Abstract
Context:
Bilateral pediatric cataracts are important cause of visual impairment in children.
Aim:
To study the outcome of bilateral pediatric cataract surgery in young children.
Setting and Design:
Retrospective case series in a tertiary center.
Materials and Methods:
Records of pediatric cataracts operated between January 2001 and December 2003, with a minimum follow-up of 3 months, were reviewed retrospectively.
Statistical Methods:
Independent sample t-test, Fisher's exact test, and logistic regression using SPSS (Statistical Package for Social Science, Chicago, USA) version 12.
Results:
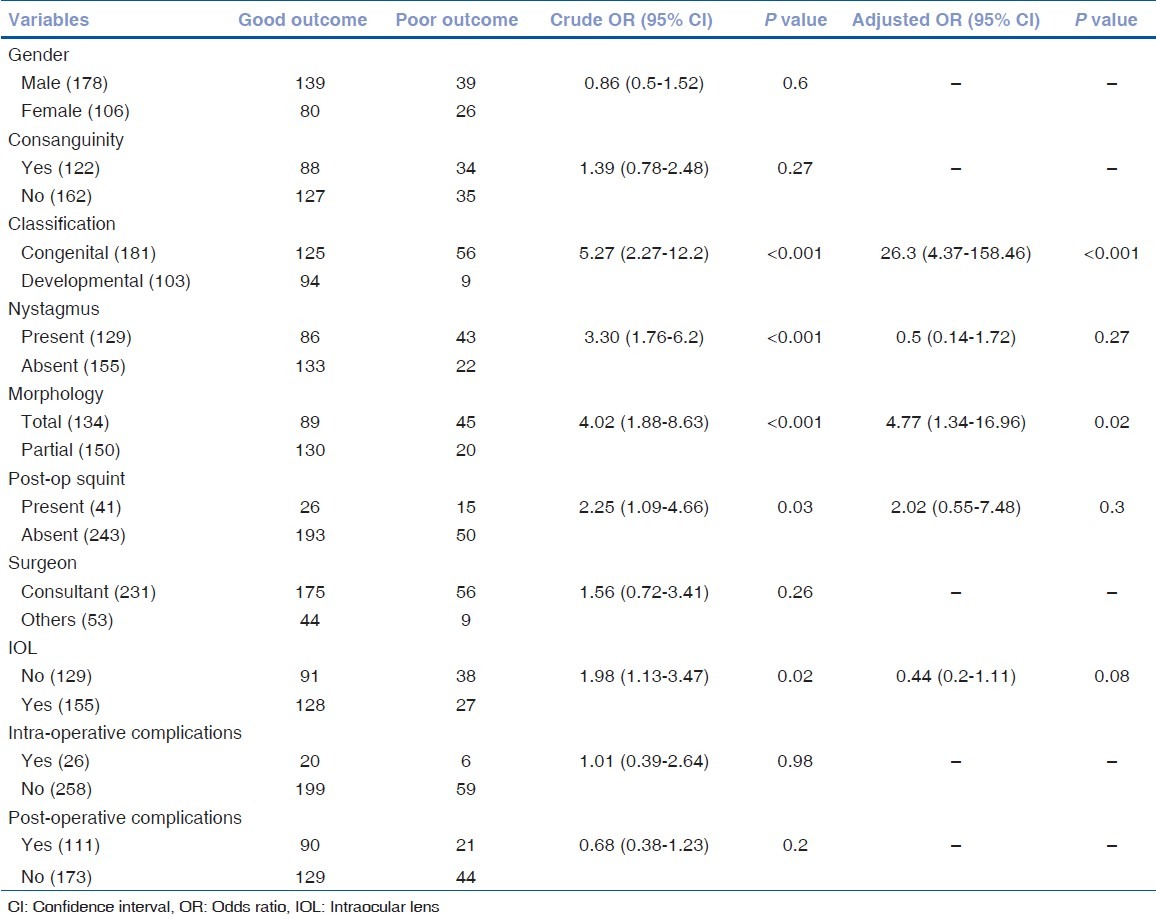
215/257 (83.7%) patients had a minimum follow-up of 3 months. The mean age of presentation to the hospital was 53 months (range: 0-168 months). Congenital cataract was present in 107 patients (58.2%) and developmental cataract in 77 patients (41.8%). The mean age at surgery was 55.2 months (range: 1-168 months). Out of 430 eyes, 269 (62.6%) had an intraocular lens implanted. The mean duration of follow-up was 13.1 months (range: 3-38 months). Pre-operatively, 102 patients (47.3%) had visual acuity <6/60, in the better eye, compared to 37 patients (17.2%) post-operatively (P < 0.001). Eighty-five patients (39.5%) had visual acuity >6/18. The most common early post-operative complication was fibrinous uveitis in 57 eyes (13.3%) and the most common delayed post-operative complication was posterior capsular opacification in 118 eyes (27.4%). The most important prognostic factor for poor outcome was congenital cataract (odds ratio [OR]: 26.3; 95% confidence interval [CI], 4.4-158.5) and total cataract (OR: 4.8; 95% CI, 1.3-17).
