Abstract
Background:
To investigate the relationship between certain maternal characteristic and infant birth weight and weight gain in puerperal women seen at a tertiary health centre.
Materials and Methods:
We measured the weight of 318, randomly selected infants after a complete physical examination at birth and at 6 weeks postnatal using standard procedures and related them to certain maternal characteristics.
Results:
There were 318 women and baby pairs. Maternal ages ranged from 16 to 42 years, with a mean of 25.6±1.3 years. Mean birth weight of babies was 3.10±1.89 kg; mean gestational age was 36±4.6 weeks, with 9.4% and 3.0% of babies born having low birth weight or Macrosomia respectively. Mothers from the North of the country, multiparity and systolic and/or diastolic hypertensions were factors associated with low birth weight. At 6 weeks, 27.1% of infants failed to gain weight as expected for their age. Similarly, 37.0% of infants born to mothers with some tertiary education showed slowed weight gain compared with those who had secondary (19.2%) or primary (14.7%) education, P=0.03. Maternal weight at delivery positively correlated with birth weight of the infant (r=0.357, P<0.001). However, maternal weight and blood pressure negatively correlated with infant weight gain at 6 weeks post-delivery.
Conclusion:
Our study demonstrates that certain maternal characteristics could play a role in the birth weight and early infant weight gain, and are preventable through simple public health approaches.
Keywords: Birth weight, infant, weight gain, Nigeria
INTRODUCTION
Birth weight plays an important role in infant survival, child development, and adult metabolic diseases.1–3 Maternal characteristics have been variously shown to impact on the progress and outcome of pregnancy, especially those related to birth weight and perinatal mortality.3–6 Such maternal factors like genetic endowment, socio-cultural, demographic, and medical conditions (e.g. hypertension, malaria, urinary tract infections, malnutrition and anaemia) are strongly associated with foetal complications especially low birth weight, prematurity and birth asphyxia all of which act individually or in concert with each other to increase neonatal and infant mortality.6–8 In Nigeria, most births are unattended to by a trained birth attendant occurring at home or in settings outside the hospital.9 Even the few that come to the hospital book very late with little or no window for effective intervention.9–11
On the other hand, not much is known about factors that affect infant weight gain in early infancy. Infant feeding is recognized as one of the most influential factors affecting weight gain. Reviews from various parts of the world have suggested a protective effect on cardiovascular diseases (CVD) risk profile from early initiation and prolonged breastfeeding2,12 In addition, limited evidence has shown that maternal characteristics such as postnatal depression and maternal eating habits influence infant weight gain and may predispose infants to weight faltering.13,14 On the other hand, infants who gain weight rapidly during early infancy especially the first 2 weeks of life are at increased risk of childhood obesity and adult metabolic disease.14,15 Stettler et al.,16 had demonstrated that excessive weight gain during the first week of life in healthy European American formula fed infants was associated with overweight 2-3 decades later. This observation they postulated may be related to the programming of the developing brain or the endocrine system of the young infant.16 Thus it is important that studies are done to examine the factors associated with infant weight gain with a view of modifying them so as to reduce the risk of developing cardiovascular disease, malnutrition and other metabolic diseases in later life.2,12
The aim of the present study is to identify the maternal predictive characteristics of birth weight and weight gain in early infancy with the aim of advocacy for policy change and behavioural changes towards attaining the MDG goals.
MATERIALS AND METHODS
This was a cross-sectional descriptive study, using the data collected in 24-months at the Jos University Teaching Hospital (JUTH) a tertiary care centre located in north central Nigeria. The subjects were puerperal married women selected based on a systematic random sampling technique (>16 years old), with gestational age determined by last menstrual period or antenatal ultrasound assessment. Characteristics of the newborns were also studied. Very low birth weight (VLBW) and extremely low birth weight (ELBW) babies were excluded because of their need for admission so as not to skew the results. Data was collected through interviews with the women and in the case of weight and anthropometry by measuring those using standard procedures. All women in the study exclusively breast fed their babies by 6 weeks postnatal. The study was approved by the Ethics Committee of the Jos University Teaching Hospital and all participants signed an informed consent form.
