Abstract
Introduction
Aging is typically associated with progressive multi-system impairment that leads to decreased physical and cognitive function and reduced adaptability to stress. Due to its capacity to characterize complex dynamics within and between physiological systems, the emerging field of complex systems biology and its array of quantitative tools show great promise for improving our understanding of aging, monitoring senescence, and providing biomarkers for evaluating novel interventions, including promising mind-body exercises, that treat age-related disease and promote healthy aging.
Material and Methods
An ongoing, two-arm randomized clinical trial is evaluating the potential of Tai Chi mind-body exercise to attenuate age-related loss of complexity. A total of 60 Tai Chi–naïve healthy older adults (aged 50–79) are being randomized to either six months of Tai Chi training (n=30), or to a waitlist control receiving unaltered usual medical care (n=30). Our primary outcomes are complexity-based measures of heart rate, standing postural sway and gait stride interval dynamics assessed at 3 and 6 months. Multiscale entropy and detrended fluctuation analysis are used as entropy- and fractal-based measures of complexity, respectively. Secondary outcomes include measures of physical and psychological function and tests of physiological adaptability also assessed at 3 and 6 months.
Discussion
Results of this study may lead to novel biomarkers that help us monitor and understand the physiological processes of aging and explore the potential benefits of Tai Chi and related mind-body exercises for healthy aging.
Keywords: cardiovascular health, postural control, gait, mind-body exercise, senescence, prevention
1. Introduction
With our rapidly expanding elderly population, the questions ‘what is healthy aging?’ and ‘how do we promote it’ are increasingly relevant. While modern biomedicine has made great strides in defining and understanding disease, the objective characterization of healthy aging remains elusive. Health requires the integration—across multiple time and spatial scales—of control systems, feedback loops, and regulatory processes that enable an organism to function and adapt to the demands of everyday life. Aging is typically associated with progressive multi-system impairment, leading to decreased physical and cognitive function and reduced adaptability to stress.1, 2 Because of the complex nature of aging processes, present reductionistic methods may not be adequate for defining good health or healthy aging. Due to its capacity to characterize complex dynamics within and between physiological systems, the emerging field of complex systems biology and its array of quantitative tools show great promise for improving our understanding of aging, monitoring senescence, and providing biomarkers for evaluating novel interventions, including traditional mind-body exercises, that treat age-related disease and promote healthy aging.3, 4
Tai Chi is a multi-component mind-body exercise that is grounded in the holistic model of traditional Chinese medicine. The explicit goals of targeting multiple physiological and cognitive processes and integrating their dynamics make Tai Chi particularly well-suited for evaluating the effects on an intervention designed to enhance healthy aging within a systems biology framework. Tai Chi is reported to improve symptoms and systems that typically are associated with age-related decline including cardiovascular function,5–7 balance,8, 9 gait,10 cognitive function,11, 12 self-efficacy,13 and quality of life.14 However, to date, few studies have attempted to study Tai Chi’s impact on age-related physiological processes using complexity measures and to relate such measures to traditional measures of function.
This paper describes the rationale and design of a two-arm randomized clinical trial to evaluate Tai Chi’s effect on age-related loss of complexity and to understand the relationship between complexity, function and adaptability or resilience. This phase II study is designed to inform a future more definitive trial by providing information on preliminary estimates of effect size, and optimal biomarkers for characterizing the impact of Tai Chi on physiological complexity, function, and adaptive capacity. A unique feature of this trial is its use of pragmatically delivered interventions, allowing participants randomized to Tai Chi to choose their training site from within a pre-screened network of long-standing community-based Tai Chi schools.
2. Materials and Methods
2.1. Use of complexity-based metrics of physiological dynamics to study aging
Aging results from gradual changes in the underlying mechanisms of physiological control. The breakdown of nonlinear feedback loops acting across multiple scales of time generally results in a loss of physiological complexity.1 Physiologic complexity is typically estimated using a number of techniques derived from the fields of nonlinear dynamics and statistical physics that quantify the moment-to-moment quality, scaling, and/or correlation properties of dynamic signals.4, 15 The two most common sets of metrics are based on the concepts of entropy and fractals. Entropy-based complexity measures relate to the information content of a signal by quantifying the degree of regularity or predictability over one or more scales of time.16 Growing evidence suggests that signals derived from healthy systems are more entropic (i.e., less regularity) across multiple scales of time, and therefore, are more complex.17–20 Fractal-based complexity metrics quantify the degree of “self-similarity” in physiologic output over multiple measurement scales.21 For example, physiologic signals with high complexity like the heart rate of a healthy young individual are statistically self-similar when observed over seconds, minutes, or hours.22 As with entropy measures, increased fractality within certain ranges has been associated with better health. In this clinical trial, we evaluate whether two widely utilized complexity-based metrics, multiscale entropy (MSE)23, 24 and detrended fluctuation analysis (DFA)21, 25 are sensitive and informative metrics for characterizing the impact of Tai Chi on complexity in cardiovascular, locomotor, and balance systems in older adults. Below we briefly summarize studies to date that support the value of complexity-based biomarkers in characterizing age-related decline in cardiovascular, postural control, and gait dynamics.
2.1.1. Cardiovascular dynamics
Several studies support the idea that heart beat dynamics exhibit features of complex systems with fractal-like, long-range correlation properties, and that the degree of complexity of dynamics decreases with age. This observation is supported by both entropy and fractal-based complexity metrics. For example, systematic age-related decline in complexity of heart rate (HR) dynamics above the age of 40 years were observed in two large cross-sectional samples of healthy adults, assessed using both Approximate Entropy (a measure of the amount of regularity and the unpredictability of fluctuations over time-series) and DFA.26, 27 Additional smaller studies employing a variety of complexity based measures support these findings;28–30 however, some studies suggest that things may not always be so simple.31
Age-related loss in HR beat-to-beat dynamics also appears to be accelerated in populations with heart murmur32 and heart failure.16, 33, 34 Of clinical relevance, loss of complexity in HR dynamics has been associated with cardiovascular disease and risks, and in some cases, complexity measures related to HR dynamics are stronger predictors of mortality in the elderly and post-myocardial infarction35, 36 than linear spectral measures of heart rate variability19, 20. Non-linear measures of HR dynamics also are independent predictors of survival in patients with depressed left ventricular function37 and heart failure;34, 38 are predictors of vulnerability to life threatening arrhythmia;39 and can distinguish subjects with coronary artery disease from healthy controls.40 Finally, there is also some evidence that the complex dynamics of other cardiovascular and cardiorespiratory processes including resting blood pressure and inter-breath intervals decline with age.28, 41–43
2.1.2. Postural control during quiet standing
A growing number of studies have confirmed that under resting conditions, postural sway of the body, as commonly assessed by studying center of pressure (COP) displacements recorded with a force platform, exhibits complex variability over a broad range of time scales.17, 44–46 A few smaller studies in healthy adults support a trend towards age-related loss of complexity of COP dynamics as assessed with MSE, DFA, and related methods17, 44, 45, 47, 48 but these observations have not yet been confirmed in larger cohorts. Further support for the COP complexity measures come from large cross-sectional studies of older adults that found lower postural sway complexity during quiet standing is associated with frailty.49 In this same population, decreased complexity was also associated with decreased visual and somatosensory input.50
2.1.3. Gait dynamics
Multiple studies support the idea that stride-to-stride variation exhibits long-range self-similar correlations extending over hundreds of steps and that fractal-like gait fluctuations vary with activities such as walking or running on treadmills.51–54 However, the evidence of gait complexity systematically declining with age in healthy adults is limited to one study. Hausdorff and colleagues evaluated dynamics of healthy older (avg. 76 y) vs. younger (avg. 25 y) adults found that DFA significantly declined with age.55 For older adults, DFA approached .5, a value that indicates white noise, randomness, and lack of internal long-range structure. Interestingly, in these older adults, other measures of lower extremity function (e.g., ‘Timed Up-and-Go’ and average stride times) were almost identical to those observed in young adults. Apparently, fractal measures of gait dynamics are sensitive to subtle changes in physiology that are not detected in others gait measures. Further evidence of the utility of complexity based markers of gait variability include studies showing associations between long-range fractal patterns in stride intervals and fall risk,56 and associations between loss of gait complexity and presence of neuromuscular disorders such as Huntington’s, Parkinson’s disease, and ALS.55, 57–59
2.1.4 Complexity and adaptability
It has been hypothesized that the complexity of physiologic control systems serves an important purpose; it enables the organism to mount a focused adaptive response in order to perform a specific task or overcome an external stress.1, 2 However, experimental evidence to support this hypothesis is limited. In one large population-based sample of older adults, Manor and colleagues50 demonstrated that the degree of complexity contained within the postural sway (i.e., COP) dynamics of quiet standing (i.e., baseline) is associated with the capacity to maintain balance while challenged by a cognitive dual task (i.e., counting backwards by 3’s from 500). Additional support for this hypothesis is summarized by Manor and Lipsitz.60
2.1.5. Restoration of complexity
Despite the association of loss of complexity with aging and disease, surprisingly few studies have prospectively evaluated the impact of therapeutic interventions on restoration of complexity. A handful of smaller studies have demonstrated that exercise training programs can increase fractal-like correlations in HR data.61–63 Other studies have demonstrated that subsensory mechanical noise applied to the feet via vibrating insoles can restore COP complexity in elderly subjects and those with diabetic neuropathy or stroke.17, 64
In summary, complexity based measures of physiological dynamics show promise as meaningful and sensitive biomarkers for age-related decline in healthy adults. Within the context of a randomized clinical trial of older adults, our comprehensive evaluation of age-related decline in complexity in multiple physiological systems and our experimental evaluation of the ability of a promising multi-component mind-body intervention to restore physiological complexity have the potential to make significant contributions to the field of healthy aging. In particular, we anticipate gaining important new insights into the mechanisms underlying three systems (cardiovascular, postural control, and gait) that play a key role to healthy aging, the interactions among these systems, and the potential to reduce age-associated declines.
2.2. Overview of trial design and specific aims
This pilot study is a two-arm randomized clinical trial to evaluate the potential of Tai Chi to attenuate age-related loss of complexity. A total of 60 Tai Chi–naïve healthy older adults (aged 50–79) are being randomized to either six months of Tai Chi training (n=30), or to a waitlist control group receiving unaltered usual medical care (n=30) (Figure 1). Our primary outcomes are complexity-based measures of cardiovascular (heart rate, HR), postural control (center of pressure, COP) and gait (stride interval) dynamics assessed at 3 and 6 months. Multiscale entropy and detrended fluctuation analysis are used as entropy and fractal-based measures of complexity, respectively. Secondary outcomes include measures of physical and psychological function and tests of physiological adaptability also assessed at 3 and 6 months. This study is designed to inform a future more definitive trial by providing information on preliminary estimates of effect size and the most informative biomarkers of complexity, function, and adaptive capacity. This trial is funded by the National Center for Complementary and Alternative Medicine (NCCAM), National Institutes of Health. All clinical research is performed in Boston, MA at the Beth Israel Deaconess Medical Center (BIDMC). Tai Chi is administered in the community as described below. The Institutional Review Board at BIDMC approved this study. The study is registered at Clinical Trials.gov (NCT01340365). At the time of submitting this manuscript, all study aspects are ongoing.
Figure 1.