Keywords: Childhood blindness, complications, outcome, pediatric cataract, risk factors
Childhood cataract blindness is one of the major avoidable causes of blindness in both developed and developing countries and it is a priority for VISION 2020: The right to sight initiative.[1] The epidemiology of childhood cataract is complicated by the fact that it is not a single disease entity, as it represents a group of etiologies defined by age. Of the 1.4 million blind children, globally, the number due to lens-related conditions is estimated to 190,000 (14%), with proportion varying in different countries.[2–4] Over the past decade, various studies have looked at the outcome of bilateral pediatric cataract,[5–15] but only a few have looked at the outcome of both congenital and developmental cataracts and most of them were small specific series.[6,7,9,12] This study looks at the outcome of bilateral pediatric cataract from a tertiary eye care center in Andhra Pradesh with the objective to document visual outcome and complications of cataract surgery and to analyze the risk factors for poor outcome.
Materials and Methods
Medical records of 257 bilateral pediatric cataracts operated at the Pediatric Ophthalmology Service in the institute over a 3-year period, from 1st January 2001 to 31st December 2003, were reviewed retrospectively. Approval of the Ethics Committee of the Institute was obtained for the data collection. Two hundred and fifteen children (83.7%) with age range from birth to 16 years and having a minimum follow-up of 3 months, after the first eye surgery, were included in the study. Patients with unilateral cataract, traumatic cataract, and having follow-up of less than 3 months were excluded. Medical records were reviewed for demographic, pre-operative, intra-operative, and post-operative information and recorded on the forms using a coding system designed for the study.
Demographic information and history included age at diagnosis, presence or absence of consanguinity, and family history of cataract. Consanguinity was defined as marriage between first, second, or third cousins. Cataract was classified as congenital, if the age of diagnosis was within 1 year of birth and developmental if the age of diagnosis was later.
The method of recording visual acuity varied, depending on the age and cooperation of the child. If optotype methods such as Allen pictures, Teller acuity, or Snellen's chart were unsuccessful, fixation pattern was determined. Other features recorded were intraocular pressure (IOP), presence or absence of nystagmus, squint, morphology of cataract, and other anomalies. Presence or absence of other pathologies responsible for loss of vision was also recorded, either by fundus examination or by a B-scan.
Pre-operative information included the type of surgery, presence or absence of primary posterior capsulotomy (PPC), anterior vitrectomy (AV), intraocular lens (IOL) type and size, method of IOL placement, surgeon profile, and complications. IOL power calculation was done on the basis of keratometry and axial length using the SRK II formula.
Post-operatively, patients routinely received topical steroids, antibiotics, and cycloplegics. Patients were usually seen on day 1, at the first week and after 5-6 weeks. Post-operative complications, method of optical correction, and presence of amblyopia were documented.
