Abstract
Objective
We sought to determine whether race or ethnicity is independently associated with mortality or intensive care unit (ICU) length of stay (LOS) among critically ill patients after accounting for patients' clinical and demographic characteristics including socioeconomic status and resuscitation preferences.
Design
Historical cohort study of patients hospitalized in intensive care units.
Setting
Adult intensive care units in 35 California hospitals during the years 2001-2004.
Patients
A total of 9,518 ICU patients (6334 white, 655 black, 1917 Hispanic and 612 Asian/Pacific Islander patients).
Measurements and Main Results
The primary outcome was risk-adjusted mortality and a secondary outcome was risk-adjusted ICU LOS. Crude hospital mortality was 15.9% among the entire cohort. Asian patients had the highest crude hospital mortality at 18.6% and black patients had the lowest at 15.0%. After adjusting for age and gender, Hispanic and Asian patients had a higher risk of death compared to white patients, but these differences were not significant after additional adjustment for severity of illness. Black patients had more acute physiologic derangements at ICU admission and longer unadjusted ICU LOS. ICU LOS was not significantly different among racial/ethnic groups after adjustment for demographic, clinical, socioeconomic factors and do-not-resuscitate status. In an analysis restricted only to those who died, decedent black patients averaged 1.1 additional days in the ICU (95% CI – 0.26 to 2.6) compared to white patients who died, although this was not statistically significant.
Conclusions
Hospital mortality and ICU LOS did not differ by race or ethnicity among this diverse cohort of critically ill patients after adjustment for severity of illness, resuscitation status, SES, insurance status and admission type. Black patients had more acute physiologic derangements at ICU admission and were less likely to have a DNR order. These results suggest that among ICU patients, there are not racial or ethnic differences in mortality within individual hospitals. If disparities in ICU care exist, they may be explained by differences in the quality of care provided by hospitals that serve high proportions of minority patients.
Keywords: critical care, intensive care unit, race, ethnicity, mortality, epidemiology
While there is a vast body of literature describing racial and ethnic differences in the use of health care services, quality of health care, and health outcomes in almost every field of medicine, relatively few studies have investigated racial and ethnic differences among critically ill patients.1 Prior studies of critically ill patients have been limited by small sample sizes, inadequate risk adjustment, or a failure to examine underlying factors including socioeconomic status (SES) and end-of-life preferences that could shed light on why disparities in care and outcomes might exist.2-4 Further, Hispanics, now the largest minority group in the United States, have not been included in most prior work examining racial and ethnic differences in outcomes among the critically ill.
The few studies that have examined racial differences in outcomes among critically ill patients have conflicting results. Williams and colleagues performed a study using data from forty hospitals from 1988-1990 and found that fewer resources were used for critically ill black patients compared with white patients.4 White patients received more monitoring, laboratory testing and more life supportive therapies compared with black patients. However, this study did not find significant differences in hospital mortality after adjustment for patient characteristics. 4 A recent study that examined outcomes of critically ill patients with acute lung injury (ALI) found that black and Hispanic patients had a higher risk of death compared to white patients.2 Possible explanations for these differing results include regional differences in care,5 incomplete adjustment for SES 6, 7 and severity of illness and failure to account for differences in end-of-life preferences.8, 9 Importantly, there has been no study comparing risk-adjusted outcomes among critically ill minority and white patients that addresses these issues. Therefore, we sought to examine the association between race/ethnicity and hospital mortality and length of stay in a diverse population of critically ill patients while taking into account severity of illness, do-not-resuscitate (DNR) status and SES.
Materials and Methods
We conducted a secondary analysis of a prospective cohort study using the California Intensive Care Outcomes (CALICO) dataset. The CALICO project was originally designed to both measure and compare hospital-specific ICU quality of care and efficiency10 measures among California hospitals. Extensive information about patient demographics and clinical characteristics including severity of illness and DNR status was collected in order to compare three primary risk adjustment models commonly used for benchmarking of ICU mortality and ICU length of stay, the Mortality Probability Model, the Simplified Acute Physiology Score, and the Acute Physiology and Chronic Health Evaluation model.11
Hospital Selection
All California hospitals with an ICU and at least 50 beds were sent a recruiting packet asking for their participation in the CALICO project. A network of 35 volunteer hospitals was then established through mailings and regional presentations. Hospitals that volunteered provided nurses for data abstraction.
