Abstract
Intratesticular cysts, once thought to be a rarity, are now being reported with an increasing prevalence as a result of the wider use of scrotal ultrasound scanning. Despite greater understanding of intratesticular cysts, their management remains unclear. Treatment has included enucleation and even radical orchiectomy over fear of the possibility of an associated malignancy. A more conservative approach with serial ultrasound scanning has been advocated if a clear distinction can be made between neoplastic and non-neoplastic testicular cysts. However, in view of the benign nature of such cysts, even repeated ultrasound scanning may not be necessary and may be considered over-treatment. In this study we present clinical and morphological characteristics of multiple cysts in the right testicle in a 62-year-old patient, where a slightly nodular lesion in the right testicle was detected.
Keywords: Cysts, Testis, Neoplasms
Intratesticular simple cysts are detected incidentally and occur in men 40 years of age and older. Their size is variable and can range from 2 mm to 2 cm in diameter. These cysts, once thought to be a rarity, are now being reported with an increasing prevalence as a result of the wider use of scrotal ultrasound scanning.1 Despite a greater understanding of intratesticular cysts, their proper management remains unclear. Treatment has included enucleation and even radical orchiectomy over fear of the possibility of an associated malignancy. A more conservative approach with serial ultrasound scanning has been advocated if a clear distinction can be made between neoplastic and non-neoplastic testicular cysts.2-4 However, given the benign nature of such cysts, even repeated ultrasound scanning may not be necessary and may be considered over-treatment. In this study we present the clinical and morphological characteristics of multiple cysts in the right testicle of a 62-year-old patient, where a slightly nodular lesion in the right testicle was detected.
CASE REPORT
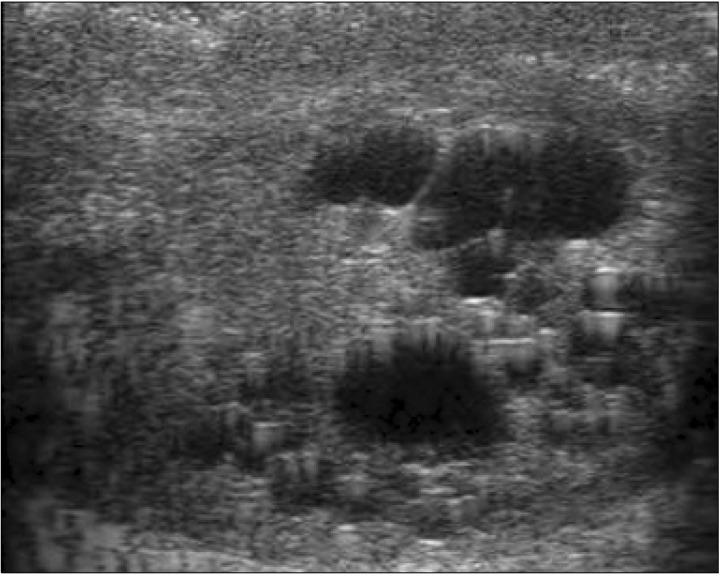
A 62-year-old male presented with chronic pain on the right scrotum. Chronic epididymitis was diagnosed after ultrasound findings of chronic inflammation of the epididymis, with further findings of multiple testicular hypoechoic lesions, according to analytical and negative markers (Fig. 1). There were no abnormalities in testicular tumor markers. Conservative management, consisting of scrotal support and non-steroidal anti-inflammatory medication, was applied without resolution of pain.
Fig. 1.
Multiple simple cyst in the right testis: a well circumscribed, anechoic area with a smooth wall and posterior acoustic enhancement.
Therefore, we performed right epididymectomy for pain relief and diagnostic testicular cyst enucleation (Fig. 2). The cyst was removed intact.
Fig. 2.
The specimen was a product of right intratesticular cyst excision, measuring 0.2 g in weight with dimensions of 1.0×0.8×0.6 cm.