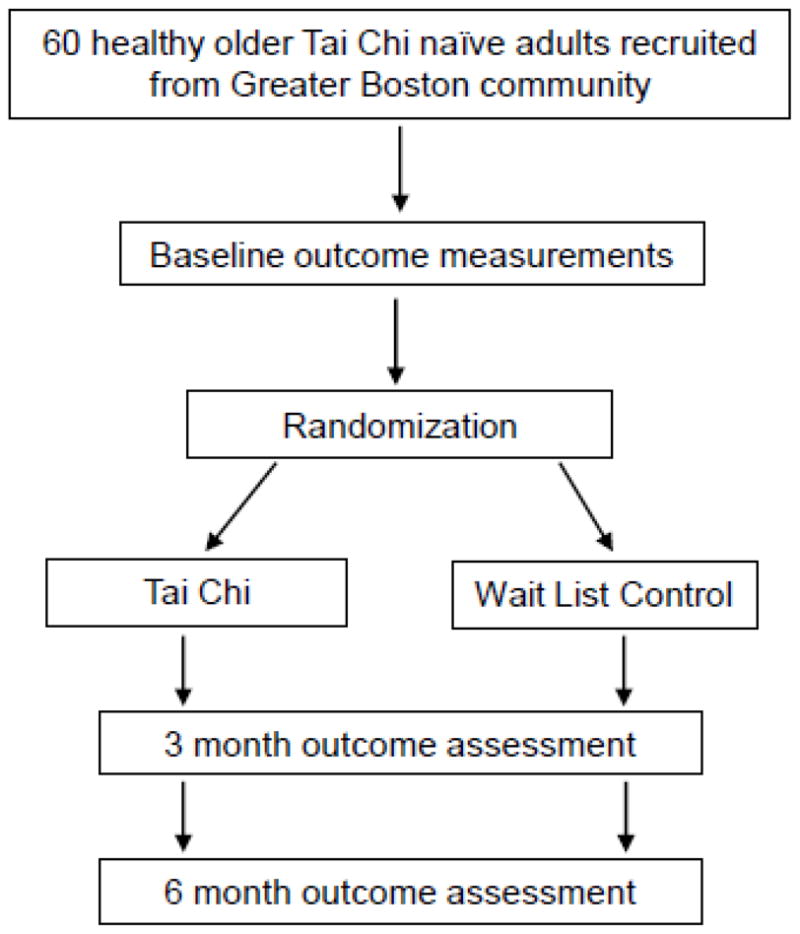
Study design
This study addresses two specific aims. Aim 1 is to determine if 6 months of Tai Chi training can increase complexity, function, and adaptive capacity of multiple physiological systems in older healthy adults and will test four hypotheses: H.1.a) Those who participate in Tai Chi will exhibit higher levels of complexity across all measured physiological systems, compared to baseline values and compared to controls; H.1.b) Those who participate in Tai Chi will exhibit higher levels of physical and cognitive function; H.1.c) Those who participate in Tai Chi will exhibit higher levels of adaptive capacity; and H.1.d) The magnitude of the effects of Tai Chi on physiological complexity, function and adaptive capacity in healthy older adults will be positively correlated with age. Aim 2 is to determine the relationships between biomarkers of physiological complexity, conventional measures of function and adaptive capacity, and tests four additional hypotheses: H.2.a) Measures of complexity will be positively correlated with physical and cognitive function; H.2.b) Measures of complexity will be positively correlated with adaptive capacity. And over time: H.2.c) Changes in complexity will be positively correlated with changes in physical and cognitive function; and H.2.d) Changes in complexity will be positively correlated with changes in adaptive capacity.
2.3. Study population and enrollment procedures
Study population
A total of 60 healthy older adults (50–79 years old) are being recruited for our study. Recruitment targets community dwellers living within the Greater Boston area. Inclusion criteria are: 1) Ages 50–79; 2) Living or working within the Greater Boston area; and 3) Willing to adhere to 6 month Tai Chi training protocol. Exclusion criteria are: 1) Diagnosis of a chronic medical condition e.g., cardiovascular disease (myocardial infarction, angina, atrial fibrillation or presence of a pacemaker), stroke, respiratory disease requiring daily use of an inhaler, diabetes mellitus, active cancer (diagnosis < 5 years ago and requiring ongoing chemotherapy or use of cytotoxic agents), or neurological conditions (e.g., seizure disorder, Parkinson’s, peripheral neuropathy); or significant neuromuscular or musculoskeletal requiring chronic use of pain medication; 2) Acute medical condition requiring hospitalization within the past 6 months; 3) Self-reported (current) smoking or alcohol/drug abuse; 4) Unmanaged hypertension (resting SBP > 140 or DBP > 90mm Hg); 5) Abnormal heart rate (resting HR > 100 bpm; <50bpm); Abnormal ECG (supraventricular tachyarrhythmia, atrial fibrillation, significant ST wave abnormality, 2nd and 3rd degree heart block); 6) Pregnancy; 7) Current use of prescription medications that affect autonomic function including cardio- or vaso-active drugs and medications; 8) Self-reported inability to walk continuously for 15 min unassisted; 9) Regular Tai Chi practice within past 3 years; 10) Regular participation in structured physical exercise on average, more than 5 hrs/wk.
2.3.1. Recruitment, screening and enrollment procedures
Potential participants are targeted with advertisements in local newspapers, and hospital based clinics and research volunteer databases. Interested individuals contact the study coordinator who conducts an initial eligibility screen by telephone. Individuals who meet initial eligibility criteria are then required to visit, by appointment, at least one of our four prescreened community-based Tai Chi schools to: a) gain a preliminary understanding of Tai Chi (they can observe but not participate in a class); and b) to experience firsthand the logistical requirements of traveling to and from local Tai Chi schools. This run-in, pre-study visit was introduced as a means to screen out individuals that are less likely to be compliant with Tai Chi class attendance and other study protocols. Individuals completing this run-in phase are then scheduled for an in-person screening visit at the BIDMC Clinic Research Center (CRC). The screening visit begins with obtaining informed consent, followed by assessment of vital signs and an EKG to confirm cardiovascular health criteria, and the Mini-Mental State Examination to confirm appropriate cognitive function (subjects with an MMSE score < 24 are excluded). Individuals who meet all screening criteria undergo baseline testing followed by randomization.
2.3.2. Randomization procedures
Study participants are randomly assigned to Tai Chi or wait list control. Randomization assignments are stratified by participant age (50–59, 60– 69, 70–79) and were generated using a permuted-blocks randomization scheme with randomly varying block sizes. Treatment assignments are sealed in opaque, sequentially numbered envelopes by stratum. All randomization materials are stored in a locked file, with access limited to non-blinded study personnel.
2.4. Interventions
2.4.1. Tai Chi
Rationale for Tai Chi Intervention
Tai Chi, also referred to as Taiji, Tai Chi Chuan or Taijiquan, is a mind-body exercise that originated in China, and that is growing in popularity in the West. Tai Chi is based on slow intentional movements, often coordinated with breathing and imagery, that aims to strengthen and relax the physical body and mind, enhance the natural flow of ‘qi’ (or life energy), and improve health, personal development, and in some systems, self defense.65 Recent surveys suggest that approximately 5 million Americans have practiced Tai Chi, and this number is increasing.66, 67 Tai Chi shows great potential for becoming widely integrated into initiatives related to healthy aging. Tai Chi appears to be safe, even for the elderly and deconditioned, and clinical and community based studies report high adherence and enjoyment. Moreover, Tai Chi may be cost-effective, requiring no special equipment or facilities. For these reasons, a growing body of clinical research has begun to evaluate the efficacy of Tai Chi as a therapy for a variety of age-related health issues; this research has been critically evaluated in recent reviews.8, 9, 68–70 Tai Chi has shown to have a positive impact on cardiovascular,71–80 postural control,81–91 and locomotor systems,92–101 as well as cognitive function, psychological well being and quality of life.11, 14, 102, 103
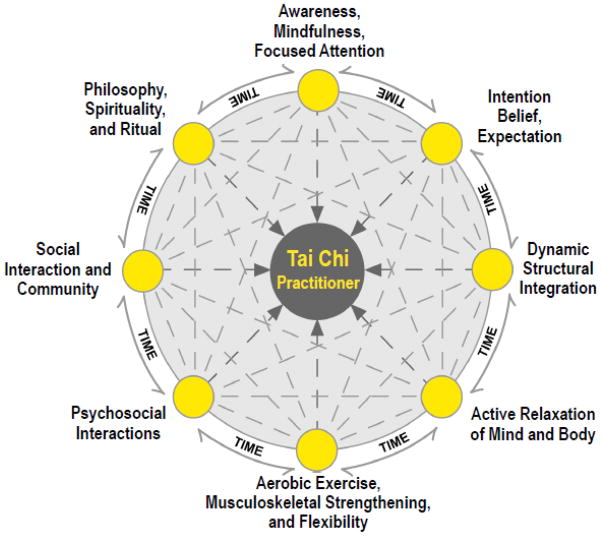
It has been argued that Tai Chi itself is inherently a complex intervention, composed of multiple components each of which has potentially independent and synergistic therapeutic value.65, 104 As such, the study of Tai Chi may best be viewed as a form of whole-systems research rather than the study of a single active ingredient. This multi-component nature of Tai Chi is depicted in Figure 2 and key components are summarized in Table 1. This complexity poses challenges to simple, single-factor, cause-and-effect reductionist models. For example, the reported improvements in balance referenced above likely result from multiple mechanisms including increased leg strength and flexibility, changes in neuromuscular patterning/control, reduced fear of falling, improved body awareness and concentration, and a number of cognitive strategies.9 Moreover, these factors are likely to interact with one another in non-linear ways, change in relative importance over time, and differ for different practitioners. Consequently, the fundamental premises and tools afforded by complexity theory and systems biology provide an excellent framework for evaluating and monitoring the therapeutic effects of Tai Chi.
Figure 2.
Schema characterizing the multicomponent nature of Tai Chi, depicting eight classes of therapeutic components or ‘active ingredients’. Arrows connecting each element acknowledges interdependence of these factors, and ‘time’ emphasizes that relevance of each component may change as practitioners skills develop. (Modified from Wayne and Kaptchuk 2008; Wayne and Fuerst 2013).145
Table 1.
