Abstract
Purpose
We performed the present study to evaluate the prognostic factors for the surgical outcome of varicocelectomy in the treatment of a painful varicocele.
Materials and Methods
A total of 77 patients undergoing varicocelectomy were enrolled. All the patients were examined for body mass index (BMI), varicocele grade, testosterone, follicle stimulating hormone (FSH), luteinizing hormone (LH), semen analysis, maximal vein diameter, and discrepancy of testicular volume. At a follow-up visit 3~6 months after the surgery, the patient response was graded as a complete response, partial response, or no response. The resolution of pain was defined as a complete or partial response. We used logistic regression analyses to determine the preoperative factors for predicting a complete response and the resolution of pain.
Results
Ten subjects were lost to follow-up. The remaining 67 patients were included in this study. The pain was completely resolved in 47.8% of patients, partial resolution was observed in 25.4% of patients, and failure was reported in 26.9% of patients. Among the parameters, only a longer duration of pain (≥3 months) was an independent factor related to the complete response of pain (odds ratio, 7.371; p=0.010) and the resolution of pain (odds ratio, 7.209; p=0.042). The parameters of semen analysis results, testosterone, LH, FSH, BMI, grade, ultrasonography results, and the type of surgical approach did not significantly predict the resolution of pain.
Conclusions
The duration of pain (≥3 months) was an independent prognostic factor for the complete response of pain and the resolution of pain.
Keywords: Varicocele, Pain, Laparoscopy, Microsurgery
INTRODUCTION
Varicocele is an abnormal tortuosity and enlargement of the veins of the pampiniform plexus in the spermatic cord. Varicocele has been known to be a cause of pain in 2% to 14% of men suffering chronic scrotal pain.1,2 Additionally, 2% to 10% of men with varicocele complain of scrotal pain.3
A varicocelectomy should be considered in patients with no alleviation of their pain after conservative management, including resting, scrotal elevation, and nonsteroidal anti-inflammatory analgesics. The success rate of the surgical approach for the treatment of painful varicocele has ranged from 53% to 92% for complete resolution, from 5% to 20% for partial resolution, and from 0% to 20% for failure.4
A longer duration of pain, body mass index (BMI), varicocele grade, and quantity and quality of preoperative pain have been reported as predictive factors for pain resolution after surgery.5-8 However, there are few data with respect to hormone levels, semen parameters, and ultrasonographic features as prognostic factors. Therefore, we performed the present study to evaluate prognostic factors for surgical outcome, including follicle stimulating hormone (FSH), luteinizing hormone (LH), testosterone, the parameters of scrotal ultrasonography, semen analysis, age, duration of pain, BMI, and varicocele grade.
MATERIALS AND METHODS
1. Patients
The institutional review board of the National Police Hospital approved this study in December 2012. Data were collected retrospectively on 77 patients with left painful varicocele undergoing a varicocelectomy during a 5-year period beginning in January 2007. None of the patients had responded to prior conservative management for 3~4 weeks. Patients who had other causes of scrotal pain, such as testicular torsion, epididymitis, orchitis, inguinal hernia, testicular tumor, or trauma were excluded from the study.
Varicocele was graded as follows9: grade I, palpable only with the Valsalva maneuver; grade II, palpable without the Valsalva maneuver; and grade III, visible from a distance. All of the patients were evaluated for the serum levels of testosterone, FSH, and LH in the morning (between 8:00 and 11:00 AM). The semen analysis was performed after 3 days of abstinence from ejaculation. The maximal vein diameter was examined while the patient relaxed using scrotal ultrasonography. The testicular volume (bilateral) was measured by ultrasonography, and a discrepancy in the testicular volume was defined as a testis volume difference ≥3 ml.10
The surgical techniques included laparoscopic varicocelectomy and subinguinal varicocelectomy with a surgical microscope (×10~×25). In the laparoscopic varicocelectomy, 3 ports (each 5 mm) were used. The spermatic veins were clipped at the site of the internal inguinal ring after incising the posterior peritoneum. An attempt was made to preserve the testicular artery. In all subinguinal varicocelectomy cases, the testis was delivered through the incision, and the gubernacular veins and external spermatic perforating veins were divided. Additionally, an attempt was made to preserve the testicular artery and lymphatics.
All patients were asked to return for a follow-up visit 3~6 months after surgery. The patient response was graded as a complete response (pain was completely absent after the surgery), partial response (pain persisted but was reduced after the surgery), or no response (pain remained unchanged after the surgery).11 The resolution of pain was defined as a complete or partial response.
2. Statistical analysis
Because of the markedly skewed distribution of the demographic characteristics, medians and interquartile ranges (IQR) were adopted.
To determine the preoperative factors for predicting a complete response and the resolution of pain after surgery, statistical analyses were performed with logistic regression analyses using the Statistical Package for the Social Sciences, version 11.0 (SPSS, Chicago, IL, USA). A p value of <0.05 was considered to be statistically significant.
RESULTS
A total of 77 patients with left painful varicocele underwent a varicocelectomy at our institution, and 10 (13%) subjects were lost to follow-up after the varicocelectomy. The remaining 67 patients were included and the median follow up period was 6.0 months (IQR: 6.0~9.0 months). The baseline characteristics of the patients are shown in Table 1.
Table 1.
Patient characteristics
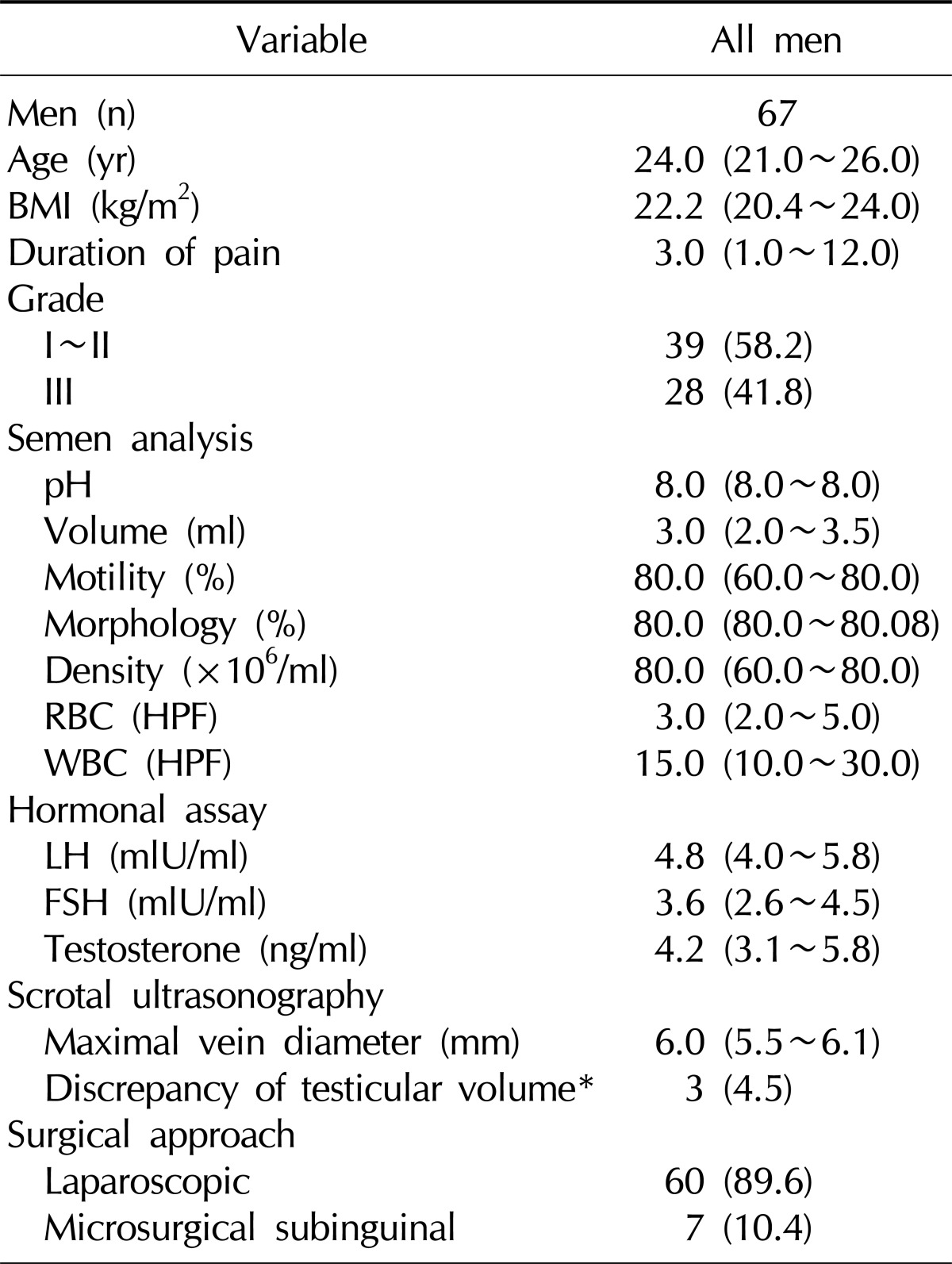
Values are presented as number (%) or median (interquartile range).
BMI: body mass index, RBC: red blood cells, WBC: white blood cells, HPF: high power field, LH: luteinizing hormone, FSH: follicle stimulating hormone.
*Testis volume difference ≥3 ml.
The pain was completely resolved in 47.8%, a partial resolution was observed in 25.4%, and failure was reported in 26.9% (Table 2).
Table 2.
Outcome of varicocelectomy performed for pain
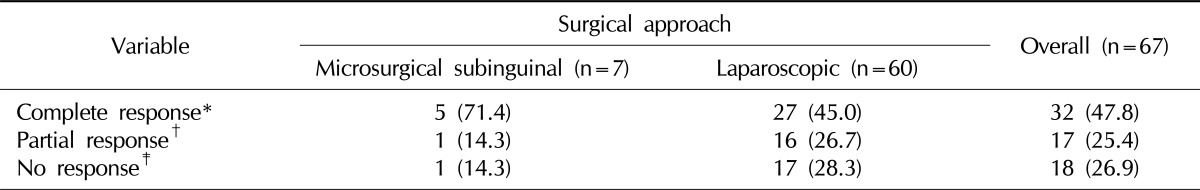
Values are presented as number (%).
*Pain was completely absent 3~6 months after surgery. †Pain persisted but was reduced 3~6 months after surgery. ‡Pain remained unchanged 3~6 months after surgery.
The results of the multivariate analysis of the predictors for the success of the varicocelectomy are presented in Tables 3 and 4. The semen parameters and levels of testosterone, LH, and FSH were not related to the response after varicocelectomy. Additionally, the BMI, varicocele grade, scrotal ultrasonography parameters, and the type of surgical approach did not significantly predict the resolution of pain. Only a longer duration of pain (≥3 months) was an independent factor related to a complete response to surgery (odds ratio, 7.371; p=0.010) and the resolution of pain (odds ratio, 7.209; p=0.042).
Table 3.
Multivariate analysis of the predictive factors for the complete resolution of pain
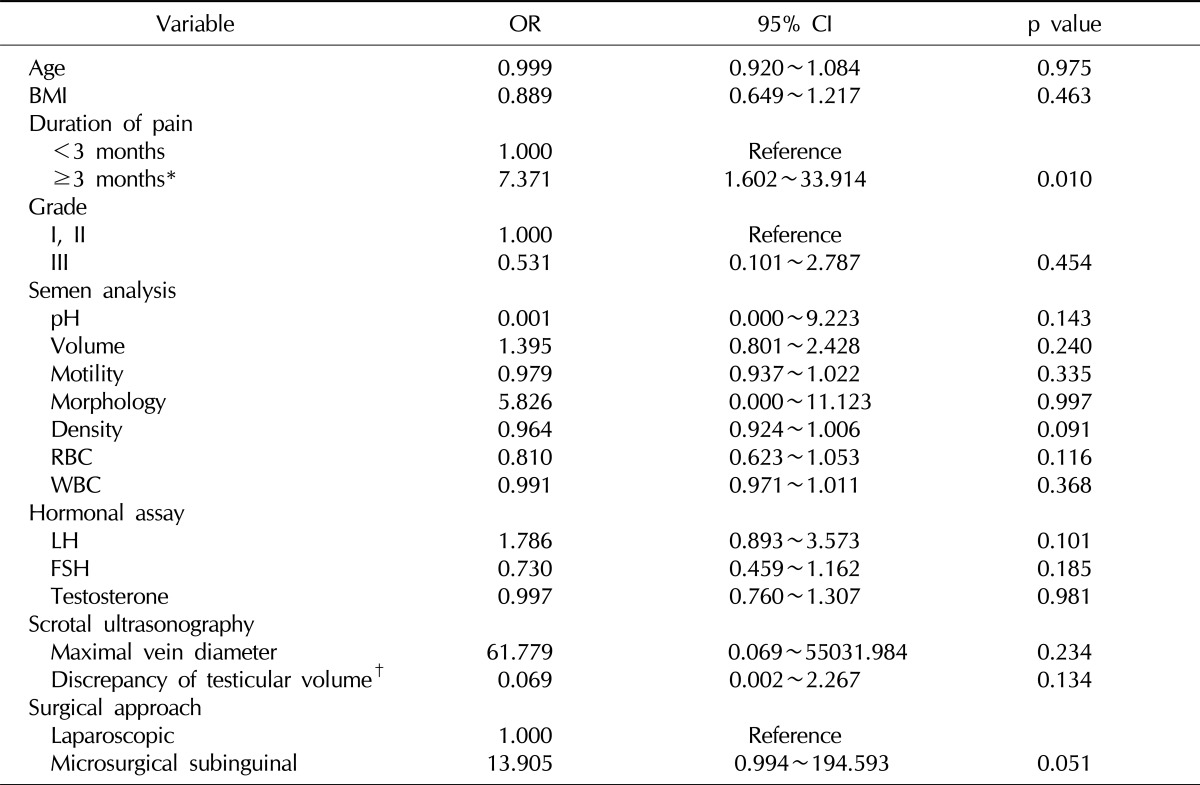
Statistical analysis performed using multiple logistic regression analysis differences between groups considered significant at p<0.05.
OR: odds ratio, CI: confidence interval, BMI: body mass index, RBC: red blood cells, WBC: white blood cells, LH: luteinizing hormone, FSH: follicle stimulating hormone.
*Statiscally significant. †Testis volume difference ≥3 ml.
Table 4.
Multivariate analysis of the predictive factors for the resolution of pain
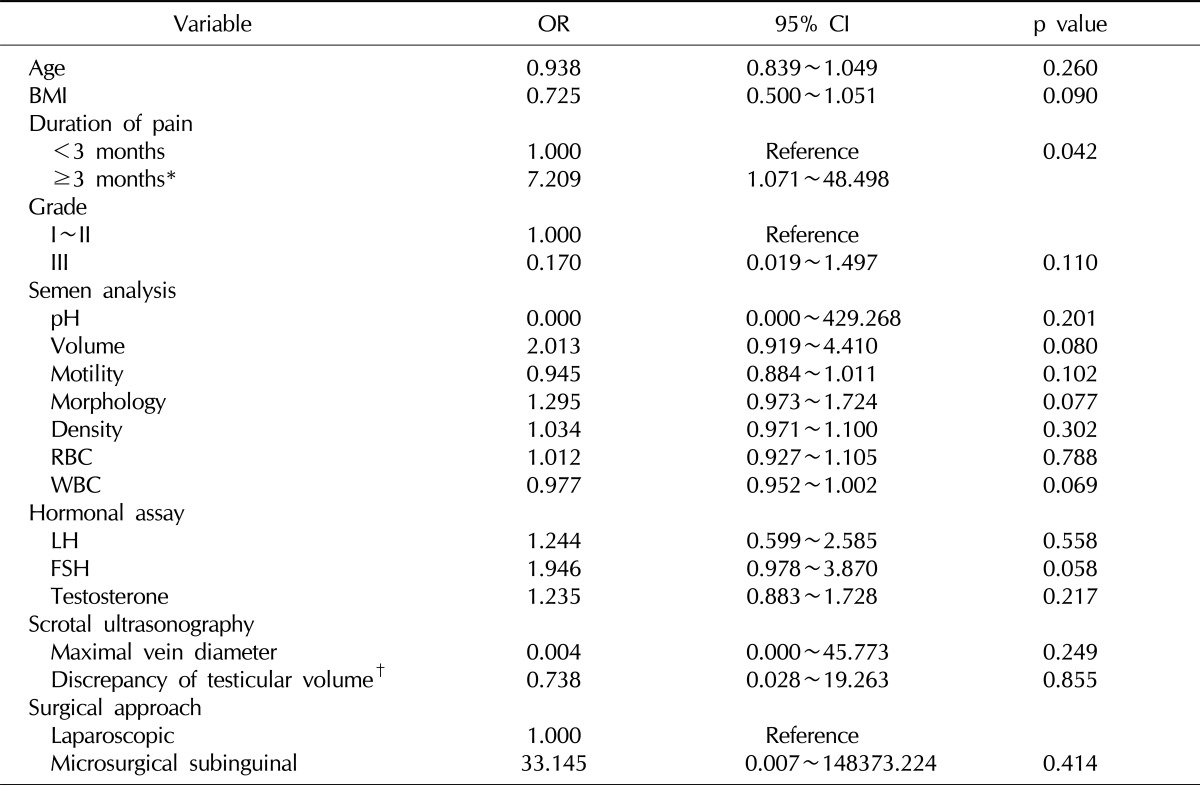
Resolution of pain: complete response and partial response. Statistical analysis performed using multiple logistic regression analysis differences between groups considered significant at p<0.05.
OR: odds ratio, CI: confidence interval, BMI: body mass index, RBC: red blood cells, WBC: white blood cells, LH: luteinizing hormone, FSH: follicle stimulating hormone.
*Statiscally significant. †Testis volume difference ≥3 ml.
DISCUSSION
Our results indicate that the duration of pain (≥3 months) is an independent prognostic factor for a complete response to surgery and the resolution of pain. The results of the present study correspond with the results of earlier studies, which reported that a longer duration of pain could predict a successful surgical outcome. In a large retrospective study that recruited 237 men who underwent a subinguinal varicocelectomy for scrotal pain, the patients who presented with long-term (>3 months) pain had a significantly higher chance of benefiting from the operation compared with the patients who presented with short-term pain (success rates: 98% in the >3 month group, 82.3% in the <3 month group; p<0.05).5 Another retrospective study including 53 cases who underwent subinguinal and inguinal varicocelectomy reported that the degree of improvement in the postoperative symptoms was relatively higher in patients who had a shorter duration of pain (<6 months) than in those who had a longer duration of pain (≥6 months) (p=0.002).8 A recent retrospective study including 76 patients also suggested that a longer duration of pain is associated with the resolution of pain (p=0.01).6 Although there are differences in the duration of pain according to each study, a longer duration of pain appears to be associated with a successful surgical outcome.
No difference with regard to the semen parameters, hormone levels, or sonographic features between the responders and non-responders was noted according to our results. To the best of our knowledge, there has only been one study utilizing data concerning the aforementioned parameters. In this retrospective study that included 76 patients, semen parameters (sperm motility, sperm morphology, sperm density, and testicular volume), ultrasonographic features (discrepancy of testicular volume and maximal vein diameter), and hormone levels (FSH, LH, and testosterone) were not related to the success of varicocelectomy for pain.6 Our findings confirmed those results.
Preoperative BMI and varicocele grade have been suggested to be associated with the success rate.8,12
Our data also showed a negative trend for BMI (odds ratio, 0.725; p=0.090) and grade III (odds ratio, 0.170; p=0.110). However, these differences were not significant. To better elucidate their relationship, follow-up studies including a larger patient population are needed. Additionally, dull pain has been reported to have a significant association with the successful resolution of pain compared with sharp pain.3,7,13 However, another study did not show a significant difference with respect to the type of pain.6,8 In this study, we could not evaluate this relationship due to the lack of data concerning the pain characteristics in the patient charts. Therefore, prospective data collection for a large population is needed to define the relationship between the type of pain and the outcome of surgery.
The overall success rate for laparoscopic varicocelectomy was 71.7% (complete response 45.0%; partial response 26.7%) in this study. According to a recent review, the overall pain resolution rate (complete and partial responses) of laparoscopic varicocelectomy for three different reports was 86% (ranging from 76% to 95%).4 Furthermore, data from Korea showed similar results.14,15 The success rate in our study was slightly lower than that in other studies. The reason for this difference might be due to the characteristics of the study populations. We collected data from policemen, who experience vigorous activity and standing or sitting positions for long periods compared with the general population. We speculate that the negative effect of the behavior of policemen could lower the success rate of a laparoscopic varicocelectomy.
Comparing success rates according to the surgical approach was not possible due to the small number of microscopic varicocelectomies that were performed. The overall pain resolution (complete and partial response) rate of microscopic varicocelectomy for seven different reports was 93% (ranging from 79.2 to 100%).4 To define which method is superior for controlling the pain of varicocele, a prospective randomized control trial is needed.
Several limitations of the present study warrant mentioning. First, retrospective studies are less reliable than prospective studies. In addition, because this study consisted of a single institution and was conducted in a single occupational cluster, there might be a potential for selection bias.
CONCLUSIONS
The present results revealed that the duration of pain (≥3 months) was an independent prognostic factor for a complete response and the resolution of pain after surgery to treat painful varicocele. Future investigations should explore this relationship. The confirmation of these associations in a prospective, longitudinal data set would also be informative.
References
- 1.Kass EJ, Marcol B. Results of varicocele surgery in adolescents: a comparison of techniques. J Urol. 1992;148:694–696. doi: 10.1016/s0022-5347(17)36696-x. [DOI] [PubMed] [Google Scholar]
- 2.Marmar JL, Kim Y. Subinguinal microsurgical varicocelectomy: a technical critique and statistical analysis of semen and pregnancy data. J Urol. 1994;152:1127–1132. doi: 10.1016/s0022-5347(17)32521-1. [DOI] [PubMed] [Google Scholar]
- 3.Peterson AC, Lance RS, Ruiz HE. Outcomes of varicocele ligation done for pain. J Urol. 1998;159:1565–1567. doi: 10.1097/00005392-199805000-00043. [DOI] [PubMed] [Google Scholar]
- 4.Shridharani A, Lockwood G, Sandlow J. Varicocelectomy in the treatment of testicular pain: a review. Curr Opin Urol. 2012;22:499–506. doi: 10.1097/MOU.0b013e328358f69f. [DOI] [PubMed] [Google Scholar]
- 5.Altunoluk B, Soylemez H, Efe E, Malkoc O. Duration of preoperative scrotal pain may predict the success of microsurgical varicocelectomy. Int Braz J Urol. 2010;36:55–59. doi: 10.1590/s1677-55382010000100009. [DOI] [PubMed] [Google Scholar]
- 6.Chen SS. Factors predicting symptomatic relief by varicocelectomy in patients with normospermia and painful varicocele nonresponsive to conservative treatment. Urology. 2012;80:585–589. doi: 10.1016/j.urology.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Kim HT, Song PH, Moon KH. Microsurgical ligation for painful varicocele: effectiveness and predictors of pain resolution. Yonsei Med J. 2012;53:145–150. doi: 10.3349/ymj.2012.53.1.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park HJ, Lee SS, Park NC. Predictors of pain resolution after varicocelectomy for painful varicocele. Asian J Androl. 2011;13:754–758. doi: 10.1038/aja.2010.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lyon RP, Marshall S, Scott MP. Varicocele in childhood and adolescence: implication in adulthood infertility? Urology. 1982;19:641–644. doi: 10.1016/0090-4295(82)90019-x. [DOI] [PubMed] [Google Scholar]
- 10.Sigman M, Jarow JP. Ipsilateral testicular hypotrophy is associated with decreased sperm counts in infertile men with varicoceles. J Urol. 1997;158:605–607. [PubMed] [Google Scholar]
- 11.Levine LA, Matkov TG, Lubenow TR. Microsurgical denervation of the spermatic cord: a surgical alternative in the treatment of chronic orchialgia. J Urol. 1996;155:1005–1007. doi: 10.1016/s0022-5347(01)66369-9. [DOI] [PubMed] [Google Scholar]
- 12.Yaman O, Ozdiler E, Anafarta K, Göğüş O. Effect of microsurgical subinguinal varicocele ligation to treat pain. Urology. 2000;55:107–108. doi: 10.1016/s0090-4295(99)00374-x. [DOI] [PubMed] [Google Scholar]
- 13.Al-Buheissi SZ, Patel HR, Wazait HD, Miller RA, Nathan S. Predictors of success in surgical ligation of painful varicocele. Urol Int. 2007;79:33–36. doi: 10.1159/000102910. [DOI] [PubMed] [Google Scholar]
- 14.Yeo JK. A comparative study of varicocelectomy for painful varicocele: modified palomo, laparoscopic approach and microscopic subinguinal approach. Korean J Androl. 2009;27:201–205. [Google Scholar]
- 15.Lee MJ, Cho SH, Choi JY, Kim SB, Lee ST, Min SK. Significance of laparoscopic varicocelectomy. Korean J Androl. 2010;28:209–216. [Google Scholar]


