Abstract
Background
Common mental disorders (CMD) have a major impact on both society and individual workers, so return to work (RTW) is an important issue. In The Netherlands, the occupational physician plays a central role in the guidance of sick-listed workers with respect to RTW. Evidence-based guidelines are available, but seem not to be effective in improving RTW in people with CMD. An intervention supporting the occupational physician in guidance of sick-listed workers combined with specific guidance regarding RTW is needed. A blended E-health module embedded in collaborative occupational health care is now available, and comprises a decision aid supporting the occupational physician and an E-health module, Return@Work, to support sick-listed workers in the RTW process. The cost-effectiveness of this intervention will be evaluated in this study and compared with that of care as usual.
Methods
This study is a two-armed cluster randomized controlled trial, with randomization done at the level of occupational physicians. Two hundred workers with CMD on sickness absence for 4–26 weeks will be included in the study. Workers whose occupational physician is allocated to the intervention group will receive the collaborative occupational health care intervention. Occupational physicians allocated to the care as usual group will give conventional sickness guidance. Follow-up assessments will be done at 3, 6, 9, and 12 months after baseline. The primary outcome is duration until RTW. The secondary outcome is severity of symptoms of CMD. An economic evaluation will be performed as part of this trial.
Conclusion
It is hypothesized that collaborative occupational health care intervention will be more (cost)-effective than care as usual. This intervention is innovative in its combination of a decision aid by email sent to the occupational physician and an E-health module aimed at RTW for the sick-listed worker.
Keywords: design protocol, randomized controlled trial, common mental disorders, sickness absence, return to work, blended E-health
Introduction
Suffering from a common mental disorder (CMD) affects many aspects of life, including work participation and functioning.1 In The Netherlands, mental health problems account for one third of all disability benefits.2 Mental health problems are also strongly associated with long-term sickness absence, ie, an estimated 10.5 extra absence days per year.3 Although long-term sickness absence constitutes only a small fraction of all absence episodes, it comprises more than a third of total days lost and up to 75% of all absence costs.4 Along with the substantial costs incurred by sickness absence, the worker’s quality of life is also affected by long-term sickness absence.4 A survey has shown that the ability to work is an important aspect of quality of life.5 Prolonged absence from work increases the risk of isolation and reduces meaningful activity, and workers may become anxious about return to work (RTW), doubting their competency and fearing the reactions of coworkers. Therefore, considering the implications for the worker’s quality of life and the massive costs incurred by sickness absence, improving the process of RTW for people with CMD is important.4,6 However, the studies reported to date have shown that although evidence-based guidelines do exist for occupational physicians,7 and the Gatekeeper Improvement Act was established in The Netherlands to make both employer and worker responsible for RTW, the guidelines are insufficiently followed8–14 and occupational physicians often lack the time and skills to deal with sick-listed workers with CMD.
For a number of years, the assumption was that recovery of function would follow automatically after recovery of symptoms, but a Cochrane review and more recent studies show that reduction of symptoms does not automatically lead to RTW.15–18 Moreover, during regular psychological treatment by a general practitioner or a mental health specialist, there is a need for more focus on work-related topics.19,20 To avoid long-term sickness absence, the Dutch guideline for psychologists states that RTW needs to be an important aspect of treatment.21 However, Oomens et al reported that the guideline was not used effectively and that RTW was often not addressed.22
Several studies have been performed recently to improve RTW of workers with CMD. A study of psychiatric consultations among Dutch occupational physicians, with a focus on work issues and RTW, found some improvement with respect to RTW.23 A more extended model of this intervention is collaborative care, that requires monitoring by a care manager.24–26 In the Dutch setting, a collaborative care model in the occupational health setting, in which one occupational physician provided treatment of major depressive disorder and another occupational physician provided regular monitoring of work absence, showed short-term improvement of depressive symptoms and a slight, but statistically insignificant, improvement in terms of RTW.27–29 These modest results may reflect implementation problems, indicating that better results could be expected if the intervention was better implemented.
Other studies have suggested that RTW interventions should be carried out close to the workplace.15,17 Workplace interventions can be considered to be a form of disability management for the individual worker that facilitates RTW by removing barriers to returning to the workforce.30 A review of the effectiveness of workplace interventions could not draw convincing conclusions for CMD due to a lack of studies. However, this review did conclude that it is important that all relevant stakeholders facilitate RTW.30
A recent review suggested that, in addition to intervening on severity of the disorder during guidance for sick-listed employees, it is important that personal factors like self-efficacy and intention to RTW despite having symptoms receive extra attention when designing interventions.1,31 A prospective study exploring factors related to self-efficacy in RTW showed that, along with health-related factors, the attitude regarding RTW with symptoms is also important.32 This suggests that, in order to achieve a more rapid and lasting RTW for workers with CMD, a focus on both symptoms and RTW, with a special focus on cognitions regarding RTW while having symptoms, is recommended. Therefore, a collaborative care model with the possibility of psychiatric consultation should be combined with a specific approach aimed at RTW.