A summary of purported therapeutic components or ‘active ingredients’ of Tai Chi. (modified from Wayne and Fuerst 2013)145
| Therapeutic component or ‘active ingredient | Brief description |
|---|---|
| Awareness, Mindfulness, and Focused Attention | Perhaps the most fundamental ingredient underlying Tai Chi, the slow, deliberate movements and attention to breathe, body positions, and sensations fosters acute self-awareness. The emphasis on moment-to- moment awareness may result in enhanced mindfulness and improved focus.146–149 |
| Intention, Belief and Expectation | Imagery, visualization, and related cognitive tools alter intention, belief, and expectation and may contribute significantly to the therapeutic and physiological effects of Tai Chi.150–152 |
| Structural Integration; Dynamic Form and Function | Enhanced integration within and between multiple structural and physiological systems is another key active ingredient that may underlie Tai Chi’s therapeutic effect. Biomechanically efficient shapes and patterns of movement may have functional consequences across many systems.10, 92, 101 |
| Active Relaxation | Tai Chi’s circular, flowing motion helps shift the body and mind into deeper levels of relaxation, and is believed to be a form of meditation in motion. |
| Strengthening and Flexibility | Tai Chi provides moderate aerobic training equal to levels obtained in walking at a moderate pace.153 The integrated movements may result in less strain, greater power with less effort, and better balance. The slowness of the Tai Chi movements, in combination with slightly flexed stances and placing weight on one leg at a time for sustained periods of time, lead to significant lower extremity strength training and increased loading on the skeleton.105, 154 In addition, slow, continuous, relaxed and repetitive movement also results in dynamic stretching, which enhances overall flexibility.92, 155, 156 |
| Natural, Freer Breathing | More efficient breathing improves gas exchange,157 massages body tissues,158 including internal organs, helps regulate the nervous system,159 improves mood,160 and is believed to balance and move qi within the body and between the body and the environment. |
| Social Support, Interaction and Community | Being part of a group has therapeutic value for a variety of medical conditions, including cancer, heart disease, depression, and anxiety.161–163 In ongoing Tai Chi classes, students develop a strong sense of community, with rich interactions and support from teachers and peers. |
| Embodied Spirituality, Philosophy and Ritual | Tai Chi creates a practical framework for practicing living with a more holistic, Eastern philosophy that integrates body, mind, and spirit. |
Pragmatic Structure of Tai Chi Intervention
All Tai Chi instruction takes place at one of five community-based Tai Chi schools within an already established network used in prior research studies. Tai Chi school characteristics, eligibility and screening procedures are described in detail elsewhere.105, 106 Briefly, schools were chosen to meet specific criteria ensuring they provide valid, stable Tai Chi programs led by experienced teachers. Importantly, since participants are being asked to make a six-month commitment to Tai Chi training, allowing them to receive training at a school they choose within their local community increases the likelihood of protocol adherence. Administering the intervention through community Tai Chi schools also affords a high level of ecological validity, as participants will be exposed to a number of traditional components of Tai Chi training that are often absent in fixed protocols provided in medical settings. Finally, because of the inclusion of multiple Tai Chi instructors and well-defined but slightly varying protocols, the results of this study will have good generalizability—applying not only to a single protocol of Tai Chi taught by one teacher, but to a range of approaches that share a common, well-defined set of criteria described elsewhere.105,107
Participants randomized to Tai Chi are required to attend, on average, two classes per week over the six months of the intervention. They are also asked to practice a minimum of 30 minutes, two additional days per week. All of the schools in our network provide DVDs or printed materials to facilitate home practice.
2.4.2. Usual Care
Participants randomized to Usual Care are instructed to continue their medical care as normal and to not begin Tai Chi instruction during the 6 months of the study.
2.5. Participant remuneration
All costs associated with participation in Tai Chi classes, including practice DVDs, are paid for by the study. Participants randomized to the control group are offered a free 3 month course of Tai Chi following the completion of their participation in the trial. Additionally, all participants receive $50 for each outcome assessment they complete (maximum total of $150) and parking expenses associated with outcomes testing visits are covered by the study.
2.6. Outcome measures
Our measurement protocol includes acquisition of 1) steady-state dynamics of the cardiovascular, locomotor and postural control systems, 2) measures of the ability of these systems to respond to imposed stressors, and 3) more traditional measures of function and health related QOL. Additionally, traditional linear outcome measures for heart rate variability, gait, and postural sway will be assessed for comparison with complexity measures. All measurements will be assessed at baseline, 3 and 6-months. All outcome assessors will remain blinded with respect to treatment allocation (Table 2).
Table 2.
Summary of outcome measures and associated variables
| Temporal dynamics during steady-state conditions | Physiological measure | Testing methods | Outcome variable |
|---|---|---|---|
| Heart rate (HR) | Beat-to-beat variation measured using ECG for a 30 minute during seated quiet resting | HR complexity* | |
| Standing balance | Center of pressure dynamics during quiet standing with eyes open | COP complexity | |
| Gait | Stride–to-stride interval at preferred speed during a 20 minute period | Stride complexity | |
| Adaptive capacity | Heart rate | Sit to stand test | Max change in heart rate |
| Standing balance | Eyes closed Cognitive dual task |
Change in COP complexity Change in magnitude of COP displacement |
|
| Gait | Cognitive dual task | Change in average stride variability | |
| Function and HRQOL | Exercise capacity | Max walking speed | m/sec |
| Musculoskeletal strength/power |
|
|
|
| Clinical balance | Single leg balance with eyes open and closed | Maximum time on balance | |
| Range of motion |
|
|
|
| Mood | Profile of Mood States | Indices of 6 domains of mood | |
| Cognitive function | Trail Making Test A and B Controlled Oral Word Association Test Backwards Digit Span Test |
Time to complete test (sec) Number of words recalled/min Number of digit sequences correctly repeated |
|
| HRQOL | SF-36 | Indices of physical and mental health in 8 domains | |
| Physical activity | Physical Activity Status Scale | Index of physical activity during prior week | |
| Protocol adherence | Tai Chi training | Teacher reported class attendance records Self-reported home practice logs |
Numbers of classes/month Hours of home practice/month |
| Additional screening instruments | Cognitive function | Mini-mental state exam | Index reflecting 5 domains of cognitive health |
All testing takes place in the Syncope and Falls in the Elderly (SAFE) laboratory, located within the BIDMC Clinical Research Center (CRC), and begins at approximately 9:00 a.m. to minimize diurnal variability in physiological outcomes. Study staff first obtain participant informed consent, and then administer screening procedures which include a health history questionnaire, the Mini Mental State Exam, assessment of vital signs (resting heart blood, blood pressure and ECGs), and a pregnancy test (for pre-menopausal women) to confirm eligibility. Eligible participants then undergo all other study related measurements. The testing protocol was designed to minimize fatigue and patient burden and maximize the validity of the data collected; the protocol follows others used in prior SAFE lab studies.107, 108 The total time for completion of measurements is approximately four hours, with interspersed resting periods and a mid-point snack provided by the CRC.
2.6.1. Cardiovascular measures
HR dynamics are assessed in multiple ways. Steady-state HR dynamics are assessed during seated rest with spontaneous breathing. To collect the sufficient number of heartbeat cycles for complexity measures, HR dynamics are assessed for 30 minutes. Additionally, two 5-minute periods of HR dynamics are assessed during paced breathing (15 and 6 breaths per minute); paced breathing enables the assessment of cardiovascular dynamics and linear measures of HR variability while controlling for the potentially confounding effects of respiration.109 The effects of perturbation to the cardiovascular system are evaluated from the well-validated sit-to-stand test.110 Standing following prolonged sitting (≥5 min) results in an immediate elevation in HR, with relative greater change in HR response reflective of impaired cardiovascular regulation. The maximum change in HR (ΔHR) will be quantified by subtracting the minimum HR during sitting from the maximum HR during the subsequent bout of 1 min standing.
2.6.2. Postural control measures
Steady-state postural control dynamics are assessed during quiet standing with eyes open. With arms at the side and bare feet shoulder width apart, subjects are asked to stand as still as possible on standard force plate (AMTI, Watertown, MA), and to visually fixate on an “X” drawn on a wall approximately 3m away at eye-level. Postural sway of the body is quantified by recording COP displacements. To collect sufficient COP data for complexity analysis, 1 min of continuous standing is obtained. The effects of visual and cognitive perturbations are also evaluated. For the visual perturbation, subjects stand similar to above, except with eyes-closed. For the cognitive perturbation, subjects perform the dual task of counting backwards, out loud, in multiples of three, while attempting to repeat the steady-state protocol. This cognitive dual-task is commonly used to challenge standing balance in both healthy and movement disordered populations.111 To avoid potential effects of learning, subjects begin each trial from 500, 499, or 498, in random order. To account for potential trial-to-trial variability, three one-minute trials are completed for each condition (steady-state, eyes-closed, dual task). Trials are randomized and at least one minute rest is given between each trial. During the first trial, the subject’s feet are outlined with chalk to ensure consistent foot placement.
2.6.3. Gait measures
Steady-state gait dynamics are assessed during over ground walking at preferred speed. Subjects walk along a long corridor (~75m) that is wide enough (~5m) to enable smooth turning. To record consecutive stride-to-stride durations, subjects have foot-switches inserted into their shoes and a data acquisition monitor (Noraxon Inc, Scottsdale, AZ) attached to their waist. To collect the sufficient number of steps required for complexity measures, 10 min of continuous walking is obtained. The effects of a locomotor perturbation on gait speed, an indicator of gait health and overall function,112 is assessed during continuous over ground walking while performing the same cognitive dual task as in postural control testing. Subjects complete three 1 min trials while counting backwards, out loud, in multiples of three.113, 114. Dual tasking decreases walking speed.111. The distance walked during each trial will be recorded and used to calculate average speed.
2.6.4. Assessment of function and health-related quality of life
Multiple clinical tests of physical and mental function are obtained to further characterize the sample, evaluate correlations between complexity measures and function, and assess the impact of Tai Chi and age on these outcomes.
Maximum walking speed is assessed by asking subjects to walk in a straight line as fast as possible, without running, on a premeasured 11m course. The time taken to walk 5m, from the 3m to 8m mark is recorded and used to calculate maximal walking speed (m/s). Performance in this clinical test is associated with functional decline.115 One-legged standing balance on the subject’s preferred leg is assessed according to Vereeck et al.116 Three 30 sec trials are completed for eyes-open and eyes-closed conditions, and the greatest duration (sec) for each condition is used for analysis. This test is correlated with fall risk in older adults.117 Maximal power output of the lower extremities is estimated by assessing maximum vertical jump height (m). After a standard warm-up consisting of five sub-maximal jumps, subjects complete three countermovement jumps on a stationary Kistler force plate (Kistler Instruments Corp, Amherst, NY). The “flight-time” for each jump, determined from the force plate reading, is used to determine the maximum height reached by the subject’s center of mass using the Bosco method.118 This test has been shown to be safe for community-dwelling older adults, and test scores correlate with mortality rate, fall-risk and overall physical function.119, 120 Maximum grip strength of the dominant hand is measured using a handgrip dynamometer Grip D (Takei Scientific Instruments, Tokyo, Japan). Measurements are recorded to the nearest 0.5 kg, repeated three times and averaged. Grip strength is correlated with mortality, and disability, and overall function in middle-aged and older adults.121 Finally, bilateral hip, knee, and ankle joint passive range of motion (degrees) is measured by a trained investigator using a goniometer and standard procedures.122 Lower body flexibility is assessed using the validated Chair Sit and Reach test.123
The amount and intensity of non-Tai Chi exercise is recorded using the Physical Activity Status Scale (PASS). Subjects are asked to estimate their general physical activity during the previous week using an 11-point scale (i.e., 0–10). The scale quantifies physical activity duration by a combination of the minutes of exercise per week and the intensity of this exercise (heavy, modest, or none). The validity of the scale has been documented in both men and women and scores correlate with maximal oxygen consumption in younger and older adults.124, 125
Health related quality of life is assessed using the SF-36. The SF-36 has been validated in a variety of populations including older healthy individuals, and has good test-retest reliability.126, 127
Cognitive function is assessed with validated measures of executive function, working and short-term memory. The Trail Making Test (TMT) is a widely used instrument that is administered in two parts.128 TMTa is a visual-scanning task; the time required to draw lines sequentially connecting numbered circles from 1 to 25 is recorded. TMTb assesses time required to connect the same number of circles in an alternating sequence of numbers and letters. TMTb is considered to evaluate executive control, and is correlated with other executive function measures.129 TMT is a sensitive indicator of overall neurological impairment,128 and has good reliability.130 The Controlled Oral Word Association Test (COWAT) examines working memory span.131 COWAT requires the participant to produce as many words as possible that begin with a given letter of the alphabet (F, A, S). There is 1 minute allowed for each of the three letters. The score is the sum of all acceptable words produced in the three trials. COWAT has good reliability and validity.132, 133 The Backwards Digit Span Test (BDS) is a widely used measure of short-term memory, i.e. the number of digits a person can absorb and recall in correct serial order. Two trials of eight number sequences are read aloud. Scores are based on the number of sequences correctly recalled (i.e., until the participant consecutively fails two trials of the same digit span length). BDS has good reliability and validity.131 All three measures have been employed in studies evaluating the impact of exercise on cognitive function in elders.134
The Mini-Mental State Examination (MMSE) is employed for screening purposes, and individuals scoring less than 24 are not eligible for the study. MMSE is used widely in primary care and in community based research settings, and has good inter-rater reliability.135–137
Mood is assessed using the 30-item Profile of Mood States (POMS-30). This well-validated instrument assesses emotional states that are transient and expected to respond to clinical intervention.138 Prior studies of Tai Chi have reported improvement in mood, decrease in anxiety, and enhancement in vigor as measured by the POMS scale.139
The degree to which participants believe that Tai Chi will be beneficial to their health is assessed using an instrument used in a number of prior complementary and alternative medical intervention studies. Participants are asked to rate how helpful they believe Tai Chi will be for their general health on a 0 to 10 scale. 140
2.6.5. Compliance with Tai Chi protocol
Compliance with the required training schedule is monitored using a combination of class attendance cards that are signed by Tai Chi instructors following each visit, and participant-completed home practice logs. Participants are asked to send class attendance and home practice logs to study staff monthly using prepaid envelopes provided at the beginning of the study. If attendance and/or practice logs are not submitted on time, the study coordinator calls the participant within 3 days of the due date. Every possible effort is made to keep subjects actively engaged in the protocol following attendance and practice guidelines.
