview participants
| Demographic characteristics | N | % |
|---|---|---|
| Type of actor | ||
| Federal level officials | 4 | 14.8 |
| State level officials | 7 | 25.9 |
| Hospital and health center managers | 10 | 37.0 |
| IT staff | 6 | 22.2 |
| Sex | ||
| Male | 20 | 74.1 |
| Female | 7 | 25.9 |
| Age | ||
| 20–39 years | 14 | 51.9 |
| 40 years or more | 13 | 48.1 |
| Training | ||
| Physician | 17 | 63.0 |
| IT specialist | 6 | 22.2 |
| Other | 4 | 14.8 |
Table 3.
Demographic characteristics of focal group discussion participants
| Demographic characteristics | N | % |
|---|---|---|
| Type of health center | ||
| Pioneer | 16 | 45.7 |
| Recently implemented | 19 | 54.3 |
| Sex | ||
| Male | 19 | 54.3 |
| Female | 16 | 45.7 |
| Age groups | ||
| 20–39 years | 22 | 62.9 |
| 40 years or more | 13 | 37.1 |
| Time using SAECCOL | ||
| None | 3 | 8.6 |
| Less than 2 years | 27 | 77.1 |
| 2 years or more | 5 | 14.3 |
| Training | ||
| Physician | 31 | 88.6 |
| Nurse | 3 | 8.6 |
| Other | 1 | 2.9 |
The Gustavo Vázquez Montes health center is an urban outpatient center with three general consultation rooms and 10 general physicians. The Colima health center has 12 consultation rooms and 22 general physicians. Tecoman and Manzanillo hospitals are general hospitals with the four basic services (internal medicine, surgery, pediatric, and obstetric) with 47 and 60 beds, respectively. Tecoman hospital has 13 consultation rooms and 12 general physicians, while Manzanillo hospital has 15 consultation rooms and 11 general physicians.
The Institutional Review Boards of the National Institute of Public Health (INSP) and Tulane University approved the research protocol. Informed consent was obtained verbally from all participants to ensure they fully understood that their participation was strictly voluntary, that the data collected were to be kept anonymous, and that their comments in the discussions would not affect their jobs in any way. Participants were also informed they could leave the interview or focus group at any time without repercussion.
Standardized interview and discussion guides were designed and tested with volunteer physicians in Mexico City. Interviewers were trained to adhere to the interview protocol in order to minimize interviewer bias. After informed consent was received from key informants, face-to-face interviews were conducted, recorded, and transcribed, and focus group discussions were audio and video recorded and transcribed. All interviews and focus group discussions were conducted in Spanish. Audio and video recordings were kept for further reference and will be destroyed at the end of the study.
Interviews were conducted by two native Spanish speaking female researchers with experience in qualitative research (August 3–19, 2011, in Colima state and September 1–19, 2011, in Mexico City). A group of experienced, Spanish speaking researchers from INSP and Tulane University read the interview and focus group transcripts to code the data and group them into key concepts and analytical axes. Some of the codes were generated according to the research questions, while others emerged from the interviews. NVivo 9.2 software22 was used to analyze the data around three analytical axes: design and development of the EHR (planning and organization, criteria, and requirements), implementation of the EHR (users, constraints, and resources), and the impact of the EHR (benefits, recommendations, and vision for the future) (table 4). Each researcher coded separate interviews. Before starting, a coding exercise was conducted to make sure all researchers were interpreting the codes in the same way and there was constant discussion during the analysis to ensure there was agreement across researchers.
Table 4.
