Abstract
Background
Recruiting and retaining participants for clinical trials, particularly women and ethnic minorities, is challenging. Studies are lacking, however, in which investigators examine gender and ethnic differences in research processes. Such information is important for findings to adequately represent the available population.
Objective
The study aim was to examine study recruitment processes (referral, eligibility, consent/enrollment) and study retention (completion) for gender and ethnic differences.
Methods
A descriptive comparative analysis of data from two randomized clinical trials focused on cancer outpatients with pain and/or fatigue. A computerized ResearchTracking software allowed documentation of recruitment and retention effort outcomes..
Results
Among the 1,464 referred patients, 612 (42%) were eligible for study participation. Lack of ongoing care at the study settings and English skills were the main reasons for ineligibility. There were no gender differences in consent/enrollment or completion rates. Ethnic minority patients were represented proportionally to the available population (13%) and were equally willing to consent/enroll and complete both studies as their white counterparts, if they were eligible.
Conclusions
Specific strategies to target language eligibility barriers are necessary to increase minority participation.
Implications for Practice
Future studies could include audio-aided tools in their native language to help recruit patients with limited English skills, if the study tools can be validly translated into other languages and are equivalent to English versions. Efforts to educate and garner support of providers could improve enrollment of patients in cancer studies, especially in studies of audio or video-recorded patient-provider interaction.
Introduction
It is a challenging task to recruit and retain participants for clinical trials, especially women and ethnic minorities.1, 2 Several factors have been implicated as barriers to this effort, including but are not limited to lack of trust in research and the medical system, fear of being used as guinea pigs, and research designs that are culturally incompetent by ignoring cultural beliefs about illness, healthcare, and professionalism.1 Overcoming the common difficulties in recruiting women and ethnic minority patients into clinical studies is important for many reasons, such as examining the health disparity between whites and ethnic minorities, addressing the National Institutes of Health Policy for Public Health Service Grants requirements, and the need to assure, to some extent, the external validity of study findings to be generalizable in the target population. Recruiting women and ethnic minority patients is particularly vital in cancer pain research because they often are at risk for under-treatment of their pain.3
Historically, little research has focused on strategies that facilitate participation of women and ethnic minorities in research.4 Although a variety of strategies have been tried,5 studies are lacking in which investigators examined the effects of strategies specific for recruiting women. Researchers have employed multifaceted strategies to recruit ethnic minority patients with varying success rates that did not guarantee higher minority enrollment6, 7 and added significantly to time and costs required for subject recruitment.7 Equally important as subject recruitment and enrollment is the retention of women and ethnic minorities in clinical studies, topics which are less addressed in the literature.4 Particularly lacking are studies in which investigators examine gender and ethnic differences in specific aspects of research processes: recruitment (referral, eligibility, and consent/enrollment) and study retention (completion). Such knowledge will assist researchers in targeting and mitigating barriers to research participation in each specific area. We employed a variety of strategies as suggested by other authors during implementation of two studies and used an electronic ResearchTracking tool to document and continually make visible our progress in recruiting and retaining women and ethnic minorities. The purpose of this analysis was to examine three aspects of the recruitment processes (study referral, eligibility, and consent/enrollment rates) and study retention (completion rates) as documented by the ResearchTracking program for differences based on subject gender and ethnicity.
For almost two decades researchers have invested considerable effort in the science of patient recruitment and retention of women and ethnic minority participants in clinical trials, because of gender and ethnic disparities in research participation. Researchers have identified several reasons that impede research participation in these populations. For example, Swanson and Ward8 reported that: (1) historic backgrounds making ethnic minorities more concerned about being a “guinea pig;” (2) lack of access to health care where studies are conducted; (3) exclusion criteria that often implicitly omit ethnic minorities; (4) lack of transportation to the study sites; and (5) economic concerns of participation were barriers to recruitment and participation in clinical studies.
In a recent systematic review, Spears and colleagues1 reported a comprehensive list of barriers, similar to Swanson’s and Ward’s findings. In addition, they identified other barriers, such as patients’ fear of genetic research and fear of new medical knowledge.9 A particularly surprising barrier to recruitment was providers’ knowledge deficit or misunderstanding with respect to research. Clearly, there are old and emerging barriers related to recruitment and retention of women and ethnic minorities in research. Despite the gain in knowledge in this area, there is paucity of studies in which investigators examined gender and ethnic differences in recruitment and retention focusing on specific aspects of research process in their studies. However, we identified only three studies in which investigators examined gender and ethnic differences on enrollment and retention.5, 10, 11 Findings from these studies are mixed.