2.7. Computation of complexity measures
Two principal complexity metrics—Multiscale Entropy (MSE) and Detrended Fluctuation Analysis (DFA)—are employed in this study.21, 25, 141 Multiscale Entropy quantifies the information content of a signal over multiple temporal or spatial scales. Compared to other entropy-based methods, MSE uniquely accounts for dynamical information encoded in physiologic signals over multiple scales and therefore is able to distinguish between highly irregular random (uncorrelated) signals and truly complex ones.18, 23, 53 DFA quantifies long-range correlation properties (i.e., fractality) of a signal. Unlike alternative approaches (e.g., Fourier spectral analysis and Hurst analysis), DFA permits the detection of intrinsic self-similarity embedded in a seemingly nonstationary time series. DFA has been successfully applied to a wide range of simulated and physiologic time series in recent years.15, 27, 111 Computations of these indices are briefly summarized below. Extensive information on these measures, including details of algorithms, tutorials, and examples of their application is provided at Research Resource for Complex Physiologic Signals (www.physionet.org).
2.7.1. Multiscale Entropy (MSE)
The MSE algorithm comprises two steps: (1) a coarse-graining procedure that allows us to look at representations of the system’s dynamics at different time scales, and (2) the quantification of the degree of irregularity of each coarse-grained time series, which can be accomplished using sample entropy (SampEn), a statistic introduced by Moorman.142 The coarse-grained time series are constructed as follows. For scale 1, the coarse-grained time series is the same as the original signal. For scale n, we divide the data into consecutive non-overlapping blocks with n data points each and calculate the mean inside each block. The sequence of average values is the coarse-grained time series for scale n.
Sample entropy is the negative natural logarithm of the conditional probability that two patterns of length m, xm(i) = {xi,…, xi + m − 1} and xm(j) = {xj,…, xj + m − 1} will still be considered similar to each other when points, xi + m and xj + m are added to patterns xm(i) and xm(j), respectively. The two patterns, xm(i) and xm(j), are separate samples within a time series and are selected based on the level of similarity between them. A threshold tolerance level of r is used – i.e. d[xm(i), xm(j)] ≤ r, where d is a function that measures the distance between vectors. The complexity index is the summation of the sample entropy values for each coarse-grained time series for a pre-selected range of time scales. A higher MSE score implies greater complexity.
2.7.2. Detrended Fluctuation Analysis (DFA)
To estimate a fractal scaling index for long-range correlation properties using DFA, time series (with N data) are first integrated using the following algorithm: y(k)= Σi=1 k.[B(i)−Bave], where B(i) is the i-th data point of the time series and Bave is the average value of the data points. Next the integrated time series is divided into boxes of equal length, n. In each box of length n, a least squares line is fit to the data (representing the trend in that box). The y coordinate of the straight line segments is denoted by yn(k). Next we detrend the integrated time series, y(k), by subtracting the local trend, yn(k), in each box. The root-mean-square fluctuation of this integrated and detrended time series is calculated by: This computation is repeated over all time scales (box sizes) to provide a relationship between F(n), the average fluctuation, as a function of box size. Typically, F(n) will increase with box size n. A linear relationship on a double log graph indicates the presence of power law (fractal) scaling. Under such conditions, the fluctuations can be characterized by a scaling exponent a, the slope relating log F(n) to log n. Since an exponent of 1 represents fractal scaling and smaller deviations from 1 are more complex, we can quantify complexity as the absolute value of 1-a complex.
2.8. Statistical analysis
2.8.1. Analytic plan
Aim 1
Our goals is to compare the change over time in the Tai Chi students versus the controls. The primary analysis will use an intention-to-treat paradigm, i.e., participants will be evaluated on the basis of group assigned by randomization without regard to subsequent adherence. Since this is a pilot study, we will not impute values for missing data; however, the statistical models we are using will include all available data. We recognize that some participants may drop out before the follow-up evaluation and that some outcome measures may not be evaluable for some participants. We will make no adjustment for multiple testing. A secondary ‘per-protocol’ analysis will be limited to participants who were compliant (attended 70% of classes and completed at least 70% of home sessions). Our primary analysis will employ linear mixed effects regression models that examine change over time (i.e., slope) for each outcome measure (i.e., the complexity measures, MSE and detrended fluctuation analysis) for each of the systems (i.e., heart rate, postural control and gait). The models will incorporate a random intercept and a random slope for each participant.
We will also conduct sensitivity analyses that incorporate additional covariates into the models, including age, gender, baseline physical and mental health, BMI, and exercise behavior. We are particularly interested in examining age with a focus on assessing whether age substantially reduces the variability of the random effects, i.e., whether it explains a substantial proportion of between-person variability in baseline complexity and slope. Analyses of secondary outcomes will follow the same general analytic approach. We will use mixed effects models to examine the effects of Tai Chi training over time on physical and cognitive function (exercise capacity, balance, upper and lower extremity strength, cognitive function, and quality of life) and adaptive capacity (change in heart rate, change in COP displacement, change in stride variability).
Aim 2
We hypothesize that function and adaptive capacity are associated with complexity. We will first examine the association between complexity measures and function/adaptive capacity at baseline. We will calculate Pearson correlation coefficients between the complexity measures (MSE and detrended fluctuation analysis) and the measures of function/adaptive capacity. To examine the independent association between complexity and function/adaptive capacity, we will fit ordinary least squares regression models using the function/adaptive capacity measures as the dependent variable. Independent variables will include age and sex as well as any other baseline characteristics associated with the function variable. We will add the complexity measure to this model and evaluate the Wald test and the change in R2. We will also investigate whether changes in complexity are associated with changes in function and adaptive capacity. We will fit linear regression models with change in function and adaptive capacity as the dependent variable and change in complexity as the independent variable of interest. Since we will have 2 observations per participant (change at 3 months and change at 6 months), we will use generalized estimating equations methods (GEE) to account for the within-person correlation. Independent variables will include the measure of function and adaptive capacity at baseline, age, sex, treatment group and time (3 vs. 6 month). Further, we hypothesize that complexity is the primary mediator of the association between Tai Chi and improvements in adaptive capacity. We will examine this using the approach recommended by Judd and Kenny.143 For example, to examine whether multi-scale entropy of postural sway (i.e., COP) during quiet standing mediates the effect of Tai Chi on the postural adaptation to a dual cognitive task among the older participants, we will fit 3 regression models: regress MSE on Tai Chi use; regress COP response on Tai Chi; and regress COP response on MSE and Tai Chi use. The associations seen in these models determine the existence and strength of mediation. Despite the implicit directionality of our hypotheses, all tests will be two-sided. We recognize that we are examining a moderate number of outcomes in this study. Since it is a pilot study and has limited power, we do not intend to adjust for multiple testing.
2.8.2. Sample size and statistical power
Our analysis will be based on a longitudinal regression analysis in which we do not have an estimate of the within-participant correlations. In the worst case, the two follow-up measures provide no more information than a single follow-up, and the power calculation is equivalent to that for a simple t-test.
With 30 participants in each group, we will have 50% power to detect an effect size of 0.52 (i.e., the sample size provides 50% sensitivity to detect a difference between groups .52 times the standard deviation of the outcome measure) and 80% power to detect an effect size of 0.74 for each of the main effects. Our primary hypothesis, however, is an interaction effect. Our sample size provides at least 50% power to detect an interaction effect size of 1.03, under this worst case scenario. At the other extreme, if the two follow-up observations are independent, we will have 50% power to detect an interaction effect size of 0.72 and 80% power to detect an effect size of 1.03. The use of regression models further increases power by accounting for additional sources of variability. Unpublished data from a trial of heart failure patients found that the mean difference in MSE change between Tai Chi and control was 2.26, which translates to an effect size of 1.2. Therefore, changes of this magnitude will likely be present in our current study and thus our sample will provide adequate power.
2.9. Adverse Events
Adverse events are monitored through participant feedback, reports from Tai Chi schools, and study team observations during testing visits and monthly follow-up calls to participants. Tai Chi schools received information on potential Tai Chi-related side effects and adverse events as well as the protocol, and are instructed to call the study PI if any participant is experiencing any symptoms of concern. Participants are provided with information on safety policy and adverse event forms, and are instructed on their use by study personnel at the conclusion of the baseline testing visit. Adverse events that take place during testing are also reported to the PI by the SAFE laboratory assessor. All adverse events are reported to the IRB as prespecified in a data and safety monitoring plan.
3. Discussion
Understanding the biology of aging and evaluating interventions that promote healthy aging are becoming increasingly important priorities. As summarized in this paper, a growing body of research supports the idea that aging is associated with loss of complexity in multiple physiological systems.. However, a number of outstanding questions remain that limit our ability to evaluate complexity-based physiological metrics as biomarkers for monitoring healthy aging, as well as their value for quantifying the impact of therapeutic interventions such as Tai Chi on age-related disease prevention and rehabilitation. Using mathematical tools drawn from the emerging field of complexity and systems biology, this study will characterize how Tai Chi—a multi component mind-body exercise—impacts moment-to-moment variations in heart beat, gait, and postural control, as well as the relationship of these patterns to more traditional measures of physical and mental function. This study will advance our understanding by systematically characterizing age-related decline in multiple physiological systems in a well-defined cohort of adults, and the relationship of these complexity metrics to more traditional measures of physical and cognitive function; and by evaluating and comparing two separate metrics for characterizing physiological complexity.
There are a number of limitations inherent in this study that are important to note. First, we are only considering two of many metrics available to characterizing the complexity of physiological dynamics. Different metrics may provide insight into unique aspects of complex dynamics.144 Which metrics prove to be optimal will require more extensive comparisons in future larger studies with diverse populations, and may also vary with the specific biological questions being explored.