Analytical axes and key concepts
| Analytical axis | Key concept | Description of key concept | Sources | References |
|---|---|---|---|---|
| Design | ||||
| Consensus | Design and development of SAECCOL was with the agreement of all actors and stakeholders | 14 | 24 | |
| Advocacy | Advocacy to develop SAECCOL | 12 | 15 | |
| Motivation | Reasons behind the decision to develop and implement SAECCOL | 8 | 19 | |
| Requirements | Experiences, best practices, and requirements of EHRs | 15 | 23 | |
| Time | Time dedicated to the design and development of SAECCOL | 10 | 12 | |
| Funding | Funds allocated for the design and development of SAECCOL | 7 | 8 | |
| Implementation | ||||
| Training | Initial training process | 22 | 23 | |
| Hardware and communications | Availability of computers and internet connectivity | 20 | 26 | |
| Infrastructure | Health centers and hospitals where SAECCOL was implemented | 19 | 27 | |
| Budget | Budget allocated for SAECCOL's implementation | 8 | 10 | |
| Time | Time dedicated by hospital and health center managers and medical staff to implement SAECCOL | 11 | 15 | |
| Benefits | ||||
| Quality of care | Monitoring health care | 16 | 35 | |
| Reliable information | Availability of quality data produced by SAECCOL | 13 | 17 | |
| Information improvement | Availability of statistical data for decision making based on SAECCOL's data | 15 | 21 | |
| Health system organization | Organization of health services (appointments, waiting time, consultation time, process standardization) | 15 | 33 | |
| Data safety | Data safety | 6 | 15 | |
| Challenges | ||||
| ICD-10 | Physicians experience with the use of SAECCOL and diagnoses using ICD-10 classification | 7 | 26 | |
| Difficulties | Difficulties experienced in the use of SAECCOL | 18 | 48 | |
| Implementation discontinuity | Reasons for interrupting implementation | 10 | 18 | |
| Disarticulation | Disarticulation in the development of SAECCOL by different actors | 13 | 15 | |
| Mixed health records | Need to maintain paper-based records coexisting with EHR | 17 | 22 | |
| Lack of infrastructure | Availability of computers/computers obsolete/no electricity or supplies | 25 | 36 | |
| Lack of training | Experiences with lack of training | 11 | 13 | |
| Does not cover all needs | Evidence that SAECCOL does not cover all the needs of doctors | 20 | 33 | |
| Resistance to change | Evidence of resistance to change from paper-based to EHRs | 12 | 14 | |
| Partial use of EHR | Experiences in partial use of SAECCOL | 11 | 13 | |
| Challenges | Documenting challenges in the implementation of an EHR | 14 | 14 |
EHR, electronic health record; ICD-10, International Classification of Diseases, Tenth Revision.
Results
Design
The EHR in Colima was conceived in 2004 by the General Directorate of the SSPH in the state as a way to collect health and administrative data on its beneficiaries. The development process was an extensive and collaborative exercise, which involved practitioners, medical specialists, hospital directors, and information technology experts, and lasted more than a year (box 1: quote 1). The information technology department of the state office of the SSPH was at first in charge of the design and development of the EHR but this responsibility was later transferred to Colima's SHS IT department. The SSPH Affiliation Director, in cooperation with IT specialists from the Colima SHS, physicians, and consultants, continued to lead the development effort. All participants understood that the EHR was being developed to meet the information needs of the SSPH, including the need to provide data to the federal health information system (box 2: quote 2). Although the EHR was not designed to provide information to physicians and other caregivers at the point of care as the key objective, it does make some relevant information available to them. It was also clear that a key objective was that the EHR should comply with the International Classification of Diseases, Tenth Revision (ICD-10). At the time SAECCOL was first conceived and developed, the official standard NOM-024-SSA1-2010 for EHRs had not yet been published, but there is now pressure for 100% compliance with it within the next 3 years.
Implementation
Colima's SHS IT department led the process of implementing the EHR in the state. They implemented the EHR using a gradual, phased approach following its launch in 2005. In selecting facilities for implementation, priority was placed on outpatient services in medium-sized health centers in urban areas that had the minimum infrastructure required, including electricity, wiring, and internet connectivity. Training in how to use the system was conducted by the SHS IT department both through facility-specific sessions attended by physicians and facility directors, and through pre-service training of residents of the University of Colima's Medical School (box 3: quote 3). The first phase of implementation took place from 2005 to 2006 with the acquisition of 300 computers, and covered almost 80% of the state's health centers and hospitals. By that time, the SHS IT department had three areas servicing SAECCOL: system development, implementation (installation and training), and technical support, but no additional operating funds (box 3: quote 4).