Complications were defined as early, if they occurred within 3 months of surgery and delayed if they occurred later. Posterior capsule (PC) rent was deemed to have occurred if it happened prior to the planned commencement of PPC. If the pupillary area showed dull reflex on distant direct ophthalmoscopy and/or on the slit lamp, or examination under anesthesia showed an obvious opacity in central 2 mm of visual area, it was diagnosed as central posterior capsular opacification (PCO). In eyes that developed significant PCO, YAG (yttrium-aluminum-garnet) laser capsulotomy was performed, but in eyes with thick fibrotic capsules or uncooperative children, surgical membranectomy and AV were performed. Glaucoma was confirmed if IOP was more than 20 mm of Hg recorded on three different occasions.
Final outcome was assessed in terms of visual acuity in the better eye at the last post-operative follow-up. For statistical analysis, SPSS version 12 was used. In univariate analysis, for a continuous variable, independent sample t-test was used and for analysis of two categorical variables, the Fisher's exact test or a Chi-square test was used. For multivariate analysis and for odds ratio, logistic regression was used.
Results
Out of 215, 131 (60.9%) patients were boys. The mean age of presentation was 53 months (median, 48 months; range, 0-168 months) and 81 children (37.7%) were within 1 year of age. The mean duration of follow-up was 13.1 months (median, 11 months; range, 3-38 months).
The age of diagnosis could be established in 184 (85.6%) patients; out of which, 58 (31.5%) patients had since birth. The mean age of diagnosis was two and half years (median, 3.5 months; range, 0-167 months). One hundred and seven patients (58.2%) were classified to have congenital cataract and 77 (41.8%) have developmental cataract. History of consanguinity among parents was present in 81 (37.7%) patients. Consanguinity among parents was more common in patients with congenital cataract when compared to developmental cataract (50.5% vs. 30.6%, P = 0.01).
Pre-operative visual acuity was most commonly recorded by the fixation pattern (59.5%) and Snellen's chart (35.3%) [Table 1]. One hundred and two patients (47.4%) had visual acuity less than 6/60 in the better eye (defined as poor fixation or visual acuity less than 6/60) [Fig. 1]. The visual acuity of children having congenital cataract was more likely to be less than 6/60 than those with developmental cataract (69.1% vs. 36.4%, P < 0.001). The mean IOP was 14 mm of Hg (SD = 4.7) in the right eye and 13.8 mm of Hg (SD = 4.2) in the left eye. Three patients had IOP more than 20 mm of Hg. In two of them, it was due to the use of topical steroids and one had associated glaucoma due to congenital rubella syndrome. Nystagmus was present in 77 (35.8%) patients. It was more common in children with congenital cataract than with developmental cataract (74.7% vs. 2.6%, P < 0.001). Squint was present in 31 (14.4%) patients. It was alternating in 19 patients (10 exotropia and 9 esotropia) and unilateral in 12 eyes (11 exotropia and 1 esotropia). Associated anomalies were present in 17 (7.9%) patients: Microphthalmos (nine patients) followed by microcornea (five patients), microphthalmos with coloboma (two patients) and associated congenital glaucoma (one patient). Lens morphology was symmetrical in 140 (65.1%) patients. In patients with symmetrical morphology, the most common was total cataract (57 patients) followed by zonular cataract (28 patients), nuclear cataract (18 patients), posterior sub-capsular cataract (14 patients), posterior lenticonus (six patients), anterior polar (three patients), and membranous (two patients). Further, 12 patients had mixed type of morphology. Children in the congenital group were more likely to have total cataract than children in the developmental group (65.4% vs. 15.8%, P < 0.001).
Table 1.
Pre-operative and post-operative method of recording visual acuity
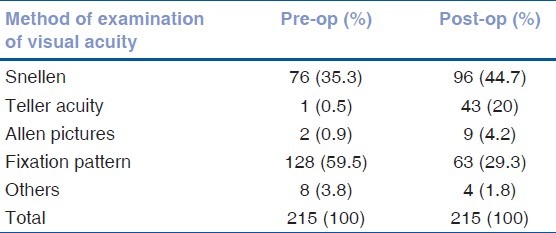
Figure 1.