Second, and related to this first limitation is the paucity of experimental research available to inform a mechanistic interpretation of complexity metrics. Our goal in the current study is to characterize the impact of Tai Chi training on complexity outcomes, and the relationship of these outcomes with multiple validated markers of age-related function. However, to better interpret how and why Tai Chi may impact physiological complexity, mechanistic studies that experimentally alter complex physiological processes will be needed. Taking postural control as an example, experimental studies that systematically perturb various combinations of processes known of contribute to postural control (e.g. plantar proprioception, vision, vestibular function, executive function) and quantify the impact of these perturbations on complexity signals (e.g. COP), will better inform the meaning and value of these metrics, and help us understand how interventions like Tai Chi may impact complexity and resilience.
Third, the duration of this study is relatively short for understanding the longer-term impact of Tai Chi in healthy aging. While many studies, especially those evaluating older adults or population with significant health impairments, have reported functional changes in periods of three to six months, the six month duration of this study will only evaluate the potential of Tai Chi to impact age-related decline. Tai Chi is traditionally considered a life-long learning tool, and it is believed that with time, both proficiency and health benefits improve. Long-term interventional studies as well as well-designed observational studies comparing long-term Tai Chi practitioners (e.g. > 10 years) to matched controls will be needs to fully evaluate the long-term impact of Tai Chi on healthy aging.
Finally, in our attempt to comprehensively evaluate multiple physiological systems and outcomes, it is possible that the large battery of tests we utilize could overly burden participants and impact the quality of the data collected. To minimize this potential limitation the following strategies were integrated into all protocol to minimize fatigue and bias. 1) Short breaks are placed between all physical activities and replications of specific physical tasks, and mid-way through the overall protocol participants are provided with a light lunch and 20 minute break. 2) Cognitive and seated tasks are interspersed with physical ones. 3) The exact same sequence of tests are used at all three evaluations, so if there is any systematic fatigue near the end of the protocol, this would be consistent between baseline and follow-up tests. However, to date we have completed more than 100 testing visits, and at no visit has anyone been incapable of completing the entire battery of tests. Moreover, in our final test which involves 10 minutes of continuous walking, we explicitly ask if participants are experiencing fatigue or pain, and to date, no one has responded with a yes.
In conclusion, limitation withstanding, results of this study may lead to novel measures that help us monitor and understand the physiological processes of aging, and explore the potential benefits of Tai Chi and related mind-body exercises for healthy aging.
Acknowledgments
This publication was made possible by grant number R21 AT005501-01A1 from the National Center for Complementary and Alternative Medicine (NCCAM) at the National Institutes of Health (NIH), and from grant number UL1 RR025758 supporting the Harvard Clinical and Translational Science Center, from the National Center for Research Resources (NCRR). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCCAM, NCRR, or the NIH. We thank Jacqueline Walsh and Danielle Berkowitz for research assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Brad Manor, Email: bmanor@bidmc.harvard.edu.
Vera Novak, Email: vnovak@bidmc.harvard.edu.
Madelena D Costa, Email: mcosta3@bidmc.harvard.edu.
Jeffrey M Hausdorff, Email: jhausdor@bidmc.harvard.edu.
Ary L Goldberger, Email: agoldber@caregroup.harvard.edu.
Andrew C Ahn, Email: aahn1@partners.org.
Gloria Y Yeh, Email: gyeh@bidmc.harvard.edu.
C-K Peng, Email: cpeng@bidmc.harvard.edu.
Matthew Lough, Email: matthewlough@hsl.harvard.edu.
Roger B. Davis, Email: rdavis@bidmc.harvard.edu.
Mary T Quilty, Email: mquilty@hsph.harvard.edu.
Lewis A Lipsitz, Email: lipsitz@hsl.harvard.edu.
Bibliography
- 1.Lipsitz LA, Goldberger AL. Loss of ‘complexity’ and aging. Potential applications of fractals and chaos theory to senescence. Jama. 1992;267(13):1806–9. [PubMed] [Google Scholar]
- 2.Lipsitz LA. Aging as a Process of Complexity Loss. In: Deisboeck TSKJ, editor. Complex Systems Science in Biomedicine. Springer; 2006. pp. 641–54. [Google Scholar]
- 3.Goldberger AL. Non-linear dynamics for clinicians: chaos theory, fractals, and complexity at the bedside. Lancet. 1996;347(9011):1312–4. doi: 10.1016/s0140-6736(96)90948-4. [DOI] [PubMed] [Google Scholar]
- 4.Goldberger AL, Giles F. Filley lecture. Complex systems. Proc Am Thorac Soc. 2006;3(6):467–71. doi: 10.1513/pats.200603-028MS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor-Piliae RE. Tai Chi as an adjunct to cardiac rehabilitation exercise training. J Cardiopulm Rehabil. 2003;23(2):90–6. doi: 10.1097/00008483-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Taylor-Piliae RE, Froelicher ES. Effectiveness of Tai Chi exercise in improving aerobic capacity: a meta-analysis. J Cardiovasc Nurs. 2004;19(1):48–57. doi: 10.1097/00005082-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Yeh GY, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, Wayne PM, et al. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117(8):541–8. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 8.Wu G. Evaluation of the effectiveness of Tai Chi for improving balance and preventing falls in the older population--a review. J Am Geriatr Soc. 2002;50(4):746–54. doi: 10.1046/j.1532-5415.2002.50173.x. [DOI] [PubMed] [Google Scholar]
- 9.Wayne P, Krebs D, Wolf S, Gill-Body K, Scarborough D, McGibbon C, et al. Can Tai Chi improve vestibulopathic postural control? Arch Phys Med Rehabil. 2004;85(1):142–52. doi: 10.1016/s0003-9993(03)00652-x. [DOI] [PubMed] [Google Scholar]
- 10.Wu G, Hitt J. Ground contact characteristics of Tai Chi gait. Gait Posture. 2005;22(1):32–9. doi: 10.1016/j.gaitpost.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 11.Lam LC, Chau RC, Wong BM, Fung AW, Tam CW, Leung GT, et al. A 1-Year Randomized Controlled Trial Comparing Mind Body Exercise (Tai Chi) With Stretching and Toning Exercise on Cognitive Function in Older Chinese Adults at Risk of Cognitive Decline. J Am Med Dir Assoc. 2012 doi: 10.1016/j.jamda.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Taylor-Piliae RE, Newell KA, Cherin R, Lee MJ, King AC, Haskell WL. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. J Aging Phys Act. 2010;18(3):261–79. doi: 10.1123/japa.18.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li F, Harmer P, McAuley E, Fisher KJ, Duncan TE, Duncan SC. Tai Chi, self-efficacy, and physical function in the elderly. Prev Sci. 2001;2(4):229–39. doi: 10.1023/a:1013614200329. [DOI] [PubMed] [Google Scholar]
- 14.Dechamps A, Bourdel-Marchasson I. Effects of Tai Chi exercises on self-efficacy and psychological health. Edr Rev Aging Phys Act. 2007;4:25–32. [Google Scholar]
- 15.Goldberger AL, Amaral LA, Hausdorff JM, Ivanov P, Peng CK, Stanley HE. Fractal dynamics in physiology: alterations with disease and aging. Proc Natl Acad Sci U S A. 2002;99 (Suppl 1):2466–72. doi: 10.1073/pnas.012579499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Costa M, Goldberger AL, Peng CK. Multiscale entropy analysis of complex physiologic time series. Phys Rev Lett. 2002;89(6):068102. doi: 10.1103/PhysRevLett.89.068102. [DOI] [PubMed] [Google Scholar]
- 17.Costa M, Priplata A, Lipsitz LA, Wu Z, Huang NE, Goldberger AL, et al. Noise and poise: enhancement of postural complexity in the elderly with a stochastic resonance- based therapy. Eur Phys Letters. 2007;77:68008.1–08.5. doi: 10.1209/0295-5075/77/68008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Costa MD, Peng CK, Goldberger AL. Multiscale analysis of heart rate dynamics: entropy and time irreversibility measures. Cardiovasc Eng. 2008;8(2):88–93. doi: 10.1007/s10558-007-9049-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norris PR, Anderson SM, Jenkins JM, Williams AE, Morris JA., Jr Heart rate multiscale entropy at three hours predicts hospital mortality in 3,154 trauma patients. Shock. 2008;30(1):17–22. doi: 10.1097/SHK.0b013e318164e4d0. [DOI] [PubMed] [Google Scholar]
- 20.Norris PR, Stein PK, Morris JA., Jr Reduced heart rate multiscale entropy predicts death in critical illness: a study of physiologic complexity in 285 trauma patients. J Crit Care. 2008;23(3):399–405. doi: 10.1016/j.jcrc.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Peng C-K, Havlin S, Stanley HE, Goldberger AL. Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. Chaos. 1995;5(1):82–87. doi: 10.1063/1.166141. [DOI] [PubMed] [Google Scholar]
- 22.Peng CK, Hausdorff JM, Havlin S, Mietus JE, Stanley HE, Goldberger AL. Multiple-time scales analysis of physiological time series under neural control. Physica A. 1998;249:491–500. doi: 10.1016/s0378-4371(97)00508-6. [DOI] [PubMed] [Google Scholar]
- 23.Costa M, Goldberger AL, Peng CK. Multiscale entropy analysis of biological signals. Phys Rev E Stat Nonlin Soft Matter Phys. 2005;71(2 Pt 1):021906. doi: 10.1103/PhysRevE.71.021906. [DOI] [PubMed] [Google Scholar]
- 24.Peng CK, Costa M, Goldberger AL. Adaptive Data Analysis of Complex Fluctuations in Physiologic Time Series. Adv Adapt Data Anal. 2009;1(1):61–70. doi: 10.1142/S1793536909000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peng CK, Buldyrev SV, Hausdorff JM, Havlin S, Mietus JE, Simons M, et al. Non-equilibrium dynamics as an indispensable characteristic of a healthy biological system. Integr Physiol Behav Sci. 1994;29(3):283–93. doi: 10.1007/BF02691332. [DOI] [PubMed] [Google Scholar]
- 26.Pikkujamsa SM, Makikallio TH, Sourander LB, Raiha IJ, Puukka P, Skytta J, et al. Cardiac interbeat interval dynamics from childhood to senescence : comparison of conventional and new measures based on fractals and chaos theory. Circulation. 1999;100(4):393–9. doi: 10.1161/01.cir.100.4.393. [DOI] [PubMed] [Google Scholar]
