Abstract
We examined the association between the therapeutic alliance and treatment outcomes among 223 women with posttraumatic stress disorder (PTSD) and substance use disorders who participated in a multisite clinical trial of group treatments for trauma and addictions in the United States throughout 2004 and 2005. General linear models indicated that women who received Seeking Safety, a cognitive-behavioral treatment, had significantly higher alliance ratings than those in Women's Health Education, a control group. Alliance was related to significant decreases in PTSD symptoms and higher attendance in both interventions. Alliance was not related to substance use outcomes. Implications and limitations of the findings are discussed.
Keywords: helping alliance, posttraumatic stress disorder, substance use disorders, retention, treatment outcomes
Introduction
The quality of the relationship between the therapist and the client is conceptualized as the therapeutic alliance. The therapeutic alliance is most often operationalized as a combination of client attachment to the therapist and client investment in the therapeutic process (Horvath & Luborsky, 1993). Two meta-analytic reviews indicate that there is a significant, positive relationship between the therapeutic alliance and psychotherapy outcomes, regardless of the type of treatment modality, alliance measure employed, or patient population assessed (Horvath & Symonds, 1991; Martin, Garske, & Davis, 2000). While the relationship between the therapeutic alliance and psychotherapy outcomes has been widely studied with general outpatient populations, there is less research on the role that alliance plays with individuals diagnosed with co-occurring posttraumatic stress disorder (PTSD) and substance use disorders (SUDs). Since the therapeutic relationship is often considered the primary vehicle through which successful trauma treatment outcomes occur (e.g., Herman, 1997), it may be important to assess the therapeutic alliance among individuals with trauma histories.
To date, research findings on the role of therapeutic alliance among substance users without diagnosed comorbidity have been mixed (Barber et al., 2001; Belding, Iguchi, Morral, & Mclellan, 1997; Carroll, Nich, & Rounsaville, 1997; Connors, Carroll, DiClemente, Longabaugh, & Donovan, 1997; Luborsky, McLellan, Woody, O'Brien, & Auerbach, 1985; Meier, Donmall, McElduff, Barrowclough, & Heller, 2006; Tunis, Delucchi, Schwartz, Banys, & Sees, 1995). For example, Carroll Nich, & Rounsaville (1997) found that patient ratings of the alliance were higher in cognitive behavioral therapy (CBT) compared to clinical management (CM) for cocaine dependence. However, alliance ratings were related to retention and cocaine use outcomes only for the CM condition and not for the CBT condition. De Weert-Van Oene, De Jong, Jorg, and Schrijvers (1999) and De Weert-Van Oene, Schippers, De Jong, and Schrijvers (2001) found that client ratings of the alliance were related to retention in both outpatient and inpatient substance user treatment.1 Connors et al. (1997) studied a large sample of primarily male outpatient clients manifesting alcohol dependence and found that alliance ratings were significant predictors of treatment participation and drinking behaviors during and after treatment. Barber et al. (2001) analyzed data from the National Institute on Drug Abuse (NIDA) Collaborative Cocaine Treatment Study (CCTS) and found that among cocaine-dependent outpatients receiving treatment, self-reported measures of the alliance were differentially associated with retention depending on the type of treatment received but were unrelated to drug use outcomes. In contrast, Belding et al. (1997) and Tunis et al. (1995) failed to find any relationship between alliance ratings and retention among opiate-dependent clients. Meier, Barrowclough, and Donmall (2005) conducted a comprehensive review of the research on alliance and drug user treatment outcomes over the past two decades and concluded that early alliance was a consistent predictor of engagement and retention in substance user treatment but an inconsistent predictor of posttreatment drug use outcomes. Nevertheless, they noted that early alliance ratings may influence clients' early treatment progress and the effect sizes of the alliance-outcome relationship in substance abusing2 samples were similar to those found in other psychotherapy studies (e.g., Horvath & Symonds, 1991; Martin et al., 2000).
Research on the alliance among trauma survivors suggest some of the long-term consequences of trauma exposure such as difficulties with emotion regulation and developing and maintaining interpersonal relationships may make it challenging to establish a therapeutic alliance (Briere, 1992; Herman, 1997; Price, Hilsenroth, Petretic-Jackson, & Bonge, 2001). Paivio and Patterson (1999) examined ratings of the alliance in a sample of 33 adult survivors of abuse (79% female) and found that early alliance was weaker for those with a history of more severe abuse. Cloitre, Stovall-McClough, Miranda, and Chemtob (2004) investigated the development of the therapeutic alliance in 34 women with a history of childhood abuse and PTSD, who received a two-phase CBT treatment, including prolonged exposure in Phase 2. The quality of the alliance during Phase 1 was a significant predictor of reductions in PTSD symptoms during Phase 2. This reduction was mediated by the women's ability to regulate negative mood states. These results underscore the potential importance of developing a positive alliance with a population often defined by difficult interpersonal relationships.
Further, individuals diagnosed with both PTSD and SUD often have more severe clinical profiles than those with either disorder alone (e.g., Brady, Back, & Coffey, 2004; Mills, Teesson, Ross, & Peters, 2006; Najavits, Weiss, & Shaw, 1999; Ouimette & Brown, 2003), making it potentially more difficult to develop and sustain a therapeutic alliance. The few studies of alliance in individuals with comorbid PTSD and SUDs are studies of Seeking Safety (SS; Najavits, 2002), an integrated cognitive-behavioral psychotherapy. Najavits, Weiss, Shaw, and Muenz (1998) assessed alliance in women manifesting comorbid PTSD and SUD and found that therapists and patients had highly correlated views. Therapists gave significantly higher alliance ratings early in treatment to women who ultimately stayed in treatment. Moreover, participants who completed treatment showed greater early treatment satisfaction compared with dropouts. Additional studies found that female prisoners and men in outpatient substance user treatment consistently reported high satisfaction with the SS treatment and tended to have strong ratings of the helping alliance throughout the course of treatment (Najavits, Schmitz, Gotthardt, & Weiss, 2005; Zlotnick, Najavits, & Rohsenow, 2003). Small sample sizes in these studies limit generalizability, and thus, further research is needed to examine the impact of alliance on outcome, particularly as it relates to trauma severity, and within interventions delivered in a group modality.
A recently completed multisite clinical trial on the effectiveness of treatments for trauma and addiction provides a unique opportunity to explore the role of the therapeutic alliance in relation to treatment improvements. The Women and Trauma Study (WTS; see Hien et al., 2009, for a full description of the study) was conducted in community-based treatment programs using the NIDA Clinical Trials Network (CTN) platform. The WTS compared 12 sessions of SS (from the 25 topics in the full treatment model; Hien, Cohen, Litt, Miele, & Capstick, 2004; Najavits, 2002; Najavits et al., 1998) with an attention control Women's Health Education (WHE) intervention, both delivered in a group format. The WTS used a randomized, controlled, repeated measures design to assess the effectiveness of adding a trauma-focused group intervention to standard outpatient substance user treatment to 353 drug-dependent women seeking treatment for a SUD(s) who met criteria for PTSD.