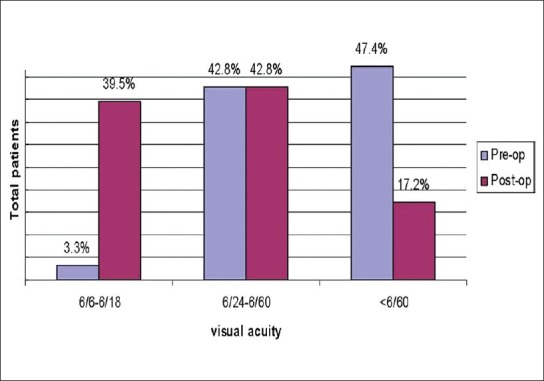
Comparison of pre-operative and post-operative visual acuity
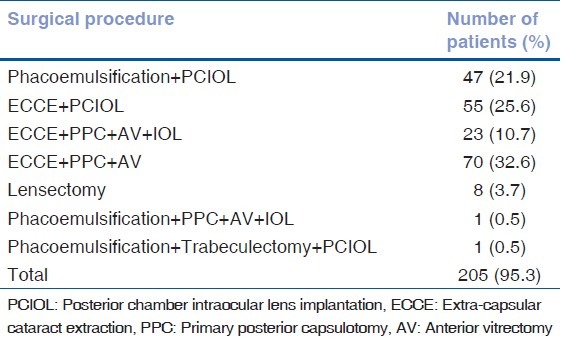
The mean age of surgery was 55.2 months (median, 48 months; range, 1-168 months). The surgical procedure was the same in both eyes in 205 (95.3%) patients [Table 2]. The most common surgical procedure was extra-capsular cataract extraction (ECCE) with PPC with AV (70 patients), followed by ECCE with posterior chamber IOL implantation (55 patients), phacoemulsification with posterior chamber IOL implantation (47 patients), ECCE with PPC with AV with posterior chamber IOL implantation (23 patients), and lensectomy (eight patients). One patient underwent phacoemulsification with PPC with AV with posterior chamber IOL implantation and one underwent phacoemulsification with trabeculectomy posterior chamber IOL implantation. In 10 patients, the surgical procedures performed were different in both eyes.
Table 2.
Surgical procedures in 205 patients
One hundred and thirty-four (62.3%) patients had bilateral IOL implantation. The most common type of IOL implanted was polymethacrylate in 218 eyes (81%) with an overall size of 12 mm (79.2%) and in-the-bag implantation (90.7%). The majority of patients (70.2%) were operated by a consultant. IOL implantation was mainly done for children aged more than 24 months. Only three children had IOL implanted at the age of 1 year.
Post-operatively, visual acuity was most commonly recorded by the Snellen's chart (44.7%) and fixation pattern (29.3%) [Table 1]. 17.2% patients had visual acuity less than 6/60 in the better eye, compared to 46.3% pre-operatively [Fig. 1]. Patients with congenital cataract were more likely to have visual acuity less than 3/60 than patients with developmental cataract (7.6% vs. 0.5%, P < 0.001), especially the ones operated after 1 year of age. The mean IOP was 11.8 mm of Hg (SD = 2.3) in the right eye and 12.1 mm of Hg in the left eye (SD = 2.7). None of the patients had IOP more than 20 mm of Hg. Most common method of optical correction was spectacles (90.7%). Contact lenses were used infrequently due to difficulty with compliance and cost. Amblyopia was present in 133 (262 eyes) patients and was the most common cause for visual impairment or blindness. One hundred and twenty-nine children had bilateral amblyopia and four had unilateral amblyopia. In the bilateral group, 108 were equally amblyopic in the 2 eyes. Amblyopia was significantly more common in cases of congenital cataract than developmental cataract (93% vs. 14.9%, P < 0.001).