Benefits of the EHR
Facility directors and physicians using the EHR suggest that the system has produced a number of important benefits, motivating them to continue using the system. For example, many respondents mentioned that the organization of healthcare delivery has been improved through the use of the appointment scheduling features of the EHR. This saves time for patients, who no longer need to wait for hours at the facility in order to receive care, and for physicians, by saving time during consultations and improving the standardization, completeness, and legibility of medical records (box 4: quote 5). A number of physicians also mentioned that the improved information from the EHR has allowed them to better understand the medical history of their patients, make diagnoses earlier, and reduce medication errors (box 4: quote 6). Facility directors also commented that the use of the administrative data produced by SAECCOL had improved their management capabilities, allowing them to monitor the performance of health centers and hospitals.
Challenges
Respondents also identified a number of challenges to the adoption and continued use of the EHR. Some respondents mentioned issues of trust. For example, physicians expressed suspicion that the SHS introduced EHRs in order to monitor medical staff. Respondents at the state level mentioned that federal program administrators sometimes have a paternalistic view of state officials, are dubious about the quality of EHR information, and insist on receiving paper-based reports. A frequently mentioned issue during the interviews and focus group discussions was the ICD-10 classification scheme, which plays a large role in the EHR system. Physicians complained about the difficulty in identifying ICD-10 disease codes, which was not part of their medical education (box 5: quotes 7–9). They mentioned that they are not trained to use ICD-10, and that although most cases are easy to code, a small portion are difficult, resulting in substantial frustration. SHS officials and staff insisted that physicians must make diagnoses using ICD-10, but were trying to develop alternative ways to facilitate physician coding of diagnoses according to ICD-10 to address physician concerns. To help implement diagnosis coding according to ICD-10, at the time of the study, the IT department was building a list of the most common diagnoses (as usually reported by physicians) with their respective ICD-10 codes; however, this effort has still not completely resolved the coding issue. Other challenges mentioned include insufficient training, which causes excessive time to be spent on entering data, frustration with features that ensure the security of records, the rigidity of the system, and resistance to change.
General results
There was a common view that the EHR (SAECCOL) is a valuable tool, and most of those interviewed agreed it was necessary to use it more effectively to improve the quality of healthcare so that it mainly benefits patients. There were important differences among the respondents regarding its functionality and usability. While young doctors found no difficulty in adapting their workflow in the consultation room to work with the EHR, older doctors complained that it was difficult to use. Doctors in health centers and hospitals where SAECCOL has recently been deployed also complained, but they also indicated interest in receiving more training in order to master its use. The one issue that respondents agreed upon was the difficulties with the use of ICD-10. They all expressed frustration with the need to classify their diagnoses and that it was not part of their training as physicians. They also agreed that Colima's SHS IT department has made important efforts to address those difficulties, but that the issue is still not resolved.
Discussion
The purpose of the study was to assess the development and implementation of SAECCOL, its perceived benefits and limitations, and to make recommendations to improve the system and implementation process. Our results show that the main driving force behind the design, development, and implementation of SAECCOL was the strengthening of mandated reporting to the SSPH and Oportunidades Program, two of the main programs to improve health and social development in Mexico. The decision to design and develop an EHR to meet the information-reporting requirements of the SSPH and federal health information systems affected the potential of the EHR to influence the quality, efficiency, and cost of health service delivery. The collaborative effort of physicians, hospital administrators, IT specialists, and state officials was fundamental in the design and development process. The University of Colima was instrumental in the decision to follow a ‘home grown’ EHR development strategy. As a result, and in spite of its reporting focus, physicians saw benefits from improved data availability, a better understanding of their patient's history, and reduced medication errors. However, these benefits fall short of the potential benefits of an EHR for improving quality of care.
The SHS of Colima was able to take advantage of the information needs of important health programs to secure funds for initial investment for the development and implementation of their EHR, which proved to be a very successful strategy. The implementation process was phased and systematic, with appropriate attention to infrastructure requirements, and included efforts to involve stakeholders and generate support for adoption among health workers. From our perspective, this is a highly recommended best practice. However, there were several significant challenges to the success of the EHR. First, physicians were concerned that the EHR was designed primarily to evaluate their performance. They also felt strongly that coding ICD-10 diagnoses is a clerical function being forced on them through the EHR and should not be part of their medical practice.23 Emphasizing the importance of performance monitoring as part of the culture of information and as a way to receive organizational feedback may positively influence the way physicians perceive and react to the EHR's monitoring capacity. Additionally, as ICD-10 coding is needed for standardization of the collection and reporting of EHR data, it must be complied with; nevertheless, the efforts of the IT department to develop alternative features to help the use of this classification scheme may improve the experience of physicians. Another solution to this controversial aspect of SAECCOL would be to allow doctors annotate unclassified diagnoses which would be coded later by specialized coders.