Findings revealed that both the SS and the WHE interventions were associated with large, clinically significant reductions in PTSD symptoms, with small differences consisting of interactive and trend effects favoring SS, particularly in participants with higher treatment attendance (Hien et al., 2009). Abstinence rates and drug/alcohol days of use were not significantly different between the two treatments. However, about 50% of the sample reported no substance use at baseline, which potentially limited the power to detect treatment effects on substance use outcomes. An additional analysis that further explored the relationship between PTSD and SUD reductions (Hien et al., 2010) revealed a differential impact on outcomes for those in SS who had heavy substance use at baseline. The probability of being classified as a heavy substance user at the 12-month follow-up was over twice as likely among those who received the control intervention than for those who received SS if the participants were heavy users before treatment. Heavy baseline substance users demonstrated reductions in PTSD scores on average by 52 points between baseline and 1 year posttreatment.
The specific aim of this secondary analysis was to examine the impact of the therapeutic alliance on treatment retention and outcomes among this sample of women with comorbid PTSD and SUD. We anticipated that a treatment model such as SS that specifically addresses trauma and emphasizes more interpersonal and interactive processes would be more conducive to the development of a therapeutic alliance. SS encourages counselors to engage clients' affect within a safe emotional range, promotes opportunities for clients to relate the material to specific problems they are currently facing, and emphasizes the need for the counselor to offer support and validation throughout sessions, all of which may promote greater connectedness in the therapeutic relationship. Based on the above research and theory, we hypothesized that (1) the therapeutic alliance will be higher in SS, a psychotherapy intervention group, than WHE, a psychoeducational control intervention; and (2) the therapeutic alliance will be a significant predictor of treatment attendance and posttreatment PTSD and substance use outcomes, above and beyond early symptom changes.
Methods
Study Overview
This randomized clinical trial was conducted at seven outpatient community-based substance user treatment programs in geographically diverse locations across the United States. All procedures were reviewed and approved by institutional review boards associated with the lead research team and at each treatment site, and all participants gave written informed consent. Because participating counselors and supervisors at each site were selected and randomly assigned to conduct one of the two treatment conditions, they were also considered research participants and gave written informed consent. A Certifcate of Confidentiality, issued by NIDA, was obtained for each clinic participating in the study (see Hien et al., 2009, for detailed study procedures).
Participants
Participants were women enrolled in outpatient treatment at each treatment program. Women were eligible to participate if they met the following inclusion criteria: (1) at least one traumatic event in their lifetime and current DSM-IV (American Psychiatric Association [APA], 1994), criteria for full or subthreshold PTSD (subthreshold PTSD was defined as meeting criteria A [exposure to a traumatic stressor], B [reexperiencing symptoms], E [symptom duration of at least 1 month], and F [significant distress or impairment of functioning], and either C [avoidance and numbing symptoms] or D [symptoms of increased arousal]); (2) 18–65 years of age; (3) used alcohol or an illicit substance within the 6 months prior to screening and met current diagnosis of drug or alcohol abuse or dependence; and (4) capable of providing informed consent. Participants were excluded if they had (1) impaired cognition as indicated by a Mini-Mental Status Examination (Folstein, Folstein, & McHugh, 1975) score of <21; (2) a significant risk of suicidal/homicidal intent or behavior (Psychiatric Research Interview for Substance and Mental Disorders [PRISM]; Hasin et al., 1996); (3) a history of schizophrenia-spectrum diagnosis or active (past 2 months) psychosis; (4) involvement in litigation related to PTSD; or (5) non-English speaking.
Procedures
This study assessed the effectiveness of 12 sessions of SS (from the 25 topics in the full treatment model; Najavits, 2002) compared with an attention control treatment (WHE; Miller, Pagan, & Tross, 1998), both delivered in a group format, plus standard substance user treatment. Recruitment occurred over a 21-month period in 2004–2005. After completing an eligibility screen and baseline assessment, participants were randomly assigned to one of the two treatment conditions consisting of two 75–90 minutes sessions per week over approximately 6 weeks. Treatment groups had a rolling admission format so that participants could enter treatment at any session. This was done to mirror standard treatment program group practices. Groups operated as long as there were three women randomized into a given intervention and at least two in attendance at a particular session. Participants were assessed weekly during treatment, and at 1 week, 3, 6, and 12 months posttreatment. All study participants were asked to attend standard treatment at their program during the 6-week treatment phase. Participants who left the treatment program prior to completing study treatment were removed from the intervention portion of the study but continued with follow-up assessments.
Interventions, Training, and Fidelity
SS treatment was abbreviated from 25 to 12 sessions to better fit within a feasible time frame for the treatment programs. SS is a structured cognitive-behavioral treatment with both safety/trauma and substance use components integrated into each session. All sessions followed the same structure: (1) check-in, including reports of “unsafe” behaviors and use of coping skills; (2) session quotation, a brief point of inspiration to affectively engage participants and link to the session topic; (3) topic discussion and structured skill practice, relating session material to the participants' lives; and (4) checkout, including a commitment to specific between-session skill practice.
WHE is a psychoeducational, manualized treatment focused on topics such as understanding the female body, human sexual behavior, pregnancy and childbirth, sexually transmitted diseases, and HIV/AIDS. WHE was designed to provide equivalent therapeutic attention, expectancy of benefit, and an issue-oriented focus, but without theory-driven techniques of SS, or any explicit content involving substance use or trauma. All sessions followed a common format: (1) introduction of topic; (2) review of group rules and between-session assignment; (3) topic presentation; (4) video, storytelling, and/or text readings; (5) topic exercises in a variety of formats to facilitate group discussion and application of session materials; and (6) between-session goal setting.
Counselors and supervisors from each site were selected based on (1) willingness to be randomized and (2) demonstrated ability to deliver a manualized, cognitive behavioral style of therapy based on an audiotaped relapse prevention session. Two counselors and two supervisors per site were randomized to deliver one of the two study interventions. Counselors and supervisors attended a comparable, centralized 3-day workshop on their respective interventions; supervisors received an additional half-day of training focused on how to carry out study supervision. Following training, counselors and supervisors were certified in the interventions after successfully completing a training group of at least four sessions. An expert from the lead training team rated the videotaped sessions for adherence to the manual and competency in intervention delivery.
During study implementation, all intervention sessions were videotaped and a proportion of tapes rated by supervisors. Counselors also met weekly with supervisors. In order to ensure competency on an ongoing basis, supervisors had weekly conference calls with lead node experts. The lead node experts corated a randomly selected quarter (29%) of the counselor session tapes reviewed by the supervisor to monitor ratings reliability on adherence measures. Internal consistency and interrater reliability for both interventions were good to excellent (see Hien et al., 2009, for a description of the adherence measures and findings).
Treatment as Usual
All study participants were enrolled in one of the participating community-based substance user treatment programs and were asked to attend treatment as usual at the program during the 6-week treatment phase of the study. Treatment as usual was not kept constant across sites in frequency and length of sessions per week, although most offered intensive outpatient services of 3 days per week or more. The treatment orientation of the programs also varied, but none of the programs provided trauma-focused treatment to participants during the study. During the study treatment and follow-up phases, treatment-as-usual data were collected and categorized as mental health, outpatient medical, inpatient substance user treatment, emergency room or hospitalization, and 12-step meeting attendance. Participants who dropped from the CTP prior to completing treatment were removed from the treatment portion of the study but continued with follow-up assessments.