Statistical analysis
Statistical analysis was performed using the SPSS/PASW statistical package for Windows version 18.0. Mean and other summary statistics were calculated and presented in tables. Frequency and percentage distribution were used in the presentation of categorical data. Analysis of variance (ANOVA) were carried out to compare and determine differences in means where there are three or more groups, and Chi-square test done to determine whether there is any statistically significant difference between categorical groups of maternal characteristics. A linear regression model was used to determine the relationship between maternal weight at delivery and at six weeks post-partum and birth weight and infant weight gain at six weeks post-partum respectively. Ethnic group were combined to create three large geographical origins i.e. North, North Central and south, in addition, maternal socioeconomic class was determined using the method by Olusanya et al.17 Maternal hypertension was defined [Table 1] based on the JNC 7 criteria18 while Table 2 took into consideration isolated systolic or diastolic hypertension. A P value of <0.05 was considered statistically significant.
Table 1.
Frequency distribution and percentage of maternal and infant characteristics
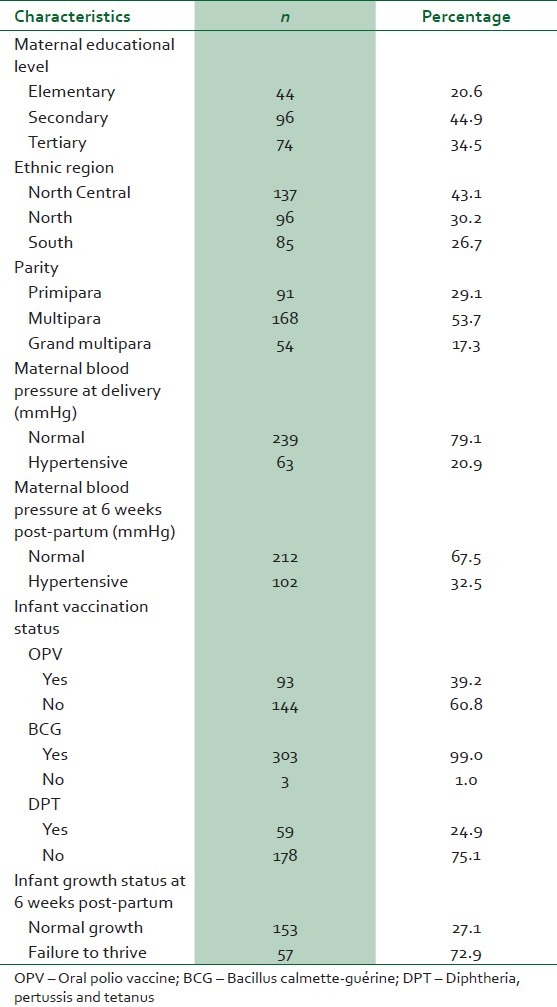
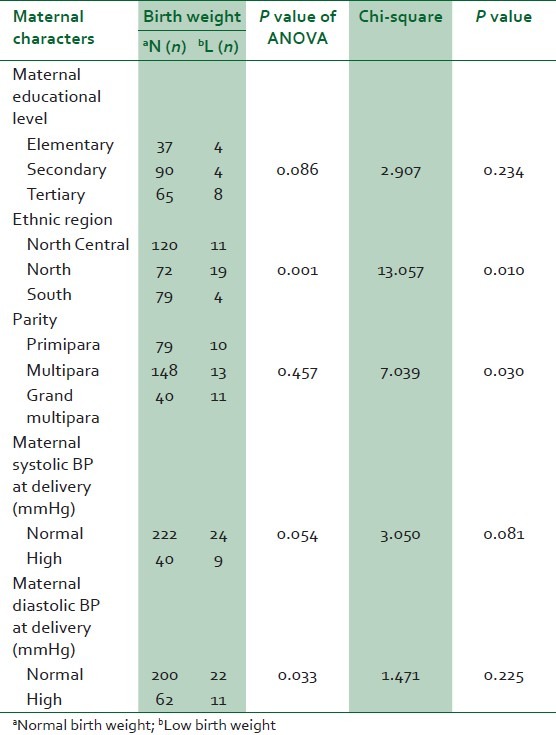
Table 2.