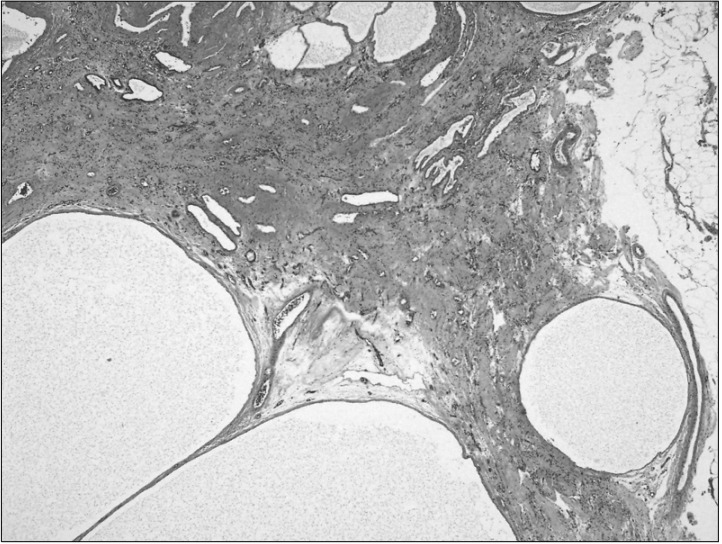
Pathology presented findings of a multiple cystic lesion filled with clear fluid free of sperm and unaffecting the epididymis or tunica albuginea, with the largest measuring 1.0×0.8 cm. The examination revealed a fibrous wall lined with simple flattened epithelium with multilobulated cysts (Fig. 3). No evidence of malignancy was found.
Fig. 3.
Multiple simple cysts were seen. The cyst wall was fibrous tissue completely lined by simple flattened epithelial cells. There were no sperm in the cyst (H&E stain, ×40).
DISCUSSION
Intratesticular cysts were once considered rare, but with increasing use of scrotal ultrasound, the prevalence would appear to be increasing.1 Leung et al5 scanned 40 normal male volunteers and found simple cysts in 8%. Gooding et al6 also found intratesticular cysts present in 9.8% of 307 normal men undergoing high-resolution scrotal ultrasound scanning. Simple intratesticular cysts have a pathognomonic echo pattern and high-resolution ultrasound permits the clear distinction between simple intratesticular cysts and other cystic lesions like epidermoid cysts and cystic testicular tumors.7
In a large series of 847 men, Hamm et al1 found cystic tumors in 16 of the 34 men with cysts in the testes.
Nearly all presented with a palpable mass and 75% had solid elements on scanning. Of the 18 non-neoplastic cysts, 13 were simple intratesticular cysts, which were all discovered incidentally, were impalpable, and had classical sonographic characteristics. Intratesticular cysts range in size from 2 mm to 2 cm.6 While the majority were found within the inner substance of the testis, those that are peripherally oriented may be suspected on physical examination by palpation of a focal, non-tender mass.8
The management of simple intratesticular cysts is controversial. Radical orchiectomy might be advocated, because benign lesions might coexist with unrecognized malignant areas.2,4 With this approach, the diagnosis can be definitively confirmed or refuted histopathologically. However, there is clearly a significant risk of unnecessary removal of a normal testis if no malignancy is actually detected. In addition, there are reports of organ-preserving procedures for benign disease by enucleation,2,7 in which follow-up revealed no evidence of recurrence.3 However, organ-preserving removal of a small (1 to 2 mm) cyst might be technically demanding, especially if the location is central.
Kratzik et al3 showed that a scrotal ultrasound surveillance strategy of simple intratesticular cysts was feasible. In their series of 15 cases of simple cysts, patients did not undergo surgery but were kept under close surveillance with high-frequency scrotal ultrasound. The surveillance strategy was extremely intensive and consisted of tumor markers and scrotal ultrasound every 4 weeks for the first 6 months, every 2 months until the end of the first year, every 3 months until the end of year 2, and then at 6-month intervals. In addition, they performed chest X-rays and retroperitoneum scrotal ultrasound at presentation. The preliminary report was encouraging: all 9 patients were sonographically free of detectable malignancy, and no patient had any change in appearance of the simple cyst by scrotal ultrasound. However, closer inspection of the data in this study revealed that the median follow-up surveillance was only 9 months (range, 6 to 21 months), and no follow-up reports from this series with long-term surveillance data have been published to date. In the study by Hamm et al,1 13 patients with simple intratesticular cysts were identified, of whom only 5 were followed up with scrotal ultrasound; the other 8 underwent surgical management. The patients undergoing surveillance had only one follow-up scrotal ultrasound examination at 1 to 6 months, and this showed no changes compared with the initial findings. In our study, although it is a retrospective analysis, we have shown that patients can be followed up successfully over 6 months with a less stringent scrotal ultrasound policy. Our patient did not required surgery for possible malignant transformation. This patient who requested follow-up, predominantly because of anxiety, was reassured with consistently normal scrotal ultrasound results.