Measures
Basic demographic data, including age and ethnicity/race, were collected at the screening visit; education was collected at baseline.
Addiction Severity Index-Lite (ASI-Lite; McLellan, Cacciola, & Zanis, 1997) is a standardized, multidimensional, semistructured, clinical interview that assesses current (past 30 days) alcohol and substance use. The ASI-Lite has been shown to have good reliability, validity, and convergence with the ASI, fifth edition (Cacciola, Alterman, McLellan, Lin, & Lynch, 2007). The ASI-Lite was administered at baseline and follow-up time points. The maximum number of days of use across any alcohol or illicit drug use (heroin, methadone, opiates, barbiturates, sedatives, cocaine/amphetamines, marijuana) was calculated and organized into four categories: 0 days, 1–11 days, 12–29 days, and 30 days.
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) is a structured interview that measures the frequency and intensity of symptoms of PTSD in the past 30 days and is used as a measure of DSM-IV (APA, 1994) PTSD diagnosis and treatment outcome. The CAPS was administered at baseline and follow-up time points. The CAPS has demonstrated excellent interrater and test–retest reliability and strong discriminant and convergent validity (Weathers, Keane, & Davidson, 2001). The scale has three symptom cluster subscales: reexperiencing, avoidance/numbing, and hyperarousal. The total severity score was used in the analysis and was calculated by summing all three symptom clusters' scores (range 0–136). The lead team conducted diagnostic reliability checks by listening to a subset (18%) of audiotaped scale assessments and held weekly conference calls with independent assessors to maintain competency and discuss challenging clinical issues. In the current study, based on 62 baseline interviews, percent agreement between two raters for current PTSD diagnosis was 94%.
PTSD Symptom Scale—Self-Report (PSS-SR; Foa, Riggs, Dancu, Constance, & Rothbaum, 1993) is a 17-item self-report measure that assesses the frequency and severity of PTSD symptoms and has demonstrated high test–retest reliability and good convergent validity (Foa et al., 1993). The PSS-SR was administered at baseline, weekly during treatment, and follow-up time points. Since the CAPS was not administered on a weekly basis, the PSS-SR was used as a measure of early improvement in PTSD symptoms (from baseline to Week 2) prior to the assessment of the alliance. Early improvement was defined as 30% or greater reduction in PTSD symptoms from baseline to Week 2.
The Revised Helping Alliance questionnaire II (HAq-II; Luborsky et al., 1996) is a well-validated measure of the counselor/patient alliance construct and excludes items that directly tap patient improvement. The HAq-II consists of 19 items rated on a 6-point Likert scale (1 = strongly feel it is not true, 6 = strongly feel it is true). Higher scores reflect more positive ratings of the alliance. Alliance can be rated by the counselor (HAq-II-C) or the client (HAq-II-P). The HAq-II-P was completed by participants at Week 2 (cronbach's alpha = 0.87) and at Week 6 (cronbach's alpha = 0.94) during the 6-week treatment phase. Only early alliance ratings (Week 2) were used in the analyses because (1) there were no significant differences between the early and late alliance measures, (2) there were more observations for the early measures due to subsequent participant dropout, and (3) studies show that patients' early alliance ratings (i.e., the third to the fifth sessions) are one of the strongest predictors of final treatment outcome (Horvath, 2001; Horvath & Symonds, 1991; Wampold, 2001).
Session attendance (0–12) was the absolute number of sessions attended by each participant.
Statistical Analyses
To test the effects of alliance ratings at Week 2 (HAq-II scores) on treatment outcomes (i.e., PTSD [CAPS scores] and substance use outcomes [ASI scores] during follow-up time points and retention as measured by the number of sessions attended), we used generalized linear models to fit each of the three outcomes as a function of treatment (SS vs. WHE), time of assessment, and participants' HAq-II scores. The identity link function was used for continuous variables (e.g., CAPS scores) and the cumulative logit link for categorical outcomes (e.g., categories of substance using days). The linear regression model on retention was estimated as a function of treatment and participants' HAq-II scores at Week 2. Early improvement in PTSD symptoms was controlled for in the model of the effects of alliance at Week 2 on PTSD during follow-ups. Race/ethnicity, age, education level, and site were included as main effects in the model (i.e., the same covariates used in the main outcome analyses; Hien et al., 2009). For each outcome, the corresponding baseline value (i.e., baseline PTSD severity and baseline substance use severity) and its possible interactions with time, treatment, and HAq-II scores were included in the model when applicable. A manual backward elimination procedure starting with the four-way interaction was used to determine a final model. The generalized estimating equations (GEE) approach (Diggle, Liang, & Zeger, 1994) was used to estimate and test the model. The GEE methodology can handle correlated data arising from repeated measurements, requires no parametric distribution assumption, provides robust inference with respect to misspecification of the within-subject correlation, and allows for the analysis of continuous, categorical, and count data, which may be missing for some observations due to an absence or treatment dropout. PROC GENMOD in SAS was used to carry out these analyses.
In order to examine the difference in treatment effect among clinical sites, site was tested as an additional fixed effect in the model. Counselor level was not included in the model, given that each intervention group was run continuously at each site by a single counselor (in the majority of cases); therefore, much of the effect of group is accounted for in the model by the inclusion of site and intervention.
Results
Participant and Counselor Demographics
Sample characteristics for clients who completed alliance ratings at Week 2 (N = 223) are displayed in Table 1. All participants were women with a mean age of 40 years (SD = 9.30). Approximately 44% were Caucasian, 33% were African Americans, 7.6% were Latina, and 15.7% were self-identified as “other”. Forty-six percent were divorced, 35% were single, 18% were married, and the average year of education was 12.64 (SD = 2.31). At baseline, the average CAPS total score among all participants was 62.09 (SD = 19.67), consistent with severe levels of PTSD symptoms (Weathers et al., 2001). The percentage of participants with current substance use (i.e., number of days used in the prior 30 days) was as follows: 0 days (40.81%), 1–11 days (30.94%), 12–29 days (17.49%), and 30 days (10.76%). The mean number of sessions attended for the total sample is 8.69 (SD = 2.84). There were no significant differences between participants in the SS groups and participants in the WHE groups in any of the sociodemographic variables. Moreover, there were no significant differences between participants who completed alliance ratings at Week 2 (N = 223) versus those who did not (N = 130).
