Abstract
To evaluate the safety and efficacy of iris claw intraocular lens (IOL) implantation for correction of monocular surgical aphakia in eyes with no capsular support. This is a prospective interventional case series of 30 eyes of monocular surgical aphakia. Patients underwent posterior iris claw implantation 4 weeks after the primary surgery. Aphakia which resulted due to posterior capsular rupture, large zonulo-dialysis (>180°) and cases of intracapsular cataract extraction in subluxated cataractous lens (>180°) where a posterior chamber IOL could not be placed were included in this study. Postoperatively, best-corrected visual acuity (BCVA) improved significantly (P < 0.02), 80% of patients had good vision of (20/20 to 20/40) and endothelial cell loss was 8.96% at 6 months. Secondary iris claw intraocular lens implantation is a viable option to correct monocular aphakia in eyes without capsular support.
Keywords: Iris claw enclaving, lens extraction, surgical aphakia
Aphakia comes from two Greek words: “a” meaning “none” and “phacos” meaning “lens.” In aphakia, there is no crystalline lens inside the eye.[1] Options available for the surgeon to correct aphakia are glasses, contact lens, keratorefractive surgery, and intraocular lens (IOL). The various IOLs available are 1) anterior chamber IOL (ACIOL), 2) scleral fixated IOL and 3) iris fixated IOL, both anterior and posterior.[2,3] In our series, the patients underwent posterior iris claw lens implantation. ACIOLs have high risk of corneal decompensation. In scleral fixated lenses, surgery is technically more difficult. Between the iris fixated IOLs, we preferred posterior chamber iris fixated IOLs because of retropupillary position and lower risk of endothelial decompensation.[4]
Materials and Methods
This study was conducted between January 2009 and July 2010. This is a prospective interventional case series with 30 eyes of 30 patients of the age group 30–75 years. Inclusion criteria were patients with monocular surgical aphakia with no capsular support with endothelial counts more than 1000 cells, visual acuity of 20/200 or better with plus 10 Diopters on Snellen chart. Exclusion criteria were patients with binocular surgical aphakia, surgical aphakia with decompensated corneas, aphakic patients with posterior segment pathologies like cystoid macular edema, choroidal neovascular membrane, etc., and aphakic patients with insufficient iris tissue.
Preoperatively, all patients underwent complete ophthalmologic evaluation including uncorrected visual acuity (UCVA), subjective refraction, and best-corrected visual acuity (BCVA). The measurements taken were as follows:
Slit-lamp examination with emphasis on position of previous surgical peripheral iridectomy and pupil.
Keratometry and A scan
A constant used for IOL power calculation is 117.0 and SRK/T formula was used.
Retinal evaluation with 90 D and indirect ophthalmoscopy.
Endothelial cell density (ECD) by specular microscopy
Goldmann applanation tonometry
The posterior iris claw lens was implanted as a secondary procedure 4 weeks after the first surgery. As the primary surgery was done in an outreach setup, where all surgeons were not adequately trained to implant the claw lens, the claw lens implantation had to be taken up as a secondary procedure by an experienced surgeon. Conjunctiva was separated from adhesions, exposing the previous temporal scleral section, and the tunnel was opened with the iris repositer. The anterior chamber was formed with viscoelastic substance. If vitreous was noted in the anterior chamber, automated vitrectomy was done. Two side ports are made diagonally opposite, i.e. at 6 o′ clock and 12 o′ clock positions. Iris claw IOL was introduced into the anterior chamber such that haptics were in line with the side ports. Holding the optic of the lens with a lens forceps, one haptic was pushed under the iris with gentle manipulation. Simultaneously, dialor was passed through the paracentesis on the same side and enclaving done. End point was noting the dimple at the site of enclavation. Similarly, haptic encalvation in the other side was done. Section was sutured with one interrupted 10-0 nylon and the conjunctiva with 8-0 vicryl. Postoperatively, topical steroid antibiotics in a tapering schedule over 6 weeks were given. The iris claw lens used in this study was of Excel Optics (Chennai Model No: PIC 5590, SIC 4280P) [Fig. 1].
Figure 1.

Posterior Iris Claw Lens Excel Optics, Model No: PIC 5590
Results
This study comprised 30 eyes of 30 patients with monocular surgical aphakia. The statistical analysis was done with SSPSS 16.0. The mean age of the patients was 57 ± 10 (range 30–75) years; majority of patients (50% of the cases) were in the age group 60–70 years. The ratio of male and female patients in the study was equal, with 15 patients in each sex; laterality was almost equal in the patients, with RE 56% and LE 44%. The ECD changes after 6 months was statistically significant with P value <0.05. The mean preoperative cell density (aphakia) was1597.43 and postoperative cell density at 6 months was 1368.23, with a mean difference of 52.196. Percentage of endothelial cell loss was 8.94% (P value 0.002). Visual outcome at 6 months was as per the WHO guidelines. Majority, i.e. 80% of patients, had visual acuity of 20/40 or better. None of our patients developed any major complications like cystoid macular edema, bullous keratopathy or retinal detachment.
Discussion
In aphakic patients, spectacle correction is associated with reduced peripheral vision,[2] image magnification of 20–35%, etc. Surgical correction with IOL implantation can overcome these problems. Over the years, surgical aphakia has become less common. However, aphakia can still be encountered as a complication of cataract surgery where there is insufficient capsular support to place posterior chamber IOL.[5] Among the IOLs in cases of no capsular support, ACIOLs have high risk of corneal decompensation, and with scleral fixated lenses, surgery is technically more difficult even though they show good results.[6] We used the posterior chamber iris fixated IOL because of retropupillary position and lower risk of endothelial decompensation [Fig. 2].
Figure 2.
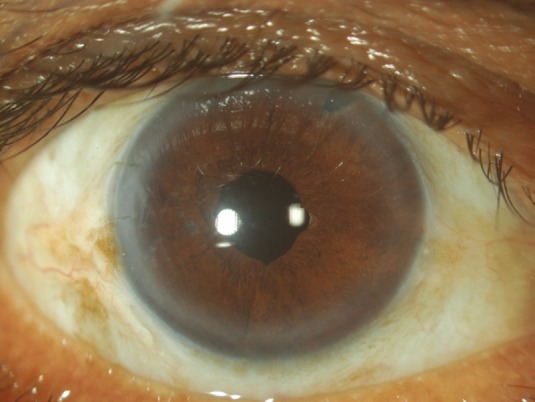
Post-operative 6 Weeks. Note the round pupil & surgical peripheral iridectomy at 11 “O” position
Patients were followed up for 6 months; the two main parameters we checked were BCVA and ECD. Postoperatively, at the end of 6 months, majority of our patients, i.e. 80%, had BCVA vision of 20/20 to 20/40[7] and endothelial cell loss was 8.96%. No significant surgical complications like raised intraocular pressure and cystoid macular edema were seen in our series. In all of our cases, IOL remained well centered until the end of the follow-up period [Fig. 3]. Some limitations of our study were short follow-up for ECD measurements and lack of data about other important parameters like coefficient of variation and percentage of hexagonal cells. To the best of our knowledge, there are no similar studies with the same IOL model (Excel Optics, Chennai Model No: PIC 5590, SIC 4280P). The retropupillary iris claw lens has the advantages of a true posterior chamber IOL with low intra- and postoperative complications. The implantation process with this technique is simple. We believe it is a better option than a scleral-fixated or an angle-fixated IOL.
Figure 3.
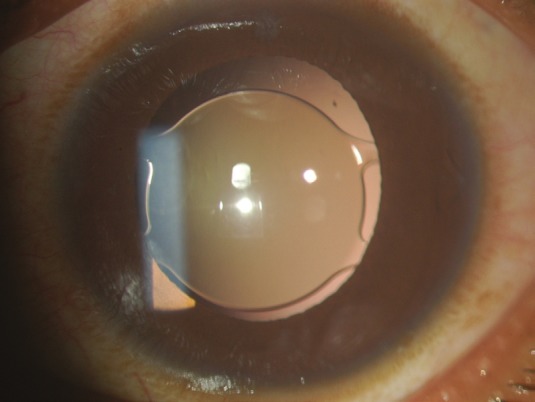
Note the well centered posterior iris claw lens after pupillary dilatation
Conclusion
Secondary iris claw IOL implantation is a viable option to correct monocular surgical aphakia in eyes without capsular support.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Alpar J. Present state of management of aphakia. Future of spectacles and contact lenses. Indian J Ophthalmol. 1989;37:54–7. [PubMed] [Google Scholar]
- 2.Gicquel JJ, Langman ME, Dua HS. Iris claw lenses in aphakia. Br J Ophthalmol. 2009;93:1273–5. doi: 10.1136/bjo.2009.159871. [DOI] [PubMed] [Google Scholar]
- 3.Heng LK, Tseng PS, Yong V. Current and future trends in the correction of aphakia. Ann Acad Med Singapore. 1989;18:171–3. [PubMed] [Google Scholar]
- 4.Baykara M, Ozcetin H, Yilmaz S, Timuçin OB. Posterior iris fixation of the iris-claw intraocular lens implantation through a scleral tunnel incision. Am J Ophthalmol. 2007;144:586–91. doi: 10.1016/j.ajo.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Rumelt S, Rehany U. The influence of surgery and intraocular lens implantation timing on visual outcome in traumatic cataract. Graefes Arch Clin Exp Ophthalmol. 2010;248:1293–7. doi: 10.1007/s00417-010-1378-x. [DOI] [PubMed] [Google Scholar]
- 6.Lundvall A, Weeber H, Jr, Jeeves M. Sulcus fixation without capsular support in children. Cataract Refract Surg. 1999;25:776–81. doi: 10.1016/s0886-3350(99)00043-7. [DOI] [PubMed] [Google Scholar]
- 7.Condon GP, Masket S, Kranemann C, Crandall AS, Ahmed II. Small-incision iris fixation of foldable intraocular lenses in the absence of capsule support. Ophthalmology. 2007;114:1311–8. doi: 10.1016/j.ophtha.2007.04.018. [DOI] [PubMed] [Google Scholar]