However, following the initial investment, the SHS did not receive further funds and the EHR was not explicitly supported by state policy. Nevertheless, SHS IT personnel continued with the development of new modules. Difficulties in providing technical support and computer maintenance developed, mainly because of a lack of resources (eg, gas, vehicles, and computer parts). In addition, the political environment prevented the channeling of financial resources to the project. EHR use started to decline as providers required training and computers needed to be repaired or replaced, and the project faltered. As part of a set of innovative strategies to make the EHR sustainable, the SHS signed an agreement with the University of Colima medical school that all students should be trained in the use of the EHR.
Another factor endangering the sustainability of the EHR was the lack of an information policy and normative framework at the time of design and development, which impeded the ability to promote governance and to negotiate for operating funds. Also, any change in Colima's SHS administration presents sustainability challenges because newly appointed leaders need to be convinced of the value of the EHR so that they will provide resources for its ongoing maintenance, operation, and development. Fortunately, with the change of administration in 2010, a new perspective on e-government was adopted and the EHR was incorporated into the Governor's State Development Plan, which provided the political basis for directing the necessary resources from both state and federal health programs to strengthen the EHR project. Moreover, the Oportunidades Program, through the SSPH, requested that additional information requirements be met through a parallel information system called Sistema Nominal de Información en Salud, but inclusion of the EHR in the State's Development Plan served as leverage to negotiate its use as the sole source of information for federal health programs, thus avoiding the need for parallel systems and allowing a more efficient use of resources.
The implementation of an EHR in the public health sector is subject to multiple pressures and requires a vast amount of financial and human resources. Operating funds are required to ensure sustainability, but political commitment is also necessary. This must be expressed in a state or national strategic plan in order to withstand administrative/political changes. The authors are well aware that most public institutions do not follow or adhere to such a process. Colima did not begin with a clear strategic plan but rather was responding to the information needs of funding agencies, but nevertheless was able to recover midway under the incoming new administration. This was a lesson learned the hard way.
Overall, our results suggest that designing and implementing EHRs is a gradual and often slow process which requires attention to be given to technical, organizational, and behavioral factors. The results of the study are very much in line with those of previous research. For example, in a study on the implementation and adoption of national EHRs in secondary care facilities in England, Sheikh et al24 found that the speed of implementation was slower than expected, and that the EHRs had a narrower focus and substantially less functionality than originally planned, with no discernible benefits for clinicians or patients among early adopters of the system. In a systematic review of studies on this issue, Boonstra and Broekhuis25 also found that, overall, EHR adoption rates are low and that there is often resistance from physicians. The authors concluded that the process of EHR implementation should be treated as a managerial change project, rather than simply as a technical strategy.
Ideally, the decision to move towards an EHR at the state or national level should be part of a national strategic plan. This promotes ownership and evidence of ability to meet information needs in order to advocate for funds, thus avoiding the creation of parallel systems. The evidence from Colima highlights the importance of including stakeholders in the planning phase in order to address their specific information needs.26 Just as important is the sharing of experiences within a country and south–south collaboration can improve the chances of successful implementation, scalability, and sustainability. It is imperative that funders recognize the potential synergies of their investments in health information systems and technology as a way to promote diagonal effects with positive spill-over effects to other health problems beyond the intended programs.
Box 1. Consensus.
Quote 1
… the designers from the Secretary of Health came to meet with us, talk to us, and give us their comments after seeing the EHR [electronic health record]. “What should it contain?” they asked. The records, ok, the health record has this and that. Then, they would go do their job, bring it back and present it to us. We would then give them feedback: “Do you know? This window should move from here to there. Maybe apply a drop down menu, add this or that, or this is easier.” That's how it was done. (Health center director)
Box 2. Source of information for the System for Social Protection in Health (SSPH) and the Oportunidades Program.