Table 1. Participant characteristics.
| Mean (SD) or % | |||||
|---|---|---|---|---|---|
|
|
|||||
| Variables | Total | SS (N = 109) | WHE (N = 114) | t or χ2 | p |
| Age (years) | 40.04 (9.30) | 40.65 (9.52) | 39.46 (9.08) | 0.96 | .34 |
| Race/ethnicity | χ2(3) = 3.68 | .30 | |||
| African American | 33.18% | 29.36% | 36.84% | ||
| Caucasian | 43.5% | 46.79% | 40.35% | ||
| Latina | 7.62% | 5.50% | 9.65% | ||
| Other | 15.70% | 18.35% | 13.16% | ||
| Marital status | χ2(3) = 2.49 | .29 | |||
| Married | 18.39% | 15.60% | 21.05% | ||
| Single | 35.43% | 33.03% | 37.72% | ||
| Divorced/separated | 46.19% | 51.38% | 41.23% | ||
| Education (years) | 12.64 (2.31) | 12.78 (2.43) | 12.50 (2.20) | 0.90 | .37 |
| CAPS | 62.09 (19.67) | 61.17 (19.48) | 62.96 (19.90) | −0.68 | .50 |
| Substance use (past 30 days) | χ2(3) = 2.62 | .45 | |||
| Zero | 40.81% | 36.70% | 44.74% | ||
| 1–11 | 30.94% | 35.78% | 26.32% | ||
| 12–29 | 17.49% | 16.51% | 18.42% | ||
| 30 | 10.76% | 11.01% | 10.53% | ||
| Early improvement in PTSD symptoms | 30.28% | 25.47% | 34.82% | χ2(3) = 2.26 | .13 |
Fourteen counselors participated in the study. They were all females with a mean age of approximately 39 years (SD = 9.2). Half of the counselors were Caucasian (n = 7), 4 were African American, and 3 were Hispanic. Counselors had an average of nearly 5 years (SD = 2.7) of providing substance user treatment and worked at their current agency for 4 years (SD = 2.9). All but one counselor had at least a bachelor's degree, with more than half (57%) holding a master's degree. Twenty-nine percent of counselors identified as being in recovery.
Alliance Ratings
Table 2 shows the mean alliance ratings (HAq-II) at Week 2 (N = 223) and Week 6 (N = 171) for participants in the two treatment groups. Both groups of participants reported high levels of alliance, with average scores between 5.15 and 5.33 (out of 6). There was a significant difference between treatment conditions in alliance ratings at Week 2. SS participants reported significantly higher alliance than WHE participants (M = 5.33 vs. 5.15, respectively, t = 2.60, p = .01, d = 0.36). There was also a statistical trend at Week 6, where SS participants reported higher alliance than WHE participants (M = 5.35 vs. 5.15, respectively, t = 1.74; p = .08, d = 0.27). There were no significant differences between Week 2 and Week 6 alliance ratings within either treatment group (SS: t = 0.89; p = .38; WHE: t = 0.25, p = .80).
Table 2. Mean participant alliance ratings at Weeks 2 and 6 during the treatment phase.
| SS | WHE | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Alliance measure | n | M | SD | n | M | SD | p value |
| Week 2 HAq-II | 109 | 5.33 | 0.44 | 114 | 5.15 | 0.56 | .01 |
| Week 6 HAq-II | 88 | 5.35 | 0.68 | 83 | 5.15 | 0.80 | .08 |
Effect of Alliance on Posttreatment PTSD Symptoms
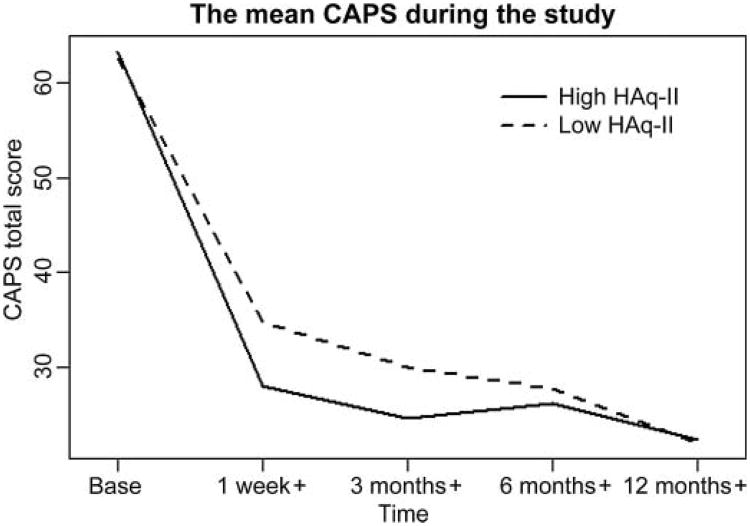
There was no main effect of treatment nor any interaction effect between treatment and alliance ratings at Week 2 on PTSD symptoms (X2 (1) = 1.46, p = .23), indicating the treatments did not differentially impact the effect of the alliance at Week 2 on PTSD symptoms. There was a significant interaction between alliance ratings at Week 2 and time on the participants' CAPS scores during follow-up (X2 (1) = 4.56, p < .05). As an illustrative point, Figure 1 shows the mean CAPS score for participants with high (≥5.15) and low (<5.15) alliance ratings at Week 2. Higher alliance ratings at Week 2 were associated with lower CAPS scores at 1 week posttreatment (X2 (1) = 11.65, p < .001). For every one unit of increase in alliance score, the CAPS scores decreased by 12 points. This effect weakened over the follow-up time period and was nonsignificant at 12-month follow-up (X2 (1) = 1.94, p = .16). Baseline CAPS scores were a significant predictor of CAPS scores at follow-up (X2 (1) = 33.95, p < .0001). In order to rule out the possibility that early improvement in PTSD symptoms (from baseline to Week 2) was responsible for the relationship between alliance at Week 2 and CAPS scores at follow-up, we included early improvement in PTSD, as measured by weekly PSS-SR scores, in the analytic model. Results revealed that early improvement in PSS-SR scores up to Week 2 (improvement was defined as a 30% or greater reduction in PSS-SR scores) was associated with significant reductions in CAPS scores during the follow-up time points (b = −6.43, SE = 2.55, X2 (1) = 6.05, p = .01). Moreover, the relationship between alliance ratings at Week 2 and PTSD symptoms at follow-up remained significant even after partialling out early improvement in PTSD symptoms (see Table 3), suggesting early alliance has an independent effect on PTSD symptom outcomes.
Figure 1.
Mean CAPS score at baseline, 1 week posttreatment, 3, 6, and 12 months posttreatment by HAq-II scores.
Table 3. Effect of alliance scores on posttreatment CAPS scores, substance use, and treatment retention.
| CAPS | Substance use | Retention | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| df | X2 | p | df | X2 | p | df | X2 | p | |
| SS (vs. WHE) | 1 | 1.46 | .2270 | 1 | 0.17 | .6821 | 1 | 0.63 | .4282 |
| Alliance scores (Week 2) | 1 | 11.65 | .0006 | 1 | 0.30 | .5851 | 1 | 3.82 | .05 |
| Time of assessment | 1 | 7.45 | .0064 | 3 | 15.71 | .0013 | |||
| Interaction between alliance and time | 1 | 4.56 | .0328 | ||||||
| Baseline CAPS | 1 | 33.95 | <.0001 | ||||||
| Early improvement in PTSD symptoms | 1 | 6.05 | .0139 | ||||||
| Baseline substance use | 1 | 12.17 | .0005 | ||||||
Note: Analyses were limited to participants with data on alliance ratings at Week 2 (N = 223). All models controlled for age, race, education, and site.
