Abstract
Objective
This study examined group differences in ratings of amounts of food at the threshold of what is considered “unusually large” to develop empirically derived definitions of binge eating criteria for bulimia nervosa and binge eating disorder.
Method
Groups included undergraduate students, community members, and participants from an eating disorder (ED) longitudinal study. Data were collected via self-report questionnaires.
Results
Ordinal logistic regression indicated that males reported a higher threshold for amounts of food compared to females. Overweight participants from the student and ED samples, but not from the community sample, reported higher thresholds. The presence of binge eating and fear of weight gain were also associated with higher thresholds.
Discussion
These findings provide evidence that gender, social context, BMI, and eating disorder status are important considerations in determining what is an unusually large amount of food. Future diagnostic guidelines should consider the importance of these factors when defining binge eating.
Keywords: binge eating, food amount, eating disorder diagnosis, bulimia nervosa, binge eating disorder
Introduction
Diagnostic criteria for both bulimia nervosa (BN) and binge eating disorder (BED) published in the Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text revision1 require the presence of binge eating (BE). The criteria define binge eating as “eating, in a discrete period of time (e.g., within any 2-h period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances” and which is accompanied by “a sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating) (p. 594).” Although the validity of the DSM-IV-TR definition of binge eating (BE) has been disputed,2 drafts of the proposed criteria for DSM-5 have retained the DSM-IV definition of BE.3
Empirical support of these criteria has been inconsistent. A number of previous studies have provided empirical evidence for loss of control (LOC) as a distinguishing factor between clinically significant and non-significant BE.4–6 In contrast, less attention has been given to quantifying the amount of food that is required to indicate clinically significant BE.7 Some researchers have even asserted that the size criterion is unnecessary in defining clinically significant BE.8,9 One particular issue that may have contributed to problems in establishing the validity of the size criterion is the lack of consensus of an exact threshold for determining amounts of food that are “definitely larger” than most people would eat. As Wilson7 wrote in 1992, which remains true to date, there still is “no widely accepted cut-off for determining what constitutes a large binge.” Although unpublished lists (C.G. Fairburn, personal communication, March 23, 2010) specifying the amount of food that is required to consider an episode of overeating objectively large have often been employed in scoring the Eating Disorder Examination (EDE),10 these amounts have not been empirically derived or validated using data from clinical or community samples.
In an attempt to establish empirical thresholds of objectively large BE, Greeno et al.11 examined subjective ratings of obese women with BED and weight matched control women. They used structured interviews to understand at what point an amount of food would “shift from not a binge to a binge” and amounts participants would label out of control. The authors reported that obese women with and without diagnoses of BED did not differ significantly in their estimates of binge size amounts. This study is notable for attempting to establish empirical thresholds of what is regarded as large among obese binge eaters and weight matched controls. However, the extent to which these findings generalize to more heterogeneous eating disorder and community samples is unclear.
The main objective of the current investigation was to systematically evaluate the threshold at which individuals from both clinical and community samples rated amounts of food as unusually large. Specifically, we sought to examine self-reported threshold definitions of unusually large amounts of food consumption in college student, community, and ED samples. Demographic variables were evaluated to understand the potential role of gender, age, and body mass index (BMI) in influencing ratings of self-reported binge size threshold amounts. Eating and body image variables including dietary restraint, binge eating frequency, hunger, and fear of weight gain were also examined to determine their influence on the self-reported threshold amount at which food sizes are rated as reaching “unusually large.”
Method
Participants
Participants were recruited from three different samples. The student sample (n = 91) included male and female undergraduate psychology students seeking course points for participating in research projects. The community sample (n = 194) included male and female community members who were recruited with advertisements. The Questionnaire on Eating and Weight Patterns-Revised (QEWP-R, described below) was used to identify participants in the student and community samples who self-reported symptoms meeting criteria for full threshold DSM-IV ED diagnoses; seven cases were identified in the community sample.a The ED sample (n = 67) consisted of females participating in an ED study of the long-term course of full and sub-threshold eating disorders.12,13 As described previously, participants had one of the following diagnoses at baseline based on the EDE: anorexia nervosa (AN), BN, BED, or eating disorder not otherwise specified (ED NOS) defined specifically as sub-threshold AN, BN, or BED. For compensation, students received course credit and community and ED participants received 10 dollars for their participation.
Procedure
This research was approved by the Institutional Review Board at the University of Minnesota. After questionnaires were completed, each participant was weighed and their height was measured by research staff to determine BMI.