Table 3 shows the list of complications. The most common intra-operative complication was posterior capsular rent seen in 33 eyes (7.6%). The most common early post-operative complication was fibrinous uveitis in 57 eyes (13.3%) and the most common delayed post-operative complication seen was PCO seen in 118 eyes (27.4%).
Table 3.
Intra- and Post-operative complications in 430 eyes undergoing cataract surgery
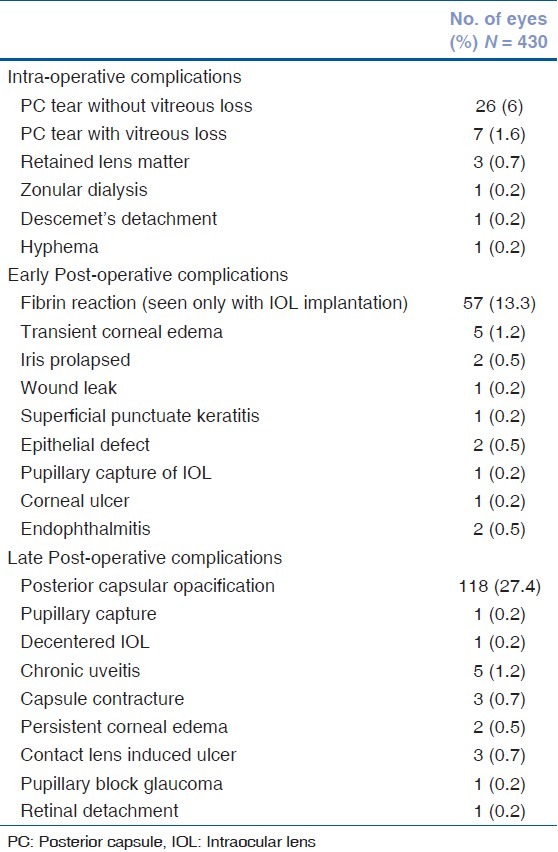
Endophthalmitis occurred in two eyes on the 2nd and 11th post-operative days. Immediate surgical intervention in the form of pars plana vitrectomy with intraocular antibiotics was performed in both cases. One recovered visual acuity of 6/18 and the other had central steady and maintained fixation (CSMF). No organism was detected in both cases.
Of 199 eyes that underwent PPC, PCO occurred in 14 eyes (7%), whereas in 215 eyes without PPC, PCO was seen in 104 eyes (48.4%; P < 0.001). Sixty-nine eyes were treated with YAG laser capsulotomy, six eyes underwent membranectomy and in two eyes, PC polishing was done.
Risk factors for poor outcomes were analyzed. Subjects having follow-up of 6 months or more were included in analysis. Poor outcome was defined as less than 6/60 acuity or poor fixation. Patients having glaucoma pre-operatively were excluded from analysis. Out of 430, 284 (66%) eyes were included for analysis. Two hundred and nineteen (50.9%) eyes had good outcome and 65 eyes (15.1%) had poor outcome. The variables that were analyzed are shown in Table 4. Factors that were significant in univariate analysis were modeled for multivariate analysis. Table 4 shows the crude and the adjusted odds ratio along with the significance level for the variables analyzed. In univariate analysis, presence of nystagmus, squint, total cataract, aphakia, and congenital cataract were significantly associated with poor outcome. In the multivariate analysis, congenital cataract and total cataract remained significant risk factors for poor outcome.
Table 4.
Univariate and multivariate analyses of poor outcome in 284 eyes having surgery for pediatric cataract
Congenital cataract patients, who were operated after first birthday, had significantly more poor outcome than those operated within 1st year of life (44.8% vs. 28.8%, P = 0.02) but, for patients operated within 3 months of birth and those between 3 and 12 months, there was no significant difference in good outcome (73.5% vs. 65.4% P = 0.4).
Surgical intervention on congenital and total cataracts before their first birthday had a better outcome compared to those operated after 1 year (72.2% vs. 38.9%, P = 0.008).