Effect of Alliance on Posttreatment Substance Use
The main effect of alliance ratings at Week 2 on posttreatment substance use outcomes was not significant (X2 (1) = 0.30, p = .59). Likewise, there were no significant two-way or three-way interactions between alliance ratings at Week 2, treatment, and time on substance use outcomes. There was, however, a significant main effect of time (X2 (1) = 15.71, p < .01), indicating that participants in both treatment groups increased the number of days they used substances over time, but this finding was independent of alliance. Baseline substance use was also a significant predictor of later substance use (X2 (1) = 12.17, p < .001).
Effect of Alliance on Treatment Retention
In both treatment conditions, there was a significant main effect of alliance at Week 2 on treatment retention, defined as the number of sessions attended (X2 (1) = 3.82, p = .05); the higher the alliance at Week 2, the more sessions the participant attended. There was no significant interaction effect between alliance at Week 2 and treatment type on participants' session attendance during treatment (X2 (1) = 0.19, p = .66).
We tested whether retention mediated the effect of alliance at Week 2 on CAPS scores using the Baron and Kenny (1986) approach. After adding the participants' retention as a main effect in the final model for CAPS (described earlier), the effect of number of sessions attended was not significant (b = −0.12, SE = 0.44, X2 (1) = 0.07, p = .79), and the effect of alliance at Week 2 on CAPS scores at follow-up remained the same (b = −11.59, SE = 2.84 at 1 week posttreatment in the model without retention, and b = −11.52, SE = 2.88 at 1 week posttreatment in the model with retention). This indicates that the number of sessions attended was not a mediator of the effect of alliance at Week 2 on CAPS outcomes.
Discussion
This study examined the association between the therapeutic alliance and treatment outcomes among women with PTSD and SUDs in outpatient treatment. Participants' ratings of the alliance were positive and high in both interventions. As expected, participants rated the alliance significantly higher in SS, a cognitive-behavioral intervention, than in WHE, a psychoeducational intervention, both at the beginning and at the end of treatment. Despite the potential for emotional dysregulation and mistrust that often interferes with trauma survivors' ability to establish strong therapeutic relationships, the women in this study were able to engage with their counselors during treatment and found the relationship helpful. We anticipated that a treatment model such as SS that specifically addresses trauma and emphasizes more interpersonal and interactive processes would be more conducive to the development of a therapeutic alliance. The fexibility and inspiring tone of the manual may have also promoted a strong therapeutic alliance. SS also encourages counselors to engage clients' affect within a safe emotional range, promotes opportunities for clients to relate the material to specific problems they are currently facing, and emphasizes the need for the counselor to offer support and validation throughout sessions, all of which may promote greater connectedness in the therapeutic relationship. Gaiton (2004) had a similar result using an observer-based measurement of alliance in a study comparing SS and relapse prevention therapy among a sample of dually diagnosed women with PTSD and substance use.
While the alliance for SS was statistically higher than WHE, both had averages above 5.0 (on a 6-point scale). Even within the structured format of the psychoeducational WHE groups, participants rated their alliance as strong. The development of a positive alliance in the WHE groups may be related to the psychoeducational nature of the groups. Studies indicate that, given the deficits in self-care that are often evident in individuals with SUDs, the provision of accurate and comprehensible information about specific health issues can lead to positive treatment outcomes (Cummings & Cummings, 2008; La Salvia, 1993). Thus, as participants received much needed health information, a strong alliance developed.
It is also notable that alliance was rated high despite some initial study counselor concerns that using manualized interventions would constrain them in developing an authentic relationship with participants. These concerns did not ultimately interfere with their ability to reliably and comfortably deliver the interventions and for participants to view the interventions and their counselors as helpful.
As hypothesized, early alliance was a significant predictor of retention and reduction in PTSD symptoms. These results are consistent with other studies that have demonstrated early alliance to be a predictor of outcome (see Horvath & Symonds, 1991), including diminished PTSD symptoms (Cloitre et al., 2004). Of interest in the present study is that alliance scores for women in both the treatment conditions predicted PTSD symptom reduction. Women who enrolled in the study may have been specifically motivated to address their trauma and PTSD symptoms, and this may have had an impact on alliance and symptom reduction, regardless of the specific intervention attended. Alliance has been shown to be positively related to clients' expectation of improvement (Constantino, Arnow, Blasey, & Agras, 2005). All of the women who enrolled in the study were aware that they were participating in a study for women with trauma histories, perhaps with the hope and expectation that they would experience some relief from their trauma symptoms. In addition, alliance has specifically been shown to play a mediating role in the relationship between expectations and group benefit, suggesting that the development of a strong bond and a collaborative relationship between the group members and the group leader is an important component of outcome (Abouguendia, Joyce, Piper, & Ogrodniczuk, 2004).
A strong early alliance also predicted treatment retention in both treatment conditions. Although we expected greater retention in the SS condition due to the stronger trauma-focused content of the treatment, women who formed an early alliance with their counselors stayed longer in WHE as well. This finding is consistent with research, showing that client's ratings of the alliance are predictive of retention during treatment (Barber et al., 2001; Carroll et al., 1997; De Weert-Van Oene, De Jong, et al., 1999; De Weert-Van Oene, Schippers, et al., 2001). The therapeutic alliance was not associated with substance use outcomes. This finding is in line with the primary outcome results from the parent study, showing that neither treatment was associated with substance use reductions over time. Other related studies have also reported no relationship between early alliance and substance use outcomes (Barber et al., 2001; Belding et al., 1997) or have reported therapeutic alliance impacting short-term substance use outcomes, but not long-term outcomes (Meier et al., 2005). This finding may also represent an artifact of the methodology in the main study in that substance use overall was low (e.g., nearly 50% of the sample had zero days of substance use in the prior 30 days), given the population was actively engaged in standard substance user treatment. This may have diminished the power to detect alliance effects on substance use outcomes.
Study's Limitations
There are several limitations to note in evaluating the relationship between the interventions and the therapeutic alliance. On the whole, the counselors participating in the study were also clinicians in the treatment programs where the participants received their ongoing treatment. A greater overlap between participants' relationships with their counselors in the research context and the treatment program would make it difficult to discern if the alliance could be attributed specifically to the study interventions or to more frequent interactions. Although study supervisors did not note this as a concern, data were not collected to examine the impact of a potential dual relationship. However, there is no reason to believe that the two treatments would differ on this, and the potential impact of this issue would most likely vary by chance. Further, group membership was not included in the statistical models. It is possible that since the treatments were delivered in rolling groups that changed membership from session to session, group process might exert its own effect upon outcomes. However, since each site ran a single ongoing group for each intervention and did so for a majority of the time using one dedicated therapist (for each intervention), the inclusion of site and intervention in the analysis handles much of the variance. Although innovative methods are currently being developed to examine relevant questions related to the complexities of group structure under rolling admission designs (e.g., Morgan-Lopez & Fals-Stewart, 2007), using these models was beyond the scope of this article.
In addition, only counselors who were proficient in delivering manualized therapy were selected for this study. It is likely that they represent a more experienced group of counselors who are better able to develop and maintain a therapeutic relationship (the mean level of experience in substance user treatment for this group of counselors was approximately 5 years). Although the counselors were selected based on their ability to competently deliver a manualized relapse prevention session, certain other counselor characteristics may have contributed to forming an alliance. Characteristics such as counselor age, experience, and job satisfaction have been shown to affect alliance (Meier et al., 2006). Data on participant characteristics that have been shown to affect alliance, such as treatment motivation and treatment expectation, were also not obtained.