Measures
The Questionnaire on Eating and Weight Patterns-Revised (QEWP-R)14 assessed eating disorder symptoms and weight and dieting history. The QEWP-R is a self administered measure designed to assess the presence or absence and frequency of diagnostic features of eating disorders.1 This questionnaire has been widely used and found to have acceptable levels of reliability and validity.15,16 The Eating Patterns Questionnaire is a 47-item scale that was designed to assess amounts of various types of food as reaching the threshold of unusually large. Specifically, participants were asked to circle the “largest quantity of the given food [they] would eat within a 2-h period that would not be an unusually large amount of food for [them] to eat.” If the amount of a specific food was not listed, participants were instructed to write in their own response.
Example from Eating Patterns Questionnaire
Dessert—Chocolate (Chocolate covered bar, e.g., Snickers®)
a) 1 2 3 4 5 _______ OTHER
Among the foods included in this survey, seven were selected for analyses in order to include foods that are typically included in binge eating episodes13: bread or toast (with or without butter/jam), chocolate covered candy bars (e.g., Snickers®), 8 oz. chocolate candy bar (e.g., Hershey’s Chocolate Bar®), small hamburger (fast food single patty with or without cheese), large hamburger (fast food: BigMac®, Quarterpounder®, Whopper®, Double Cheeseburger®), sheet cake (9” × 13”, 12 pieces) and layer cake (double layer, 9”, eight pieces). These items included a range of choices equidistant from each other and with a normative choice placed at the center of choices. The center choice was that recommended by guidelines accompanying the ‘gold standard’ in eating disorders interviews (Fairburn, personal communication).17
Statistical Analyses
Analyses were conducted in three stages. First, means and standard errors for each food amount were calculated by sample. Second, responses were combined to examine whether age, gender, or BMI influenced perceived thresholds. For each variable, models were created using ordinal logistic regression with an exchangeable correlation matrix to account for repeated measures. However, because the ED sample had only women and the college sample had little diversity in age, these variables were not included for their corresponding models. Age was treated as a continuous measure, whereas gender was categorical and BMI was categorized as underweight (<18.5), normal (18.5–25), and overweight (>25). Third, cognitive and behavioral factors that may influence perceived binge size were examined. These variables from the QEWP-R were based on participants’ responses regarding current hunger at the time of completing the questionnaire, and endorsement of the following over the past month: dietary restraint, fear of weight gain, binge eating frequency, and feelings of LOC. Again for each sample, ordinal logistic regression models were created to examine whether ratings participants made on cognitive and behavioral factors affected responses. Each of these models was adjusted for age, gender, and BMI for the appropriate samples.
Results
Significant differences were found for gender, with males reporting higher threshold amounts than females. For instance, in the community group males reported an average of 1.9 small hamburgers and females reported 1.3 small hamburgers as the largest amount they would eat that would not be unusually large. In the college group, males averaged 2.9 pieces of sheet cake and females reported on average 1.6 pieces of sheet cake (see Fig. 1). Demographic information for the three study samples is displayed in Table 1.
FIGURE 1.
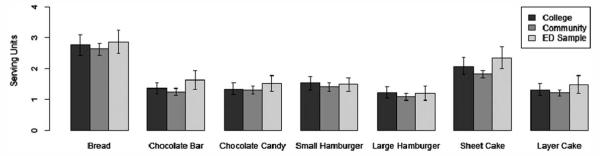
Thresholds for “unusually large” food amounts (in units).
TABLE 1.
Participant demographic characteristics
| Students | Community | Eating Disorder | |
|---|---|---|---|
| n | 91 | 194 | 67 |
| Age (mean) | 20.4 | 28.5 | 37.9 |
| Age ranges | 17–27 | 18–56 | 19–61 |
| Female (%) | 63.7 | 76.8 | 100.0 |
| Caucasian (%) | 75.8 | 86.1 | 100.0 |
| BMI | n = 83a | n = 169a | n = 63a |
| <18.5 (%) | 2.4 | 3.6 | 11.1 |
| 18.5–25 (%) | 75.9 | 62.7 | 23.8 |
| >25 (%) | 21.7 | 33.7 | 65.1 |
BMI calculations were not available for all participants.
As shown in Table 2, ordinal logistic regression analyses indicated that males in the student and community groups reported a higher threshold for what was objectively large compared to females. Overweight participants in the student sample and the ED sample, but not the community sample, reported higher thresholds. Age was not found to have a significant effect on thresholds for any of the three samples. Table 3 shows the results of ordinal logistic regression analyses for the presence of other associated factors. Current BE in the community and eating disorder groups, as well as fear of weight gain in the eating disorder group, predicted higher thresholds. No significant differences were found for measures of dietary restraint, current hunger, or LOC across the three samples.
TABLE 2.