Discussion
Management of childhood cataract remains a challenge and is complicated by the fact that it requires special surgical skills, tends to have more inflammation, and over a period of time has a risk of amblyopia along with change in refractive state of the eye. But in our series, all the children had a significant improvement over their pre-operative visual acuity, included those who were operated late.
In this study, the visual outcome of 39.5% having post-operative visual acuity ≥6/18 is comparable to a study from central India that reported 16.4% having post-operative vision ≥6/18,[16] whereas a study from Pune had 35.5% eyes having post-operative vision ≥6/18,[17] and a series from Nepal that had 36.6% eyes having post-operative vision ≥6/18,[18] but these series included some traumatic cataracts too. We defined CSMF as equivalent to 6/60 or better.[19,20] Post-operatively, there was significant improvement in visual acuity [Fig. 1]. Overall, 17.2% patients had visual acuity less than 6/60 of which 8.9% had visual acuity less than 3/60 in the better eye. This outcome is comparable to results from Nepal[18] and India,[17,16] but poorer than reports from the developed world.[7,10,12,14,15] This could be due to the duration of follow-up being only 11 months or the large proportion of congenital cataracts in our group. It has been shown that in congenital cataracts, operated earlier in life (within 1 year), the visual development continues till the age of 10-12 years.[10] Hence, with a long-term follow-up, these children will, expectedly, have further improvement in their visual acuity. Overall, 39.5% patients achieved visual acuity 6/18 or better in the better eye.
The risk of poor outcome in congenital cataract was nearly 20 times more than for developmental cataract, especially if operated after the age of 1 year. The visual system got the opportunity to develop and mature in the latter before its progress was halted by the development of cataract while the visual system could not develop at all in a dense congenital cataract. Hence, early surgery is important in congenital cataract. Various authors have addressed the issue of timing in case of surgery for bilateral congenital cataract, but controversy persists as early surgery increases the risk of developing subsequent glaucoma and late surgery is associated with deprivation of visual development. In contrast to other authors,[5,8,10,14] we were unable to document any difference in outcome for patients operated within 3 months and those operated between 3 and 12 months. It could be due to the shorter follow-up of patients. But even those who were operated late, nonetheless, improved over their pre-operative visual acuity.
As in other studies,[8,14,15,21] we found that the prognosis was poorer in cases of total cataract with the risk of poor outcome being 4-5 times higher.
The most common early post-operative complication encountered was presence of fibrin reaction (13.3%). It was seen only in eyes that had IOL implantation (20.8%) and occurred within 1-2 weeks of surgery. Similar findings are reported by other authors.[6,9,15] Complications related to IOL implantation were few, possibly due to the use of biocompatible IOLs and in-the-bag implantation in most cases.
Numerous authors have reported PCO rates ranging from 50%[9,22] to nearly 100%,[6,23] if the posterior capsule is left intact. In our series, 48.4% eyes that did not have PPC developed PCO. Only 7% of eyes that had PPC developed opacification of visual axis. Hence, we agree with other authors[24,25] that PPC with AV should be mandatorily done in all children till 6-7 years of age.
Retinal detachment is reported nowadays to be rare with the advances in microsurgical technique and proper management of vitreous loss. We had one case of retinal detachment in a patient who had got YAG laser capsulotomy done.
Though glaucoma is one of the frequent serious complications,[26–28] there were no cases of new glaucoma in our series; however, follow-up was short. A long-term follow-up of these cases will help to establish the incidence of glaucoma.
Amblyopia was the most common cause of visual deprivation, and it was symmetrical in most of the cases. Follow-up at 6 months was available for only 66% of our patients and among those lost to follow-up, 24.3% had poor outcome when seen at 3 months; therefore, there is a need to determine the reasons for failure to attend follow-up and improve future attendance.