Finally, it is not uncommon in substance use research and substance user treatment to have a high rate of treatment dropout and modest rates of retention. This study was no exception, with retention rates of 61.4% for SS and 63.3% for WHE at 1 week posttreatment. Alliance data were, thus, available only for the subset of women who might realistically be expected to have higher alliance (compared with those who dropped from treatment). Therefore, the results can only be generalized to those participants who remained in the treatment.
Conclusions
Alliance scores in this study were comparable with those from other large-scale studies, including the NIDA CCTS, a longer, more intensive study that included individual therapy. In this protocol, alliance was determined based solely on the experience of individual group members in relation to their group counselor. These data add further support to initial findings of high alliance among participants in SS group and individual treatment studies (Gaiton, 2004; Najavits et al., 1998; Zlotnick et al., 2003). In all, this study demonstrates that this typically challenging group of women can develop a strong therapeutic alliance within a relatively brief treatment episode in a group format, facilitating reductions in PTSD symptoms and leading to treatment retention.
Glossary
- Retention
In this study, retention was defined as the number of sessions attended
- Substance use disorder
Substance use disorder is defined as a diagnosis of either alcohol/drug abuse or dependence
- Therapeutic alliance
The therapeutic alliance refers to the collaborative relationship between the client and the therapist. The alliance includes the bond between the client and the therapist as well as the degree of agreement between the client and the therapist about the goals and tasks of therapy
Biographies
Lesia M. Ruglass, Ph.D., is an assistant professor of psychology at the City College of New York, The City University of New York, New York, New York, USA, and a research scientist in the Trauma and Addictions Project at City College. Dr. Ruglass received her bachelor's degree from New York University, her master's degree from Boston University, and her Ph.D. in clinical psychology from the New School for Social Research. Her research interests center on understanding the influence of race and ethnicity on the diagnosis and treatment of individuals with PTSD and addictions and understanding and reducing risk factors that contribute to the HIV/AIDS epidemic among African Americans. Dr. Ruglass has authored/coauthored several peer-reviewed articles and presented her work at national and international conferences. Dr. Ruglass also maintains a private practice based in Manhattan, NY.

Gloria M. Miele, Ph.D., is an instructor of clinical psychology in Department of Psychiatry at the College of Physicians and Surgeons, Columbia University. Since 1990, she has been involved in research, treatment, and training in the areas of substance use and comorbid mental disorders. She is the training director for the Greater New York Node of NIDA's Clinical Trials Network (CTN) and has been a regional trainer for the American Psychological Association's HIV Office for Psychology Education (HOPE) for nearly 10 years. Her most recent work involves the use of technology, specifically Web-based interventions and new media, in substance abuse research. Dr. Miele is primary or coauthor of dozens of articles on the evaluation and treatment of substance abuse, HIV, and co-occurring mental health problems. She is also coauthor of the book, Trauma services for women in substance abuse treatment: An integrated approach (Hien et al., 2008). Dr. Miele is also a business development and leadership coach, working with entrepreneurs and other business leaders to sharpen their skills and optimize their success in their personal and professional lives. She provides training and coaching in strengths-based leadership, effective communication, emotional intelligence, and other areas that increase business success. She lives and works in Southern California.

Denise A. Hien, Ph.D., is a professor of clinical psychology at The City College of New York and maintains an appointment as a senior research scientist in the Department of Psychiatry at the College of Physicians and Surgeons, Columbia University. She is the founding executive director of the Women's Health Project. Over the past 16 years with funding from the National Institute on Drug Abuse, Office of Research on Women's Health, and National Institute on Alcoholism and Alcohol Abuse, she and her team have conducted research that has helped to characterize the psychosocial and diagnostic correlates of interpersonal violence among innercity minority women and their families. She has also contributed to science on the treatment of trauma-related disorders with substance comorbidities, conducting single and multisite clinical trials across the United States in community-based substance abuse treatment settings. She has authored, coauthored, and presented extensively in scientific journals, and at national and international conferences. Dr. Hien is considered a leader in the feld of women's trauma and addiction treatment. She has been a member of NIDA's Asian Pacifc Islanders Scholars Workgroup since 1999, and she has sponsored and mentored numerous predoctoral and postdoctoral minority researchers in their long-term health disparities career development. She is coauthor of the book entitled Trauma services for women in substance abuse treatment: An integrated approach.

Dr. Aimee Campbell, Ph.D., M.S.S.W., received her doctorate in social work and is a research scientist in the Substance Abuse Division of the New York State Psychiatric Institute (NYSPI) and an assistant professor of clinical psychiatric social work in the Department of Psychiatry at the College of Physicians and Surgeons, Columbia University. Her expertise centers on behavioral interventions for substance use disorders and HIV prevention intervention research, with a specific interest in the study of dissemination and implementation strategies to increase the use and effectiveness of empirically supported treatments in community settings.

Mei-Chen Hu obtained her Ph.D. in social welfare from the University of Wisconsin-Madison (discipline: social work) and is associate research scientist in the Department of Psychiatry, Columbia University. Areas of interest include drug dependence, psychiatric disorder, and child development.

Nathilee A. Caldeira, Ph.D., in clinical psychology and is a psychologist at the School of Medicine, New York University, New York, NY. Areas of interest include trauma and addictions.

Dr. Huiping Jiang, Ph.D., received his bachelor's degree in mathematics in 1998 from Nankai University, China, and received his Ph.D. in statistics from Southern Methodist University in 2003. From September 2003 to May 2009, Dr. Jiang was employed by the Research Foundation for Mental Hygiene, Inc., as a research biostatistician at the Biostatistics Division of the New York State Psychiatric Institute (NYSPI). From May 2009 to now, Dr. Jiang works as a statistical consultant at the Substance Abuse division of the New York State Psychiatric Institute. Dr. Jiang's research is focused on conducting independent methodological research in statistical analysis of brain imaging data, estimation and diagnosis for longitudinal data, and time series data analysis. Dr. Jiang also collaborates with NYSPI researchers and undertakes the solution of nonstandard statistical problems related to the field of neuroscience and psychiatry.
Dr. Lisa Litt, Ph.D., is a clinical psychologist and is clinical director of the Women's Health Project Treatment and Research Center and the Men's Center for Healing and Recovery, the Trauma Focused Programs at the Addiction Institute of New York at St. Luke's Hospital. There Dr. Litt oversees the programs' clinical services and professional training. She is also an assistant clinical professor of medical psychology in Psychiatry at College of Physicians and Surgeons, Columbia University, and has served as an adjunct professor of psychology and education at Columbia University Teachers College. Dr. Litt has expertise working with individuals traumatized in childhood or adulthood and is trained in several methods developed specifically for the treatment of trauma. She has been director, trainer, and supervisor of numerous psychotherapy studies funded by the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism exploring effective treatments for Posttraumatic Stress Disorder and cooccurring substance use disorders for women. She has recently coauthored a book entitled Trauma Services for Women in Substance Abuse Treatment. Also, experienced using integrated models of treatment for mental health and substance use issues. Dr. Litt maintains her private practice in New York City.