Differences in threshold ratings based on gender, BMI, and age
| Students |
Community |
Eating Disorder |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | p value | OR (95% CI) | Coefficient | p value | OR (95% CI) | Coefficient | p value | OR (95% CI) | ||
| Gender | F | reference | 1.0 | reference | 1.0 | n/a | ||||
| M | 2.832 | <0.001** | 16.98 (8.96–32.17) | 0.501 | 0.012* | 1.65 (1.12–2.44) | ||||
| BMI | <18.5 | −0.44 | 0.462 | 0.64 (0.20–2.08) | −0.795 | 0.154 | 0.45 (0.15–1.35) | 0.477 | 0.557 | 1.61 (0.33–7.89) |
| 18.5–25 | reference | 1.0 | reference | 1.0 | reference | 1.0 | ||||
| >25 | 0.625 | 0.035* | 1.87 (1.04–3.34) | 0.261 | 0.127 | 1.30 (0.93–1.82) | 1.844 | <.001** | 6.32 (2.14–18.66) | |
| Age (continuous) | n/a | 20.011 | 0.157 | 0.99 (0.97–1.00) | −0.008 | 0.623 | 0.99 (0.96–1.02) | |||
TABLE 3.
Differences in threshold ratings based on psychological variables
| Students |
Community |
Eating Disorder |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | p value | OR (95% CI) | Coefficient | p value | OR (95% CI) | Coefficient | p value | OR (95% CI) | |
| Restraint | 0.339 | 0.329 | 1.40 (0.71–2.77) | 0.266 | 0.155 | 1.30 (0.90–1.88) | 0.486 | 0.345 | 1.63 (0.59–4.45) |
| Fear of Weight Gain | −0.143 | 0.71 | 0.87 (0.41–1.84) | 0.210 | 0.218 | 1.23 (0.88–1.72) | 0.568 | 0.048* | 1.76 (1.00–3.10) |
| Binge | 0.372 | 0.201 | 1.45 (0.82–2.57) | 0.483 | 0.004** | 1.62 (1.17–2.25) | 1.310 | <0.001** | 3.72 (1.88–7.36) |
| Hunger | 0.018 | 0.948 | 1.02 (0.59–1.75) | −0.058 | 0.703 | 0.94 (0.70–1.27) | 0.145 | 0.61 | 1.16 (0.66–2.02) |
| LOC | n/a | n/a | 0.354 | 0.401 | 1.42 (0.62–3.25) | ||||
Discussion
The current results show that self-reported definitions of amount of food at the threshold of what is considered “unusually large” varies by gender, BMI, and presence of disordered eating symptoms including binge eating and fear of weight gain. These findings support the premise that threshold definitions of unusually large amounts of food differ across reference groups and by gender. Specifically, it appears that being male significantly increases the threshold at which one considers an amount of food unusually large. Also, in both the college-aged sample and eating disorder sample, having a BMI > 25 increases the likelihood for rating amounts of food at the threshold of unusually large. These findings corroborate clinician guidelines18 and the Eating Disorder Examination instructions19 that indicate, “…amount may need to be adjusted (generally upwards) to suit particular social groups (e.g., young men).”
Strengths of the current research study include the large number of participants from student, community, and clinical samples. Another strength is the use of measured BMI rather than self-report. However, several limitations are worth noting and may affect the generalizability of the findings. Items used in these analyses queried about eating one type of food (e.g., how many pieces of bread?) when, in fact, patients who over-eat often report multi-item BE. Another limitation of this investigation is that normative eating and binge eating may not be dichotomous constructs. In other words, an upper limit of normative eating may not necessarily be equivalent to a lower limit of objectively large binge eating. Although participants in the current study answered a question that may not be perfectly representative of this undefined construct, the findings remain informative to future diagnostic classification discussions.
Overall, BE assessment is one of the most difficult diagnostic aspects of eating disorder classification.20 The current findings attempt to quantify thresholds in defining the DSM-IV BE size criterion. This study did not examine the validity of requiring that the amount of food consumed during BE be objectively large, a topic that has been examined in a number of previous studies and remains debated in the context of DSM-5.2 In addition, this investigation did not assess the experience of loss of control while eating, a criterion required for BE in the DSM-IV and the DSM-5 draft.3 The importance and clinical significance of this criterion in defining BE (particularly in contrast to the amount of food consumed) has been examined in previous studies.2 However, demographic and psychological factors that may influence the experience of loss of control in eating disorder and community samples have not been investigated. The findings of the current investigation suggest that age, gender, BMI, and eating disorder symptoms may influence the perception of binge size; the extent to which these variables might also influence the perception of loss of control while eating should be considered in future research.
At this time, the proposed DSM-5 guidelines retain the large amount of food criterion for BE required for the diagnosis of both BN and BED. Future research is needed to further demonstrate variations in what is perceived as unusually large across diverse samples. The current findings suggest that the threshold between what is and is not considered unusually large on average differs depending on BMI, gender, and eating disorder status. Future research in this area should examine additional variables; for example, ethnic identity, food types, and activity levels, which may also prove to be important influences on perceived binge size thresholds. This study supports the importance of understanding potential influences on amounts of food that are considered large. Future research on the predictive validity of perceived thresholds on treatment outcome might also be helpful in understanding the clinical significance of how patients judge what a large amount of food is.