- 27.Beckers F, Verheyden B, Aubert AE. Aging and nonlinear heart rate control in a healthy population. Am J Physiol Heart Circ Physiol. 2006;290(6):H2560–70. doi: 10.1152/ajpheart.00903.2005. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan DT, Furman MI, Pincus SM, Ryan SM, Lipsitz LA, Goldberger AL. Aging and the complexity of cardiovascular dynamics. Biophys J. 1991;59(4):945–9. doi: 10.1016/S0006-3495(91)82309-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iyengar N, Peng CK, Morin R, Goldberger AL, Lipsitz LA. Age-related alterations in the fractal scaling of cardiac interbeat interval dynamics. Am J Physiol. 1996;271(4 Pt 2):R1078–84. doi: 10.1152/ajpregu.1996.271.4.R1078. [DOI] [PubMed] [Google Scholar]
- 30.Vuksanovic V, Gal V. [Analysis of heart rhythm variability by linear and non-linear dynamics methods] Vojnosanit Pregl. 2005;62(9):621–7. doi: 10.2298/vsp0509621v. [DOI] [PubMed] [Google Scholar]
- 31.Schmitt DT, Ivanov P. Fractal scale-invariant and nonlinear properties of cardiac dynamics remain stable with advanced age: a new mechanistic picture of cardiac control in healthy elderly. Am J Physiol Regul Integr Comp Physiol. 2007;293(5):R1923–37. doi: 10.1152/ajpregu.00372.2007. [DOI] [PubMed] [Google Scholar]
- 32.Gomez-Garcia JA, Martinez-Vargas JD, Castellanos-Dominguez G. Complexity-based analysis for the detection of heart murmurs. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:2728–31. doi: 10.1109/IEMBS.2011.6090748. [DOI] [PubMed] [Google Scholar]
- 33.Angelini L, Maestri R, Marinazzo D, Nitti L, Pellicoro M, Pinna GD, et al. Multiscale analysis of short term heart beat interval, arterial blood pressure, and instantaneous lung volume time series. Artif Intell Med. 2007;41(3):237–50. doi: 10.1016/j.artmed.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 34.Ho KK, Moody GB, Peng CK, Mietus JE, Larson MG, Levy D, et al. Predicting survival in heart failure case and control subjects by use of fully automated methods for deriving nonlinear and conventional indices of heart rate dynamics. Circulation. 1997;96(3):842–8. doi: 10.1161/01.cir.96.3.842. [DOI] [PubMed] [Google Scholar]
- 35.Huikuri HV, Makikallio TH, Peng CK, Goldberger AL, Hintze U, Moller M. Fractal correlation properties of R-R interval dynamics and mortality in patients with depressed left ventricular function after an acute myocardial infarction. Circulation. 2000;101(1):47–53. doi: 10.1161/01.cir.101.1.47. [DOI] [PubMed] [Google Scholar]
- 36.Bigger JT, Jr, Steinman RC, Rolnitzky LM, Fleiss JL, Albrecht P, Cohen RJ. Power law behavior of RR-interval variability in healthy middle-aged persons, patients with recent acute myocardial infarction, and patients with heart transplants. Circulation. 1996;93(12):2142–51. doi: 10.1161/01.cir.93.12.2142. [DOI] [PubMed] [Google Scholar]
- 37.Makikallio TH, Hoiber S, Kober L, Torp-Pedersen C, Peng CK, Goldberger AL, et al. Fractal analysis of heart rate dynamics as a predictor of mortality in patients with depressed left ventricular function after acute myocardial infarction. TRACE Investigators. TRAndolapril Cardiac Evaluation. Am J Cardiol. 1999;83(6):836–9. doi: 10.1016/s0002-9149(98)01076-5. [DOI] [PubMed] [Google Scholar]
- 38.Arzeno NM, Kearney MT, Eckberg DL, Nolan J, Poon CS. Heart rate chaos as a mortality predictor in mild to moderate heart failure. Conf Proc IEEE Eng Med Biol Soc. 2007;2007:5051–4. doi: 10.1109/IEMBS.2007.4353475. [DOI] [PubMed] [Google Scholar]
- 39.Makikallio TH, Seppanen T, Airaksinen KE, Koistinen J, Tulppo MP, Peng CK, et al. Dynamic analysis of heart rate may predict subsequent ventricular tachycardia after myocardial infarction. Am J Cardiol. 1997;80(6):779–83. doi: 10.1016/s0002-9149(97)00516-x. [DOI] [PubMed] [Google Scholar]
- 40.Makikallio TH, Ristimae T, Airaksinen KE, Peng CK, Goldberger AL, Huikuri HV. Heart rate dynamics in patients with stable angina pectoris and utility of fractal and complexity measures. Am J Cardiol. 1998;81(1):27–31. doi: 10.1016/s0002-9149(97)00799-6. [DOI] [PubMed] [Google Scholar]
- 41.Barnett SR, Morin RJ, Kiely DK, Gagnon M, Azhar G, Knight EL, et al. Effects of age and gender on autonomic control of blood pressure dynamics. Hypertension. 1999;33(5):1195–200. doi: 10.1161/01.hyp.33.5.1195. [DOI] [PubMed] [Google Scholar]
- 42.Butler GC, Yamamoto Y, Hughson RL. Fractal nature of short-term systolic BP and HR variability during lower body negative pressure. Am J Physiol. 1994;267(1 Pt 2):R26–33. doi: 10.1152/ajpregu.1994.267.1.R26. [DOI] [PubMed] [Google Scholar]
- 43.Peng CK, Mietus JE, Liu Y, Lee C, Hausdorff JM, Stanley HE, et al. Quantifying fractal dynamics of human respiration: age and gender effects. Ann Biomed Eng. 2002;30(5):683–92. doi: 10.1114/1.1481053. [DOI] [PubMed] [Google Scholar]
- 44.Thurner S, Mittermaier C, Ehrenberger K. Change of complexity patterns in human posture during aging. Audiol Neurootol. 2002;7(4):240–8. doi: 10.1159/000063740. [DOI] [PubMed] [Google Scholar]
- 45.Duarte M, Sternad D. Complexity of human postural control in young and older adults during prolonged standing. Exp Brain Res. 2008;191(3):265–76. doi: 10.1007/s00221-008-1521-7. [DOI] [PubMed] [Google Scholar]
- 46.Collins JJ, De Luca CJ, Burrows A, Lipsitz LA. Age-related changes in open-loop and closed-loop postural control mechanisms. Exp Brain Res. 1995;104(3):480–92. doi: 10.1007/BF00231982. [DOI] [PubMed] [Google Scholar]
- 47.Bernard-Demanze L, Dumitrescu M, Jimeno P, Borel L, Lacour M. Age-related changes in posture control are differentially affected by postural and cognitive task complexity. Curr Aging Sci. 2009;2(2):139–49. [PubMed] [Google Scholar]
- 48.Lin D, Seol H, Nussbaum MA, Madigan ML. Reliability of COP-based postural sway measures and age-related differences. Gait Posture. 2008;28(2):337–42. doi: 10.1016/j.gaitpost.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 49.Kang HG, Costa MD, Priplata AA, Starobinets OV, Goldberger AL, Peng CK, et al. Frailty and the degradation of complex balance dynamics during a dual-task protocol. J Gerontol A Biol Sci Med Sci. 2009;64(12):1304–11. doi: 10.1093/gerona/glp113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manor B, Costa MD, Hu K, Newton E, Starobinets O, Kang HG, et al. Physiological complexity and system adaptability: evidence from postural control dynamics of older adults. J Appl Physiol. 2010;109(6):1786–91. doi: 10.1152/japplphysiol.00390.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hausdorff JM, Peng CK, Ladin Z, Wei JY, Goldberger AL. Is walking a random walk? Evidence for long-range correlations in stride interval of human gait. J Appl Physiol. 1995;78(1):349–58. doi: 10.1152/jappl.1995.78.1.349. [DOI] [PubMed] [Google Scholar]
- 52.Hausdorff JM, Purdon PL, Peng CK, Ladin Z, Wei JY, Goldberger AL. Fractal dynamics of human gait: stability of long-range correlations in stride interval fluctuations. J Appl Physiol. 1996;80(5):1448–57. doi: 10.1152/jappl.1996.80.5.1448. [DOI] [PubMed] [Google Scholar]
- 53.Costa M, Peng CK, Goldberger AL, Hausdorff JM. Multiscale entropy analysis of human gait dynamics. Physica A. 2003;330:53–60. doi: 10.1016/j.physa.2003.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scafetta N, Marchi D, West BJ. Understanding the complexity of human gait dynamics. Chaos. 2009;19(2):026108. doi: 10.1063/1.3143035. [DOI] [PubMed] [Google Scholar]
- 55.Hausdorff JM, Mitchell SL, Firtion R, Peng CK, Cudkowicz ME, Wei JY, et al. Altered fractal dynamics of gait: reduced stride-interval correlations with aging and Huntington’s disease. J Appl Physiol. 1997;82(1):262–9. doi: 10.1152/jappl.1997.82.1.262. [DOI] [PubMed] [Google Scholar]
- 56.Hausdorff JM, Edelberg HK, Mitchell SL, Goldberger AL, Wei JY. Increased gait unsteadiness in community-dwelling elderly fallers. Arch Phys Med Rehabil. 1997;78(3):278–83. doi: 10.1016/s0003-9993(97)90034-4. [DOI] [PubMed] [Google Scholar]
- 57.Hausdorff JM, Lertratanakul A, Cudkowicz ME, Peterson AL, Kaliton D, Goldberger AL. Dynamic markers of altered gait rhythm in amyotrophic lateral sclerosis. J Appl Physiol. 2000;88(6):2045–53. doi: 10.1152/jappl.2000.88.6.2045. [DOI] [PubMed] [Google Scholar]
- 58.Hausdorff JM, Schaafsma JD, Balash Y, Bartels AL, Gurevich T, Giladi N. Impaired regulation of stride variability in Parkinson’s disease subjects with freezing of gait. Exp Brain Res. 2003;149(2):187–94. doi: 10.1007/s00221-002-1354-8. [DOI] [PubMed] [Google Scholar]
- 59.Hausdorff JM. Gait dynamics in Parkinson’s disease: common and distinct behavior among stride length, gait variability, and fractal-like scaling. Chaos. 2009;19(2):026113. doi: 10.1063/1.3147408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Manor B, Lipsitz L. Physiologic Complexity and Aging: Implications for Physical Function and Rehabilitation. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tulppo MP, Hautala AJ, Makikallio TH, Laukkanen RT, Nissila S, Hughson RL, et al. Effects of aerobic training on heart rate dynamics in sedentary subjects. J Appl Physiol. 2003;95(1):364–72. doi: 10.1152/japplphysiol.00751.2002. [DOI] [PubMed] [Google Scholar]
- 62.Heffernan KS, Sosnoff JJ, Jae SY, Gates GJ, Fernhall B. Acute resistance exercise reduces heart rate complexity and increases QTc interval. Int J Sports Med. 2008;29(4):289–93. doi: 10.1055/s-2007-965363. [DOI] [PubMed] [Google Scholar]
- 63.Millar PJ, Levy AS, McGowan CL, McCartney N, Macdonald MJ. Isometric handgrip training lowers blood pressure and increases heart rate complexity in medicated hypertensive patients. Scand J Med Sci Sports. 2012 doi: 10.1111/j.1600-0838.2011.01435.x. [DOI] [PubMed] [Google Scholar]
- 64.Priplata AA, Patritti BL, Niemi JB, Hughes R, Gravelle DC, Lipsitz LA, et al. Noise-enhanced balance control in patients with diabetes and patients with stroke. Ann Neurol. 2006;59(1):4–12. doi: 10.1002/ana.20670. [DOI] [PubMed] [Google Scholar]
- 65.Wayne P, Kaptchuk T. Challenges inherent to Tai Chi research: Part I--Tai Chi as a complex multi-component intervention. J Altern Complement Med. 2008 doi: 10.1089/acm.2007.7170a. In Review. [DOI] [PubMed] [Google Scholar]
- 66.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and Alternative Medicine Use Among Adults: United States, 2002. Advance Data from Vital Health and Statistics. 2004;343:1–19. [PubMed] [Google Scholar]
- 67.Wojtek C-Zao. National Expert Meeting on Qi Gong and Tai Chi Consensus Report. Urbana, IL: University of Illnois at Urbana-Champaign; 2005. p. 17. [Google Scholar]
- 68.Lan C, Lai J, Chen S. Tai Chi Chuan: an ancient wisdom on exercise and health promotion. Sports Med. 2002;32:217–24. doi: 10.2165/00007256-200232040-00001. [DOI] [PubMed] [Google Scholar]
- 69.Li J, Hong Y, Chan K. Tai chi: physiological characteristics and beneficial effects on health. Br J Sports Med. 2001;35:118–56. doi: 10.1136/bjsm.35.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sandlund ES, Norlander Torsten. The Effects of Tai Chi Chuan Relaxation and Exercise on Stress Responses and Well-Being: An Overview of Research. International Journal of Stress Management. 2000;7(2):139–49. [Google Scholar]
- 71.Yeh GY, Wang CC, Wayne PM, Phillips RS. The Effect of Tai Chi Exercise on Blood Pressure: A Systematic Review. Preventive Cardiology. 2008;11:82–89. doi: 10.1111/j.1751-7141.2008.07565.x. [DOI] [PubMed] [Google Scholar]
- 72.Lee MS, Pittler MH, Taylor-Piliae RE, Ernst E. Tai chi for cardiovascular disease and its risk factors: a systematic review. J Hypertens. 2007;25(9):1974–5. doi: 10.1097/HJH.0b013e32828cc8cd. [DOI] [PubMed] [Google Scholar]
- 73.Taylor-Piliae RE. The effectiveness of Tai Chi exercise in improving aerobic capacity: an updated meta-analysis. Med Sport Sci. 2008;52:40–53. doi: 10.1159/000134283. [DOI] [PubMed] [Google Scholar]
- 74.Lai J, Lan C, Wong M, Tenh S. Two-year trends in cardiorespiratory function among older Tai Chi Chuan practitioners and sedentary subjects. J Am Geriatr Soc. 1995;43:1222–7. doi: 10.1111/j.1532-5415.1995.tb07397.x. [DOI] [PubMed] [Google Scholar]
- 75.Barrow DE, Bedford A, Ives G, O’Toole L, Channer KS. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: a randomised controlled pilot study. Postgrad Med J. 2007;83(985):717–21. doi: 10.1136/pgmj.2007.061267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yeh G, Wood M, Lorell B, Stevenson L, Eisenberg D, Wayne P, et al. Effects of Tai-Chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117(8):541–8. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 77.Yeh GY, McCarthy EP, Wayne PM, Stevenson LW, Wood MJ, Forman D, et al. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171(8):750–7. doi: 10.1001/archinternmed.2011.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Audette JF, Jin YS, Newcomer R, Stein L, Duncan G, Frontera WR. Tai Chi versus brisk walking in elderly women. Age Ageing. 2006;35(4):388–93. doi: 10.1093/ageing/afl006. [DOI] [PubMed] [Google Scholar]
- 79.Vaananen J, Xusheng S, Wang S, Laitinen T, Pekkarinen H, Lansimies E. Taichiquan acutely increases heart rate variability. Clin Physiol Funct Imaging. 2002;22(1):2–3. doi: 10.1046/j.1475-097x.2002.00355.x. [DOI] [PubMed] [Google Scholar]
- 80.Lu WA, Kuo CD. The effect of Tai Chi Chuan on the autonomic nervous modulation in older persons. Med Sci Sports Exerc. 2003;35(12):1972–6. doi: 10.1249/01.MSS.0000099242.10669.F7. [DOI] [PubMed] [Google Scholar]
- 81.Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164(5):493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 82.Komagata S, Newton R. The Effectiveness of Tai Chi on Improving Balance in Older Adults: An Evidence-based Review. Journal of Geriatric Physical Therapy. 2003;26(2):9–16. [Google Scholar]
- 83.Barnett A, Smith B, Lord SR, et al. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomized controlled trial. Age Ageing. 2003;32:407–14. doi: 10.1093/ageing/32.4.407. [DOI] [PubMed] [Google Scholar]
- 84.Li F, Fisher K, Weimer C, Shirai M. The effects of a simplified 8-form easy Tai Chi training program on functional mobility in older adults. Gerontologist. 2003;43:266–66. [Google Scholar]
- 85.Li F, Fisher KJ, Harmer P, McAuley E. Falls self-efficacy as a mediator of fear of falling in an exercise intervention for older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60(1):P34–40. doi: 10.1093/geronb/60.1.p34. [DOI] [PubMed] [Google Scholar]
- 86.Li F, Harmer P, Fisher KJ, McAuley E. Tai Chi: improving functional balance and predicting subsequent falls in older persons. Med Sci Sports Exerc. 2004;36(12):2046–52. doi: 10.1249/01.mss.0000147590.54632.e7. [DOI] [PubMed] [Google Scholar]
- 87.Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(2):187–94. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 88.Wolf S, Barnhart H, Ellison G, Coogler C. The effect of Tai Chi Quan and computerized balance training on postural stability in older subjects. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies on Intervention Techniques. Phys Ther. 1997;77(4):371–81. doi: 10.1093/ptj/77.4.371. [DOI] [PubMed] [Google Scholar]
- 89.Wolf S, Barnhart H, Kutner N, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. J Am Geriatr Soc. 1996;44(5):489–97. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 90.Wolf S, Sattin R, Kutner N, O’Grady M, Greenspan A, Gregor R. Intense Tai Chi exercise training and fall occurrences in older, transitionally frail adults: a randomized controlled trial. J Am Geriatr Soc. 2003;51(12):1693–701. doi: 10.1046/j.1532-5415.2003.51552.x. [DOI] [PubMed] [Google Scholar]
- 91.Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. J Am Geriatr Soc. 2007;55(8):1185–91. doi: 10.1111/j.1532-5415.2007.01244.x. [DOI] [PubMed] [Google Scholar]
- 92.Wu G, Liu W, Hitt J, Millon D. Spatial, temporal and muscle action patterns of Tai Chi gait. J Electromyogr Kinesiol. 2004;14(3):343–54. doi: 10.1016/j.jelekin.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 93.Wu G, Millon D. Joint kinetics during Tai Chi gait and normal walking gait in young and elderly Tai Chi Chuan practitioners. Clin Biomech (Bristol, Avon) 2008;23(6):787–95. doi: 10.1016/j.clinbiomech.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 94.Xu DQ, Li JX, Hong Y. Effect of regular Tai Chi and jogging exercise on neuromuscular reaction in older people. Age Ageing. 2005;34(5):439–44. doi: 10.1093/ageing/afi114. [DOI] [PubMed] [Google Scholar]
- 95.Mao DW, Hong Y, Li JX. Characteristics of foot movement in Tai Chi exercise. Phys Ther. 2006;86(2):215–22. [PubMed] [Google Scholar]
- 96.Mao DW, Li JX, Hong Y. The duration and plantar pressure distribution during one-leg stance in Tai Chi exercise. Clin Biomech (Bristol, Avon) 2006;21(6):640–5. doi: 10.1016/j.clinbiomech.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 97.Mao DW, Li JX, Hong Y. Plantar pressure distribution during Tai Chi exercise. Arch Phys Med Rehabil. 2006;87(6):814–20. doi: 10.1016/j.apmr.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 98.Chan SP, Luk TC, Hong Y. Kinematic and electromyographic analysis of the push movement in tai chi. Br J Sports Med. 2003;37(4):339–44. doi: 10.1136/bjsm.37.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hass CJ, Gregor RJ, Waddell DE, Oliver A, Smith DW, Fleming RP, et al. The influence of Tai Chi training on the center of pressure trajectory during gait initiation in older adults. Arch Phys Med Rehabil. 2004;85(10):1593–8. doi: 10.1016/j.apmr.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 100.Gatts SK, Woollacott MH. How Tai Chi improves balance: biomechanics of recovery to a walking slip in impaired seniors. Gait Posture. 2007;25(2):205–14. doi: 10.1016/j.gaitpost.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 101.McGibbon C, Krebs D, Parker S, Scarborough D, Wayne P, Wolf S. Tai Chi and vestibular rehabilitation improve vestibulopathic gait via different neuromuscular mechanisms: preliminary report. BMC Neurology. 2005;5(1):3. doi: 10.1186/1471-2377-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, Schmid CH. Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med. 2010;10:23. doi: 10.1186/1472-6882-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Taylor-Piliae RE, Haskell WL, Waters CM, Froelicher ES. Psychosocial responses to Tai Chi exercise in ethnic Chinese with cardiovascular disease risk factors. Circulation. 2005;112(17):U485–U86. [Google Scholar]
- 104.Wayne P, Kaptchuk T. Challenges inherent to Tai Chi Research: Part II--Defining the intervention adn optimal study design. J Altern Complement Med. 2008 doi: 10.1089/acm.2007.7170b. In Review. [DOI] [PubMed] [Google Scholar]
- 105.Wayne PM, Buring JE, Davis RB, Connors EM, Bonato P, Patritti B, et al. Tai Chi for osteopenic women: design and rationale of a pragmatic randomized controlled trial. BMC Musculoskelet Disord. 2010;11:40. doi: 10.1186/1471-2474-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wayne PM, Kiel DP, Buring JE, Connors EM, Bonato P, Yeh GY, et al. Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: a pilot pragmatic, randomized trial. BMC Complement Altern Med. 2012;12:7. doi: 10.1186/1472-6882-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Novak V, Hu K, Vyas M, Lipsitz LA. Cardiolocomotor coupling in young and elderly people. J Gerontol A Biol Sci Med Sci. 2007;62(1):86–92. doi: 10.1093/gerona/62.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Novak V, Novak P, Opfer-Gehrking TL, O’Brien PC, Low PA. Clinical and laboratory indices that enhance the diagnosis of postural tachycardia syndrome (POTS) Mayo Clinic Proc. 1998;73:1141–50. doi: 10.4065/73.12.1141. [DOI] [PubMed] [Google Scholar]
- 109.Novak V, Novak P, de Champlain J, Le Blanc AR, Martin R, Nadeau R. Influence of respiration on heart rate and blood pressure fluctuations. J Appl Physiol. 1993;74(2):617–26. doi: 10.1152/jappl.1993.74.2.617. [DOI] [PubMed] [Google Scholar]
- 110.Sorond FA, Serrador JM, Jones RN, Shaffer ML, Lipsitz LA. The sit-to-stand technique for the measurement of dynamic cerebral autoregulation. Ultrasound Med Biol. 2009;35(1):21–9. doi: 10.1016/j.ultrasmedbio.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23(3):329–42. doi: 10.1002/mds.21720. quiz 472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fried LP, Tangen CM, Walston JD, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for phenotype. J Gerontol Med Sci. 2001;56A:M146–M56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 113.Beauchet O, Annweiler C, Allali G, Berrut G, Herrmann FR, Dubost V. Recurrent falls and dual task-related decrease in walking speed: is there a relationship? J Am Geriatr Soc. 2008;56(7):1265–9. doi: 10.1111/j.1532-5415.2008.01766.x. [DOI] [PubMed] [Google Scholar]
- 114.Beauchet O, Annweiler C, Allali G, Berrut G, Dubost V. Dual task-related changes in gait performance in older adults: a new way of predicting recurrent falls? J Am Geriatr Soc. 2008;56(1):181–2. doi: 10.1111/j.1532-5415.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 115.Shinkai S, Watanabe S, Kumagai S, Fujiwara Y, Amano H, Yoshida H, et al. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age Ageing. 2000;29(5):441–6. doi: 10.1093/ageing/29.5.441. [DOI] [PubMed] [Google Scholar]
- 116.Vereeck L, Wuyts F, Truijen S, Van de Heyning P. Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol. 2008;47(2):67–75. doi: 10.1080/14992020701689688. [DOI] [PubMed] [Google Scholar]
- 117.Kuh D, Bassey EJ, Butterworth S, Hardy R, Wadsworth ME. Grip strength, postural control, and functional leg power in a representative cohort of British men and women: associations with physical activity, health status, and socioeconomic conditions. J Gerontol A Biol Sci Med Sci. 2005;60(2):224–31. doi: 10.1093/gerona/60.2.224. [DOI] [PubMed] [Google Scholar]
- 118.Bosco C, Luhtanen P, Komi PV. A simple method for measurement of mechanical power in jumping. Eur J Appl Physiol Occup Physiol. 1983;50(2):273–82. doi: 10.1007/BF00422166. [DOI] [PubMed] [Google Scholar]
- 119.Fujita Y, Nakamura Y, Hiraoka J, Kobayashi K, Sakata K, Nagai M, et al. Physical-strength tests and mortality among visitors to health-promotion centers in Japan. J Clin Epidemiol. 1995;48(11):1349–59. doi: 10.1016/0895-4356(95)00533-1. [DOI] [PubMed] [Google Scholar]
- 120.Perry MC, Carville SF, Smith IC, Rutherford OM, Newham DJ. Strength, power output and symmetry of leg muscles: effect of age and history of falling. Eur J Appl Physiol. 2007;100(5):553–61. doi: 10.1007/s00421-006-0247-0. [DOI] [PubMed] [Google Scholar]
- 121.Bohannon RW. Hand-grip dynamometry predicts future outcomes in aging adults. J Geriatr Phys Ther. 2008;31(1):3–10. doi: 10.1519/00139143-200831010-00002. [DOI] [PubMed] [Google Scholar]
- 122.Norkin C. Measurment of Joint Motion: A Guide to Goniometry. 3. 2003. [Google Scholar]
- 123.Jones CJ, Rikli RE, Max J, Noffal G. The reliability and validity of a chair sit-and-reach test as a measure of hamstring flexibility in older adults. Res Q Exerc Sport. 1998;69(4):338–43. doi: 10.1080/02701367.1998.10607708. [DOI] [PubMed] [Google Scholar]
- 124.Heil DP, Freedson PS, Ahlquist LE, Price J, Rippe JM. Nonexercise regression models to estimate peak oxygen consumption. Med Sci Sports Exerc. 1995;27(4):599–606. [PubMed] [Google Scholar]
- 125.Jackson AS, Beard EF, Wier LT, Ross RM, Stuteville JE, Blair SN. Changes in aerobic power of men, ages 25–70 yr. Med Sci Sports Exerc. 1995;27(1):113–20. [PubMed] [Google Scholar]
- 126.Ware JE, Kosinski M. Interpreting SF-36 summary health measures: a response. Qual Life Res. 2001;10(5):405–13. doi: 10.1023/a:1012588218728. discussion 15–20. [DOI] [PubMed] [Google Scholar]
- 127.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): a conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 128.Bowie CR, Harvey PD. Administration and interpretation of the Trail Making Test. Nat Protoc. 2006;1(5):2277–81. doi: 10.1038/nprot.2006.390. [DOI] [PubMed] [Google Scholar]
- 129.Arbuthnott K, Frank J. Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. J Clin Exp Neuropsychol. 2000;22(4):518–28. doi: 10.1076/1380-3395(200008)22:4;1-0;FT518. [DOI] [PubMed] [Google Scholar]
- 130.Franzen M. Cross-validation of the alternative forms of reliability of the Trail Making Test. Clin Neuropsyhcol. 1996;10:125–29. [Google Scholar]
- 131.Strauss E, Sherman E, Spreeen A. A compendium of neuropsychological tests: Administration, norms, and commentary. 3. 2006. [Google Scholar]
- 132.Ross TP, Calhoun E, Cox T, Wenner C, Kono W, Pleasant M. The reliability and validity of qualitative scores for the Controlled Oral Word Association Test. Arch Clin Neuropsychol. 2007;22(4):475–88. doi: 10.1016/j.acn.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 133.Ross TP, Furr AE, Carter SE, Weinberg M. The psychometric equivalence of two alternate forms of the Controlled Oral Word Association Test. Clin Neuropsychol. 2006;20(3):414–31. doi: 10.1080/13854040590967153. [DOI] [PubMed] [Google Scholar]
- 134.Brown AK, Liu-Ambrose T, Tate R, Lord SR. The effect of group-based exercise on cognitive performance and mood in seniors residing in intermediate care and self-care retirement facilities: a randomised controlled trial. Br J Sports Med. 2009;43(8):608–14. doi: 10.1136/bjsm.2008.049882. [DOI] [PubMed] [Google Scholar]
- 135.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 136.Rovner BW, Folstein MF. Mini-mental state exam in clinical practice. Hosp Pract (Off Ed) 1987;22(1A):99, 103, 06, 10. [PubMed] [Google Scholar]
- 137.Tangalos EG, Smith GE, Ivnik RJ, Petersen RC, Kokmen E, Kurland LT, et al. The Mini-Mental State Examination in general medical practice: clinical utility and acceptance. Mayo Clin Proc. 1996;71(9):829–37. doi: 10.4065/71.9.829. [DOI] [PubMed] [Google Scholar]
- 138.McNair DM, Lorr M, Droppelman LF. Manual for the profile of mood states. San Diego: EDITS Educational and Industrial Testing Services, Inc; 1992. [Google Scholar]
- 139.Brown DR, Wang Y, Ward A, Ebbeling CB. Chronic psychlogical effects of exercise and exercise plus cognitive strategies. Med Sci Sports. 1995;27(5):765–75. [PubMed] [Google Scholar]
- 140.Myers SS, Phillips RS, Davis RB, Cherkin DC, Legedza A, Kaptchuk TJ, Hrbek A, Buring JE, Post D, Connelly MT, Eisenberg DM. Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med. 2008 doi: 10.1007/s11606-007-0460-5. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Costa M, Goldberger AL, Peng CK. Multiscale entropy to distinguish physiologic and synthetic RR time series. Comput Cardiol. 2002;29:137–40. [PubMed] [Google Scholar]
- 142.Richman JS, Lake DE, Moorman JR. Sample entropy. Methods Enzymol. 2004;384:172–84. doi: 10.1016/S0076-6879(04)84011-4. [DOI] [PubMed] [Google Scholar]
- 143.Judd CA, Kenny DA. Process analysis: estimating mediation in evaluation research. Evaluation Research. 1981;5:602–19. [Google Scholar]
- 144.Kuusela TA, Jartti TT, Tahvanainen KU, Kaila TJ. Nonlinear methods of biosignal analysis in assessing terbutaline-induced heart rate and blood pressure changes. Am J Physiol Heart Circ Physiol. 2002;282(2):H773–83. doi: 10.1152/ajpheart.00559.2001. [DOI] [PubMed] [Google Scholar]
- 145.Wayne PM, Fuerst ML. Harvard Medical School Guide to Tai Chi. Boston: Harvard Health Publications and Shambala Press; 2013. [Google Scholar]
- 146.Caldwell K, Emery L, Harrison M, Greeson J. Changes in mindfulness, well-being, and sleep quality in college students through taijiquan courses: a cohort control study. J Altern Complement Med. 2011;17(10):931–8. doi: 10.1089/acm.2010.0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Caldwell K, Harrison M, Adams M, Quin RH, Greeson J. Developing mindfulness in college students through movement-based courses: effects on self-regulatory self-efficacy, mood, stress, and sleep quality. J Am Coll Health. 2010;58(5):433–42. doi: 10.1080/07448480903540481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol Med. 2010;40(8):1239–52. doi: 10.1017/S0033291709991747. [DOI] [PubMed] [Google Scholar]
- 149.Killingsworth MA, Gilbert DT. A wandering mind is an unhappy mind. Science. 2010;330(6006):932. doi: 10.1126/science.1192439. [DOI] [PubMed] [Google Scholar]
- 150.Lang EV, Berbaum KS, Faintuch S, Hatsiopoulou O, Halsey N, Li X, et al. Adjunctive self-hypnotic relaxation for outpatient medical procedures: a prospective randomized trial with women undergoing large core breast biopsy. Pain. 2006;126(1–3):155–64. doi: 10.1016/j.pain.2006.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Eremin O, Walker MB, Simpson E, Heys SD, Ah-See AK, Hutcheon AW, et al. Immuno-modulatory effects of relaxation training and guided imagery in women with locally advanced breast cancer undergoing multimodality therapy: a randomised controlled trial. Breast. 2009;18(1):17–25. doi: 10.1016/j.breast.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 152.Achterberg J. Imagery In Healing: Shamanism and Modern Medicine. Austin, Texas: Shambhala Publications, Inc; 1985. [Google Scholar]
- 153.Lan C, Chen SY, Lai JS. The exercise intensity of tai chi chuan. Med Sport Sci. 2008;52:12–9. doi: 10.1159/000134225. [DOI] [PubMed] [Google Scholar]
- 154.Wayne PM, Kiel DP, Krebs DE, Davis RB, Savetsky-German J, Connelly M, et al. The effects of Tai Chi on bone mineral density in postmenopausal women: a systematic review. Arch Phys Med Rehabil. 2007;88(5):673–80. doi: 10.1016/j.apmr.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 155.Lan C, Lai JS, Chen SY, Wong MK. 12-month Tai Chi training in the elderly: its effect on health fitness. Med Sci Sports Exerc. 1998;30(3):345–51. doi: 10.1097/00005768-199803000-00003. [DOI] [PubMed] [Google Scholar]
- 156.Lee EN, Kim YH, Chung WT, Lee MS. Tai chi for disease activity and flexibility in patients with ankylosing spondylitis--a controlled clinical trial. Evid Based Complement Alternat Med. 2008;5(4):457–62. doi: 10.1093/ecam/nem048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chan AW, Lee A, Suen LK, Tam WW. Tai chi Qigong improves lung functions and activity tolerance in COPD clients: a single blind, randomized controlled trial. Complement Ther Med. 2011;19(1):3–11. doi: 10.1016/j.ctim.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 158.Mead J, Yoshino K, Kikuchi Y, Barnas GM, Loring SH. Abdominal pressure transmission in humans during slow breathing maneuvers. J Appl Physiol. 1990;68(5):1850–3. doi: 10.1152/jappl.1990.68.5.1850. [DOI] [PubMed] [Google Scholar]
- 159.Raupach T, Bahr F, Herrmann P, Luethje L, Heusser K, Hasenfuss G, et al. Slow breathing reduces sympathoexcitation in COPD. Eur Respir J. 2008;32(2):387–92. doi: 10.1183/09031936.00109607. [DOI] [PubMed] [Google Scholar]
- 160.Kubzansky LD, Sparrow D, Jackson B, Cohen S, Weiss ST, Wright RJ. Angry breathing: A prospective study of hostility and lung function in the Normative Aging Study. Thorax. 2006;61(10):863–8. doi: 10.1136/thx.2005.050971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mookadam F, Arthur HM. Social support and its relationship to morbidity and mortality after acute myocardial infarction: systematic overview. Arch Intern Med. 2004;164(14):1514–8. doi: 10.1001/archinte.164.14.1514. [DOI] [PubMed] [Google Scholar]
- 162.Hafner S, Emeny RT, Lacruz ME, Baumert J, Herder C, Koenig W, et al. Association between social isolation and inflammatory markers in depressed and non-depressed individuals: results from the MONICA/KORA study. Brain Behav Immun. 2011;25(8):1701–7. doi: 10.1016/j.bbi.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 163.Koenig HGC, Jay Harvey. The Link between Religion and Health. New York, NY: Oxford University Press; 2002. [Google Scholar]