Conclusion
Most cases of poor outcome occurred in the congenital cataract group, especially those operated later in life and are attributed to early visual deprivation and attending amblyopia. Early detection and surgery, optical rehabilitation, and close follow-up are essential for good outcome. This is especially crucial in those aged less than 1 year.
Acknowledgements
Dr. Usha Raman for language editing; Sabera Banu for library assistance; and all the children whose records were reviewed in this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Thylefors B. A global initiative for the elimination of avoidable blindness. Community Eye Health. 1998;11:1–3. [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Geneva: WHO; 2000. Preventing blindness in children: report of WHO/IAPB scientific meeting. Programme for prevention of blindness and deafness and International Agency for prevention of blindness. [Google Scholar]
- 3.Elder MJ, De Cock R. Childhood blindness in the West Bank and Gaza Strip: Prevalence, aetiology and hereditary factors. Eye (Lond) 1993;7:580–3. doi: 10.1038/eye.1993.126. [DOI] [PubMed] [Google Scholar]
- 4.Rogers NK, Gilbert CE, Foster A, Zakhidov BO, McCollum CJ. Childhood blindness in Uzbekistan. Eye (Lond) 1999;13:65–70. doi: 10.1038/eye.1999.13. [DOI] [PubMed] [Google Scholar]
- 5.Bradford GM, Keech RV, Scott WE. Factors affecting visual outcome after surgery for bilateral congenital cataracts. Am J Ophthalmol. 1994;117:58–64. doi: 10.1016/s0002-9394(14)73015-6. [DOI] [PubMed] [Google Scholar]
- 6.Cassidy L, Rahi J, Nischal K, Russell-Eggitt I, Taylor D. Outcome of lens aspiration and intraocular lens implantation in children aged 5 years and under. Br J Ophthalmol. 2001;85:540–2. doi: 10.1136/bjo.85.5.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eckstein M, Vijayalakshmi P, Gilbert C, Foster A. Randomised clinical trial of lensectomy versus lens aspiration and primary capsulotomy for children with bilateral cataract in south India. Br J Ophthalmol. 1999;83:524–9. doi: 10.1136/bjo.83.5.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gelbart SS, Hoyt CS, Jastrebski G, Marg E. Long-term visual results in bilateral congenital cataracts. Am J Ophthalmol. 1982;93:615–21. doi: 10.1016/s0002-9394(14)77377-5. [DOI] [PubMed] [Google Scholar]
- 9.Gimbel HV, Basti S, Ferensowicz M, DeBroff BM. Results of bilateral cataract extraction with posterior chamber intraocular lens implantation in children. Ophthalmology. 1997;104:1737–43. doi: 10.1016/s0161-6420(97)30033-5. [DOI] [PubMed] [Google Scholar]
- 10.Magnusson G, Abrahamsson M, Sjöstrand J. Changes in visual acuity from 4 to 12 years of age in children operated for bilateral congenital cataracts. Br J Ophthalmol. 2002;86:1385–9. doi: 10.1136/bjo.86.12.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O′Keefe M, Mulvihill A, Yeoh PL. Visual outcome and complications of bilateral intraocular lens implantation in children. J Cataract Refract Surg. 2000;26:1758–64. doi: 10.1016/s0886-3350(00)00561-7. [DOI] [PubMed] [Google Scholar]
- 12.Peterseim MW, Wilson ME. Bilateral intraocular lens implantation in the pediatric population. Ophthalmology. 2000;107:1261–6. doi: 10.1016/s0161-6420(00)00141-x. [DOI] [PubMed] [Google Scholar]
- 13.Rabiah PK, Smith SD, Awad AH, Al-garni A, Al-mesfer SA, Al-turkmani S. Results of surgery for bilateral cataract associated with sensory nystagmus in children. Am J Ophthalmol. 2002;134:586–91. doi: 10.1016/s0002-9394(02)01645-8. [DOI] [PubMed] [Google Scholar]