ANOVA test comparing the difference in mean birth weight as influenced by maternal characteristics; Chi-square test also shows association between maternal characteristics and birth weight
RESULTS
Descriptive
Maternal characteristics
A total of 318 women were interviewed; all women were 42 years old and under, with the youngest being 16 years old as at the time of this study [Table 3] and all women indicating that they are currently exclusively breast feeding and intend to do so for a minimum of 6 month. In terms of ethnic origin, one hundred and thirty seven (43.1%) of the mothers were from the North Central region of the country while 96 (30.2%) are from the northern part of the country and 85 (26.7%) are from the southern parts of the country. Majority of the mothers surveyed had at least secondary education (44.9%), followed by 44 (20.6%) with primary (elementary) and then 74 (34.5%) with tertiary education [Table 1].
Table 3.
Maternal and neonatal characteristics at birth and at 6 weeks post-partum
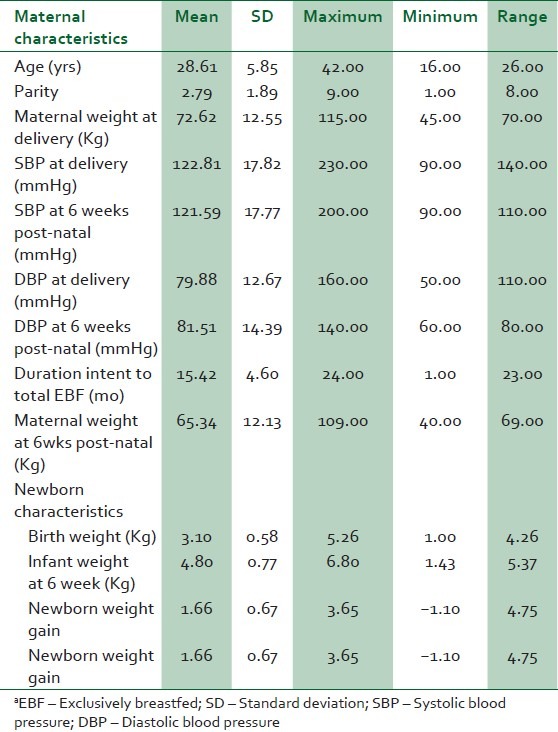
One hundred and sixty eight (53.7%) were multiparous, 96 (44.9%) were primiparous and 74 (34.5%) were grand multiparous women respectively. Sixty three (20.9%) had hypertension in pregnancy [Table 1].
Neonatal characteristics
The mean birth weight was 3.10±1.89 kg. The mean gestational age was 36±4.6 weeks. In all, 9.4% and 3.0% of babies were low birth weight or macrosomic respectively. Majority (99.0%) of the neonates has had Bacillus Calmette-Guérine (BCG) vaccine by the sixth week of life. However, less than half (39.2% and 24.9%) have had their first dose of oral polio vaccine (OPV) or diphtheria, pertussis and tetanus (DPT) vaccines. At 6 weeks, 79.2% of infants were gaining weight as expected for their age, while 27.1% had either lost weight or were not gaining weight adequately [Table 1].
Analytical statistics
To determine which of the maternal socio-demographic characteristic and health decisions affect birth weight and infant weight gain at 6 weeks post-partum and the difference in mean birth weight and infant weight gain at 6 weeks post-partum based on these maternal characteristics was determined using the ANOVA test; the results are displayed in Tables 2 and 4. Based on the ANOVA test carried out, there was a statistically significant difference in the mean birth weight of infants born to mothers from the different geographical category (P=0.001) with those infant born to mothers from the North more likely to have a low birth weight compared with the other two groups. The same result was replicated by the Chi-square analysis which showed that proportionately more infant born to mothers from the North had low birth weight compared to the other two groups (P=0.010). The Chi-square analysis also showed that proportionately more grand multiparous women had low birth babies (P=0.030). Mothers with a high systolic and/or diastolic blood pressures are more likely to have a low birth weight baby compared with those with normal blood pressures (P=0.054 and 0.033) respectively. With the Chi-Square for high maternal systolic blood pressure only showing a trend (P=0.081).
Table 4.
ANOVA test comparing the difference in mean infant weight gain at 6 weeks post-partum as influenced by maternal and other factors
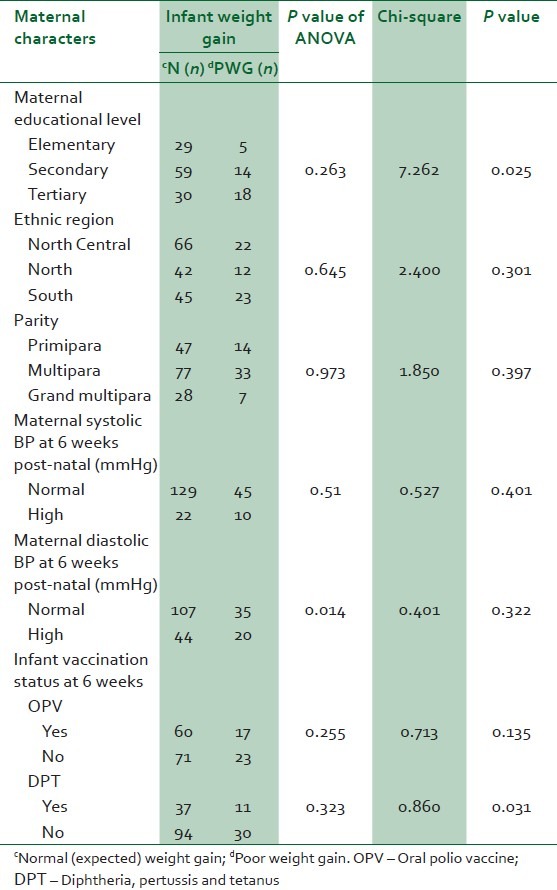
The infant weight gain at 6 weeks did show a reversal in how some of the maternal characteristics influenced birth weight. For example as shown in Table 2, proportionately more infant (37.5%) born to mothers with a tertiary education of some sort, showed evidence of slowed weight gain in the first 6 post-natal weeks of life, compared to those secondary education (19.2%) and primary education (14.7%) with P=0.025. While infants who have already had the DPT vaccination showed a modestly more likelihood to gain weight in the first 6 post-natal week of life compared to those who haven’t (P=0.031).
Using correlation statistics, we discovered that maternal weight at delivery positively correlated with birth weight of the infant (r=0.357, P<0.001) but the reverse is the case for infant weight gain at 6 weeks post-delivery (r=–0.188, P=0.01). When extended to infant weight gain and maternal weight at 6 weeks post-partum a similar negative correlation was observed (r=–0.163, P=0.019). In the same way, maternal blood pressure at delivery negatively correlates with birth weight with r=–0.175, P=0.002 and r= –0.0161, P=0.006 for systolic and diastolic blood pressures respectively. In the same way, maternal high systolic blood pressure was associated with decreased infant weigh gain by 6 weeks post-partum (r=0.185, P=0.011). Figures 1–4 represent some the other data in graphical form.
Figure 1.
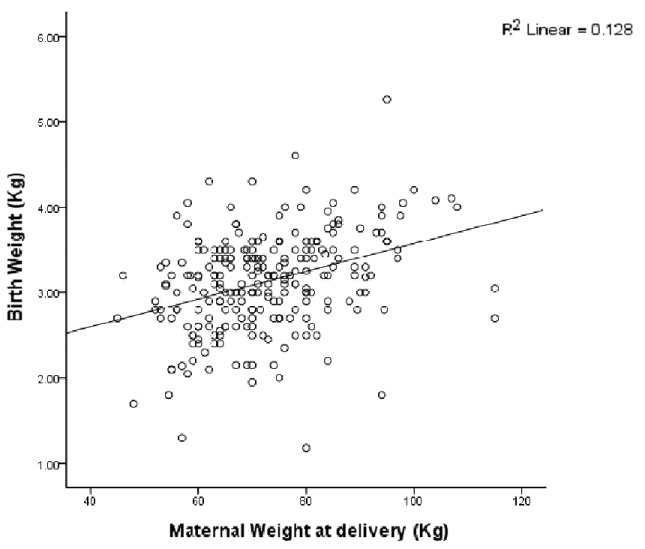
Linear relationship between maternal weight at delivery. It shows a positive correlation between maternal weight at delivery and birth weight of the baby
Figure 4.
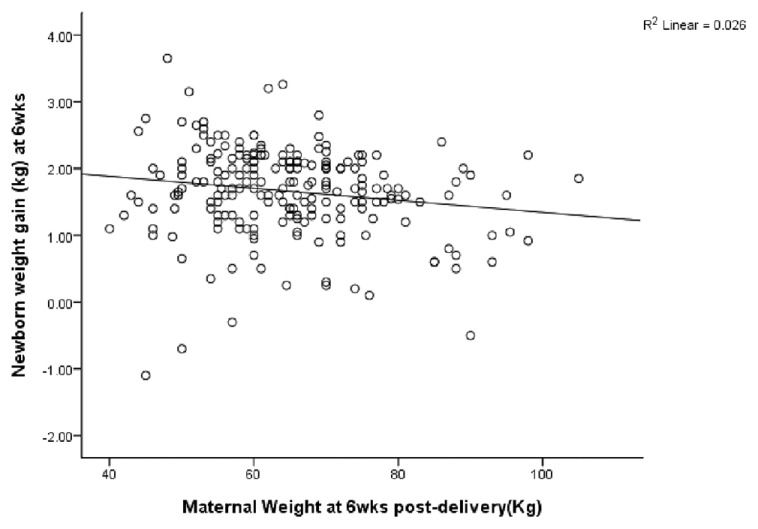
Maternal weight at 6 weeks post-partum negatively with infant weight gain
Figure 2.
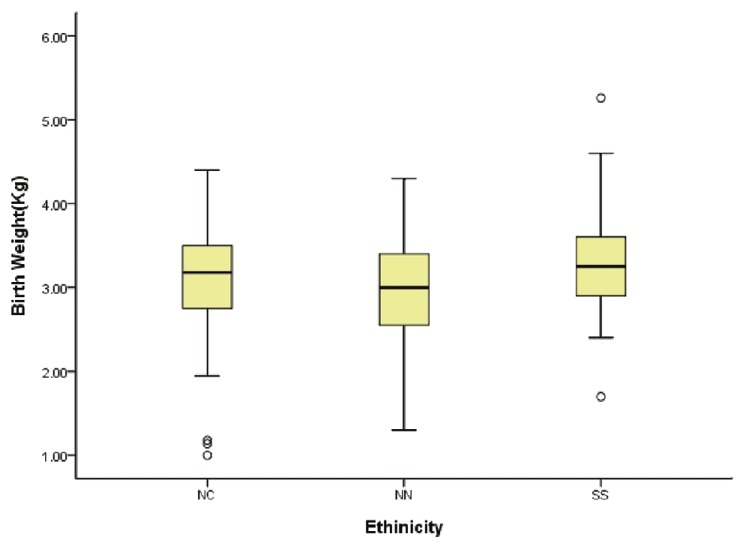
Birth weight variation with ethno-geographic origin of mother
Figure 3.
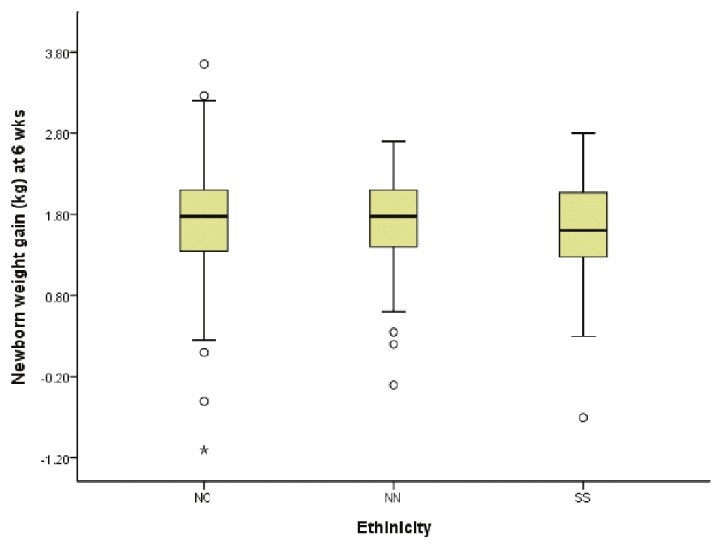
Relationship between newborn weight gain at 6 weeks postnatal and maternal ethno-geographic origin
It is worth noting that there was no significant relationship between maternal age categories or extremes of maternal age and mean infant birth weight or weight gain 6 weeks post-partum, duration of EBF or intent to EBF. Similarly there was no significant relationship between maternal socioeconomic class and mean infant birth weight or weight gain 6 weeks post-partum, duration of EBF or intent to EBF, although the mean of these factors tend to increase with increasing maternal socioeconomic class.
DISCUSSION
Birth weight is used as an indicator of individual and population health. It is one of the main determinants of perinatal and infant mortality and has strong associations with both child and adult health, being associated with childhood growth, cognition and disability.2
The prevalence of low birth weight in this study was found to be 9.4%. This is lower than 12.7% previously reported in 2003 in the same locality.8 It is also lower than what has been reported from other parts of the developing world.3–5,7 The improvement in the prevalence seen in this report may not be unconnected with the fact that health care delivery in Nigeria may be making some gains albeit slow but significant gains as reflected in the modest decrease in the neonatal and infant mortality figures reported in the 2009 National demographic health survey.19 On the other hand, it is also likely that this figures may not reflect the reality in the general population, considering that this study was carried out among a tertiary healthcare population which is not usually a true representation of the population of the country since only a few women access such care facilities in the country with majority of the population left un-catered for. But because of the heterogeneous population that use this facility, this result is a starting point. However, the fact that the infants of mothers from Northern Nigerian comprise the bulk of those with low birth weight is worrisome. Whether this is a result of genetic predisposition and/or interaction with socioeconomic and environmental factors is a subject for further research. However, low educational and economic status which have been well established to have a relationship with low birth weight4–8 are prevalent amongst women from this (Northern) part of the country.20
Though in this study the role of education and socioeconomic status in producing low birth weight was not investigated, most of the mothers who had low birth weight infants were observed to have 6 years or less of formal education. Karim et al.,21 found that birth weight increases with higher maternal education, while in Germany22 women with the lowest education had significantly elevated risk for small for gestational age newborns (SGA).
Similarly, that most of the infants with low birth weight were born to multiparous and grand multiparous women is not surprising. Yilgwan et al.,8 in a similar study had reported an association between multiparity and low birth weight. Elshibly and Schmalisch23 in Sudan had shown that as the birth order increases beyond the third pregnancy, the birth weight tends to drop especially if the spacing is poor. Besides, multiparity and higher number of births is a common feature seen in women of low socioeconomic status a factor associated with low birth weight.2–6
Studies have shown maternal hypertension has been associated with low birth weight,5 although we found no significant association between it and low birth weight in our study; with the mean birth weight being lower among normotensive women. This however contrast what was reported by Badshah et al.,24 in Peshawar Pakistan were they reported higher odds of having a low birth weight infant in mothers with hypertension. Maternal hypertension is thought to cause LBW by affecting placental blood flow thus limiting nutrient supply. Our findings suggest a possible multi-factorial cause of lower birth weight in our population with maternal hypertension as only one of many. However, seeing that our sample size is too small for us to answer this question, a much larger, prospective study design will be necessary for us to be able to answer this question.
With respect to infant weight gain, our study found higher maternal educational level to be significantly associated with poor weight gain. Though higher schooling is associated with better health behaviour,19,23 but because of the harsh economic realities in our country, most women are engaged in salaried profession with longer hours away from home and the baby thus exposing the infant to factors that could predispose to poor intake and hence low or inadequate weight gain. Thus there is a need for further studies to address the relationship between the length of maternal work hours and it relationship with early infant weight gain.
We also observed that DPT immunization status was significantly associated with adequate weight gain. The reason for this observation is not immediately clear especially since the first DPT immunization is received by 6 weeks; however, infant immunization status is usually related to maternal health seeking behaviour. Considering the time that the first DPT vaccine is given and the age of the infants studied, we could not explain why this relationship exists. This is because the first DPT dose is usually given at 6-8 weeks and the infants in our study were all around 6 weeks of age at the time of the study.
Other factors found to be associated with poor weight gain though not statistically significant were maternal systolic and diastolic hypertension. The exact mechanism is not known, but the fact that maternal illness affects child care is known and could adversely affect infant and child nutritional status and thus growth.19–21
CONCLUSION
We have demonstrated that certain maternal antenatal and postnatal characteristics could play a role in the birth weight and early infant weight gain. Our study showed a lower prevalence of low birth weight than previously reported. Although the small sample size and site of the study might not be a factor, the trend is undeniable, considering the diversity of the patients that use this healthcare facility. Also, maternal educational and social economic status along with perinatal health conditions influence the birth weight and weight gain in early infant life.
These factors are preventable; thus we recommend a strengthening of the universal basic education programme to help increase girl child education and thence maternal education with the aim of reducing the prevalence of LBW.
ACKNOWLEDGMENT
We thank the Resident doctors and Nursing staff of the labour ward and the post natal clinic for assistance with anthropometric data collection. This study was also partly funded through Part funding by NIH/NHLBI-R21HL092358s
Footnotes
Source of Support: Part Funding by NIH/NHLBI-R21HL092358s
Conflict of Interest: None declared.
REFERENCES
- 1.Power C, Li L. Cohort study of birthweight, mortality, and disability. Br Med J. 2000;320:840–1. doi: 10.1136/bmj.320.7238.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang RC, Burke V, Newnham JP, Stanley FJ, Kendall GE, Landau LI, et al. Perinatal and childhood origins of cardiovascular disease. Int J Obes. 2007;31:236–44. doi: 10.1038/sj.ijo.0803394. [DOI] [PubMed] [Google Scholar]
- 3.Lawoyin TO. Risk factors for infant mortality in a rural community in Nigeria. Perspect Public Health. 2001;121:114–7. doi: 10.1177/146642400112100213. [DOI] [PubMed] [Google Scholar]
- 4.Padilhal PD, Accioly PE, Chagas C, Portela E, Da Silva CL, Saunders C. Birth weight variation according to maternal characteristics and gestational weight gain in Brazilian women. Nutr Hosp. 2009;24:207–21. [PubMed] [Google Scholar]
- 5.Fairley L. Changing patterns of inequality in birth weight and its determinants: A population-based study, Scotland 1980-2000. Paediatr Perinat Epidemiol. 2005;19:342–51. doi: 10.1111/j.1365-3016.2005.00665.x. [DOI] [PubMed] [Google Scholar]
- 6.Grimmer I, Buhrer C, Dudenhausen JW, Stroux A, Reiher H, Halle H, et al. Preconceptional factors associated with very low birthweight delivery in East and West Berlin: A case control study. BMC Public Health. 2002;2:10. doi: 10.1186/1471-2458-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohanty C, Prasad R, Srikanth AR, Ghosh JK, Singh TB, Das BK. Maternal anthropometry as predictors of low birth weight. J Trop Pediatr. 2006;52:24–9. doi: 10.1093/tropej/fmi059. [DOI] [PubMed] [Google Scholar]
- 8.Yilgwan CS, Abok II, Yinnang WD, Vajime BA. Prevalence and risk factors of low birth weight in Jos. Jos J Med. 2009;4:12–5. [Google Scholar]
- 9.Etuk SJ, Ekanem AD. Socio-demographic and reproductive characteristics of women who default from orthodox obstetric care in Calabar, Nigeria. Int J Gynecol Obstet. 2001;73:57–60. doi: 10.1016/s0020-7292(00)00386-6. [DOI] [PubMed] [Google Scholar]
- 10.Etuk SJ, Asuquo EE. Maternal mortality following postpartum haemorrhage in Calabar - A six year review. West Afr J Med. 1997;16:165–9. [PubMed] [Google Scholar]
- 11.Udofia I, Okonofua F. Preventing primary postpartum haemorrhage in unskilled births in Africa. Afr J Reprod Health. 2008;12:7–9. [PubMed] [Google Scholar]
- 12.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: A quantitative review of published evidence. Pediatrics. 2005;115:1367–77. doi: 10.1542/peds.2004-1176. [DOI] [PubMed] [Google Scholar]
- 13.Wright CL, Parkinson KN, Drewett RF. The influence of maternal socioeconomic and emotional factors on infant weight gain and weight faltering (failure to thrive): Data from a prospective birth cohort. Arch Dis Child. 2006;91:312–7. doi: 10.1136/adc.2005.077750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villalpando S, Lopez-Alarco M. Growth faltering is prevented by breast-feeding in underprivileged infants from Mexico City. J Nutr. 2000;130:546–52. doi: 10.1093/jn/130.3.546. [DOI] [PubMed] [Google Scholar]
- 15.Singhal A, Fewtrell M, Cole TJ, Lucas A. Low nutrient intake and early growth for later insulin resistance in adolescents born preterm. Lancet. 2003;361:1089–97. doi: 10.1016/S0140-6736(03)12895-4. [DOI] [PubMed] [Google Scholar]
- 16.Stettler N, Stallings VA, Troxel AB, Zhao J, Schinnar R, Nelson SE, et al. Weight gain in the first week of life and overweight in adulthood: A cohort study of European American subjects fed infant formula. Circulation. 2005;111:1897–903. doi: 10.1161/01.CIR.0000161797.67671.A7. [DOI] [PubMed] [Google Scholar]
- 17.Olusanya O, Okpere E, Ezimokhai M. The importance of social class in voluntary fertility control in a developing country. West Afr J Med. 1985;4:205. [Google Scholar]
- 18. National High Blood Pressure Education Program Working Group on High Blood.
- 19.National Population Commission. Population and Housing Census. 2006;1:275–312. [Google Scholar]
- 20.Pressure in Children and Adolescents. The 7th report on the diagnosis, evaluation and treatment of high blood pressure. 2004 [PubMed] [Google Scholar]
- 21.Karim E, Mascie-Taylor CG. The association between birth weight, socio-demographic variables and maternal anthropometry in an urban sample from Dhaka, Bangladesh. Ann Hum Biol. 1997;24:387–401. doi: 10.1080/03014469700005152. [DOI] [PubMed] [Google Scholar]
- 22.Raum E, Arabin B, Schlaud M, Walter U, Schwartz FW. The impact of maternal education on intrauterine growth: A comparison of former West and East Germany. Int J Epidemiol. 2001;30:81–7. doi: 10.1093/ije/30.1.81. [DOI] [PubMed] [Google Scholar]
- 23.Elshibly EM, Schmalisch G. The effect of maternal anthropometric characteristics and social factors on gestational age and birth weight in Sudanese newborn infants. BMC Public Health. 2008;8:244–51. doi: 10.1186/1471-2458-8-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Badshah S, Mason L, McKelvie K, Payne R, Lisboa PJ. Risk factors for low birth weight in the public-hospitals at Peshawar, NWFP-Pakistan. BMC Public Health. 2008;8:197. doi: 10.1186/1471-2458-8-197. [DOI] [PMC free article] [PubMed] [Google Scholar]