Quote 2
From the start, the project was developed with the belief that it would cover everything, that it was going to be installed in every health center and that it was going to be the primary source of information, and we keep going in this process to reach that goal; fortunately it was developed to that purpose from the beginning. (State IT specialist)
Box 3. Implementation.
Quote 3
Training was done at different levels; we went to the university and explained, because many doctors are still students. It was easier dealing with them because they all have a good understanding of computers. So, we went to the university, took the EHR system to them, and left it with them. At the beginning we used to provide training to the young doctors and in a couple of days they were ready to use the system, even in one day. We did this so that once they graduated they each had a EHR chip and when they got to their communities we didn't have to train them again… and start all over again… (State director)
Quote 4
When the first computer buying was done, 300 computers to cover about 80% of the facilities, it's when it is decided to make a structure based in three areas: software development, and of course most of us continued working there, an implementation area, dedicated exclusively to training and follow up, and another for technical support, which was the infantry, the one in which to serve… (State IT specialist)
Box 4. Benefits.
Quote 5
When the system works ok I think it's perfect; you enter your password and access the EHR, you can check your starting time, your patient list, you select a patient, open his/her file and I can review observations in past encounters and make a medical note a lot easier and clearer and it can be reviewed by any other doctor who may access the record. (Hospital director)
Quote 6
We now have a more specific, focused, and simpler clinical history. (Health center focus group discussion participant)
Box 5. Challenges.
Quote 7
It happened to me many times that I was not able to write in the diagnosis and since I wasn't able to do so, I had to write the diagnosis in a separate box in the hope that when it was printed, at least my diagnosis would show up somewhere in the form. But it wasn't the correct diagnosis… (Hospital director)
Quote 8
It is very difficult to fill in the form in a short period because there is a set amount of time for the consultation: for the use of devices and systems, to conduct a physical check-up and make a presumptive diagnosis plus writing the prescription; and for the preparation of the particulars and setting up the next appointment. If we put this in time, it would take 30–40 minutes per patient. If we only did the health consultation note, we are talking about a period of 10–15 minutes per patient. (Hospital director)
Quote 9
In our case, what we do is to print it with a diagnostic, the closest we can find, and write notes in the analysis section to register our diagnostic, the real one, to put it that way. This is how we have being functioning. (Hospital focus group participant)
Acknowledgments
We would like to thank the state of Colima and all participants in this project.
Footnotes
Contributors: JEHA, LSPM, ALE, MAB, MLD, DH, BP, ES, and ASP: conception and study design; LSPM, MAB, and ASP: field work supervision; LSPM, MAB, and ES: data analysis and interpretation; JEHA, LSPM, ALE, MLD, DH, BP, ES, and ASP: drafting the paper, critical review, and final review and approval of the manuscript.
Funding: Support for this study was obtained from MEASURE Evaluation, which is funded by the US Agency for International Development (USAID) through Cooperative Agreement GHA-A-00-08-00003-00. The views expressed in this publication do not necessarily reflect the views of USAID or the US Government.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Open Access: This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
References
- 1.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med 2003;348:2526–34 [DOI] [PubMed] [Google Scholar]
- 2.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742–52 [DOI] [PubMed] [Google Scholar]
- 3.Furukawa MF, Raghu TS, Shao BBM. Electronic medical records and cost efficiency in hospital medical-surgical units. Inquiry 2010;47:110–23 [DOI] [PubMed] [Google Scholar]
- 4.Furukawa MF, Raghu TS, Spaulding T, et al. Adoption of health information technology for medication safety in US hospitals, 2006. Healh Affairs 2008;27:865–75 [DOI] [PubMed] [Google Scholar]
- 5.Kazley AS, Ozcan YA. Do hospitals with electronic medical records (EMRs) provide higher quality care? Med Care Res Rev 2008;65:496–513 [DOI] [PubMed] [Google Scholar]
- 6.Kazley AS, Ozcan YA. Electronic medical record use and efficiency: a DEA and windows analysis of hospitals. Socio-Econ Plann Sci 2009;43:209–16 [Google Scholar]
- 7.McCullough JS, Casey M, Moscovice I, et al. The effect of health information technology on quality in US hospitals. Healh Affairs 2010;29:647–54 [DOI] [PubMed] [Google Scholar]
- 8.Menachemi N, Chukmaitov A, Saunders C, et al. Hospital quality of care: does information technology matter? The relationship between information technology adoption and quality of care. Health Care Manage Rev 2008;33:51–9 [DOI] [PubMed] [Google Scholar]
- 9.Zhivan NA, Diana ML. US hospital efficiency and adoption of health information technology. Health Care Manag Sci 2011. Published Online First: Epub Date. doi:10.1007/s10729-011-9179-2 [DOI] [PubMed] [Google Scholar]
- 10.Aqil A, Lippeveld T, Hozumi D. PRISM framework: a paradigm shift for designing, strengthening and evaluating routine health information systems. Health Policy Plann 2009;24:217–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hotchkiss DR, Aqil A, Lippeveld T, et al. Evaluation of the Performance of Routine Information System Management Framework (PRISM): evidence from Uganda. BMC Health Serv Res 2010;10:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Becerra JL. Primer avance hacia el expediente clínico electrónico nacional. Política Digital 2008;45:32–3 [Google Scholar]
- 13.Humpage S. Benefits and costs of electronic medical records: the experience of Mexico's Social Security Institute. Technical Notes No. IDB-TN-122 USA: Inter-American Development Bank, 2010 [Google Scholar]
- 14.Secretaría de Salud Norma Oficial Mexicana NOM-024SSA32010. Que establece los objetivos funcionales y funcionalidades que deberán observar los productos de sistemas de expediente clínico electrónico para garantizar la interoperabilidad, procesamiento, interpretación, confidencialidad, seguridad y uso de estándares y catálogos de la información de los registros electrónicos en salud. Mexico: Diario Oficial de la Federación, 2007 [Google Scholar]
- 15.Instituto Nacional de Salud Pública Evaluación y estrategias de portabilidad y convergencia hacia la integración del SNS. Entregable 5. Informe final de resultados de las entrevistas a responsables de las capacidades y situación operativa de los sistemas de expediente clínico electrónico en los ámbitos estatal y federal. Instituto Nacional de Salud Pública. México: Instituto Nacional de Salud Pública, 2011 [Google Scholar]
- 16.Instituto Nacional de Salud Pública Evaluación y estrategias de portabilidad y convergencia hacia la integración del SNS. Entregable 6. Anexos del informe preliminar de la verificación de las capacidades ECE. Mexico: Instituto Nacional de Salud Pública, 2011 [Google Scholar]
- 17.Dirección General de Información en Salud Base de datos de Estimaciones de población 1990–2012, Colmex. Secondary Base de datos de Estimaciones de población 1990–2012, Colmex http://www.sinais.salud.gob.mx (Consulta: 1 Noviembre 2011)
- 18.Instituto Nacional de Estadistica y Geografia INEGI Sistema Municipal de Bases de Datos. Secondary Sistema Municipal de Bases de Datos (Consulta: 20 octubre 2011)
- 19.Castillo VH, Martínez-García AI, Pulido J. Evaluación y estrategias de portabilidad y convergencia hacia la integración del SNS. BMC Med Inform Decis Mak 2010;10:1–1720067612 [Google Scholar]
- 20.Spencer RJ. Qualitative data analysis for applied policy research. In: Bryman A, Burguess RG, eds. Analyzing qualitative data. New York, USA: Routledge, 1994:173–94 [Google Scholar]
- 21.Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. JOAAG 2009;4:8 [Google Scholar]
- 22.QSR International. NVivo 9.2. Secondary NVivo 9.2 2011.
- 23.iHealthBeat Groups take issue with AMA vote to block ICD-10 rollout. http://www.ihealthbeat.org/about.aspx (accessed 19 Feb 2011)
- 24.Sheikh A, Cornfod T, Barber N, et al. Implementation and adoption of nationwide electronic health records in secondary care in England: final qualitative results from prospective national evaluation in “early adopter” hospitals. BMJ 2011;343:1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res 2010;10:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.del Estado de Colima G Plan Estatal de Desarrollo 2009–2015. http://www.colima-estado.gob.mx/transparencia/archivos/plan_estatal_2009-2015.pdf (accessed 15 May 2011)