- 14.Wright KW, Christensen LE, Noguchi BA. Results of late surgery for presumed congenital cataracts. Am J Ophthalmol. 1992;114:409–15. doi: 10.1016/s0002-9394(14)71850-1. [DOI] [PubMed] [Google Scholar]
- 15.Yorston D, Wood M, Foster A. Results of cataract surgery in young children in east Africa. Br J Ophthalmol. 2001;85:267–71. doi: 10.1136/bjo.85.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khandekar R, Sudhan A, Jain BK, Shrivastav K, Sachan R. Pediatric cataract and surgery outcomes in Central India: A hospital based study. Indian J Med Sci. 2007;61:15–22. [PubMed] [Google Scholar]
- 17.Gogate P, Khandekar R, Shrishrimal M, Dole K, Taras S, Kulkarni S, et al. Delayed presentation of cataracts in children: Are they worth operating upon? Ophthalmic Epidemiol. 2010;17:25–33. doi: 10.3109/09286580903450338. [DOI] [PubMed] [Google Scholar]
- 18.Thakur J, Reddy H, Wilson ME, Jr, Paudyal G, Gurung R, Thapa S, et al. Pediatric cataract surgery in Nepal. J Cataract Refract Surg. 2004;30:1629–35. doi: 10.1016/j.jcrs.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 19.Derick RJ, Leguire LE, Rogers GL, Bremer DL. The predictability of infant visual-evoked response testing on future visual acuity. Ann Ophthalmol. 1990;22:432–8. [PubMed] [Google Scholar]
- 20.Laws D, Noonan CP, Ward A, Chandna A. Binocular fixation pattern and visual acuity in children with strabismic amblyopia. J Pediatr Ophthalmol Strabismus. 2000;37:24–8. doi: 10.3928/0191-3913-20000101-07. [DOI] [PubMed] [Google Scholar]
- 21.Parks MM. Visual results in aphakic children. Am J Ophthalmol. 1982;94:441–9. doi: 10.1016/0002-9394(82)90237-9. [DOI] [PubMed] [Google Scholar]
- 22.Brady KM, Atkinson CS, Kilty LA, Hiles DA. Glaucoma after cataract extraction and posterior chamber lens implantation in children. J Cataract Refract Surg. 1997;23:669–74. doi: 10.1016/s0886-3350(97)80052-1. [DOI] [PubMed] [Google Scholar]
- 23.Knight-Nanan D, O'Keefe M, Bowell R. Outcome and complications of intraocular lenses in children with cataract. J Cataract Refract Surg. 1996;22:730–6. doi: 10.1016/s0886-3350(96)80312-9. [DOI] [PubMed] [Google Scholar]
- 24.Basti S, Ravishankar U, Gupta S. Results of a prospective evaluation of three methods of management of pediatric cataracts. Ophthalmology. 1996;103:713–20. doi: 10.1016/s0161-6420(96)30624-6. [DOI] [PubMed] [Google Scholar]
- 25.Wilson ME, Pandey SK, Thakur J. Paediatric cataract blindness in the developing world: Surgical techniques and intraocular lenses in the new millennium. Br J Ophthalmol. 2003;87:14–9. doi: 10.1136/bjo.87.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egbert JE, Wright MM, Dahlhauser KF, Keithahn MA, Letson RD, Summers CG. A prospective study of ocular hypertension and glaucoma after pediatric cataract surgery. Ophthalmology. 1995;102:1098–101. doi: 10.1016/s0161-6420(95)30906-2. [DOI] [PubMed] [Google Scholar]
- 27.Mills MD, Robb RM. Glaucoma following childhood cataract surgery. J Pediatr Ophthalmol Strabismus. 1994;31:355–60. doi: 10.3928/0191-3913-19941101-03. [DOI] [PubMed] [Google Scholar]
- 28.Parks MM, Johnson DA, Reed GW. Long-term visual results and complications in children with aphakia. A function of cataract type. Ophthalmology. 1993;100:826–40. doi: 10.1016/s0161-6420(93)31566-6. [DOI] [PubMed] [Google Scholar]