Acknowledgments
Supported by P30 DK 50456, K02 MH 65919 and the McKnight Foundation.
Footnotes
Post-hoc exploration of these seven cases indicated that they did not differ significantly from the rest of the community sample on reported food amounts.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 2.Wolfe BE, Baker CW, Smith AT, Kelly-Weeder S. Validity and utility of the current definition of binge eating. Int J Eat Disord. 2009;42:674–686. doi: 10.1002/eat.20728. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association DSM-5 development. 2010 Available at: http://www.dsm5.org/ProposedRevisions/Pages/EatingDisorders.aspx.
- 4.Beglin SJ, Fairburn CG. What is meant by the term “binge”? Am J Psychiatry. 1992;149:123–124. doi: 10.1176/ajp.149.1.123. [DOI] [PubMed] [Google Scholar]
- 5.Latner JD, Clyne C. The diagnostic validity of the criteria for binge eating disorder. Int J Eat Disord. 2008;41:1–14. doi: 10.1002/eat.20465. [DOI] [PubMed] [Google Scholar]
- 6.Telch CF, Pratt EM, Niego SH. Obese women with binge eating disorder define the term binge. Int J Eat Disord. 1998;24:313–317. doi: 10.1002/(sici)1098-108x(199811)24:3<313::aid-eat9>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 7.Wilson GT. Diagnostic criteria for bulimia nervosa. Int J Eat Disord. 1992;11:315. [Google Scholar]
- 8.Niego SH, Pratt EM, Agras WS. Subjective or objective binge: Is the distinction valid? Int J Eat Disord. 1997;22:291–298. doi: 10.1002/(sici)1098-108x(199711)22:3<291::aid-eat8>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 9.Pratt EM, Niego SH, Agras WS. Does the size of a binge matter? Int J Eat Disord. 1998;24:307–312. doi: 10.1002/(sici)1098-108x(199811)24:3<307::aid-eat8>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 10.Cooper Z, Fairburn C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int J Eat Disord. 1987;6:1–8. [Google Scholar]
- 11.Greeno CG, Wing RR, Marcus MD. How many donuts is a “binge”? Women with BED eat more but do not have more restrictive standards than weight-matched non-BED women. Addictive Behav. 1999;24:299. [PubMed] [Google Scholar]
- 12.Crow SJ, Agras WS, Halmi K, Kraemer HC, Mitchell JE. Full syndromal versus subthreshold anorexia nervosa, bulimia nervosa, and binge eating disorder: A multicenter study. Int J Eat Disord. 2002;32:309–318. doi: 10.1002/eat.10088. [DOI] [PubMed] [Google Scholar]
- 13.Agras WS, Crow S, Mitchell JE, Halmi KA, Bryson S. A 4-year prospective study of eating disorder NOS compared with full eating disorder syndromes. Int J Eat Disord. 2009;42:565–570. doi: 10.1002/eat.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spitzer RL, Yanovski SZ, Marcus M. The questionnaire on eating and weight patterns-revised (QWEP-R) New York State Psychiatric Institute; New York: 1993. [Google Scholar]
- 15.Nangle DW, Johnson WG, Carr-Nangle RE, Engler LB. Binge eating disorder and the proposed DSM-IV criteria: Psychometric analysis of the questionnaire of eating and weight patterns. Int J Eat Disord. 1994;16:147–157. doi: 10.1002/1098-108x(199409)16:2<147::aid-eat2260160206>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 16.Celio AA, Wilfley DE, Crow SJ, Mitchell J, Walsh BT. A comparison of the binge eating scale, questionnaire for eating and weight patterns-revised, and eating disorder examination questionnaire with instructions with the eating disorder examination in the assessment of binge eating disorder and its symptoms. Int J Eat Disord. 2004;36:434–444. doi: 10.1002/eat.20057. [DOI] [PubMed] [Google Scholar]
- 17.Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment and Treatment. 12th ed Guildford Press; New York: 1993. pp. 317–360. [Google Scholar]
- 18.Fairburn CG. The definition of bulimia nervosa: Guidelines for clinicians and research workers. Anna Behav Med. 1987;9:3–7. [Google Scholar]
- 19.Fairburn CG, Wilson GT. Binge eating: Definition and classification. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment and Treatment. Guildford Press; New York: 1993. pp. 3–14. [Google Scholar]
- 20.Anderson DA, Lundgren JD, Shapiro JR, Paulosky CA. Assessment of eating disorders: Review and recommendations for clinical use. Behav Modif. 2004;28:763–782. doi: 10.1177/0145445503259851. [DOI] [PubMed] [Google Scholar]