In the current study, an intervention known as the “E-health module embedded in Collaborative Occupational Health Care” (ECO) is being evaluated. ECO is a blended E-health intervention aimed at RTW. ECO comprises a decision aid sent by email supporting the occupational physician and a separate E-health module for the sick-listed worker, both of which were developed for this study. The decision aid will support occupational physicians in the guidance of sick-listed workers with CMD and includes elements of collaborative care, such as continuous monitoring of progress and access to psychiatric consultation. The E-health module, known as “Return@Work”, for sick-listed workers gives information and homework, and focuses on the importance of work for people with CMD and their perceptions regarding RTW with symptoms.
This paper describes the design of a cluster randomized controlled trial in which the cost-effectiveness of the Return@Work intervention combined with collaborative care (ECO) is compared with that of care as usual in sick-listed workers with CMD. The study protocol was approved by the medical ethics committee at the Institutions for Mental Health, Utrecht, The Netherlands, in February, 2011.
Materials and methods
Objectives
The primary aim of this randomized controlled trial is to evaluate the effectiveness of ECO intervention versus care as usual in terms of time to RTW. Time to RTW is defined as the duration of sickness absence in calendar days, from the day of randomization until the first RTW in own or other work with equal earnings for at least 4 weeks without recurrence. The secondary aim is to evaluate the effectiveness of the ECO intervention in terms of response and remission of depressive symptoms. Third, the cost-effectiveness of the ECO intervention will be evaluated, and includes both direct and indirect costs.
Study design
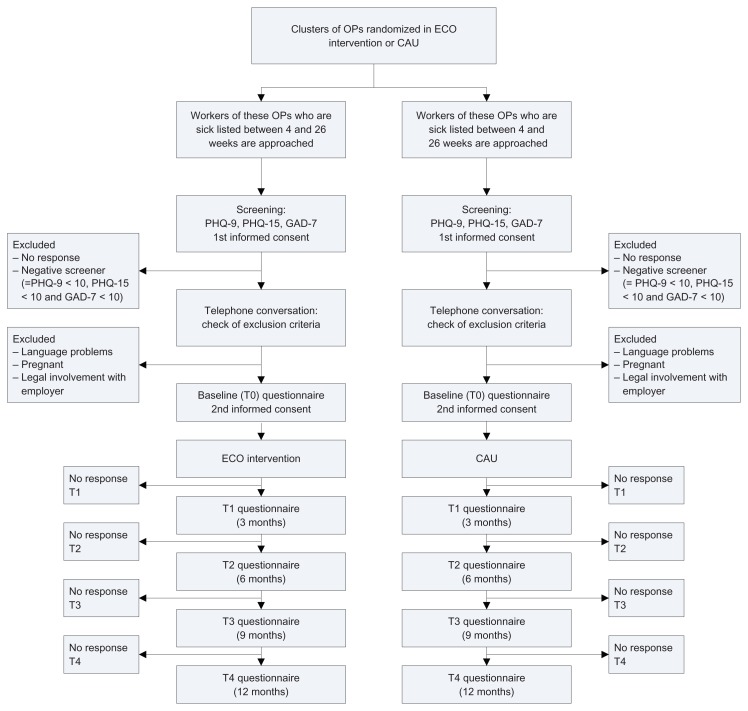
This study is a two-armed cluster randomized trial. Cluster randomization will occur at the level of occupational physicians in order to prevent contamination and dilution of the effect of intervention. Occupational physicians working in the same region will be clustered, because they would take over each other’s work in the event of a vacation or an emergency. Occupational physicians allocated to the intervention group will receive training in ECO, ie, the principles of the decision aid and in following up on the recommendations derived from the E-health module for workers, ie, Return@Work. Workers whose occupational physicians are allocated to the intervention group will receive the ECO intervention, ie, they will receive guidance from their occupational physician and will work through the E-health Return@Work module. Occupational physicians allocated to the care as usual group will not receive training or get the decision aid, nor will their workers get access to Return@Work. The intervention cannot be blinded because the occupational physicians and their patients would be aware of their group allocation. This is common in psychiatric intervention research and several approaches can be taken to diminish possible bias.50 Patient data will be obtained from self-reported questionnaires and registers held by the occupational health service and insurance company in order to exclude the possibility of interviewer bias. Figure 1 shows a flow chart for the participants.
Figure 1.
Flow chart of participants.
Abbreviations: OP, occupational physician; CAU, care as usual; PHQ-9, Depression scale of the Patient Health Questionnaire; PHQ-15, Somatization scale of the Patient Health Questionnaire; GAD-7, Generalized Anxiety Disorder scale.
Recruitment of occupational physicians
The occupational physicians will be recruited in collaboration with Arbo Vitale, a large occupational health service, and GGzBreburg a large mental health service employer, both in The Netherlands. Occupational physicians identified by Arbo Vitale and GGzBreburg and allocated to the intervention group will receive training in ECO before the workers are approached.
Recruitment of patients
The study will focus on workers with CMD who are on sickness absence for 4–26 weeks. A minimum of 4 weeks of sickness absence was chosen to avoid including patients with spontaneous recovery. The participants are to be recruited in collaboration with Arbo Vitale and GGzBreburg. Arbo Vitale is an occupational health service for employees in small-sized to medium-sized companies, whose employers are insured for the costs of sick leave and sickness guidance.
First, all workers sick-listed for 4–26 weeks will receive written information about the study from their occupational health service (Arbo Vitale) or employer (GGzBreburg), a letter from the occupational health service or employer, together with an information leaflet from the Trimbos Institute, an informed consent form, and a short screening instrument for depression, anxiety, and somatization. The depression and somatization subscales of the Patient Health Questionnaire (PHQ) will be used, ie, PHQ-9 for depression and PHQ-15 for somatization, and the Generalized Anxiety Disorder (GAD-7) scale for anxiety. These instruments have shown good psychometric properties for screening of depression, anxiety, and somatization.33–35 The workers are asked if they are willing to participate in a study investigating guidance for sick-listed workers with CMD. If they agree, they will be asked to sign the informed consent form and to return it to the researchers, together with the completed screener. In the information leaflet, it is emphasized that participation in the study is voluntary and that refusal to participate will not have consequences for their (future) guidance and sickness certification. Scores on the PHQ-9, GAD-7, and PHQ-15 will then be calculated for workers who return the screening questionnaires and give their informed consent. Workers will be considered screen-positive if they score ≥ 10 on one of the three questionnaires. These workers will be contacted by telephone.
The telephone conversations will be conducted by trained research assistants who are blinded to the randomization scheme. The research assistants will check for inclusion and exclusion criteria and give information about the study. Sick-listed workers who do not meet any of the exclusion criteria will receive the baseline questionnaire and a second informed consent form. Workers who complete the questionnaire and give their informed consent will be included in the study. Workers in the intervention group will be sent a login code for the Return@Work intervention.
Exclusion criteria
Workers with insufficient knowledge of the Dutch language and those who are pregnant will be excluded from the study. Workers involved in legal action against their employer, eg, because of a conflict at work, will also be excluded.
Training
Prior to starting the intervention, the occupational physicians allocated to the intervention group will receive training in ECO. The training will focus on sickness guidance for sick-listed workers with CMD, working with the decision aid, and contact with other stakeholders in the RTW process. As mentioned earlier, the guidelines for occupational physicians on guidance and treatment of sick-listed workers with CMD are insufficiently followed. The decision aid will help the occupational physicians to guide the worker according to the guideline and will give specific stepped-care treatment suggestions. During training, the occupational physicians will also be encouraged to contact other key stakeholders in the RTW process. In the event of stagnation, the occupational physician is required to contact other health care providers from whom the worker receives treatment, and discuss other treatment options according to the stepped-care advice outlined in the decision aid. Another important stakeholder is the employer, and the decision aid will advise occupational physicians to involve the employer in the RTW process and conduct a workplace intervention as defined by the STECR guideline if necessary.36 This training will be conducted by the researchers and a psychiatrist.
Guidance in intervention group
Return@Work aimed at RTW for sick-listed workers
The worker will receive an individual login code for the E-health RTW module, which is placed on a secure website. Through Return@Work, workers will receive information and homework assignments. They work through Return@Work individually, but workers are free to discuss topics or assignments with their occupational physicians. In that case, workers can print down specific pages in the module. The symptoms, functioning, and RTW of the worker are monitored in Return@Work on a regular basis. Workers can choose whether they want to have their monitor outcomes sent to the occupational physician. As in usual sickness guidance, the occupational physician and worker meet with each other face-to-face on a regular basis. The occupational physician cannot login to the worker’s E-health module, but can inquire about the worker’s progress in Return@Work and ask whether the worker needs support.
The content of Return@Work is tailored to the needs of workers. The content depends on the worker’s symptoms and perceptions about RTW. Return@Work begins with a baseline measurement, which includes questions about symptoms, functioning, and cognitions about RTW. The worker will receive the elements of Return@Work that best fit their symptoms. Return@Work includes the following elements:
Psychoeducation.
A module aimed at perceptions with regard to RTW while having symptoms, based on cognitive-behavioral principles.
A module containing problem-solving treatment exercises, aimed at clearly def ining problems and goals, learning and applying problem-solving skills, and developing more control in problem situations. The worker learns how to formulate practical ways of dealing with problems.37 In Return@Work, the problem-solving treatment focuses on the problems the worker encounters in the process of RTW.
A module for pain and fatigue management and for reactivation.
A module for relapse prevention, facilitating the worker in identifying a list of risk factors for situations increasing the likelihood of recurrence of loss of control, as stated by The Netherlands Society of Occupational Medicine guideline.7
Continuous monitoring of functioning (including RTW), symptoms, and defining personal goals. The workers will be monitored with the questionnaire that best fits their symptoms. This is the PHQ-9 for workers with predominantly depressive symptoms, GAD-7 for workers with anxiety symptoms, and PHQ-15 for workers with somatization. The Sickness Impact Profile will be used to monitor functioning in multiple aspects.38
Decision aid sent by email to occupational physician to guide sick-listed workers
The email messages include a decision aid and is based on principles of stepped collaborative care. The decision aid assists the occupational physician in guiding the sick-listed worker, monitoring of symptoms, functioning, and RTW. As noted earlier, the symptoms, functioning, and RTW of the worker will be regularly assessed in the Return@Work module. If the worker consents to their monitor outcomes being sent to the occupational physician, these are used in email messages for the occupational physician to give advice tailored to the individual worker. If the worker does not give permission to send monitor outcomes from Return@Work to the occupational physician, the email message gives more global information. In addition to specific stepped-care treatment suggestions that the decision aid gives in the email messages, it will also urge the occupational physician to involve the employer in the RTW process and to conduct a workplace intervention as defined by the STECR guideline if necessary.36 Further, the occupational physician will have access to a consultant psychiatrist who, when needed, gives advice in the event of stagnation.
Guidance in control group
The occupational physicians in the control group will not receive training in ECO, and will instead provide usual guidance to their sick-listed workers. Care as usual will be delivered according to the guidelines of the Dutch Board for Occupational Medicine.7
Data collection
The study data will be collected by The Netherlands Institute of Mental Health and Addiction. Patients will be sent questionnaires and asked to participate in the study and provide their written informed consent. Measurement will be done at baseline (T0), and at 3 (T1), 6 (T2), 9 (T3), and 12 months (T4) after entry to the study. The questionnaires should be completed on the Internet and will be processed automatically and anonymously. Data about RTW will also be derived from registers held by the occupational health service and the insurance company.
Primary outcome measure
The primary outcome measure is RTW, defined as the duration of work absence due to CMD in calendar days, from the day of randomization until the point of first partial RTW in own or equal work with equal earnings, for at least 4 weeks without relapse. Data will be derived from the sick leave databases of the occupational health service, the insurance company, and GGzBreburg. Missing or incomplete data will be derived from the second part of the Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness (TiC-P), ie, on the short form of the Health and Labor Questionnaire (SF-HLQ), with an added question asking explicitly about RTW.39,40 The full RTW will be analyzed separately in the secondary analysis. Presenteeism, as assessed by the TiC-P, will also be taken into account.
Secondary outcome measures
The secondary outcome measures are the severity of depressive, anxiety, and somatization symptoms, as measured with the PHQ-9, GAD-7, and PHQ-15,33–35 respectively. Response is defined as a 50% reduction in symptoms. Another secondary outcome measure is remission, defined as a score lower than 5.
Tertiary outcome measure
The tertiary outcome is the cost-effectiveness of ECO compared with care as usual. The economic evaluation will be performed from a societal perspective, including direct and indirect costs. A cost minimization analysis will be used to identify differences in costs of ECO versus care as usual by quantification of productivity losses. The Trimbos/iMTA questionnaire for TiC-P is used for calculating costs.40 The TiC-P consists of two parts. The first part collects data on medical consumption. The second part of the TiC-P, the SF-HLQ, is used for collecting data on productivity costs due to absence from work and reduced efficiency.39
Health care costs
Health care costs for the participants will be collected over a 12-month period, starting from the date of inclusion. Because mental health problems may affect both physical and mental functioning, all health care-related costs will be collected during follow-up. Calculating the total direct medical costs, the total number of medical contacts (eg, outpatient visits, hospital length of stay, use of medication) will be multiplied by the unit costs of the corresponding health care services. Reference unit prices of health care services will be applied and adjusted to the year of this study using the consumer price index.
Productivity costs
The cumulative number of sickness absence days during a one-year follow-up will be used. Costs associated with productivity loss will be calculated by the friction cost method and human capital approach. Using the friction cost method, productivity losses are limited to the time needed to restore production back to its initial level. This means that the friction cost method is the estimated time it takes a company to find a replacement for the sick worker. Productivity loss costs using the friction cost method will be estimated by multiplying the average daily wage by the gross number of sickness absence days up to a standard friction cost period. Productivity loss costs using the human capital approach will be estimated by multiplying the average daily wage by the total gross number of sickness absence days, using the entire period of sickness absence.
Additional outcome measures
The worker’s self-efficacy with regard to RTW and barriers to and facilitators of RTW will be measured using 14 questions on a 5-point Likert scale.41 Quality of life will be measured using the EuroQol42 and the Short-Form-36,43 both of which are validated instruments for measuring general health-related quality of life. Six scales of the Sickness Impact Profile will be used to measure functioning in life areas such as social interactions, and work and leisure time.38 Patient satisfaction with the occupational physician will be assessed using the Patient Satisfaction with Occupational Health Questionnaire.44 Physical symptoms are measured by the Physical Symptom Questionnaire.45 Further, the Whitely index will be used to measure attitude towards illness.46
Age, gender, nationality, marital status, living situation, and education will be measured at baseline. Comorbid chronic medical illness will be measured using a 28-item questionnaire developed by the Dutch Central Department of Statistics. Job characteristics will be measured by the Job Content Questionnaire at baseline.47 Neuroticism will be measured at baseline using the neuroticism scale of the NEO Five-Factor Inventory.48
Power calculations
A power calculation was performed on the primary outcome measure of time to RTW. In order to calculate the sample size, a hazard ratio of 1.6 was assumed as the smallest clinically and societally relevant ratio. A hazard ratio of 1.6 indicates that workers in the intervention group return to work about 1.5 times more quickly than workers in the care as usual group. This hazard ratio is based on recent studies of RTW and on preliminary results from a pilot randomized controlled trial in a population of workers on sick leave because of CMD, in which workers returned to work at 122 days, being 68 days earlier after receiving an intervention with collaborative care than after care as usual.23 Based on the assumed hazard ratio of 1.6, the calculation showed that a sample size of 160 completers would be needed. Because multilevel analysis will be performed, this number will be multiplied by a factor of 1.25 to account for possible intraclass correlation. Therefore, 200 completers will be needed.49 Noncompleters are not expected in the primary outcome, because data for time to RTW will be derived from the sick leave databases of the occupational health service, the insurance company, and GGzBreburg.
The duration of the study will be 4 years, with a preparation phase of one year. The inclusion phase will last 1.5 years. Follow-up points will be at 3, 6, 9, and 12 months after inclusion, which takes one year. Data analyses will take 6 months. This study was initiated in 2010 and the results are expected in 2014.
Statistical analysis
All analysis will be conducted according to the intention-to-treat principle. Multilevel analysis will be performed using clusters of occupational physicians at the first hierarchical level and individual participants at the second level. The Cox proportional hazards model will be used to derive the hazard ratio for RTW rates. Evaluation of the effectiveness of intervention will be performed with two-tailed tests at a significance level of 5%. The analyses will be controlled for duration of sickness absence at baseline. If differences in RTW are indeed found between the two experimental conditions, the cost differences due to productivity loss because of differences in RTW will be reported in a cost minimization analysis. Further, the 95% confidence intervals for the differences in mean costs in both groups will be computed by bias correction and accelerated bootstrapping with 2000 replications. In the event of missing data on costs, and any additional uncertainty introduced, we will use multiple imputation. Further, we will investigate if there are any differences in the effects of intervention for workers included by the occupational health service (Arbo Vitale) or their employer (GGZBreburg).
Discussion
The basis for this study is the large burden of CMD on the level of sickness absence for society as well as for individual workers, and the substantial costs involved. The aim of the study is to achieve an earlier and durable RTW and to reduce the symptoms of CMD.
Comparison with other studies
The ECO is aimed at RTW and comprises a decision aid communicated via email to support the occupational physician and a separate E-health module for the sick-listed worker, both were developed for this study. The decision aid will support occupational physicians when guiding sick-listed workers with CMD, and will include elements based on collaborative care, such as ongoing monitoring of progress and access to psychiatric consultation. A collaborative care model for major depressive disorder in the occupational health setting was recently investigated and showed limited results in terms of RTW, probably as a result of implementation problems.27–29 The authors stated that there would be a need to operationalize collaborative care differently in the occupational health care setting in future studies. The dual focus on RTW and depressive symptoms remains important, but it is not advisable to combine both strategies in one intervention delivered by one occupational physician.27–29 In the present study, the role of the occupational physician is to refer and monitor the efficacy of treatment and to improve collaboration between occupational physicians and the curative health sector.
The E-health module, Return@Work, provides information and homework for sick-listed workers, and focuses on the importance of work for people with CMD and their perceptions regarding RTW while still having symptoms. This is in line with the conclusions of several studies, ie, in addition to intervening on the severity of the disorder when guiding sick-listed employees, it is important that personal factors, such as self-efficacy and intention to RTW despite having symptoms, receive attention.1,31
Several studies have shown that it is important to increase the focus on graded activity and workplace interventions aimed at RTW. Return@Work focuses on RTW and on motivating the worker.15,16 The decision aid advises the occupational physician to involve the employer in the RTW process and to conduct a workplace intervention if necessary.
Strengths and limitations
This study is innovative in its combination of a decision aid by email for the occupational physician with the possibility of consulting a psychiatrist and an E-health module aimed at RTW for the sick-listed worker. Effective elements of other studies have been brought together in this study. Therefore, it is anticipated that ECO will reduce symptoms and sick leave, and decrease the associated costs.
A potential limitation of this study is that the study design does not allow inferences to be made about the effectiveness of the different components of ECO (a decision aid sent by email to the occupational physician or the e-health module Return@Work for the sick-listed worker), but only about the (cost)-effectiveness of the whole intervention. Further, at the screening stage, workers will be asked if they are willing to participate in the study, which may introduce a self-selection bias in the sense that those who are better motivated may be more likely to participate. However, if ECO proves to be effective and is implemented, employees will also be asked if they want to participate, because their engagement will be needed. In this way, the outcomes of the study will reflect daily practice, which will make the results of this study more generalizable to daily practice. A strength of the study design is that the intervention has a strong focus on RTW in addition to symptoms and involves the sick-listed worker as well as the occupational physician in the intervention. If the intervention proves to be (cost-)effective in the guidance of sick-listed workers with CMD, wider implementation would be considered, given the impact of CMD and long-term sickness absence on the individual worker and society.
Acknowledgments
This study is funded by The Netherlands Organization for Health Research and Development (ZonMw) and by Achmea, a Dutch insurance company.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Lagerveld SE, Bultmann U, Franche RL, et al. Factors associated with work participation and work functioning in depressed workers: a systematic review. J Occup Rehabil. 2010;20:275–292. doi: 10.1007/s10926-009-9224-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kenniscentrum UWV. UWV Kennisverslag. Amsterdam: UWV; 2012. [Google Scholar]
- 3.de Graaf R, Tuithof M, Dorsselaer van S, Have ten M. Sick Leave due to Psychological and Physical Illnesses among Employees. Utrecht, The Netherlands: Trimbos Instituut; 2011. Dutch. [Google Scholar]
- 4.Henderson M, Glozier N, Holland EK. Long term sickness absence. BMJ. 2005;330:802–803. doi: 10.1136/bmj.330.7495.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowling A. What things are important in people’s lives? A survey of the public’s judgements to inform scales of health related quality of life. Soc Sci Med. 1995;41:1447–1462. doi: 10.1016/0277-9536(95)00113-l. [DOI] [PubMed] [Google Scholar]
- 6.Bilsker D, Wiseman S, Gilbert M. Managing depression-related occupational disability: a pragmatic approach. Can J Psychiatry. 2006;51:76–83. doi: 10.1177/070674370605100203. [DOI] [PubMed] [Google Scholar]
- 7.Nederlandse Vereniging voor Arbeids-en Bedrijfsgeneeskunde (NVAB) Richtlijn voor bedrijfsartsen. Eindhoven, The Netherlands: Center of Excellence of the Netherlands Society of Occupational Medicine; 2000. Handelen van de bedrijfsarts bij werknemers met psychische klachten. Dutch. [Google Scholar]
- 8.Bodenheimer T. Helping patients improve their health-related behaviors: what system changes do we need? Dis Manag. 2005;8:319–330. doi: 10.1089/dis.2005.8.319. [DOI] [PubMed] [Google Scholar]
- 9.Ormel J, Bartel M, Nolen WA. Undertreatment of depression; causes and recommendations. Ned Tijdschr Geneeskd. 2003;147:1005–1009. Dutch. [PubMed] [Google Scholar]
- 10.Rebergen DS, Bruinvels DJ, Bos CM, van der Beek AJ, van MW. Return to work and occupational physicians’ management of common mental health problems – process evaluation of a randomized controlled trial. Scand J Work Environ Health. 2010;36:488–498. doi: 10.5271/sjweh.3084. [DOI] [PubMed] [Google Scholar]
- 11.Landelijke Stuurgroep Multidisciplinaire Richtlijnontwikkeling in de GGZ. [Multidisciplinary guideline for anxiety disorders [second revision]]. 2010. Dutch. [Google Scholar]
- 12.Landelijke Stuurgroep Multidisciplinaire Richtlijnontwikkeling in de GGZ. [Multidisciplinary guideline for medically unexplained physical symptoms and somatoform disorder]. 2011. Dutch. [Google Scholar]
- 13.Landelijke Stuurgroep Multidisciplinaire Richtlijnontwikkeling in de GGZ. [Multidisciplary guideline for depression [second revision]]. 2010. Dutch. [Google Scholar]
- 14.van der Feltz CM, Hoedeman R, Keuter EJ, Swinkels JA. Presentation of the multidisciplinary guideline medically unexplained physical symptoms (MUPS) and somatoform disorder in The Netherlands: disease management according to risk profiles. J Psychosom Res. 2012;72:168–169. doi: 10.1016/j.jpsychores.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Nieuwenhuijsen K, Bültmann U, Neumeyer-Gromen A, Verhoeven AC, Verbeek JH, Van der Feltz-Cornelis CM. Interventions to improve occupational health in depressed people. Cochrane Database Syst Rev. 2008;2:CD006237. doi: 10.1002/14651858.CD006237.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Blonk RW, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: a comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work and Stress. 2006;20:129–144. [Google Scholar]
- 17.Adler DA, McLaughlin TJ, Rogers WH, Chang H, Lapitsky L, Lerner D. Job performance deficits due to depression. Am J Psychiatry. 2006;163:1569–1576. doi: 10.1176/appi.ajp.163.9.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med. 2003;60:429–437. doi: 10.1136/oem.60.6.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buijs P, Anema JR, Evers M, van Dijk F, van der Klink J. How general practitioners can manage work-related psychological complaints. Design and pilot of a guideline: a contribution towards solving a huge problem. Eur J Gen Pract. 2006;12:38–41. doi: 10.1080/13814780600881201. [DOI] [PubMed] [Google Scholar]
- 20.Buijs PC, van Dijk FJH, Evers M, van der Klink JJL, Anema H. Managing work-related psychological complaints by general practitioners, in coordination with occupational physicians: a pilot study. Ind Health. 2007;45:37–43. doi: 10.2486/indhealth.45.37. [DOI] [PubMed] [Google Scholar]
- 21.Nederlands Instituut van Psychologen, Landelijke Vereniging van Eerstelijnspsychologen. [Work and Psychological Symptoms. Guideline for Psychologists]. Amsterdam, The Netherlands: NIP/LVE; 2005. Dutch. [Google Scholar]
- 22.Oomens PCJ, Huijs JJHM, Blonk RWB. Effectiveness of the Guideline ‘Work and Psychological Symptoms’ for Psychologists. Hoofddorp, The Netherlands: TNO; 2010. Dutch. [Google Scholar]
- 23.van der Feltz CM, Hoedeman R, de Jong FJ, et al. Faster return to work after psychiatric consultation for sick-listed employees with common mental disorders compared to care as usual. A randomized clinical trial. Neuropsychiatr Dis Treat. 2010;6:375–385. doi: 10.2147/ndt.s11832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 25.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 26.Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- 27.Vlasveld M, Anema JR, Beekman ATF, et al. Multidisciplinary collaborative care for depressive disorder in the occupational health setting: design of a randomised controlled trial and cost-effectiveness study. BMC Health Serv Res. 2008;8:99. doi: 10.1186/1472-6963-8-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vlasveld MC, Van der Feltz-Cornelis CM, Adèr HJ, et al. Collaborative care for major depressive disorder in an occupational healthcare setting. Br J Psychiatry. 2011;200:510–511. doi: 10.1192/bjp.bp.111.095687. [DOI] [PubMed] [Google Scholar]
- 29.Vlasveld MC, Van der Feltz-Cornelis CM, Adèr HJ, et al. Collaborative care for sick-listed workers with major depressive disorder: a randomised controlled trial from The Netherlands Depression Initiative aimed at return to work and depressive symptoms. Occup Environ Med. 2012 Oct 30; doi: 10.1136/oemed-2012-100793. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 30.van Oostrom SH, Driessen MT, de Vet HCW, et al. Workplace interventions for preventing work disability. Cochrane Database Syst Rev. 2009;2:CD006955. doi: 10.1002/14651858.CD006955.pub2. [DOI] [PubMed] [Google Scholar]
- 31.van Oostrom SH, van MW, Terluin B, de Vet HC, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. Occup Environ Med. 2010;67:596–602. doi: 10.1136/oem.2009.050849. [DOI] [PubMed] [Google Scholar]
- 32.Volker D, Vlasveld MC, Brouwers EPM, van Lomwel AGC, van der Feltz-Cornelis CM. Predicting return to work self-efficacy in sicklisted employees with different health conditions. 2012 Submitted. [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 36.STECR Werkwijzer Werkaanpassing. 2006. STECR Platform Reïntegratie. Dutch. [Google Scholar]
- 37.Mynors-Wallis L. Problem-solving treatment in general psychiatric practice. Adv Psych Treatment. 2001;7:417–425. [Google Scholar]
- 38.Jacobs HM, Luttik A, Touw-Otten F, De Melker RA. The Sickness Impact profile: results of an evaluation study of the Dutch version. Ned Tijdschr Geneeskd. 1990;134:1950–1954. Dutch. [PubMed] [Google Scholar]
- 39.van Roijen L, Essink-Bot ML, Koopmanschap MA, et al. Labor and health status in economic evaluation of health care. The Health and Labor Questionnaire. Int J Technol Assess Health Care. 1996;12:405–415. doi: 10.1017/s0266462300009764. [DOI] [PubMed] [Google Scholar]
- 40.Hakkaart-van Roijen L. Manual Trimbos/iMTA Questionnaire for Costs Associated with Psychiatric Illness. Rotterdam, The Netherlands: Institute for Medical Technology Assessment; 2002. Dutch. [Google Scholar]
- 41.van Oostrom SH, Anema JR, Terluin B, de Vet HC, Knol DL, van MW. Cost-effectiveness of a workplace intervention for sick-listed employees with common mental disorders: design of a randomized controlled trial. BMC Public Health. 2008;8:12. doi: 10.1186/1471-2458-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Euroqol Group. Eq-5D User Guide. Rotterdam, The Netherlands: Sanders Instituut, EUR; 1995. [Google Scholar]
- 43.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36) Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 44.Verbeek JH, de Boer AG, van der Weide WE, et al. Patient satisfaction with occupational health physicians, development of a questionnaire. Occup Environ Med. 2005;62:119–123. doi: 10.1136/oem.2004.016303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hemert AM. Lichamelijke Klachten Vragenlijst. Leiden, The Netherlands: Leids Universitair Medisch Centrum; 2003. Dutch. [Google Scholar]
- 46.Speckens AE, Spinhoven P, Sloekers PP, Bolk JH, Hemert AMv. A validation study of the Whitely Index, the Illness Attitude Scales and the Somatosensory Amplification Scale in general medical and general practice patients. J Psychosom Res. 1995;40:95–104. doi: 10.1016/0022-3999(95)00561-7. [DOI] [PubMed] [Google Scholar]
- 47.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 48.Costa PT, Jr, McCrae RR. Domains and facets: hierarchical personality assessment using the revised NEO personality inventory. J Pers Assess. 1995;64:21–50. doi: 10.1207/s15327752jpa6401_2. [DOI] [PubMed] [Google Scholar]
- 49.Tosteson TD, Buzas JS, Demindenko E, Karagas M. Power and sample size calculations for generalized regression models with covariate measurement error. Stat Med. 2003;22:1069–1082. doi: 10.1002/sim.1388. [DOI] [PubMed] [Google Scholar]
- 50.Van der Feltz-Cornelis CM, Adèr HJ. Randomization in psychiatric intervention research in the general practice setting. Int J Methods Psychiatr Res. 2000;9(3):136–144. [Google Scholar]