We did not identify any studies in which the investigators examined gender and ethnic differences in rates of referral, eligibility, or consent/enrollment. This knowledge is useful and will assist investigators to target recruitment and retention processes in these patient populations. We addressed this gap in our study using ResearchTracking, an electronic system for tracking, monitoring, and facilitating research recruitment and retention and ongoing study processes. The ResearchTracking keeps recruitment and retention data readily available to the entire research team so that outcomes of all other recruitment and retention efforts are visible at all times. We report the outcomes of the combined efforts that the team used to recruit and retain women and minorities in cancer symptom research, specifically to determine if there were differences in recruitment and retention rates by gender and ethnic minority group.
Methods
Study Design
We conducted a step-by-step descriptive and comparative analysis of recruitment and retention rates in two randomized clinical trials: a pain study (R01 CA62477) and a symptom study (RO1 CA81918). Both studies were conducted in the same settings within a similar timeframe.
Setting and Sample
At the University of Washington Cancer Center or the Seattle Cancer Care Alliance (SCCA), the typical proportion of ethnic minority cancer patients was 13%, our a priori recruitment goal. General inclusion criteria for both studies required that the oncologist consented to audiotaped clinic visits and the patient: (1) had a diagnosis of cancer and would receive ongoing care at the SCCA for the specified study period; (2) could read, write, and speak English; and (3) was aged 18 years or older. Specific eligibility for the pain study required patients having tumor-related pain in the past week. Additional eligibility for the symptom study required patients who had pain and/or fatigue in the past week and would be followed in the study clinics for at least three weeks. Participants received no financial compensation.
Instrument
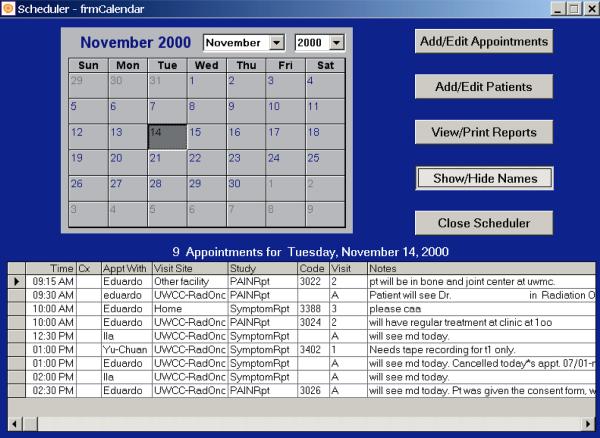
We used a computerized scheduling program (ResearchTracking) to document brief demographic data (age, gender and ethnicity), eligibility status, reasons for ineligibility, enrollment status, completion status, and reasons for withdrawing. ResearchTracking was developed using Visual Basic™ (software development tool) and Access™ (relational database software), both of which are commercially available from Mircrosoft Corporation, Redmond, WA (Figure 1). ResearchTracking allowed systematic tracking of subjects during all study stages and produced reports needed for systematic monitoring of subjects as they progressed through study protocols. Skilled software developers created and tested it for the principal investigator based on specifications from her research experience. ResearchTracking includes reports that are available at the subject level as well as aggregated across subjects, which facilitates annual reports that are required by the institutional review board and funding agency. A daily schedule of all subject appointments allows the research team to know exactly what study work needs to be done on any given day, which facilitates completing subject recruitment and data collection activities when a staff member is sick or unexpectedly unable to work. This feature also allows scheduling of research team meetings on days and at times that will not interfere with subject-related research activities. This program streamlines and organizes the research process for all studies, be they small or large, one or many.
Figure 1.
Procedures
To increase the participation of ethnic minorities, we hired ethnic minority staff as data collectors whenever possible. Our research staff entered all referrals in ResearchTracking and scheduled referred patients for an eligibility-check appointment instead of asking the busy clinicians to determine eligibility. The research staff assessed and entered eligibility status and reasons if not eligible in ResearchTracking. Before recruiting patients to assure a uniform implementation of the consent process and appropriate study description, the research staff were well trained and demonstrated skill competency during a trial-run or role-play test with the principal investigator acting the patient role. Research staff were trained not to pressure patients to consent. Based on general referral criteria, clinicians referred adult patients undergoing cancer treatment to participate in one of the two clinical trials. At the beginning of the consent process, the research staff asked patients to test their eyes by reading a one line header, such as “What are the benefits of this research to me;” this procedure determined English reading eligibility. During the consent process, we asked patients to silently read the consent form along with the research staff as she/he read it aloud. If a potential participant indicated interest in the study but did not have the time to complete the consent, we sent the patient home with the consent form to read. When the patient returned for the study visit, the research staff also read the consent form aloud along with the patient. In addition, we designed our consent form in a three-fold brochure style format, which makes it less intimidating and visually appealing to patients. The research staff invited eligible patients to participate and answered questions before the patient signed the consent form.
In the pain study, consenting patients completed a baseline PAINReportIt® using a touch screen pentablet computer, and then were randomized into control or experimental groups. PAINConsultN,® a computer-generated decision support, was printed and given to the provider of experimental group patients. One week later, patients completed the posttest PAINReportIt.® In the symptom study, consenting patients completed baseline SymptomReport using the same computer, and then were randomized into control or experimental groups. The experimental group patients received individually tailored multimedia educational information for managing pain and fatigue. About three-four weeks later, patients completed the posttest SymptomReport. At each staff meeting that were held weekly to monthly over the study period depending on staff and study issues, the team used the ResearchTracking reports to identify issues and discuss potential solutions to assure that we achieved study aims.
Data Analysis
A total of 1,464 patients (59% female and 41% male) were referred to one of the two studies; 45% were referred to the pain study (mean age =53.6 years, SD=14.8) and 55% to the symptom study (mean age = 52.9 years, SD = 14). Among them, 79% were white and 13% were ethnic minorities. For the other 8% (n = 120) of the referrals, ethnicity was unknown. Among the 1,464 referred patients, 612 (42%) were determined to be eligible for participation in one of the studies, and 164 (11%) were not assessed for eligibility, due to scheduling difficulties or missed appointments. There were no statistically significant differences by age (ANOVA p>.05), gender, ethnic distribution, or study between those for whom eligibility was assessed or not assessed (Fisher’s exact test, p > .05). Therefore, patients not assessed for eligibility were excluded from further analyses.
As typically defined, we defined “rate” as the ratio of two counts (measurements), which we reported as a percentage. Comparison of age, gender, ethnic distribution, and eligibility, enrollment and completion rates between the two studies indicated that the symptom study had statistically significantly higher proportions of women, eligible patients, enrolled patients, and completed patients than the pain study, but there were no significant differences in age or ethnic distribution. Because of the observed differences, we analyzed study data separately. We used Fisher’s exact tests to examine the proportion of whites versus ethnic minorities, and men versus women, who were referred, eligible, enrolled, and retained to complete the studies.
Results
Referral
The final sample included 1,300 patients with known eligibility (n =572, pain study; n = 728, symptom study). For the pain study, the majority of the 572 referred patients were female (52%). There was no statistically significant gender difference in referral rates. Of the 572 patients referred to the pain study, 78% were white, 13% were ethnic minority, and 9% were unknown ethnicity; the 9% are not include in further analyses. We found no statistically significant difference between whites and ethnic minorities regarding the referral rate.
For the symptom study, the majority of the 728 referred patients were female (65%). There were no statistically significant gender differences in referral rates. Of the 728 patients referred to the symptom study, 81% were whites, 13% were ethnic minorities, and 6% were of unknown ethnicity; the 6% are not include in further analyses. There was no statistically difference between whites and ethnic minorities in referral rates. Ethnic minorities and whites were equally likely to be referred to the studies. Ethnic group distribution was not different by gender.
Eligibility
For the pain study, 41% of the 572 referred patients were eligible. There were no statistically significant differences in the eligibility rate between men and women or between white and ethnic minority patients (Table 1). However, a significantly higher proportion of the few patients with unknown ethnicity (<10%) was ineligible (92%) rather than eligible (8%). The major reasons for being ineligible were (a) no tumor-induced pain (22%), (b) no ongoing care at the SCCA (20%), and (c) non-English speaker (6%). Those with unknown ethnicity were not included in further analyses.
Table 1.
Comparison of eligibility, enrollment, and completion rates between women and men and between whites and ethnic minorities.
| Gender | Ethnicity | ||||||
|---|---|---|---|---|---|---|---|
| Women N (%)a |
Men N (%) |
Fisher’s Exact Two-tailed p |
White N (%) |
Ethnic Minority N (%) |
Fisher’s Exact Two-tailed p |
||
| Pain Study | Eligible (n = 234, 41% of the referred patients) |
112 (38%) | 122 (46%) |
0.11 | 200 (45%) |
30 (41%) |
0.53 |
| Enrolled (n = 148, 63% of the eligible patients) |
77 (69%) |
71 (58%) |
0.11 | 128 (64%) |
20 (67%) |
0.84 | |
| Completed (n = 138, 93% of the enrolled patients) |
72 (94%) |
66 (93%) |
1.00 | 118 (92%) |
20 (100%) |
0.36 | |
| Symptom Study |
Eligible (n = 378, 52% of the referred patients) |
248 (53%) |
130 (51%) |
0.64 | 331 (56%) |
39 (42%) |
0.02* |
| Enrolled (n = 286, 76% of the eligible patients) |
185 (75%) |
101 (78%) |
0.53 | 257 (78%) |
29 (74%) |
0.69 | |
| Completed (n = 230, 80% of the enrolled patients) |
147 (80%) |
83 (82%) |
0.64 | 207 (81%) |
23 (79%) |
0.81 | |
Percentage was calculated within the specified gender or ethnic group.
denotes p < .05
For the symptom study, 52% of the 728 referred patients were eligible. A statistically smaller proportion of ethnicity minorities (42%) was eligible for the symptom study than their white counterparts (56%) (Table 1). We found no differences in eligibility between men and women. The major reasons for ineligibility included (a) no pain or fatigue (27%), (b) not receiving ongoing care at the SCCA (26%), (c) no oncologist consent (8%), and non-English speaker (5%).
Consent/Enrollment Rate
For both the pain and symptom studies, all subjects who consented to participate also enrolled in the study; we therefore collapsed the two concepts into one variable consent/enrollment. For the pain study, 63% of subjects consented/enrolled in the study if eligible. There were no statistically significant gender or ethnic differences in the consent/enrollment rates. That is, male and female, white and ethnic minority subjects were equally likely to participate in the study if eligible.
For the symptom study, 76% of subject consented/enrolled in the study if eligible. There was no gender or ethnic differences in the consent/enrollment rates (Table 1).
Retention and Study Completion
For the pain study, 93% of enrolled subjects were retained and completed the study. There were no statistically significant differences in the retention and completion rates between men and women or between whites and ethnic minorities (Table 1). For the symptom study, 80% of enrolled subjects were retained and completed the study. We also found that there were no statistically significant gender or ethnic differences in retention and completion rates. Reasons for attrition in both studies included: (1) too sick (n=13); (2) moved and lost to follow-up (n=17); and (3) voluntary withdrawal (n=36).
Discussion
We found that men and women were equally willing to participate in and complete cancer symptom studies, if they were eligible. We observed the same pattern for whites and ethnic minority patients. Our study findings also indicated that women and ethnic minority patients were as likely to be referred to the studies as their male and white counterparts. The strategy we used to get a high referral rate was to give clinicians general inclusion criteria so that the detailed eligibility assessment would not be the clinicians’ responsibility but done by the research staff. Using this method, about half of the referred patients were not eligible for the study. This approach may have increased the time and cost for study recruitment, but prevented the pre-exclusion of patients due to clinicians’ bias about the patients’ symptoms.
Lack of ongoing care at the study setting, lack of oncologist consent, and English skills were barriers to eligibility. Specific strategies to target these barriers, especially to encourage oncologists’ support of studies and include non-English speakers, are necessary to increase minority participation when levels greater than their distribution in the general population is needed, especially in areas with small numbers of ethnic minority patients such as in Seattle, WA. For example, we can minimize potential subject ineligibility due to lack oncologist consent by early partnering with the oncologists during the design of the study. This approach will boost their understanding of the research study and the potential benefit. This understanding is pertinent because researchers have found that provider ignorance and lack of understanding about the research process is a barrier to research participation.10 Although a remarkable number of oncologists consented to the study, 8% of them did not want to be audio-taped. While this percentage is relatively small, likely because the studies were conducted in academic research centers, where research awareness is high, we missed the opportunity to recruit the patients cared for by these oncologists.
Our finding that ethnic minorities are equally willing to consent and enroll in research is supported by Wendler’s and colleagues’ systematic literature review.12 We attribute our success of consent/enrollment rates in both studies to our diverse research staff and the innovative consenting approach that unobtrusively assessed patients’ reading and comprehension abilities and the reading of the consent form aloud. This approach intended to increase comprehension because language understanding is greater in the auditory mode than when read silently. Understanding what the research entails is a prerequisite to consent/enrollment. Researchers have found that one of the barriers to research participation by under-represented minority subjects relates to patients’ knowledge deficit.1 Other have found that minority participants’ willingness to participate in studies could depend on the characteristics of the individual studies.12
Our finding that women equally consented and enrolled in our studies as men is welcome news given the National Institutes of Health’s requirement for adequate gender representation in clinical trials. In both studies, we successfully met our goal for a female patient sample that was comparable to the available female cancer population. Other investigators of a non-cancer study reported that women were more likely to refuse consent/enrollment than men,11 but like our study women and men were as likely to complete the study.11 Contrary to findings of other investigators in a non-cancer study where completion rates were significantly lower for women than men5, our completion rates were similar for women and men. It is possible that our ResearchTracking system contributed to differences in our findings and those of others,5 but comparative studies are needed to confirm this possibility.
Our finding that both women and ethnic minority subjects were equally retained as the men and whites, which was remarkable, given the patient population from which we recruited. Sullivan-Marx and colleagues7 reported similar finding with respect to retention of women in their study, where they retained 71% of women in their 16-week exercise study. Our consent procedures facilitated by our research tool, ResearchTracking, was effective for systematic monitoring of our success in achieving our recruitment and retention goals based on gender and ethnic minority status. Active monitoring is the key to success in any clinical trial and an effective computerized tool such as ResearchTracking, is crucial in monitoring recruitment and retention processes.
Although our findings are important, some limitations detracted from them. Our study findings are limited to the study settings, research-intensive medical centers. The clinicians were well aware of research ongoing at the center and may have been more willing to refer minority patients to us. We do not have information about the ethnic composition of clinicians or the impact of the clinicians’ ethnicity on referrals. We were not able to obtain ethnicity for 8% of the referred patients, and it is unknown how many of those patients were from ethnic minority groups. Also, we were not able to determine eligibility for 11% of the referred patients, and it not clear how this issue affected study findings. Finally, we did not design the study to determine the effect of specific strategies for obtaining referrals, recruiting subjects to consent and enroll in the studies, and retaining the subjects to the end of the studies.
Implications
Our study findings are encouraging and show that our strategies for facilitating recruitment, consent, enrollment, retention were effective. These strategies were multiple and inclusive of ongoing monitoring of study processes via ResearchTracking. These strategies were implemented as a set and may include best practices for recruitment, enrollment, and retention of women and ethnic minorities in cancer research. For example our strategy of using a brochure style consent form to reduce its intimidating appearance and then reading it aloud may reduce confusion about the study procedures and what the subject will be expected to do during the study. Greater clarity may be important to women and ethnic minorities completing a study to which they consent to participate.
Like others,13 we identified language as one of the barriers in recruiting minority patients. Newer immigrants whose English is not fluent or requires an interpreter are likely to be ineligible. In future studies, an audio-aided recruitment tool, where a voice recorded consent form could be read to potential patients in their preferred language, may be useful. Such an aid would also require study instruments that are validly translated into other languages and equivalent to English tools. We can also minimize exclusion of patients due to language barrier by hiring bilingual research staff, as has been done by other researchers9 or taking advantage of translation services within the institution, especially to answer patients’ questions once they have used the audio-aided consent tool. Given these encouraging findings and evolution in technologies, our group has migrated the ResearchTracking tool from a Visual Basic application to an Internet-based format for use in all our research studies.
Acknowledgements
This research was made possible by Grant Numbers 2RO1 CA62477 and 1RO1 CA81918 from the National Institutes of Health, National Cancer Institute. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute. The authors thank Kevin Grandfield for editorial assistance and Veronica Angulo for administrative support.
Footnotes
Two authors (DW, MKMJ) are owners of a company that has no relationship to the research reported in this manuscript. The other authors have no conflicts related to the research reported in this manuscript.
Contributor Information
Hsiu-Ying Huang, Taipei Medical University-Shuang Ho Hospital No. 291, Jhongjheng Road, Jhonghe District, New Taipei City 23561, Taiwan, R.O.C..
Miriam O. Ezenwa, Biobehavioral Health Science (MC 802) College of Nursing, University of Illinois at Chicago 845 South Damen Ave, Chicago, IL 60612-7350.
Diana J. Wilkie, Department of Biobehavioral Health Science (MC 802) College of Nursing, University of Illinois at Chicago 845 South Damen Avenue, Room 660, Chicago, IL 60612-7350.
M. Kay Judge, Nursing Consult LLC, Seattle, WA 98125.
References
- 1.Spears CR, Nolan BV, O’Neill JL, Arcury TA, Grzywacz JG, Feldman SR. Recruiting underserved populations to dermatologic research: a systematic review. Int J Dermatol. 2011;50(4):385–395. doi: 10.1111/j.1365-4632.2010.04813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ejiogu N, Norbeck JH, Mason MA, Cromwell BC, Zonderman AB, Evans MK. Recruitment and retention strategies for minority or poor clinical research participants: lessons from the Healthy Aging in Neighborhoods of Diversity across the Life Span study. Gerontologist. 2011;51(Suppl 1):S33–45. doi: 10.1093/geront/gnr027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330(9):592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 4.Ness RB, Nelson DB, Kumanyika SK, Grisso JA. Evaluating minority recruitment into clinical studies: how good are the data? Ann Epidemiol. 1997;7(7):472–478. doi: 10.1016/s1047-2797(97)00080-x. [DOI] [PubMed] [Google Scholar]
- 5.Falcon R, Bridge DA, Currier J, et al. Recruitment and retention of diverse populations in antiretroviral clinical trials: practical applications from the gender, race and clinical experience study. J Womens Health (Larchmt) 2011;20(7):1043–1050. doi: 10.1089/jwh.2010.2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson KS, Elbert-Avila K, Kuchibhatla M, Tulsky JA. Racial differences in next-of-kin participation in an ongoing survey of satisfaction with end-of-life care: a study of a study. J Palliat Med. 2006;9(5):1076–1085. doi: 10.1089/jpm.2006.9.1076. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan-Marx EM, Mangione KK, Ackerson T, et al. Recruitment and retention strategies among older African American women enrolled in an exercise study at a PACE program. Gerontologist. 2011;51(Suppl 1):S73–81. doi: 10.1093/geront/gnr001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swanson GM, Ward AJ. Recruiting minorities into clinical trials: toward a participant-friendly system. J Natl Cancer Inst. 1995;87(23):1747–1759. doi: 10.1093/jnci/87.23.1747. [DOI] [PubMed] [Google Scholar]
- 9.Kao B, Lobato D, Grullon E, et al. Recruiting Latino and Non-Latino Families in Pediatric Research: Considerations from a Study on Childhood Disability. J Pediatr Psychol. 2011;36(10):1093–1101. doi: 10.1093/jpepsy/jsr030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allman RM, Sawyer P, Crowther M, Strothers HS, 3rd, Turner T, Fouad MN. Predictors of 4-year retention among African American and white community-dwelling participants in the UAB study of aging. Gerontologist. 2011;51(Suppl 1):S46–58. doi: 10.1093/geront/gnr024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis RM, Hitch AD, Nichols M, Rizvi A, Salaam M, Mayer-Davis EJ. A collaborative approach to the recruitment and retention of minority patients with diabetes in rural community health centers. Contemp Clin Trials. 2009;30(1):63–70. doi: 10.1016/j.cct.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Wendler D, Kington R, Madans J, et al. Are racial and ethnic minorities less willing to participate in health research? PLoS Med. 2006;3(2):e19. doi: 10.1371/journal.pmed.0030019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacEntee MI, Wyatt C, Kiyak HA, et al. Response to direct and indirect recruitment for a randomised dental clinical trial in a multicultural population of elders. Community Dent Oral Epidemiol. 2002;30(5):377–381. doi: 10.1034/j.1600-0528.2002.00003.x. [DOI] [PubMed] [Google Scholar]