Patient Selection
Data was collected between 2001 and 2004. Inclusion criteria were age ≥ 18 years and ICU stay ≥ 4 hours. Patients with burns, trauma, or coronary bypass graft were excluded, as these conditions were not examined across all the risk adjustment models. Patients who had more than one ICU admission during a single hospitalization were included only once, and data was abstracted from the index admission.1 We also excluded patients without hospital mortality information and those without linkable identifiers to California's Office of Statewide Health Planning and Development's (OSHPD) patient discharge database (PDD), our primary source for race/ethnicity and socioeconomic status. In order to decrease the burden of data collection among smaller institutions with fewer resources, the sample size at each hospital was a function of its annual ICU admissions.12
Data Collection
Data collectors underwent extensive training and automated software was used to block or query implausible data entry. Data collectors attended a training session, completed sample chart abstractions, and received feedback on their performance before starting data collection. Data abstraction was duplicated by auditors on a 5% random sample of patients with excellent inter-rater reliability.12
Hospital Sample Characteristics
We compared the hospital characteristics (i.e., number of beds, JCAHO accreditation, Accreditation Council for Graduate Medical Education [ACGME] residency, medical school affiliation, ownership, and number of medical/surgical ICU beds) of our sample to all California hospitals with ≥ 50 hospital beds using the 2006 American Hospital Association survey.
Patient Demographic Characteristics
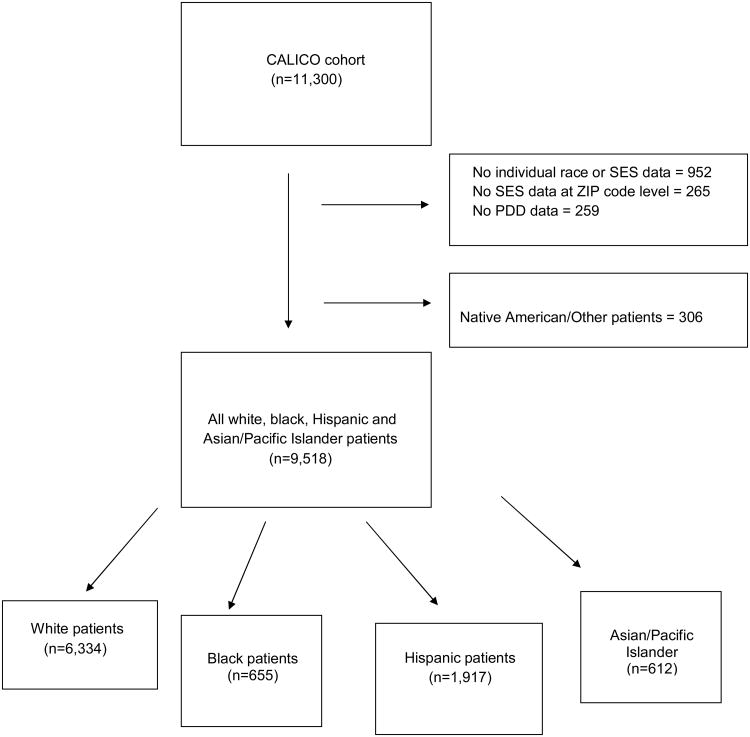
Race/ethnicity was assigned through linkage with the California Office of Statewide Health Planning and Development's (OSHPD) Patient Discharge Database (PDD). Both race and ethnicity were obtained by the hospital via patient self-report upon presentation to the emergency department or at hospital admission. 13 The PDD classifies race/ethnicity into five mutually exclusive categories: white/non-Hispanic, black/non-Hispanic, Hispanic, Asian/Pacific Islander, or Native American/other. Patients reported as Hispanic were categorized as Hispanic regardless of race. Because the racial and ethnic composition of the group designated as Native American/other is unknown, and because the limited sample size of this population resulted in unreliable estimates, we limited our analysis to patients identified as white, black, Hispanic or Asian (Figure 1).
Figure 1. Inclusion and Exclusion Criteria, SES=socioeconomic status, PDD=Patient Discharge Database.
SES was assessed using patients' ZIP codes from the PDD. Patients' ZIP codes were then geocoded and linked with socioeconomic variables from the 2000 U.S. census at the block-group level. Seven census variables were then used to create an index of SES that was developed and validated by Bonito and colleagues for the Agency for Healthcare Research and Quality.14 This index was created in order to separate the impact of SES from the effect of race/ethnicity. Based largely upon prior work from Krieger and colleagues15-18, the index was derived from a principal components analysis of area-level census measures that are related to, or are proxies for, SES. 15 These measures include: 1) percentage of persons aged 16 years or older in the labor force who are unemployed and actively seeking work, 2) percentage of persons below the federally defined poverty line, 3) median household income, 4) median value of owner-occupied homes, 5) percentage of persons aged ≥ 25 years with less than a 12th-grade education, 6) percentage of persons aged ≥ 25 years with at least 4 years of college, and 7) percentage of households containing one or more person per room. The index can range from 0 to 100, with lower scores corresponding to a lower SES.
End-of-life preferences
We used an individual's do-not-resuscitate (DNR) status as a measure of resuscitation preference. DNR status was assessed at hospital admission and was abstracted from the medical record.
Patient severity of illness
All patient-level clinical data and length of stay were abstracted from the chart. We used this data to generate a summary estimate of the patients' severity of illness. Severity of illness estimates at ICU admission were assessed with the Acute Physiology and Chronic Health Evaluation® IV (APACHE® IV) Acute Physiology Score (APS).9, 19 Key factors included in the APACHE APS include vital signs (e.g. blood pressure and heart rate) and laboratory values measured during the first 24 hours of ICU admission.
Insurance status
Insurance status was categorized based on the expected source of payment (Medicare, Medicaid, private insurance [any], other [e.g., other government insurance], and uninsured [indigent, charity, no charge]) as recorded in the PDD.
Patient Outcomes
The primary outcome was in-hospital mortality. ICU length of stay was a secondary outcome measured in days and truncated at 30 days to reduce the impact of outliers.(4,5).
Statistical Analysis
Characteristics of CALICO hospitals and all California hospitals were compared using chi-square and Wilcoxon rank sum tests. Demographic and clinical characteristics of the different race/ethnicity groups were compared using a chi-square or Fisher exact test for categorical variables and an analysis of variance (ANOVA) or Kruskal-Wallis test for continuous variables.
To estimate the independent association between race/ethnicity and in-hospital mortality, we fit staged logistic regression models using hospital mortality as the dependent variable. Similarly, we used staged linear regression models to determine the independent effect of race/ethnicity on the continuous outcome of ICU LOS.10 We included variables in the models if they were associated with race/ethnicity in the bivariate analyses (p ≤ 0.20) or if they were considered clinically relevant on an a priori basis. The initial model included race, age and gender. We then examined the effect of severity of illness by adding APS. In addition, we included admission type (medical admission, elective surgery, emergency surgery) as this may be an additional proxy for severity of illness. Because published reports have shown variation in DNR status and insurance status by race,20-22 and DNR status is known to be associated with an increased risk of death,23 we added DNR status to our model. Finally, we added SES index and expected source of payment to understand whether any effect of race/ethnicity was independent of socioeconomic status and insurance status. Random effects hierarchical logistic regression modeling was used in order to account for patient clustering at the hospital level for all multivariable analyses.
Length of Stay
Because recent studies have shown that minority patients receive more life-sustaining treatments at the end-of life,24 they may have longer ICU LOS prior to death compared to white patients. We performed a sub-group analysis restricted only to those who died to determine whether there were any racial/ethnic differences in ICU LOS among patients who died. In addition, to determine if DNR status was a significant factor explaining the association between race/ethnicity and ICU LOS, we compared ICU LOS in two fully adjusted regression models, one including and one excluding DNR status.
Sensitivity Analysis
To evaluate whether race/ethnicity modified the effect of age, gender, severity of illness, SES or DNR status on mortality, we evaluated possible interactions among these. The presence of interaction was assessed using the likelihood ratio test. An interaction was considered statistically significant if the p value was ≤ 0.10, to ensure that clinically significant interactions were not overlooked. The institutional review boards of the University of California, San Francisco and the State of California approved the study. All analyses were performed using STATA 9.2 (StataCorp, College Station, TX).
Results
The final study sample included 9,518 patients in 35 hospitals (Figure 1). There were no significant differences in hospital characteristics comparing CALICO hospitals to all California hospitals.12 A total of 6334 white, 655 black, 1917 Hispanic and 612 Asian/Pacific Islander patients were included in the sample. There were several significant demographic differences between the racial and ethnic groups (Table 1). White patients were the oldest on average and were more likely to be male. White patients were more likely to have Medicare or private insurance as the expected source of payment. Hispanic patients had the lowest SES index score and white patients the highest. Clinical characteristics also varied significantly between groups. Hispanic patients were most likely to have a comorbid condition. Black patients were most likely to have a medical admission while white patients were most likely to have an admission for elective surgery. Black patients had the most physiologic derangements at ICU admission, as measured by the Acute Physiology Score (APS). Black and Hispanic patients had the highest median length of ICU stay. White patients were most likely to have a DNR advanced directive at hospital admission. White patients were more likely to be discharged to a long-term acute care facility or skilled nursing facility.
Table 1. Demographic and Clinical Characteristics of the CALICO cohort by Race/Ethnicity*.
| Characteristic | White (n=6334) | Black (n=655) | Hispanic (n=1917) | Asian/Pacific Islander (n=612) | P value |
|---|---|---|---|---|---|
| Age | 64.8 ± 16.7 | 57.6 ± 17.2 | 57.1 ± 18.5 | 63.3 ± 17.1 | <0.001 |
| Male | 3291 (52.3) | 320 (49.0) | 1062 (55.5) | 341 (56.1) | 0.006 |
| APACHE IV probability of death, Median (IQR)† | 0.06 (0.02 to 0.18) | 0.06 (0.02 to 0.19) | 0.06 (0.02 to 0.19) | 0.08 (0.03 to 0.23) | 0.0046 |
| Acute Physiology Score, Median (IQR)† | 37 (25 to 56) | 41 (27 to 63) | 39 (26 to 60) | 39 (25 to 61) | <0.001 |
| Comorbid conditions | <0.001 | ||||
| None | 5551 (87.6) | 577 (88.1) | 1611 (84.0) | 521 (85.1) | |
| Cirrhosis | 112 (1.8) | 8 (1.2) | 88 (4.6)) | 14 (2.3) | |
| Immunosuppression | 261 (4.1) | 25 (3.8) | 75 (3.9) | 17 (2.8) | |
| Metastatic Cancer | 236 (3.7) | 15 (2.3) | 58 (3.0) | 38 (6.2) | |
| Lymphoma | 46 (0.7) | 3 (0.5) | 24 (1.3) | 5 (0.8) | |
| Hepatic Failure | 58 (0.9) | 5 (0.8) | 40 (2.1) | 8 (1.3) | |
| AIDS | 20 (0.3) | 18 (2.8) | 8 (0.4) | 2 (0.3) | |
| Leukemia | 50 (0.8) | 4 (0.6) | 13 (0.7) | 7 (1.1) | |
| Medical/Operative Status | <0.001 | ||||
| Medical Admission | 4800 (75.8) | 555 (84.7) | 1554 (81.1) | 488 (79.7) | |
| Elective Surgery | 1257 (19.9) | 77 (11.8) | 275 (14.4) | 101 (16.5) | |
| Emergency Surgery | 277 (4.4) | 23 (3.5) | 88 (4.6) | 23 (3.8) | |
| Expected source of payment | <0.001 | ||||
| Medicare | 3513 (55.5) | 270 (41.2) | 764 (39.9) | 240 (39.2) | |
| Medicaid | 612 (9.7) | 145 (22.1) | 543 (28.3) | 185 (30.2) | |
| Private | 1798 (28.4) | 169 (25.8) | 357 (18.6) | 127 (20.8) | |
| Other | 411 (6.5) | 71 (10.8) | 253 (13.2) | 60 (9.8) | |
| Full Code at Admission | 5971 (94.3) | 636 (97.1) | 1858 (96.9) | 583 (95.3) | <0.001 |
| AHRQ SES index score‡ | 48.6 (3.7) | 46.9 (4.1) | 45.1 (4.3) | 48.5 (4.0) | <0.001 |
| Discharge Disposition | <0.001 | ||||
| Home | 4352 (68.7) | 454 (69.3) | 1292 (67.4) | 437 (71.4) | |
| Long-term acute care | 415 (6.6) | 40 (6.1) | 89 (4.6) | 22 (3.6) | |
| Skilled nursing facility | 811 (12.8) | 83 (12.7) | 142 (7.4) | 102 (8.3) | |
| Other | 756 (11.9) | 78 (11.9) | 394 (20.1) | 102 (16.7) |
Values are mean ± SD or n (%), unless otherwise indicated.
APACHE IV® predicted mortality and APS were measured at ICU admission.
Agency for Healthcare Research and Quality Socioeconomic Status index score
Overall, crude hospital mortality was 15.9% among the entire cohort. Asian patients had the highest crude hospital mortality at 18.6% and black patients had the lowest at 15.0%. After adjusting for age and gender, Asian patients still had a significantly increased risk of hospital mortality compared to white patients (OR=1.37, 95% CI, 1.09-1.72 Table 2), as did Hispanic patients (OR=1.40, 95% CI 1.20-1.62). After adjustment for APS and admission type, this increased risk of death for Asian and Hispanic patients was attenuated and was no longer statistically significant (Asian patients, OR=1.05, 95% CI 0.78-1.04, Hispanic patients OR=1.06 95% CI, 0.87-1.28). Further adjustment for, DNR status, SES, and expected source of payment did not substantively change any of the point estimates and no racial/ethnic group had a statistically significant higher or lower risk of death compared to white patients.
Table 2. Association of race/ethnicity and hospital mortality.
| Outcome | White | Black | Hispanic | Asian/Pacific Islander |
|---|---|---|---|---|
| Hospital mortality | Odds Ratio (95% CI) | Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| Model 1* | Reference | 1.15 (0.91-1.46) | 1.40 (1.20-1.62) | 1.37 (1.09-1.72) |
| Model 2† | Reference | 0.91 (0.68-1.21) | 1.09 (0.90-1.31) | 1.18 (0.89-1.56) |
| Model 3‡ | Reference | 0.91 (0.68-1.23) | 1.12 (0.92-1.35) | 1.19 (0.89-1.58) |
| Model 4§ | Reference | 0.91 (0.67 -1.21) | 1.10 (0.90-1.22) | 1.18 (0.88-1.57) |
Adjusted for age + gender
Adjusted for age, gender + APS + admission type
Adjusted for age, gender, APS + admission type + DNR status
Adjusted for age, gender, APS, + admission type + DNR status + SES + expected source of payment
All analyses were adjusted for hospital effects.
SES=socioeconomic status, DNR=do not resuscitate Bold face type indicates statistical significance.
Overall the median ICU length of stay (LOS) was 2.0 days IQR (1.0-4.1 days). Black and Hispanic patients had the longest crude ICU LOS at 2.1 days (IQR Black patients 1.1-4.9, Hispanic patients 1.1-4.3). After adjusting for age and gender, black patients had a significantly longer ICU LOS compared to white patients (black patients ICU LOS = 0.68 days longer 95% CI 0.26-1.09, Table 3). Further adjustment for APS and admission type, DNR status, SES, and expected source of payment attenuated this difference, making it no longer statistically significant (black patients ICU LOS =0.39 days longer, 95% CI -0.14 – 0.79). None of the other racial/ethnic groups had a statistically significant longer or shorter ICU LOS compared with white patients.
Table 3. Association of race/ethnicity and ICU length of stay.
| Outcome | Mean Difference In ICU Length of Stay (95% CI) | |||
|---|---|---|---|---|
|
| ||||
| White | Black | Hispanic | Asian/Pacific Islander | |
| Model 1* | Reference | 0.68 (0.27 to 1.09) | 0.11 (-0.17 to 0.39) | 0.42 (-0.01 to 0.85) |
| Model 2† | Reference | 0.52 (0.12 to 0.92) | -0.11 (-0.38 to 0.16) | 0.33 (-0.09 to 0.74) |
| Model 3‡ | Reference | 0.50 (0.10 to 0.90) | -0.13 (-0.09 to 0.73) | 0.32 (-0.09 to 0.74) |
| Model 4§ | Reference | 0.39 (-0.01 to 0.79) | -0.24 (-0.52 to 0.05) | 0.23 (-0.19 to 0.65) |
Adjusted for age + gender
Adjusted for age, gender + APS
Adjusted for age, gender, APS + DNR status
Adjusted for age, gender, APS, DNR status + SES + expected source of payment + admission type
All analyses were adjusted for hospital effects.
SES=socioeconomic status, DNR=do not resuscitate APS= acute physiology score
Bold face type indicates statistical significance.
When we performed an analysis of ICU LOS restricted only to those who died, the adjusted LOS was considerably longer for black patients compared to the other racial groups. In this sub-group analysis that adjusted for age, gender, APS, admission type, DNR status, SES, and expected source of payment black patients who died averaged 1.1 additional days in the ICU (95% CI – 0.26 to 2.6) compared to white patients who died. However, this was not a statistically significant difference. DNR status did not play a significant role in explaining this increased ICU LOS among black patients as the point estimate did not change significantly when DNR status was removed from the model (1.3 days, 95% CI -0.15 to 2.7).
Sensitivity Analyses
There were no significant interactions between race/ethnicity and age, gender, severity of illness, SES or DNR status (p>0.10 for all interaction terms). Accounting for patient clustering within hospitals using hierarchical analyses did not substantively change the point estimates or confidence intervals for hospital mortality or ICU LOS.
Discussion
Among this large, racially and ethnically diverse cohort of critically ill patients from California ICUs, we found no significant racial or ethnic disparities in hospital mortality after adjusting for patient characteristics including severity of illness, admissions type, SES, DNR status and insurance status. However, black patients had more acute physiologic derangements at ICU admission and had longer unadjusted ICU LOS. This longer ICU LOS among black patients seemed to be mediated primarily by acute severity of illness and socioeconomic status.
A study by Yergan and colleagues performed in the 1980's demonstrated that racial/ethnic minorities were significantly less likely to be admitted to the ICU compared with white patients who had the same diagnosis.25 Twenty years later, whether minorities are still less likely to be admitted to the ICU is unknown, but some aspects of our findings and other recent literature suggest that this issue may persist. Our observation that black patients have greater severity of illness with more physiologic derangements at ICU admission has been made by others, and suggests that there may be delays in ICU admission or delays in presentation to the hospital that are accounting for these differences.2, 26 A recent study examining emergency department (ED) boarding times for patients admitted to the hospital showed that ED LOS was significantly longer for black patients admitted to ICU beds.27 Our study revealed that black patients had longer unadjusted ICU LOS compared to white patients. That black patients have more physiologic derangements at ICU admission seems to explain part of this finding. An additional explanation involves the differences in LOS among patients who lived versus those who died. A recent study showed that at the end of life, black and Hispanic patients having strikingly greater use of life-sustaining interventions, such as mechanical ventilation, dialysis and gastrostomy tubes.24 These differences may explain why we found a longer unadjusted ICU LOS among black patients in our study. In addition, racial and ethnic disparities in preventive care28, 29 and management of chronic diseases30, 31 increase the likelihood that minority patients will present to the hospital at more advanced stages of disease, resulting in fewer elective admissions and higher severity of illness. Improving access to and utilization of high quality primary care32, 33 may be keys to eliminating these disparities in acute severity of illness.
Although minority patients in our cohort presented with greater severity of illness and had fewer elective admissions we did not observe racial or ethnic differences in mortality after adjustments for severity of illness. This suggests that despite possible disparities in care preceding ICU admission (e.g. decreased access to primary care, or lack of timely triage), once patients are admitted to the ICU their hospital mortality outcomes are similar. There have been very few large, multi-center studies examining outcomes by race/ethnicity across broad ICU populations. A 42 center U.S. study conducted from 1989-1990 found that, despite having more physiologic derangements at admission, critically ill black patients did not have a higher risk of death compared to white patients after adjustment for severity of illness.4 Notably, investigators in this study did not adjust for SES or resuscitation status. Findings from our current study support and build upon these previous findings. Ours is among the first ICU studies to perform comprehensive adjustments for severity of illness, resuscitation preferences, SES, and insurance status. Further, no prior study has examined outcomes among Hispanics with a broad range of critical illnesses. In addition, although our cohort included only California hospitals, the hospitals are more diverse in size, ownership, and teaching status compared to the predominately academic and tertiary care hospitals included prior studies. In sum, the hospitals included in our study are more representative of community hospitals where most Americans receive care.
We found that black patients had longer unadjusted ICU LOS compared to white patients, but after adjusting for severity of illness, source of admission, DNR status, SES, and insurance status there was no statistically significant difference in ICU LOS. Severity of illness seemed to be a significant contributor to this increased ICU LOS. Two prior studies examined the effect of race and ethnicity on length of stay.4, 34 The 1995 study by Williams and colleagues found that black patients had 0.32 day shorter ICU LOS compared to white patients after adjusting for severity of illness (APACHE II) and insurance status.4 A more recent study of patients from Project IMPACT did not reveal differences in ICU LOS comparing black and white patients.34 Both of these studies utilized risk-adjustment methodologies that have since been updated, and did not adjust for end-of-life preferences, SES beyond insurance status, or account for within-hospital clustering.
That we found no difference in risk-adjusted mortality among racial/ethnic groups is an encouraging finding that is somewhat unexpected, especially when contrasted with other recent studies that have found racial/ethnic disparities in outcomes in specific critical illnesses.2, 35 By focusing on a specific disease process like acute lung injury within a more homogeneous ICU population, investigators have been able to elucidate greater detail about those diseases, including identifying racial and ethnic disparities in outcomes. In the case of acute lung injury and sepsis, there may be important processes of care, complications, or biological differences that may not be observed across a diverse set of medical and surgical conditions. Our objective was not to better define racial and ethnic differences in specific disease processes, but rather to determine whether there were racial or ethnic disparities in treatment or care among a population of general ICU patients.
There are several possible reasons why we did not find racial or ethnic differences in mortality among this cohort of ICU patients. First, the hospitals included in the CALICO project volunteered to participate because they were interested in receiving information about the quality of their ICU care. Therefore, these hospitals may have been more focused on providing high quality care to critically ill patients than non-participating hospitals. Prior studies illustrate that the quality of care provided in a hospital is associated with the racial/ethnic makeup of its patients. Hospitals that care for high proportions of black patients tend to provide lower quality care to all racial/ethnic groups.36 By only including hospitals that are more likely to provide high quality of care in our analysis we may have reduced our ability to detect disparities. This hypothesis is supported by a number of recent studies demonstrating that many of the differences in care or outcomes for black patients are explained by the quality of care provided by the hospitals with high proportions of black patients compared to hospitals with low proportions, rather than differential treatment by race inside a given hospital.37, 38 Second, because there is significant regional variation in the quality of hospital care provided in the U.S.,5 and our study was limited to hospitals in California, the variability in quality of care among these hospitals may have been too small to detect differences.
While our study included one of the largest and most diverse cohorts of ICU patients to date, our study may have been underpowered to detect small, but clinically important differences in mortality. The 95% confidence intervals include the possibility that there is up to 22% increased odds of death among black and Hispanic patients and a 57% increased odds of death among Asian/Pacific Islander patients. In addition, as with any administrative source of data, there is potential for misclassification of race/ethnicity. Most likely this misclassification is non-differential, which would bias results towards the null. The degree of misclassification in the California PDD has not been well characterized, although a prior study reported a high degree of accuracy when compared with death records.39
Conclusions
In contrast to other studies that have investigated health outcomes among different racial and ethnic groups, our study is encouraging in that we did not find any significant differences in mortality or ICU LOS between white and minority ICU patients. Despite this, it still appears that minority patients who are admitted to the ICU have more acute physiologic derangements. This could be due to delayed presentation to the ER, delay within the hospital or disparities in preventive and chronic care. Our results suggest that, among ICU patients, there may not be racial or ethnic differences in mortality within individual hospitals, but rather that disparities in treatment and care may be explained by the quality of care provided by specific hospitals. Future research should address the reasons for differences in health status immediately prior to ICU admission. A study that includes a broad spectrum of hospitals from every region of the U.S. will be necessary to adequately address the question of whether racial and ethnic disparities in mortality exist among ICU patients.
Acknowledgments
Financial Support: This work was supported by the California Office of Statewide Health Planning and Development and the Agency for Healthcare Research and Quality (R01 HS13919‐01). Dr. Dudley's work was also supported by an Investigator Award in Health Policy from the Robert Wood Johnson Foundation. Dr. Vasilevskis was supported by a Ruth L. Kirschstein National Research Service Award institutional research training grant T32, the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research Education and Clinical Center, Veterans Affairs, Tennessee Valley Healthcare, Nashville, Tennessee. Dr. Erickson was supported by the NIH (KL2 RR025009) – Atlanta Clinical and Translational Science Institute.
The funding sources had no role in the design and conduct of the study; collection, management, analysis, interpretation of the data or in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Drs. Erickson and Vasilevskis had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Contributor Information
Sara E. Erickson, Email: sara.e.erickson@kp.org.
Eduard E. Vasilevskis, Email: eduard.vasilevskis@vanderbilt.edu.
Michael W. Kuzniewicz, Email: kuzniewiczm@peds.ucsf.edu.
Brian A. Cason, Email: casonB@anesthesia.ucsf.edu.
Rondall K. Lane, Email: laner@anesthesia.ucsf.edu.
Mitzi L. Dean, Email: mitzi.dean@ucsf.edu.
Deborah J. Rennie, Email: drennie@earthlink.com.
R. Adams Dudley, Email: adams.dudley@ucsf.edu.
References
- 1.Smedley BD, SA, Nelson AR, et al. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, D.C.: Institute of Medicine; 2003. [PubMed] [Google Scholar]
- 2.Erickson SE, Shlipak MG, Martin GS, et al. Racial and ethnic disparities in mortality from acute lung injury. Crit Care Med. 2009;37:1–6. doi: 10.1097/CCM.0b013e31819292ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horner RD, Lawler FH, Hainer BL. Relationship between patient race and survival following admission to intensive care among patients of primary care physicians. Health Serv Res. 1991;26:531–42. [PMC free article] [PubMed] [Google Scholar]
- 4.Williams JF, Zimmerman JE, Wagner DP, Hawkins M, Knaus WA. African-American and white patients admitted to the intensive care unit: is there a difference in therapy and outcome? Crit Care Med. 1995;23:626–36. doi: 10.1097/00003246-199504000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Fisher E, GD, Skinner J, Bronner K. Health Care Spending, Quality and Outcomes: The Dartmouth Institute. 2009 [PubMed] [Google Scholar]
- 6.Hutchings A, Raine R, Brady A, Wildman M, Rowan K. Socioeconomic status and outcome from intensive care in England and Wales. Med Care. 2004;42:943–51. doi: 10.1097/00005650-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–8. [PubMed] [Google Scholar]
- 8.Degenholtz HB, Thomas SB, Miller MJ. Race and the intensive care unit: disparities and preferences for end-of-life care. Crit Care Med. 2003;31:S373–8. doi: 10.1097/01.CCM.0000065121.62144.0D. [DOI] [PubMed] [Google Scholar]
- 9.Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009;24:695–701. doi: 10.1007/s11606-009-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vasilevskis EE, Kuzniewicz MW, Cason BA, et al. Mortality probability model III and simplified acute physiology score II: assessing their value in predicting length of stay and comparison to APACHE IV. Chest. 2009;136:89–101. doi: 10.1378/chest.08-2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vasilevskis EE, Kuzniewicz MW, Dean ML, et al. Relationship between discharge practices and intensive care unit in-hospital mortality performance: evidence of a discharge bias. Med Care. 2009;47:803–12. doi: 10.1097/MLR.0b013e3181a39454. [DOI] [PubMed] [Google Scholar]
- 12.Kuzniewicz MW, Vasilevskis EE, Lane R, et al. Variation in ICU risk-adjusted mortality: impact of methods of assessment and potential confounders. Chest. 2008;133:1319–27. doi: 10.1378/chest.07-3061. [DOI] [PubMed] [Google Scholar]
- 13. [Accessed June 20, 2010];Medical Information Reporting for California. 2004 at www.oshpd.ca.gov/hid/mircal/Text_pdfs/Bulletins/QuickNotesV2.pdf.
- 14.Creation of New Race-Ethnicity Codes and Socioeconomic Status (SES) Indicators for Medicare Beneficiaries. Agency for Healthcare Research and Quality. 2008 Accessed at http://ftp.ahrq.gov/qual/medicareindicators/
- 15.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures--the public health disparities geocoding project. Am J Public Health. 2003;93:1655–71. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95:312–23. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57:186–99. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures--the public health disparities geocoding project (US) Public Health Rep. 2003;118:240–60. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today's critically ill patients. Crit Care Med. 2006;34:1297–310. doi: 10.1097/01.CCM.0000215112.84523.F0. [DOI] [PubMed] [Google Scholar]
- 20.Shepardson LB, Gordon HS, Ibrahim SA, Harper DL, Rosenthal GE. Racial variation in the use of do-not-resuscitate orders. J Gen Intern Med. 1999;14:15–20. doi: 10.1046/j.1525-1497.1999.00275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008;26:4131–7. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wenger NS, Pearson ML, Desmond KA, et al. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155:2056–62. [PubMed] [Google Scholar]
- 23.Higgins TL, Teres D, Copes WS, Nathanson BH, Stark M, Kramer AA. Assessing contemporary intensive care unit outcome: an updated Mortality Probability Admission Model (MPM0-III) Crit Care Med. 2007;35:827–35. doi: 10.1097/01.CCM.0000257337.63529.9F. [DOI] [PubMed] [Google Scholar]
- 24.Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169:493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yergan J, Flood AB, LoGerfo JP, Diehr P. Relationship between patient race and the intensity of hospital services. Med Care. 1987;25:592–603. doi: 10.1097/00005650-198707000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Barnato AE, Alexander SL, Linde-Zwirble WT, Angus DC. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177:279–84. doi: 10.1164/rccm.200703-480OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pines JM, Russell Localio A, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009;16:403–10. doi: 10.1111/j.1553-2712.2009.00381.x. [DOI] [PubMed] [Google Scholar]
- 28.Laiyemo AO, Doubeni C, Pinsky PF, et al. Race and colorectal cancer disparities: health-care utilization vs different cancer susceptibilities. J Natl Cancer Inst. 2010;102:538–46. doi: 10.1093/jnci/djq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu P, Bridges CB, Euler GL, Singleton JA. Influenza vaccination of recommended adult populations, U.S., 1989-2005. Vaccine. 2008;26:1786–93. doi: 10.1016/j.vaccine.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 30.Sequist TD, Fitzmaurice GM, Marshall R, Shaykevich S, Safran DG, Ayanian JZ. Physician performance and racial disparities in diabetes mellitus care. Arch Intern Med. 2008;168:1145–51. doi: 10.1001/archinte.168.11.1145. [DOI] [PubMed] [Google Scholar]
- 31.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347:1585–92. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 32.Kronman AC, Ash AS, Freund KM, Hanchate A, Emanuel EJ. Can primary care visits reduce hospital utilization among Medicare beneficiaries at the end of life? J Gen Intern Med. 2008;23:1330–5. doi: 10.1007/s11606-008-0638-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–84. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 34.Higgins TL, McGee WT, Steingrub JS, Rapoport J, Lemeshow S, Teres D. Early indicators of prolonged intensive care unit stay: impact of illness severity, physician staffing, and pre-intensive care unit length of stay. Crit Care Med. 2003;31:45–51. doi: 10.1097/00003246-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Mayr FB, Yende S, Linde-Zwirble WT, et al. Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. Jama. 2010;303:2495–503. doi: 10.1001/jama.2010.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167:1177–82. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 37.Bradley EH, Herrin J, Wang Y, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. Jama. 2004;292:1563–72. doi: 10.1001/jama.292.13.1563. [DOI] [PubMed] [Google Scholar]
- 38.Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361:22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Loggers ET, Maciejewski PK, Paulk E, et al. Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol. 2009;27:5559–64. doi: 10.1200/JCO.2009.22.4733. [DOI] [PMC free article] [PubMed] [Google Scholar]