SUMMARY
Human papillomavirus (HPV) types 16 and 18 are causally related to a sub-set of oral cavity and oropharyngeal squamous cell cancers. However, a clear estimate of the prevalence of HPV-16/18 in oral cavity and oropharyngeal dysplasia (OOPD) is not available. This literature review and meta-analysis was conducted to provide a prevalence estimate for HPV-16/18 in OOPD. Twenty-two studies that reported prevalence of HPV-16 and/or 18 in 458 OOPD lesions were analyzed. Meta-analysis was used to evaluate the prevalence of HPV-16/18 and logistic regression was used for stratified analysis by age, gender, and histological grade. The overall prevalence of HPV-16/18 in OOPD lesions was 24.5% [95% confidence interval (CI), 16.4–36.7%)]. The individual prevalence for HPV-16 alone was 24.4%. The prevalence of HPV-16/18 in oral cavity lesions alone was 25.3% (95% CI, 14.2–45.2%). The odds of detection of HPV-16/18 in dysplastic lesions in males were twice that of females [odds ratio (OR), 2.44]. HPV-16/18 were 3 times more common in dysplastic lesions (OR, 3.29; 95% CI, 1.95–5.53%) and invasive cancers (OR, 3.43; 95% CI, 2.07–5.69%), when compared to normal biopsies. There was no significant difference in HPV-16/18 rates between dysplastic lesions and cancers or between mild, moderate or severe dysplastic lesions. This meta-analysis provides a quantification of the prevalence of HPV types 16/18 in OOPD lesions. These results also support the assumption that HPV-16/18 infection occurs during the early phase of the oral cavity and oropharyngeal carcinogenesis.
Keywords: Human papillomavirus, Oral epithelial dysplasia, Oral cancer, Oropharyngeal cancer, Oral precancerous lesion, Epithelial carcinogenesis, Meta-analysis, Prevalence
Introduction
Oral cavity and oropharyngeal squamous cell carcinoma (OOSCC) accounts for over 3% of all cancers, making it the sixth most common cancer worldwide.1 In 2010, the number of OOSCC-related deaths in the US was estimated to be 7880.2 Although the overall incidence of OOSCC has gradually decreased in the past few decades,2 the cancers arising from certain anatomical sub-sites have shown an increase, especially among younger individuals without typical risk factors such as tobacco or alcohol use.3,4 Human papillomavirus (HPV) is proposed as an etiologic risk factor for this sub-set of OOSCCs.5
While over 100 different types of HPV are known6, only about 15 types have been identified as ‘high-risk’ serotypes (HR-HPV) with oncogenic potential.7,8 Currently marketed vaccines offer protection against two HR-HPV types: HPV-16 and 18.9 HPV-16/18 are associated with about 70% of all cervical cancers and about 35% of OOSCCs.8,10,11 HPV-16/18 are also the most common (>90%) serotypes detected in the HPV-related OOSCCs.5,8,12 The successful implementation of prophylactic immunization for cervical cancer has led to discussions on immunizing for other HPV-related cancers including OOSCCs. However, unlike cervical carcinogenesis, the role of HPV-16/18 in the early oral cavity (OC) and oropharyngeal (OP) carcinogenic process has not been clearly defined. Also, while HPV-16/18 have been well established as risk factors for the cancers of OP sites,5,13–15 they are less strongly associated with the OC cancers. Establishing the timeline and likelihood of HPV-16/18 infection, in relation to early OC and OP carcinogenesis, may improve our understanding of its role and eventually aid in the planning of immunization strategies.
OC and OP squamous carcinogenesis involves sequential histological transformation of normal epithelium, to dysplasia, to in situ carcinoma, and finally to invasive cancer.16 While the prevalence of different HPV types in OOSCCs has been evaluated in detail,11,12 there is limited information on its prevalence in histopathologically confirmed dysplastic lesions. Previous studies that evaluated oral cavity and oropharyneal dysplasia (OOPD) have reported widely varying HPV prevalence ranging between 0% and 100%.17,18 Many of these studies were limited by small sample size. Therefore, a clear estimate of the prevalence of HPV types 16 and 18 in OOPD lesions is not available. We conducted this literature review and meta-analysis to provide an estimate of the prevalence of HPV-16/18 in OOPD.
Methods
Study selection
The PubMed, MEDLINE, and SCOPUS databases were used to perform a comprehensive literature search on HPV detection in OOPD. The search was limited to English language studies published between January 1985 and November 2010. The search was conducted using both MeSH terminology and more general search terms. Search terms included, but were not limited to: HPV, head and neck cancer, oral cancer, oropharyngeal cancer, intra-epithelial neoplasia, hyperplasia, dysplasia, leukoplakia, biopsy, polymerase chain reaction (PCR), and in situ hybridization (ISH). References cited in the identified research articles were also reviewed. Based on the preliminary review, 43 studies that reported HPV prevalence in head and neck squamous dysplastic lesions were identified.19–61 To be included in the final analysis the articles had to: (1) provide individual estimates for histopathologically confirmed dysplastic lesions, (2) differentiate dysplasia of OP and/or OC from other head and neck sites, and (3) provide type specific prevalence for HPV-16 and/or 18. Only 22 of the 43 articles met all the criteria and were used for this study.21,22,24,27–31,33–36,40,41,43,44,48,50,53,54,56,60 These articles were evaluated independently by two authors (E.H., V.J.) to identify relevant data points including: number and grade of dysplasia, HPV prevalence, anatomical location, sample type, detection technique and patient demographics. Only the numbers specific to HPV types 16 and 18 and for OC and OP sites were used for this analysis. Studies that did not differentiate between OC and OP lesions were not included for the stratified analysis on anatomical location.
Statistical analysis
The analysis was conducted in two steps. For the first step, the prevalence of HPV-16/18 and 95% confidence intervals (CI) were calculated for each study. Overall prevalence was defined as the number of OOPD samples that tested positive for HPV-16/18 divided by the total number of OOPD samples. The 95% CI were then calculated using the Wilson ‘score’ method with continuity correction.62 As a second step, meta-analysis was conducted to estimate the overall pooled prevalence of HPV-16/18 in OOPD. Sub-group analyses were conducted stratified by variables that are potential causes of heterogeneity among the studies. Sub-group meta-analyses were done to identify prevalence based on HPV serotype, detection technique, geographical location and the year of publication of the study. We explored the heterogeneity between study-specific results using the Q statistic at the significance level of p = 0.05. Estimates were obtained by both the fixed and random-effects models, and only random-effects model (REM) results were presented if significant heterogeneity was noted. The studies that reported HPV-16/18 prevalence of 0% or 100% were not included in the final meta-analysis. In order to make sure that the studies with prevalence of 0% or100% did not significantly change the overall estimates, we also repeated the meta-analysis by adjusting the estimates by ±1%. Only the results that excluded the studies with 0% or 100% are presented here. Stratified analysis was also conducted based on histological grade, anatomical location, patient age, and gender. However, several studies either did not report stratified data for these variables or reported only very small sample sizes; thereby making it difficult to obtain valid meta-analysis estimates. Therefore, for these variables, crude prevalence estimates and adjusted odds ratios (OR) were reported based on multiple logistic regression. STATA V.10 software was used for this analysis.
Results
The 22 studies together evaluated a total of 458 OOPDs. The number of samples per-study varied from 1 to 60 (Table 1). The detection rate of HPV-16 and/or 18 differed based on study and detection method.
Table 1.
Characteristics of 22 studies that evaluated HPV-16 and/or 18 in dysplastic oral or oropharyngeal lesions.
| Study | Year | Country | Number of samples (HPV positive/all dysplastic samples) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HPV-16/18b |
HPV-16 alone |
HPV-18 alone |
|||||||||
| ISH | SB/FB | PCR | ISH | SB/FB | PCR | ISH | SB/FB | PCR | |||
| Maitland et al.21 | 1987 | UK | – | 1/2 | – | – | – | – | – | – | – |
| Syrjanen et al.22 | 1988 | Finland | 3/21 | – | – | 2/21 | – | – | 1/21 | – | – |
| Greer et al.24 | 1990 | USA | 2/60 | – | – | 2/60 | – | – | 0/60 | – | – |
| Zeuss et al.27 | 1991 | USA | 0/15 | – | – | – | – | – | – | – | – |
| Young et al.28 | 1991 | USA | 0/3 | – | – | – | – | – | – | – | – |
| Shroyer et al.29 | 1991 | USA | 3/24 | 4/24 | – | – | 4/24 | – | – | – | |
| Holladay et al.30 | 1993 | USA | – | – | 6/27 | – | – | 6/27 | – | – | 0/27 |
| Cox et al.31 | 1993 | UK | – | 1/1 | – | – | 1/1 | – | – | – | – |
| Palefsky et al.33 | 1994 | USA | – | – | 9/13 | – | – | 9/13 | – | – | 1/13 |
| Fouret et al.34 | 1995 | France | – | – | 0/7 | – | – | 0/7 | – | – | 0/7 |
| Mao et al.35 | 1996 | USA | – | – | 2/5 | – | – | 2/5 | – | – | – |
| Fornatora et al.36 | 1996 | USA | 16/48 | – | – | – | – | – | – | – | – |
| Lo Muzio et al.40 | 1997 | Italy | 8/21 | – | – | – | – | – | – | – | – |
| Elamin et al.41 | 1998 | UK | – | – | 2/7 | – | – | 2/7 | – | – | – |
| Bouda et al.43 | 2000 | Greece | – | – | 5/5 | – | – | 3/5 | 4/5 | ||
| Ha et al.44 | 2002 | USA | – | – | 1/52 | – | – | 1/52 | – | – | – |
| Sugiyama et al.48 | 2003 | Japan | – | – | 31/51 | – | – | 31/51 | – | – | 0/51 |
| Begum et al.50 | 2005 | USA | 9/9 | – | – | 9/9 | – | – | – | – | – |
| Cunningham et al.53 | 2006 | USA | – | – | 5/41 | – | – | 5/41 | – | – | – |
| Bagan et al.54 | 2007 | Spain | – | – | 0/2 | – | – | 0/2 | 0/2 | ||
| Acay et al.56 | 2008 | Brazil | 4/30 | – | – | – | – | – | – | – | – |
| Angiero et al.60 | 2010 | Italy | – | – | 2/14a | – | – | – | – | – | – |
Abbreviations: ISH, in situ hybridization; SB/FB, Southern Blot / Filter blot; PCR, polymerase chain reaction.
Only moderate and severe dysplasia included.
HPV-16 alone or HPV-18 alone or both HPV-16/18.
Meta-analysis for overall prevalence based on HPV type
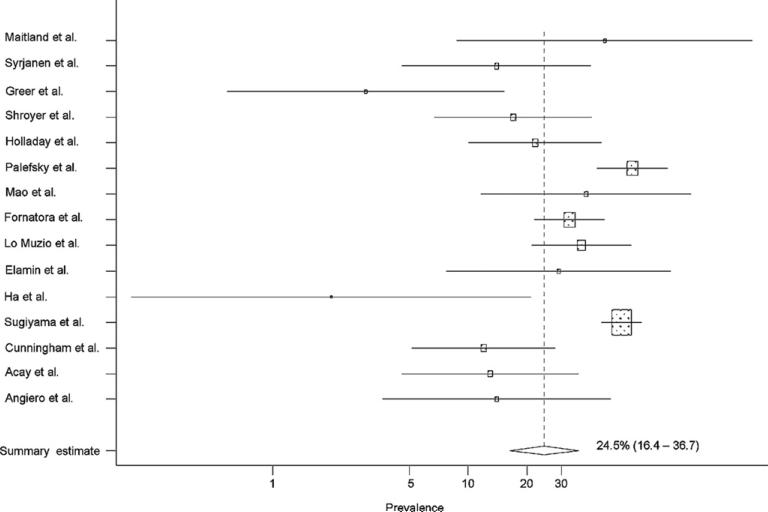
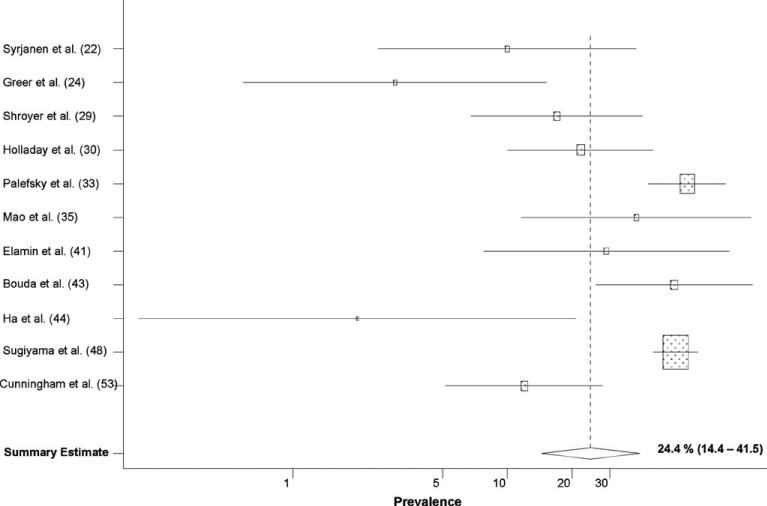
Eight studies reported the prevalence rate of both HPV-16 and 18 types, seven studies reported on HPV-16 alone and the other seven studies did not distinguish between HPV-16/18 (Table 1). Based on REM, the prevalence of either HPV-16/18 types in OOPD lesions was 24.5% [95% confidence interval (CI), 16.4–36.7%; Q = 59.2 (p-heterogeneity < 0.001)] (Fig. 1). The individual prevalence of HPV-16 in OOPDs was 24.4% [95% CI, 14.4–41.5%; Q = 49.8 (p-heterogeneity < 0.001)] (Fig. 2). Eight studies reported individual estimates for HPV-18, out of which only three studies reported a prevalence of >0%. Therefore, a separate estimate for HPV-18 is not presented.
Fig. 1.
Pooled prevalence of HPV-16/18 in all dysplastic lesions.  , summary estimate;
, summary estimate;  , random weight of each study;
, random weight of each study;  , 95% confidence interval.
, 95% confidence interval.
Fig. 2.
Pooled prevalence of HPV-16 alone in all dysplastic lesions.  , summary estimate;
, summary estimate;  , random weight of each study;
, random weight of each study;  , 95% confidence interval.
, 95% confidence interval.
Meta-analysis stratified by detection technique
Ten studies used PCR technique, eight used ISH, two used southern or filter blot, and the other two studies utilized both PCR and ISH (Table 1). Based on REM, the overall HPV-16/18 prevalence in OOPD was higher by PCR [26.8%; 95% CI, 15.7–45.8%; Q = 36.8 (p-heterogeneity < 0.001)] than by ISH technique [18.7%; 95% CI, 10.5–33.5%; Q = 13.8 (p-heterogeneity = 0.02)], but the difference was not statistically significant (p-value: 0.17).
Meta-analysis stratified by anatomical site
Only 15 of the 22 studies clearly differentiated OC dysplasia from OP dysplasia. Of these, 12 studies reported separate prevalence estimates for OC dysplastic lesions.21,22,27,31,34,36,40,41,43,48,53,54,56,60 One study did not provide location specific estimates for all lesions and was not included in the meta-analysis specific for OC.36 The OC dysplastic samples from the studies included 44 samples from oral tongue, 24 from floor of the mouth/ventral tongue, 53 from buccal gingiva/vestibule, 4 from hard palate, 14 from oral commissure/lip and another 47 samples from unspecified OC sites. Based on the REM, the overall prevalence of HPV-16/18 in OC dysplastic lesions was 25.3% [95% CI, 14.2–45.2%; Q = 27.6 (p-heterogeneity < 0.001)]. There was no significant difference in prevalence among the different OC sub-sites (p-value = 0.95). Only four studies reported individual prevalence estimates for OP dysplastic lesions, thus, separate meta-analysis was not feasible for this sub-group.34,36,50,53
Meta-analysis stratified by geographical location of the study
Overall, 9 studies were from Europe and 11 were from the United States (Table 1). The prevalence of HPV-16/18 in OOPD in European studies [28.9%; 95% CI, 18.7–44.8%; Q = 3.9 (p-value for heterogeneity = 0.41)] was higher than in the United States [20.3%; 95% CI, 10.8–38.2%; Q = 34.4 (p-value for heterogeneity = < 0.001)]; the difference was not statistically significant (p-value 0.18).
Meta-analysis stratified by the year of publication of the study
Ten studies were published up until 1995, and the remaining 12 studies were published in the years after 1995 (Table 1). Based on the random-effects model, the prevalence of HPV-16/18 in OOPD in the studies that were published after 1995 [25.7%; 95% CI, 15.6–42.3%; Q = 33.5 (p-heterogeneity < 0.001)] was slightly higher than the prevalence reported by studies published in or before 1995 [21.4%; 95% CI, 9.1–50.5%; Q = 25.1 (p-heterogeneity < 0.001)]; this difference was not statistically significant (p-value: 0.51).
Results based on age and gender
Only eight studies reported individual-level data on the age of the patients31,36,40,41,43,48,53,54 and nine studies reported on gender.27,31,36,40,41,43,48,53,54 The age distribution of 160 patients was available for analysis, of which 40% were less than 50 years of age. As shown in Table 2, the HPV-16/18 detection rate in OOPD was not significantly different between patients over and under 50 years of age (p-value: 0.16). The odds of detection of HPV-16/18 in OOPD lesions in males were twice that of females (OR 2.44; 95% CI, 1.26–4.74%; p-value: 0.008).
Table 2.
Odds of HPV-16/18 detection in oral dysplastic lesions, stratified by age and gender.
| Characteristic | Number of studies | Number of samples | Crude prevalence (%) | Adjusted odds ratioa | p-Value |
|---|---|---|---|---|---|
| Age group b | 8 | ||||
| <50 years | 66 | 39.1 | 1 | ||
| ≥50 years | 94 | 45.7 | 2.06 (0.76-5.62) | 0.16 | |
| Gender b | 9 | ||||
| Female | 75 | 29.3 | 1 | ||
| Male | 98 | 46.9 | 2.44 (1.26-4.74) | 0.008 |
Adjusted by study ID and type of diagnostic test.
Only dysplastic lesions.
Results based on histological grade of the lesion
Ten studies reported on HPV-16/18 prevalence in benign, dysplastic and OOSCC lesions in the same population.21,28–31,34,43,44,48,50,56 The odds of detection of HPV-16/18 was over 3 times greater in dysplastic lesions and invasive cancers, when compared with biopsies diagnosed as normal or benign keratosis (Table 3). However, there was no significant difference in HPV-16/18 rates between dysplastic lesions and OOSCC or between mild, moderate, or severe dysplastic lesions. Separate evaluation of hyperplastic lesions was not feasible because of the small number of lesions and heterogeneity of their clinical and histological description.
Table 3.
Odds of HPV-16/18 detection in oral cavity and oropharyngeal lesions, stratified by histologic grade.
| Characteristic | Number of studies | Number of samples | Crude prevalence (%) | Adjusted odds ratiob | p-Value for trend |
|---|---|---|---|---|---|
| Type of lesion | 10 | ||||
| Benigna | 207 | 14.0 | 1 | ||
| Squamous dysplasia | 204 | 30.4 | 3.29 (1.95–5.53) | <0.001 | |
| OOSCC | 241 | 30.7 | 3.43 (2.07–5.69) | ||
| Grade of dysplasia | 8 | ||||
| Mild dysplasia | 67 | 28.4 | 1 | ||
| Moderate dysplasia | 73 | 28.8 | 1.05 (0.50–2.23) | 0.92 | |
| Severe dysplasia | 50 | 26.0 | 0.95 (0.41–2.20) |
Includes normal and simple keratotic lesions.
Adjusted by study ID and type of diagnostic test.
Discussion
The hypothesis that viral infections may play a role in the development of OOSCCs is not new, having been proposed over three decades ago.63,64 This belief was further strengthened by three studies, published in the early 1980s, that reported the presence of HPV in OOSCCs and pre-malignant lesions.65–67 In spite of further evidence supporting these findings, the role of HPV in the development of OOSCC has remained controversial.23,68–76 However, in the past decade, several factors have led to a renewed interest in evaluating the role of HPV in the development of OOSCCs. First, technological advancements leading to more sensitive and broad-spectrum detection methodologies have facilitated more efficient and large-scale studies evaluating HPV prevalence.77 Second, the simultaneous increase in the rate of OOSCCs in non-users of tobacco and alcohol in the past three decades has led to increased efforts to identify the etiology of these cancers.78–80 Finally, the success of the prophylactic immunization campaign for cervical cancer has provided an opportunity for prevention, thereby instilling greater interest in preventable HPV-related cancers. Recent molecular and epidemiological studies have established an association between HPV and OOSCCs, specifically those arising from the OP.5,13–15 The current evidence is strong enough that the monographs of both the International Agency for Research on Cancer and the National Cancer Institute, USA, have listed HPV-16 as a risk factor for OP cancers.77,81 The prevalence of HPV in OOSCC is estimated to be between 23% and 46%; with the higher prevalence being noted in OP cancers.11,12,17 HPV-16 is the most common serotype reported in over 90% of these OOSCCs.82,83
Several studies have also evaluated HPV in clinically visible potentially malignant oral conditions, like leukoplakia and lichen planus.29,31,38,49,66,68 However, the prevalence in OOPD lesions has not been thoroughly evaluated. Some studies, based on small cohorts, have reported varying estimates for HPV in OOPD.21,22,24,27–31,33–36,40,41,43,44,48,53,54,56,60 Miller et al. in a comprehensive meta-analysis on OOSCCs and pre-malignant lesions, reported HPV (both low-risk and high-risk serotypes) prevalence of 22.2% in benign leukoplakia, 26.2% in intra-epithelial neoplasia and 46.5% in OOSCCs.17 HPV-16 and 18 were the most common high-risk serotypes and were detected in 30% of the OOSCC samples. All other high-risk types were noted in less than 1% of the cases. While Miller et al. provide the most detailed evaluation to-date of the prevalence of HPV in histopathologically diagnosed pre-malignant lesions of OC and OP, they failed to provide separate estimates for HR-HPV-16/18 in these lesions. Additionally, the study does not differentiate HPV prevalence in pre-malignant lesions in OP from those in OC. In the current meta-analysis of 458 OOPD lesions, we estimate that the prevalence of HPV-16/18 to be 24.5%. Because of the strict inclusion criteria for the current analysis, some studies listed in the Miller et al. report are not included in this meta-analysis. The current study, to our knowledge, is the first to provide prevalence estimates of the preventable HPV-16/18 types in OOPD lesions.
It is, however, important to consider the limitations of the current meta-analysis while interpreting these results. The current meta-analysis was limited to English language studies identified on PubMed, MEDLINE and SCOPUS. These criteria may have inadvertently introduced the possibility of language and publication bias. An inherent limitation of meta-analysis methodology is the possibility of heterogeneity of results due to dissimilarities between the individual studies. In the current study, the variability in the patient population, collection methodology, detection technique, diagnostic criteria, control selection, and anatomical location coding may have resulted in heterogeneity. We tried to address these issues by: (1) reporting REM estimates whenever significant heterogeneity was noted and (2) presenting results stratified by potential confounding and biasing factors. There was little or no information reported on sample selection criteria, collection methodology and on other potentially major confounders such as sexual habits, tobacco, and alcohol use; making adjustment for these factors or a stratified analysis unfeasible. In spite of these limitations, our results were consistent with previously published literature, thus supporting the validity of our study. For example, as previously mentioned, the prevalence of HR-HPV in dysplastic lesions was similar to the rate of HPV in intra-epithelial neoplasia reported by Miller et al..17 Also as expected, the stratified estimates show that the studies that used the more sensitive PCR technique reported a greater prevalence of HPV-16/18 in OOPD lesions (26.8%), compared to the ones that used the less sensitive ISH technique (18.7%). Additionally, HPV-16/18 was almost 2.5 times more common in OOPD in males than females. This is consistent with reports that HPV-positive OOSCCs are 3 times more common in men as compared to women.4,84
The presence of HPV-16/18 in one-fourth of OOPD lesions is consistent with the hypothesis that HPV plays a significant role in the early phase of OC and OP carcinogenesis. HPV infection can however be transient and HPV detection alone might not prove a causal association. Several studies have previously shown that HPV can be detected even in normal oral tissue.85–90 On the other hand, based on a review of 18 studies, Kreimer et al. estimated the prevalence of oral HR-HPV in healthy individuals to be 3.5%, only about 1.3% being HPV-16.91 This is a much lower prevalence than the estimates in OOPD lesions reported by the current study. It is also important to note that, in the current study, HPV-16/18 were over 3 times more common in OOPD and OOSCC lesions than in normal samples. This finding is consistent with other recent studies showing a significantly greater prevalence of HPV in oral pre-malignant and malignant lesions compared to normal tissue.17,92,93 While the greater prevalence in OOPD compared to normal samples suggests a role for HPV in the early carcinogenic process, it does not by itself directly imply a causal relationship. Further studies are needed to evaluate the significance of this upsurge in HPV-16/18 infection during the early carcinogenic process and its role in the progression of dysplastic tissues to invasive cancers.
Although this study included lesions from both OC and OP sites, only 15 of the 22 studies differentiated between biopsies from these two anatomical locations. Twelve of these studies evaluated only OC dysplasia, thereby limiting our ability to determine a clear estimate of HPV-16/18 prevalence for OP dysplasia alone. It is also possible that samples from the remaining 10 studies were also pre-dominantly from the OC. The reason may be that pre-malignant changes in the OP are hard to identify and biopsy as compared to OC sites. Therefore, it is possible that the restrictive inclusion criteria, including only histologically confirmed squamous dysplasia, inadvertently biases these results towards the lower OC prevalence. Despite this limitation, this is the first study to report a clear estimate of HPV-16/18 in dysplasia of the OC alone. Contrary to the opinion that HPV is a risk factor primarily for OP cancers, our results suggest the possibility that HPV-16/18 may play a role in the development of a sub-set of OC cancers also.
In summary, the current meta-analysis provides a quantification of the prevalence of HR-HPV-16/18 in OOPD lesions. This study also supports the hypothesis that HPV-16/18 infection may be a risk factor not only for OP cancers, but also in a sub-set of OC cancers. Understanding the process of HPV-related carcinogenesis is critical for the development of efficient HPV-targeted prevention strategies. This data on the prevalence of HPV-16/18 in OOPD lesions may be useful in the future to evaluate the effect of prophylactic vaccines in the prevention of carcinogenic HPV-16/18 infections. However, large and well-designed prospective studies are needed to confirm these results and to further understand the prognostic significance of HPV infection in oral dysplasia.
Abbreviations
- OOSCC
oral cavity and oropharyngeal squamous cell carcinoma
- HPV
human papillomavirus
- HR-HPV
high risk human papillomavirus
- OC
oral cavity
- OP
oropharynx
- OOPD
oral cavity and oropharyngeal dysplasia
- REM
random-effects model
- PCR
polymerase chain reaction
- ISH
in situ hybridization
- OR
odds ratio
- CI
confidence interval
Footnotes
Conflict of interest statement
The authors confirm the adherence to ethical policies of research and that there is no conflict of interest.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 3.Ryerson AB, Peters ES, Coughlin SS, Chen VW, Gillison ML, Reichman ME, et al. Burden of potentially human papillomavirus-associated cancers of the oropharynx and oral cavity in the US, 1998–2003. Cancer. 2008;113:2901–9. doi: 10.1002/cncr.23745. [DOI] [PubMed] [Google Scholar]
- 4.Chaturvedi AK, Engels EA, Anderson WF, Gillison ML. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26:612–9. doi: 10.1200/JCO.2007.14.1713. [DOI] [PubMed] [Google Scholar]
- 5.Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J. Natl Cancer Inst. 2000;92:709–20. doi: 10.1093/jnci/92.9.709. [DOI] [PubMed] [Google Scholar]
- 6.de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H. Classification of papillomaviruses. Virology. 2004;324:17–27. doi: 10.1016/j.virol.2004.03.033. [DOI] [PubMed] [Google Scholar]
- 7.Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118:3030–44. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- 8.Munoz N, Bosch FX, Castellsague X, Diaz M, de Sanjose S, Hammouda D, et al. Against which human papillomavirus types shall we vaccinate and screen? The international perspective. Int J Cancer. 2004;111:278–85. doi: 10.1002/ijc.20244. [DOI] [PubMed] [Google Scholar]
- 9.WHO Human papillomavirus vaccines: WHO position paper. Biologicals. 2009;37:338–4. doi: 10.1016/j.biologicals.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907. doi: 10.1016/S0140-6736(07)61416-0. [DOI] [PubMed] [Google Scholar]
- 11.Termine N, Panzarella V, Falaschini S, Russo A, Matranga D, Lo Muzio L, et al. HPV in oral squamous cell carcinoma vs head and neck squamous cell carcinoma biopsies: a meta-analysis (1988–2007). Ann Oncol. 2008;19:1681–90. doi: 10.1093/annonc/mdn372. [DOI] [PubMed] [Google Scholar]
- 12.Kreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14:467–75. doi: 10.1158/1055-9965.EPI-04-0551. [DOI] [PubMed] [Google Scholar]
- 13.Gillison ML. Human papillomavirus-associated head and neck cancer is a distinct epidemiologic, clinical, and molecular entity. Semin Oncol. 2004;31:744–54. doi: 10.1053/j.seminoncol.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 14.Smith EM, Ritchie JM, Summersgill KF, Hoffman HT, Wang DH, Haugen TH, et al. Human papillomavirus in oral exfoliated cells and risk of head and neck cancer. J Natl Cancer Inst. 2004;96:449–55. doi: 10.1093/jnci/djh074. [DOI] [PubMed] [Google Scholar]
- 15.D'Souza G, Fakhry C, Sugar EA, Seaberg EC, Weber K, Minkoff HL, et al. Six-month natural history of oral versus cervical human papillomavirus infection. Int J Cancer. 2007;121:143–50. doi: 10.1002/ijc.22667. [DOI] [PubMed] [Google Scholar]
- 16.Barnes L, Eveson J, Reichart P, Sidransky D. World Health Organization classification of tumors. IARC Press; Lyon: 2005. Pathology and Genetics of Head and Neck Tumors. [Google Scholar]
- 17.Miller CS, Johnstone BM. Human papillomavirus as a risk factor for oral squamous cell carcinoma: a meta-analysis, 1982–1997. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:622–35. doi: 10.1067/moe.2001.115392. [DOI] [PubMed] [Google Scholar]
- 18.Chaudhary AK, Singh M, Sundaram S, Mehrotra R. Role of human papillomavirus and its detection in potentially malignant and malignant head and neck lesions: updated review. Head Neck Oncol. 2009;1:22. doi: 10.1186/1758-3284-1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adler-Storthz K, Newland JR, Tessin BA, Yeudall WA, Shillitoe EJ. Human papillomavirus type 2 DNA in oral verrucous carcinoma. J Oral Pathol. 1986;15:472–5. doi: 10.1111/j.1600-0714.1986.tb00661.x. [DOI] [PubMed] [Google Scholar]
- 20.Lookingbill DP, Kreider JW, Howett MK, Olmstead PM, Conner GH. Human papillomavirus type 16 in bowenoid papulosis, intraoral papillomas, and squamous cell carcinoma of the tongue. Arch Dermatol. 1987;123:363–8. [PubMed] [Google Scholar]
- 21.Maitland NJ, Cox MF, Lynas C, Prime SS, Meanwell CA, Scully C. Detection of human papillomavirus DNA in biopsies of human oral tissue. Br J Cancer. 1987;56:245–50. doi: 10.1038/bjc.1987.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Syrjanen SM, Syrjanen KJ, Happonen RP. Human papillomavirus (HPV) DNA sequences in oral precancerous lesions and squamous cell carcinoma demonstrated by in situ hybridization. J Oral pathol. 1988;17:273–8. doi: 10.1111/j.1600-0714.1988.tb01536.x. [DOI] [PubMed] [Google Scholar]
- 23.Gassenmaier A, Hornstein OP. Presence of human papillomavirus DNA in benign and precancerous oral leukoplakias and squamous cell carcinomas. Dermatologica. 1988;176:224–33. doi: 10.1159/000248710. [DOI] [PubMed] [Google Scholar]
- 24.Greer RO, Jr, Eversole LR, Crosby LK. Detection of human papillomavirusgenomic DNA in oral epithelial dysplasias, oral smokeless tobacco-associated leukoplakias, and epithelial malignancies. J Oral Maxillofac Surg. 1990;48:1201–5. doi: 10.1016/0278-2391(90)90538-d. [DOI] [PubMed] [Google Scholar]
- 25.Kashima HK, Kutcher M, Kessis T, Levin LS, de Villiers EM, Shah K. Human papillomavirus in squamous cell carcinoma, leukoplakia, lichen planus, and clinically normal epithelium of the oral cavity. Ann Otol Rhinol Laryngol. 1990;99:55–61. doi: 10.1177/000348949009900110. [DOI] [PubMed] [Google Scholar]
- 26.Abdelsayed RA. Study of human papillomavirus in oral epithelial dysplasia and epidermoid carcinoma in the absence of tobacco and alcohol use. Oral Surg Oral Med Oral Pathol. 1991;71:730–2. doi: 10.1016/0030-4220(91)90283-i. [DOI] [PubMed] [Google Scholar]
- 27.Zeuss MS, Miller CS, White DK. In situ hybridization analysis of human papillomavirus DNA in oral mucosal lesions. Oral Surg Oral Med Oral Pathol. 1991;71:714–20. doi: 10.1016/0030-4220(91)90280-p. [DOI] [PubMed] [Google Scholar]
- 28.Young SK, Min KW. In situ DNA hybridization analysis of oral papillomas, leukoplakias, and carcinomas for human papillomavirus. Oral Surg Oral Med Oral Pathol. 1991;71:726–9. doi: 10.1016/0030-4220(91)90282-h. [DOI] [PubMed] [Google Scholar]
- 29.Shroyer KR, Greer RO., Jr Detection of human papillomavirus DNA by in situ DNA hybridization and polymerase chain reaction in premalignant and malignant oral lesions. Oral Surg Oral Med Oral Pathol. 1991;71:708–13. doi: 10.1016/0030-4220(91)90279-l. [DOI] [PubMed] [Google Scholar]
- 30.Holladay EB, Gerald WL. Viral gene detection in oral neoplasms using the polymerase chain reaction. Am J Clin Pathol. 1993;100:36–40. doi: 10.1093/ajcp/100.1.36. [DOI] [PubMed] [Google Scholar]
- 31.Cox M, Maitland N, Scully C. Human herpes simplex-1 and papillomavirus type 16 homologous DNA sequences in normal, potentially malignant and malignant oral mucosa. Eur J Cancer. 1993;29B:215–9. doi: 10.1016/0964-1955(93)90025-a. [DOI] [PubMed] [Google Scholar]
- 32.Donofrio V, Lo Muzio L, Mignogna MD, Troncone G, Staibano S, Boscaino A, et al. Prognostic evaluation of HPV-associated precancerous and microinvasive carcinoma of the oral cavity: combined use of nucleolar organiser regions (AgNOR) and proliferating cell nuclear antigen (PCNA). Eur J Cancer. 1995;31B:174–80. doi: 10.1016/0964-1955(95)00003-z. [DOI] [PubMed] [Google Scholar]
- 33.Palefsky JM, Silverman S, Jr, Abdel-Salaam M, Daniels TE, Greenspan JS. Association between proliferative verrucous leukoplakia and infection with human papillomavirus type 16. J Oral Pathol Med. 1995;24:193–7. doi: 10.1111/j.1600-0714.1995.tb01165.x. [DOI] [PubMed] [Google Scholar]
- 34.Fouret P, Martin F, Flahault A, Saint-Guily JL. Human papillomavirus infection in the malignant and premalignant head and neck epithelium. Diagn Mol Pathol. 1995;4:122–7. doi: 10.1097/00019606-199506000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Mao EJ, Oda D, Haigh WG, Beckmann AM. Loss of the adenomatous polyposis coli gene and human papillomavirus infection in oral carcinogenesis. Eur J Cancer. 1996;32B:260–3. doi: 10.1016/0964-1955(96)00008-5. [DOI] [PubMed] [Google Scholar]
- 36.Fornatora M, Jones AC, Kerpel S, Freedman P. Human papillomavirus-associated oral epithelial dysplasia (koilocytic dysplasia): an entity of unknown biologic potential. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:47–56. doi: 10.1016/s1079-2104(96)80377-5. [DOI] [PubMed] [Google Scholar]
- 37.Mao EJ, Schwartz SM, Daling JR, Oda D, Tickman L, Beckmann AM. Human papilloma viruses and p53 mutations in normal pre-malignant and malignant oral epithelia. Int J Cancer. 1996;69:152–8. doi: 10.1002/(SICI)1097-0215(19960422)69:2<152::AID-IJC15>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 38.Nielsen H, Norrild B, Vedtofte P, Praetorius F, Reibel J, Holmstrup P. Human papillomavirus in oral premalignant lesions. Eur J Cancer. 1996;32B:264–70. doi: 10.1016/0964-1955(96)00011-5. [DOI] [PubMed] [Google Scholar]
- 39.Wen S, Tsuji T, Li X, Mizugaki Y, Hayatsu Y, Shinozaki F. Detection and analysis of human papillomavirus 16 and 18 homologous DNA sequences in oral lesions. Anticancer Res. 1997;17:307–11. [PubMed] [Google Scholar]
- 40.Lo Muzio L, Mignogna MD, Staibano S, de Vico G, Salvatore G, Damiano S, et al. Morphometric study of nucleolar organiser regions (AgNOR) in HPV-associated precancerous lesions and microinvasive carcinoma of the oral cavity. Oral Oncol. 1997;33:247–59. doi: 10.1016/s0964-1955(97)00003-1. [DOI] [PubMed] [Google Scholar]
- 41.Elamin F, Steingrimsdottir H, Wanakulasuriya S, Johnson N, Tavassoli M. Prevalence of human papillomavirus infection in premalignant and malignant lesions of the oral cavity in U.K. subjects: a novel method of detection. Oral Oncol. 1998;34:191–7. doi: 10.1016/s1368-8375(97)00081-x. [DOI] [PubMed] [Google Scholar]
- 42.Matzow T, Boysen M, Kalantari M, Johansson B, Hagmar B. Low detection rate of HPV in oral and laryngeal carcinomas. Acta Oncol. 1998;37:73–6. doi: 10.1080/028418698423203. [DOI] [PubMed] [Google Scholar]
- 43.Bouda M, Gorgoulis VG, Kastrinakis NG, Giannoudis A, Tsoli E, Danassi-Afentaki D, et al. “High risk” HPV types are frequently detected in potentially malignant and malignant oral lesions, but not in normal oral mucosa. Mod Pathol. 2000;13:644–53. doi: 10.1038/modpathol.3880113. [DOI] [PubMed] [Google Scholar]
- 44.Ha PK, Pai SI, Westra WH, Gillison ML, Tong BC, Sidransky D, et al. Real-time quantitative PCR demonstrates low prevalence of human papillomavirus type 16 in premalignant and malignant lesions of the oral cavity. Clin Cancer Res. 2002;8:1203–9. [PubMed] [Google Scholar]
- 45.Giovannelli L, Campisi G, Lama A, Giambalvo O, Osborn J, Margiotta V, et al. Human papillomavirus DNA in oral mucosal lesions. J Infect Dis. 2002;185:833–6. doi: 10.1086/339193. [DOI] [PubMed] [Google Scholar]
- 46.Regezi JA, Dekker NP, Ramos DM, Li X, Macabeo-Ong M, Jordan RC. Proliferation and invasion factors in HIV-associated dysplastic and nondysplastic oral warts and in oral squamous cell carcinoma: an immunohistochemical and RT-PCR evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:724–31. doi: 10.1067/moe.2002.129760. [DOI] [PubMed] [Google Scholar]
- 47.Ostwald C, Rutsatz K, Schweder J, Schmidt W, Gundlach K, Barten M. Human papillomavirus 6/11, 16 and 18 in oral carcinomas and benign oral lesions. Med Microbiol Immunol. 2003;192:145–8. doi: 10.1007/s00430-002-0161-y. [DOI] [PubMed] [Google Scholar]
- 48.Sugiyama M, Bhawal UK, Dohmen T, Ono S, Miyauchi M, Ishikawa T. Detection of human papillomavirus-16 and HPV-18 DNA in normal, dysplastic, and malignant oral epithelium. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:594–600. doi: 10.1067/moe.2003.36. [DOI] [PubMed] [Google Scholar]
- 49.Campisi G, Giovannelli L, Arico P, Lama A, Di Liberto C, Ammatuna P, et al. HPV DNA in clinically different variants of oral leukoplakia and lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:705–11. doi: 10.1016/j.tripleo.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 50.Begum S, Cao D, Gillison M, Zahurak M, Westra WH. Tissue distribution of human papillomavirus 16 DNA integration in patients with tonsillar carcinoma. Clinical Cancer Res. 2005;11:5694–9. doi: 10.1158/1078-0432.CCR-05-0587. [an official journal of the American Association for Cancer Research].
- 51.Simionescu C, Margaritescu C, Georgescu CV, Surpateanu M. HPV and p53 expression in dysplastic lesions and squamous carcinomas of the oral mucosa. Rom J Morphol Embryol. 2005;46:155–9. [PubMed] [Google Scholar]
- 52.Cianfriglia F, Di Gregorio DA, Cianfriglia C, Marandino F, Perrone Donnorso R, Vocaturo A. Incidence of human papillomavirus infection in oral leukoplakia. Indications for a viral aetiology. J Exp Clin Cancer Res. 2006;25:21–8. [PubMed] [Google Scholar]
- 53.Cunningham LL, Jr, Pagano GM, Li M, Tandon R, Holm SW, White DK, et al. Overexpression of p16INK4 is a reliable marker of human papillomavirus-induced oral high-grade squamous dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:77–81. doi: 10.1016/j.tripleo.2005.11.028. [DOI] [PubMed] [Google Scholar]
- 54.Bagan JV, Jimenez Y, Murillo J, Gavalda C, Poveda R, Scully C, et al. Lack of association between proliferative verrucous leukoplakia and human papillomavirus infection. J Oral Maxillofac Surg. 2007;65:46–9. doi: 10.1016/j.joms.2005.12.066. [DOI] [PubMed] [Google Scholar]
- 55.Zarei MR, Moradie A, Hamkar R, Mohammadalizadeh S, Chamani G, Alizadeh N, et al. Detection of human papillomavirus DNA sequnces in oral lesions using polymerase chain reaction. Acta Medica Iranica. 2007;45:177–82. [Google Scholar]
- 56.Acay R, Rezende N, Fontes A, Aburad A, Nunes F, Sousa S. Human papillomavirus as a risk factor in oral carcinogenesis: a study using in situ hybridization with signal amplification. Oral Microbiol Immunol. 2008;23:271–4. doi: 10.1111/j.1399-302X.2007.00422.x. [DOI] [PubMed] [Google Scholar]
- 57.Llamas-Martinez S, Esparza-Gomez G, Campo-Trapero J, Cancela-Rodriguez P, Bascones-Martinez A, Moreno-Lopez LA, et al. Genotypic determination by PCR-RFLP of human papillomavirus in normal oral mucosa, oral leukoplakia and oral squamous cell carcinoma samples in Madrid (Spain). Anticancer Res. 2008;28:3733–41. [PubMed] [Google Scholar]
- 58.Debanth S, Singh PA, Mehrotra R, Singh M, Gupta SC, Pandya S, et al. Human papillomavirus infection and premalignant lesions of the oral cavity: a cross-sectional study in Allahabad, North India. Asia–Pacific J Clin Oncol. 2009;5:111–8. [Google Scholar]
- 59.Yang SW, Lee YS, Chen TA, Wu CJ, Tsai CN. Human papillomavirus in oral leukoplakia is no prognostic indicator of malignant transformation. Cancer Epidemiol. 2009;33:118–22. doi: 10.1016/j.canep.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 60.Angiero F, Gatta LB, Seramondi R, Berenzi A, Benetti A, Magistro S, et al. Frequency and role of HPV in the progression of epithelial dysplasia to oral cancer. Anticancer Res. 2010;30:3435–40. [PubMed] [Google Scholar]
- 61.Jalouli J, Ibrahim SO, Sapkota D, Jalouli MM, Vasstrand EN, Hirsch JM, et al. Presence of human papilloma virus, herpes simplex virus and Epstein-Barr virus DNA in oral biopsies from Sudanese patients with regard to toombak use. J Oral Pathol Med. 2010;39:599–604. doi: 10.1111/j.1600-0714.2010.00910.x. [DOI] [PubMed] [Google Scholar]
- 62.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–72. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 63.Newell GR, Krementz ET, Roberts JD. Excess occurrence of cancer of the oral cavity, lung, and bladder following cancer of the cervix. Cancer. 1975;36:2155–8. doi: 10.1002/cncr.2820360933. [DOI] [PubMed] [Google Scholar]
- 64.zur Hausen H. Human papillomaviruses and their possible role in squamous cell carcinomas. Curr Top Microbiol Immunol. 1977;78:1–30. doi: 10.1007/978-3-642-66800-5_1. [DOI] [PubMed] [Google Scholar]
- 65.Syrjanen K, Syrjanen S, Lamberg M, Pyrhonen S, Nuutinen J. Morphological and immunohistochemical evidence suggesting human papillomavirus (HPV) involvement in oral squamous cell carcinogenesis. Int J Oral Surg. 1983;12:418–24. doi: 10.1016/s0300-9785(83)80033-7. [DOI] [PubMed] [Google Scholar]
- 66.Loning T, Ikenberg H, Becker J, Gissmann L, Hoepfer I, zur Hausen H. Analysis of oral papillomas, leukoplakias, and invasive carcinomas for human papillomavirus type related DNA. J Invest Dermatol. 1985;84:417–20. doi: 10.1111/1523-1747.ep12265517. [DOI] [PubMed] [Google Scholar]
- 67.de Villiers EM, Weidauer H, Otto H, zur Hausen H. Papillomavirus DNA in human tongue carcinomas. Int J Cancer (Journal International du Cancer) 1985;36:575–8. doi: 10.1002/ijc.2910360510. [DOI] [PubMed] [Google Scholar]
- 68.Balaram P, Nalinakumari KR, Abraham E, Balan A, Hareendran NK, Bernard HU, et al. Human papillomaviruses in 91 oral cancers from Indian betel quid chewers–high prevalence and multiplicity of infections. Int J Cancer (Journal International du Cancer) 1995;61:450–4. doi: 10.1002/ijc.2910610403. [DOI] [PubMed] [Google Scholar]
- 69.Anderson JA, Irish JC, McLachlin CM, Ngan BY. H-ras oncogene mutation and human papillomavirus infection in oral carcinomas. Arch Otolaryngol Head Neck Surg. 1994;120:755–60. doi: 10.1001/archotol.1994.01880310059011. [DOI] [PubMed] [Google Scholar]
- 70.Brandwein M, Zeitlin J, Nuovo GJ, MacConnell P, Bodian C, Urken M, et al. HPV detection using “hot start” polymerase chain reaction in patients with oral cancer: a clinicopathological study of 64 patients. Modern Pathol. 1994;7:720–7. [(an official journal of the United States and Canadian Academy of Pathology, Inc.].
- 71.Chang KW, Chang CS, Lai KS, Chou MJ, Choo KB. High prevalence of human papillomavirus infection and possible association with betel quid chewing and smoking in oral epidermoid carcinomas in Taiwan. J Med Virol. 1989;28:57–61. doi: 10.1002/jmv.1890280113. [DOI] [PubMed] [Google Scholar]
- 72.Cruz IB, Snijders PJ, Steenbergen RD, Meijer CJ, Snow GB, Walboomers JM, et al. Age-dependence of human papillomavirus DNA presence in oral squamous cell carcinomas. Eur J Cancer B Oral Oncol. 1996;32B:55–62. doi: 10.1016/0964-1955(95)00060-7. [DOI] [PubMed] [Google Scholar]
- 73.Honig JF, Becker HJ, Brinck U, Korabiowska M. Detection of human papillomavirus DNA sequences in leucocytes: a new approach to identify hematological markers of HPV infection in patients with oral SCC. Bull Group Int Rech Sci Stomatol Odontol. 1995;38:25–31. [PubMed] [Google Scholar]
- 74.Maden C, Beckmann AM, Thomas DB, McKnight B, Sherman KJ, Ashley RL, et al. Human papillomaviruses, herpes simplex viruses, and the risk of oral cancer in men. Am J Epidemiol. 1992;135:1093–102. doi: 10.1093/oxfordjournals.aje.a116209. [DOI] [PubMed] [Google Scholar]
- 75.Min BM, Baek JH, Shin KH, Gujuluva CN, Cherrick HM, Park NH. Inactivation of the p53 gene by either mutation or HPV infection is extremely frequent in human oral squamous cell carcinoma cell lines. Eur J Cancer B Oral Oncol. 1994;30B:338–45. doi: 10.1016/0964-1955(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 76.Watts SL, Brewer EE, Fry TL. Human papillomavirus DNA types in squamous cell carcinomas of the head and neck. Oral Surg Oral Med Oral Pathol. 1991;71:701–7. doi: 10.1016/0030-4220(91)90278-k. [DOI] [PubMed] [Google Scholar]
- 77.Adelstein DJ, Ridge JA, Gillison ML, Chaturvedi AK, D'Souza G, Gravitt PE, et al. Head and neck squamous cell cancer and the human papillomavirus: summary of a National Cancer Institute State of the Science Meeting, November 9–10, 2008, Washington, DC. Head Neck. 2009;31:1393–422. doi: 10.1002/hed.21269. [DOI] [PubMed] [Google Scholar]
- 78.Frisch M, Hjalgrim H, Jaeger AB, Biggar RJ. Changing patterns of tonsillar squamous cell carcinoma in the United States. Cancer Causes Control: CCC. 2000;11:489–95. doi: 10.1023/a:1008918223334. [DOI] [PubMed] [Google Scholar]
- 79.Shiboski CH, Schmidt BL, Jordan RC. Tongue and tonsil carcinoma: increasing trends in the U.S. population ages 20–44 years. Cancer. 2005;103:1843–9. doi: 10.1002/cncr.20998. [DOI] [PubMed] [Google Scholar]
- 80.Hammarstedt L, Lindquist D, Dahlstrand H, Romanitan M, Dahlgren LO, Joneberg J, et al. Human papillomavirus as a risk factor for the increase in incidence of tonsillar cancer. Int J Cancer (Journal International du Cancer) 2006;119:2620–3. doi: 10.1002/ijc.22177. [DOI] [PubMed] [Google Scholar]
- 81.IARC monographs on the evaluation of carcinogenic risks in humans. Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 2007;90:1–636. [PMC free article] [PubMed] [Google Scholar]
- 82.Kreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14:467–75. doi: 10.1158/1055-9965.EPI-04-0551. [a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology].
- 83.D'Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356:1944–56. doi: 10.1056/NEJMoa065497. [DOI] [PubMed] [Google Scholar]
- 84.Vidal L, Gillison ML. Human papillomavirus in HNSCC: recognition of a distinct disease type. Hematol/Oncol Clin North Am. 2008;22:1125–42. vii. doi: 10.1016/j.hoc.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 85.Canadas MP, Bosch FX, Junquera ML, Ejarque M, Font R, Ordonez E, et al. Concordance of prevalence of human papillomavirus DNA in anogenital and oral infections in a high-risk population. J Clin Microbiol. 2004;42:1330–2. doi: 10.1128/JCM.42.3.1330-1332.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.D'Souza G, Agrawal Y, Halpern J, Bodison S, Gillison ML. Oral sexual behaviors associated with prevalent oral human papillomavirus infection. J Infect Dis. 2009;199:1263–9. doi: 10.1086/597755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kreimer AR, Alberg AJ, Daniel R, Gravitt PE, Viscidi R, Garrett ES, et al. Oral human papillomavirus infection in adults is associated with sexual behavior and HIV serostatus. J Infect Dis. 2004;189:686–98. doi: 10.1086/381504. [DOI] [PubMed] [Google Scholar]
- 88.Kurose K, Terai M, Soedarsono N, Rabello D, Nakajima Y, Burk RD, et al. Low prevalence of HPV infection and its natural history in normal oral mucosa among volunteers on Miyako Island, