Abstract
Expulsive suprachoroidal hemorrhage can be surgical or spontaneous. Spontaneous expulsive suprachoroidal hemorrhage (SESCH) is a rare entity. Most of the reported cases of SESCH were caused by a combination of corneal pathology and glaucoma. We are reporting a rare presentation of SESCH with no pre-existing glaucoma or corneal pathology and caused by massive intra- and peri-ocular hemorrhage due to decompensated liver disease.
Keywords: Liver disease, spontaneous expulsive hemorrhage, suprachoroidal
Spontaneous expulsive choroidal hemorrhage is a serious ocular condition where expulsion of the intraocular contents occurs through the anterior eye wall. Very few reports of this condition exist in the literature.[1–4] The predisposing factors of this rare condition are age more than 60 years, arteriosclerosis, vascular disease, glaucoma, diseased eye wall with thinning, and intra-ocular malignancies.[5,6]
We are reporting a case of a spontaneous expulsive suprachoroidal hemorrhage (SESCH) caused by bleeding diathesis secondary to decompensated liver disease.
Case Report
A 57-year-old Female patient who was admitted for decompensated cirrhosis of liver developed sudden onset of ocular pain associated with loss of vision. Ocular examination revealed peribulbar hemorrhage, lid edema, conjunctival congestion with chemosis, and mild (2 mm) proptosis. Perception of light was absent. Cornea was clear. Anterior chamber was of normal depth with a 2 mm hyphema. Fresh Vitreous hemorrhage with no view of fundus was noted, and the intraocular pressure was 44 mmHg. Left eye examination was normal. Patient denied history of trauma of any nature and had no past history of any ocular ailment.
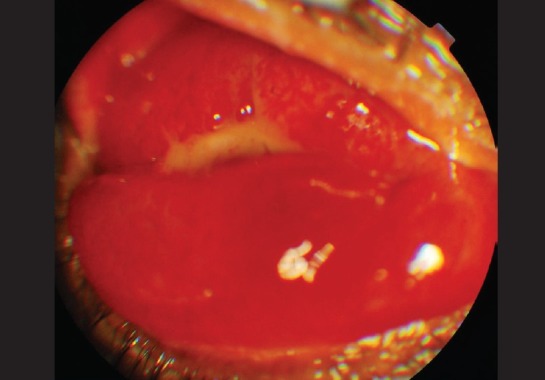
The patient was started on timolol 0.5% eye drops and oral Acetazolamide 250 mg 6 hourly. After 24 hours, on review, the patient was found to have perforation at the inferior limbus with prolapse of iris tissue and total hyphema [Fig. 1]. Fresh bleeding was noted from the perforation. Pressure patch was applied, and the patch was found soaked with blood within 30 minutes. An emergency evisceration was planned, but surgery could not be done because of bleeding diathesis. Prothrombin time (PT) was 23.2 sec. in test vs. 14 sec. in control with international normalized ratio (INR) of 2.15, for which blood transfusion was commenced. But, by 24 hours, there was spontaneous expulsion of intra-ocular contents with the crystalline lens found expelled out [Fig. 2]. The hemorrhage arrested spontaneously, and the eyeball became phthisical [Fig. 3]. Computerized tomography scan of the orbit showed a collapsed and deformed globe with absence of crystalline lens [Fig. 4].
Figure 1.
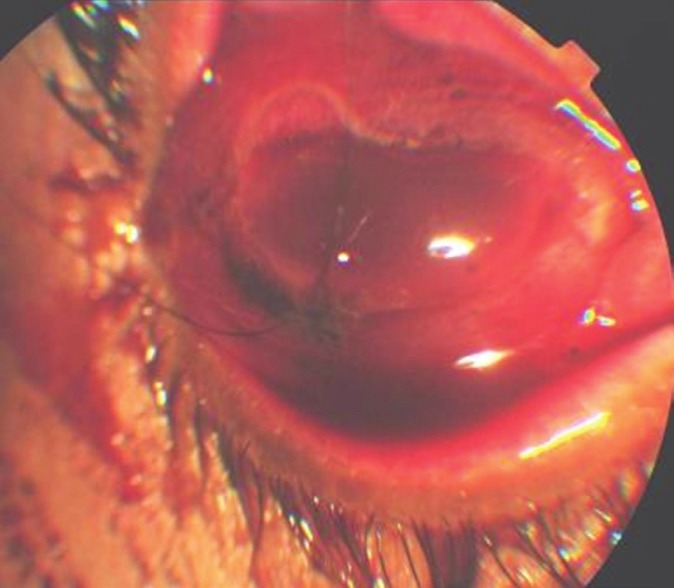
Collapsed globe with inferior limbal perforation with iris prolapse and hyphema
Figure 2.

Expulsive hemorrhage with crystalline lens extruded out
Figure 3.
Phthisical eye with large sub-conjunctival hemorrhage
Figure 4.

Computerized tomography scan showing collapsed globe
Discussion
Expulsive supra choroidal hemorrhage is of 2 types, surgical and spontaneous. The 3 possible mechanisms of supra choroidal hemorrhage are sudden decompression causing rupture of posterior ciliary arteries,[7] acute inflammatory necrosis of the choroidal vessel wall,[8] and a third mechanism of hemorrhages from posterior ciliary artery as the primary event.[9] Necrosis or rupture of posterior ciliary arteries can be induced by hypertension, arteriosclerosis, or glaucoma.[7] Most of the reported cases of SESCH had glaucoma with corneal ulceration predisposing to the supra choroidal hemorrhage.[2–4] But, Sudhir et al. reported a 54-years-old diabetic patient with spontaneous expulsive choroidal hemorrhage who had a normal cornea, except for blood staining documented on the day before the patient developed SESCH.[1] They postulated that an elevated intra-ocular pressure with possible weakening of cornea caused by blood staining would have caused the globe rupture. Similarly, our patient also had an intact cornea on the day before she developed SESCH though she had a 2 mm hyphema. Ophir et al. have suggested that difference in elasticity of the cornea at the limbus makes it vulnerable to perforation at this site.[2] In their case report, a central corneal ulcer was complicated by an annular rupture at the limbus due to SECH. Yang et al. reported the management and outcome of 5 cases of spontaneous choroidal hemorrhage without expulsion.[10] Of these, 3 were on anti-coagulant therapy. Our patient had bleeding diathesis predisposed by liver failure with prolonged PT. The possible sequence of events in this case could be the bleeding diathesis secondary to the liver disease resulted in a massive intra-ocular and peri-ocular hemorrhage with sudden elevated intra-ocular pressure. The inferior limbal perforation was possibly caused by dellen due to chemosis or exposure keratopathy due to proptosis.
Amarapurkar et al. have suggested that global evaluation of coagulation like thrombin generation time, thromboelastography, sonorheometry, and national normalized ratio calibrated for cirrhosis (INRliver) are more relevant to study coagulopathy in liver disease since there is reduction in both anti and procoagulant factors.[11] In the case being reported, we carried out only the routine PT (the facility for which was available in our hospital) as per the management protocol devised by the treating physician. Decompensated liver disease was the only predisposing factor we could identify in the present case as cause of SESCH.
We are reporting this case for its unique presentation in that the patient had no corneal pathology or pre-existing glaucoma prior to the expulsion while other reports suggest some form of corneal pathology and glaucoma. Also, it is the first case of SESCH caused by bleeding diathesis secondary to decompensated liver disease to be reported in literature.
Footnotes
Source of Support: Nil,
Conflict of Interest: None
References
- 1.Sudhir RR, Rao SK, Biswas J, Padmanabhan P. Spontaneous expulsive suprachoroidal hemorrhage. Cornea. 2002;21:632–3. doi: 10.1097/00003226-200208000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Ophir A, Pikkel J, Groisman G. Spontaneous expulsive suprachoroidal hemorrhage. Cornea. 2001;20:893–6. doi: 10.1097/00003226-200111000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Martorina M. Spontaneous corneal perforation with expulsive hemorrhage. Ann Ophthalmol. 1993;25:324–5. [PubMed] [Google Scholar]
- 4.Lam A, Faye M, Borzeix A. Spontaneous expulsive hemorrhage after total necrosis of the cornea. Apropos of 3 cases. J Fr Ophtalmol. 1991;14:643–6. [PubMed] [Google Scholar]
- 5.Winslow RL, Stevenwon W, Yanoff M. Spontaneous expulsive choroidal hemorrhage. Arch Ophthalmol. 1974;92:33–6. doi: 10.1001/archopht.1974.01010010037009. [DOI] [PubMed] [Google Scholar]
- 6.Pery HD, Hsieh RC, Evans RM. Malignant melanoma of the choroid associated with spontaneous expulsive choroidal hemorrhage. Am J Ophthalmol. 1977;84:205–8. doi: 10.1016/0002-9394(77)90853-4. [DOI] [PubMed] [Google Scholar]
- 7.Manschot WA. The pathology of expulsive hemorrhage. Am J Ophthalmol. 1955;40:15–24. [PubMed] [Google Scholar]
- 8.Pe′er J, Weiner A, Vidauri L. Clinicopathologic report of spontaneous expulsive hemorrhage. Ann Ophthalmol. 1987;19:139–41. [PubMed] [Google Scholar]
- 9.Manschot WA. Telangiectatic granulomas in an eye with spontaneous expulsive hemorrhage. Am J Ophthalmol. 1957;43:872–9. doi: 10.1016/0002-9394(57)91788-9. [DOI] [PubMed] [Google Scholar]
- 10.Yang SS, Fu AD, McDonald HR, Johnson RN, Ai E, Jumper JM. Massive spontaneous choroidal hemorrhage. Retina. 2003;23:139–44. doi: 10.1097/00006982-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Amarapurkar PD, Amarapurkar DN. Management of coagulopathy in patients with decompensated liver cirrhosis. Int J Hepatol. 2011;2011:695470. doi: 10.4061/2011/695470. [DOI] [PMC free article] [PubMed] [Google Scholar]