Furthermore, the average age at presentation in most series is between 60 and 65 years (our average was 59 years), a population in whom germ cell malignancy is admittedly less common.6,9 Repeated ultrasound scanning, therefore, may not be justified.
It has been suggested that testicular cysts arise from remnants of Mullerian or Wolfian ducts, since such cysts have been reported in children.10 Other possible etiologies include trauma and inflammation, which can cause occlusion of the spermatic ducts with subsequent ectasia and cystic alterations in the rete testis.1 There was no history of trauma or inflammation in our patients and therefore the etiology of the cysts in these patients remains unclear.
We accept that our study, being a retrospective review, has limitations. Our main findings concerning simple intratesticular cysts are, however, consistent with the literature, in that the case was almost always accidentally discovered, was impalpable, and was not generally associated with symptoms. These cysts can very occasionally enlarge and cause pain, as shown by the lone example in our study. The patients did not require surgery for malignant transformation and most patients were reassured and discharged after repeat scanning.
ACKNOWLEDGEMENTS
This work was supported by a 2011 clinical research grant from Pusan National University Hospital.
References
- 1.Hamm B, Fobbe F, Loy V. Testicular cysts: differentiation with US and clinical findings. Radiology. 1988;168:19–23. doi: 10.1148/radiology.168.1.3289090. [DOI] [PubMed] [Google Scholar]
- 2.Khorsandi M, Lobby N, Harkaway RC, Ginsberg PC. Testicular cysts: management and literature review. J Am Osteopath Assoc. 1999;99:537–538. doi: 10.7556/jaoa.1999.99.10.537. [DOI] [PubMed] [Google Scholar]
- 3.Kratzik C, Hainz A, Kuber W, Donner G, Lunglmayr G, Frick J, et al. Surveillance strategy for intratesticular cysts: preliminary report. J Urol. 1990;143:313–315. doi: 10.1016/s0022-5347(17)39943-3. [DOI] [PubMed] [Google Scholar]
- 4.Höbarth K, Kratzik C. High resolution ultrasonography in the diagnosis of simple intratesticular cysts. Br J Urol. 1992;70:546–549. [PubMed] [Google Scholar]
- 5.Leung ML, Gooding GA, Williams RD. High-resolution sonography of scrotal contents in asymptomatic subjects. AJR Am J Roentgenol. 1984;143:161–164. doi: 10.2214/ajr.143.1.161. [DOI] [PubMed] [Google Scholar]
- 6.Gooding GA, Leonhardt W, Stein R. Testicular cysts: US findings. Radiology. 1987;163:537–538. doi: 10.1148/radiology.163.2.3550884. [DOI] [PubMed] [Google Scholar]
- 7.Dmochowski RR, Rudy DC, Weitzner S, Corriere JN., Jr Simple cyst of the testis. J Urol. 1989;142:1078–1081. doi: 10.1016/s0022-5347(17)38997-8. [DOI] [PubMed] [Google Scholar]
- 8.Rifkin M, Cochlin DL. Imaging of the Scrotum & Penis. 1st ed. New York: Martin Dunitz; 2002. pp. 33–94. [Google Scholar]
- 9.Shergill IS, Thwaini A, Kapasi F, Potluri BS, Barber C. Management of simple intratesticular cysts: a single-institution 11-year experience. Urology. 2006;67:1266–1268. doi: 10.1016/j.urology.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 10.García CJ, Zúñiga S, Rosenberg H, Arce JD, Zúñiga F. Simple intratesticular cysts in children: preoperative sonographic diagnosis and histological correlation. Pediatr Radiol. 1999;29:851–855. doi: 10.1007/s002470050712. [DOI] [PubMed] [Google Scholar]