Therese K. Killeen, Ph.D., A.P.R.N. BC, discipline is nursing and is an associate professor at the Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC. Areas of interest include addiction, comorbidity, PTSD, evidence-based practice, and motivational interviewing.
Mary Akiko Hatch-Maillette, Ph.D., clinical psychology, is a research scientist at the University of Washington Alcohol and Drug Abuse Institute; clinical instructor at the Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle, WA; and clinical psychologist in private practice. Areas of interest include treatment of addictions, PTSD, women's health, and depression.

Lisa M. Najavits, Ph.D., A.B.P.P., is professor of psychiatry at the School of Medicine, Boston University, Boston, MA; lecturer at the Harvard Medical School; clinical psychologist at VA Boston; and clinical associate at McLean Hospital. She is the author of Seeking Safety: A treatment manual for PTSD and substance abuse (2002) and A Woman's addiction workbook (2002), and over 140 professional publications. She is currently past-president of the American Psychological Association Division on Addictions. She has received various awards, including the 1997 Young Professional Award of the International Society for Traumatic Stress Studies; the 1998 Early Career Contribution Award of the Society for Psychotherapy Research; the 2004 Emerging Leadership Award of the American Psychological Association Committee on Women; and the 2009 Betty Ford Award of the Association for Medical Education and Research in Substance Abuse. She has received a variety of National Institutes of Health grants. She is a practicing therapist and psychotherapy supervisor.

Chanda Funcell Brown, Ph.D., L.M.S.W., obtained her Ph.D. in social work from the University of South Carolina, Charleston, SC, where biracial identity development was the research area; masters in social work from the State University of New York at Buffalo, NY, where clinical social work and addictions were the major areas; BA from the University of Pittsburgh at Bradford, PA, with human relations as major. Dr. Brown is currently the Director of the Charleston Center, Charleston County Department of Alcohol and Other Drug Abuse Services, Charleston, SC. Research interests include substance use disorders, co-occurring disorders, motivational incentives, biracial identity development, and racial socialization.

James A. Robinson, M.Ed., is the Director of Innovative Clinical Research Solutions and the Information Sciences Division at the Nathan S. Kline Institute for Psychiatric Research, Orangeburg, NY. He is also the Director of Clinical Research Informatics and Data Management at the New York University Langone Medical Center. Research interests are in developing innovative products and methodologies that will expedite the implementation and completion of clinical research studies.

Gregory S. Brigham, Ph.D., A.B.P.P., is a psychologist and chief research officer at Maryhaven, Inc., Columbus, OH, and research scientist at the Department of Psychiatry, University of Cincinnati, Cincinnati, OH. Area of interest includes treatment and prevention of chronic addiction disorders.

Edward V. Nunes, M.D., is professor of clinical psychiatry at the College of Physicians and Surgeons, Columbia University, New York, NY, and research psychiatrist at New York State Psychiatric Institute. Areas of interest include diagnosis and treatment of co-occurring psychiatric and substance use disorders.
Footnotes
All authors contributed to the design of the study. Ruglass, Miele, and Hien conceptualized and led the writing of the article. Ruglass, Miele, Hien, Hu, and Jiang participated in the statistical analysis and interpretation of the data. All remaining authors assisted with data collection, interpretation of the findings, and writing the article.
Declaration of Interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Treatment can be briefly and usefully defined as a unique, planned, goal-directed, temporally structured, multidimensional change process of necessary quality, appropriateness, and conditions (endogenous and exogenous), which is bounded (culture, place, time, etc.) and can be categorized into professional-based, tradition-based, mutual-help based (AA, NA, etc.), and self-help (“natural recovery”) models. There are no unique models or techniques used with substance users—of whatever types and heterogeneities—which are not also used with nonsubstance users. Whether or not a treatment technique is indicated or contraindicated, and its selection underpinnings (theory-based, empirically-based, “principle of faith-based, tradition-based, etc.), continues to be a generic and key treatment issue. In the West, with the relatively new ideology of “harm reduction” and the even newer Quality of Life (QOL) and well-being treatment-driven models, there are now a new set of goals in addition to those derived from/associated with the older tradition of abstinence-driven models. Each ideological model has its own criteria for success as well as failure. Treatment is implemented in a range of environments, ambulatory as well as within institutions, which can include controlled environments. Treatment includes a spectrum of clinician–caregiver–patient relationships representing various forms of decision-making traditions/models: (1) the hierarchical model in which the clinician-treatment agent makes the decision(s) and the recipient is compliant and relatively passive, (2) shared decision-making that facilitates the collaboration between clinician and patient(s) in which both are active, and (3) the “informed model” in which the patient makes the decision(s). Editor's note.
The journal's style utilizes the category substance abuse as a diagnostic category. Substances are used or misused; living organisms are and can be abused. Editor's note.
References
- Abouguendia M, Joyce AS, Piper WE, Ogrodniczuk JS. Alliance as a mediator of expectancy effects in short-term group psychotherapy. Group Dynamics: Theory, Research, and Practice. 2004;8:3–12. [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Barber JP, Luborsky L, Gallop R, Crits-Christoph P, Frank A, Weiss RD, et al. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Journal of Consulting and Clinical Psychology. 2001;69:119–124. doi: 10.1037//0022-006x.69.1.119. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Belding MA, Iguchi MY, Morral AR, Mclellan AT. Assessing the helping alliance and its impact in the treatment of opiate dependence. Drug and Alcohol Dependence. 1997;48:51–59. doi: 10.1016/s0376-8716(97)00103-8. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13(5):206–209. [Google Scholar]
- Briere J. Child abuse trauma: Theory and treatment of the lasting effects. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Cacciola JS, Alterman AI, McLellan AT, Lin YT, Lynch KG. Initial evidence for the reliability and validity of a “Lite” version of the Addiction Severity Index. Drug and Alcohol Dependence. 2007;87:297–302. doi: 10.1016/j.drugalcdep.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Rounsaville BJ. Contribution of the therapeutic alliance to outcome in active versus control psychotherapies. Journal of Consulting and Clinical Psychology. 1997;65:510–514. doi: 10.1037//0022-006x.65.3.510. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough KC, Miranda R, Chemtob CM. Therapeutic alliance, negative mood regulation, and treatment outcome in child abuse-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2004;72:411–416. doi: 10.1037/0022-006X.72.3.411. [DOI] [PubMed] [Google Scholar]
- Connors GJ, Carroll KM, DiClemente CC, Longabaugh R, Donovan DM. The therapeutic alliance and its relationship to alcoholism treatment participation and outcome. Journal of Consulting and Clinical Psychology. 1997;65:588–598. doi: 10.1037//0022-006x.65.4.588. [DOI] [PubMed] [Google Scholar]
- Constantino MJ, Arnow BA, Blasey C, Agras WS. The association between patient characteristics and the therapeutic alliance in cognitive-behavioral and interpersonal therapy for bulimia nervosa. Journal of Consulting and Clinical Psychology. 2005;73:203–211. doi: 10.1037/0022-006X.73.2.203. [DOI] [PubMed] [Google Scholar]
- Cummings NA, Cummings JL. Psychoeducation in conjunction with psychotherapy practice. In: O'Donohue W, Cummings NA, editors. Evidence-based adjunctive treatments. New York: Academic Press; 2008. pp. 41–60. [Google Scholar]
- De Weert-Van Oene GH, De Jong CA, Jorg F, Schrijvers GJ. The helping alliance questionnaire: Psychometric properties in patients with substance dependence. Substance Use and Misuse. 1999;34:1549–1569. doi: 10.3109/10826089909039414. [DOI] [PubMed] [Google Scholar]
- De Weert-Van Oene GH, Schippers GM, De Jong CA, Schrijvers GJ. Retention in substance dependence treatment: The relevance of in-treatment factors. Journal of Substance Abuse Treatment. 2001;20:253–264. doi: 10.1016/s0740-5472(01)00160-x. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Liang KY, Zeger SL. Analysis of longitudinal data. Oxford: Oxford University Press; 1994. [Google Scholar]
- Foa E, Riggs DS, Dancu CV, Constance V, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Folstein M, Folstein S, McHugh PR. A minimental state examination. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gaiton LR. Doctoral dissertation. Adelphi University; Garden City, NY: 2004. Investigation of therapeutic alliance in a treatment study with substance-abusing women with PTSD. Available from ProQuest Dissertations and Theses (Accession Order No. AAT 3147366) [Google Scholar]
- Hasin D, Trautman K, Miele G, Samet S, Smith M, Endi-cott J. Psychiatric Research Interview for Substance and Mental Disorders (PRISM): Reliability for substance abusers. American Journal of Psychiatry. 1996;153:1195–1201. doi: 10.1176/ajp.153.9.1195. [DOI] [PubMed] [Google Scholar]
- Herman JL. Trauma and recovery. New York: Basic Books; 1997. [Google Scholar]
- Hien DA, Cohen LR, Litt L, Miele GM, Capstick C. Promising empirically supported treatments for substance-using women with PTSD: A randomized clinical trial comparing Seeking-Safety with Relapse Prevention. American Journal of Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Hien DA, Jiang H, Campbell ANC, Hu M, Miele GM, Cohen LR, et al. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA's clinical trials network. American Journal of Psychiatry. 2010;167:95–101. doi: 10.1176/appi.ajp.2009.09091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell ANC, Cohen LR, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology. 2009;77:607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO. The alliance. Psychotherapy: Theory, Research, Practice, Training. 2001;38:365–372. [Google Scholar]
- Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. Journal of Consulting and Clinical Psychology. 1993;61:561–573. doi: 10.1037//0022-006x.61.4.561. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology. 1991;38:139–149. [Google Scholar]
- La Salvia T. Enhancing addiction treatment through psychoeducational groups. Journal of Substance Abuse Treatment. 1993;10(5):439–444. doi: 10.1016/0740-5472(93)90003-k. [DOI] [PubMed] [Google Scholar]
- Luborsky L, Barber JP, Siqueland L, Johnson S, Najavits LM, Frank A, et al. The revised helping alliance questionnaire (HAq-II) The Journal of Psychotherapy Practice and Research. 1996;5:260–271. [PMC free article] [PubMed] [Google Scholar]
- Luborsky L, McLellan AT, Woody GE, O'Brien CP, Auerbach A. Therapist success and its determinants. Archives of General Psychiatry. 1985;42:602–611. doi: 10.1001/archpsyc.1985.01790290084010. [DOI] [PubMed] [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68:438–450. [PubMed] [Google Scholar]
- McLellan AT, Cacciola JS, Zanis D. The Addiction Severity Index-“Lite” (ASI-“Lite”) Philadelphia, PA: Center for the Studies of Addiction, University of Pennsylvania/Philadelphia VA Medical Center; 1997. [Google Scholar]
- Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: A critical review of the literature. Addiction. 2005;100:304–316. doi: 10.1111/j.1360-0443.2004.00935.x. [DOI] [PubMed] [Google Scholar]
- Meier PS, Donmall MC, McElduff P, Barrowclough C, Heller RF. The role of the early therapeutic alliance in predicting drug treatment dropout. Drug and Alcohol Dependence. 2006;83:57–64. doi: 10.1016/j.drugalcdep.2005.10.010. [DOI] [PubMed] [Google Scholar]
- Miller S, Pagan D, Tross S. Women's health education. Unpublished manual; 1998. [Google Scholar]
- Mills KL, Teesson M, Ross J, Peters L. Trauma, PTSD, and substance use disorders: Findings from the Australian national survey of mental health and well-being. American Journal of Psychiatry. 2006;163(4):652–658. doi: 10.1176/ajp.2006.163.4.652. [DOI] [PubMed] [Google Scholar]
- Morgan-Lopez AA, Fals-Stewart W. Analytic methods for modeling longitudinal data from rolling therapy groups with membership turnover. Journal of Consulting and Clinical Psychology. 2007;75:580–593. doi: 10.1037/0022-006X.75.4.580. [DOI] [PubMed] [Google Scholar]
- Najavits LM. Seeking safety: A treatment manual for PTSD and substance abuse. New York: Guilford Press; 2002. [Google Scholar]
- Najavits LM, Schmitz M, Gotthardt S, Weiss RD. Seeking safety plus exposure therapy for dual diagnosis men. Journal of Psychoactive Drugs. 2005;27:425–435. doi: 10.1080/02791072.2005.10399816. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR. A clinical profile of women with PTSD and substance dependence. Psychology of Addictive Behaviors. 1999;13:98–104. [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR, Muenz LR. “Seeking Safety”: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. Journal of Traumatic Stress. 1998;11:437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Ouimette P, Brown PJ. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. Washington, DC: American Psychological Association; 2003. [Google Scholar]
- Paivio SC, Patterson LA. Alliance development in therapy for resolving child abuse issues. Psychotherapy. 1999;36:343–354. [Google Scholar]
- Price J, Hilsenroth M, Petretic-Jackson P, Bonge D. A review of individual psychotherapy outcomes for adult survivors of childhood sexual abuse. Clinical Psychology Review. 2001;21:1095–1121. doi: 10.1016/s0272-7358(00)00086-6. [DOI] [PubMed] [Google Scholar]
- Tunis SL, Delucchi KL, Schwartz K, Banys P, Sees KL. The relationship of counselor and peer alliance to drug use and HIV risk behaviors in a six-month methadone detoxification program. Addictive Behaviors. 1995;20:395–405. doi: 10.1016/0306-4603(94)00080-i. [DOI] [PubMed] [Google Scholar]
- Wampold B. The great psychotherapy debate: Models, methods, and findings. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Najavits LM, Rohsenow DJ. A cognitive-behavioral treatment for incarcerated women with substance use disorder and posttraumatic stress disorder: Findings from a pilot study. Journal of Substance Abuse Treatment. 2003;25:99–105. doi: 10.1016/s0740-5472(03)00106-5. [DOI] [PubMed] [Google Scholar]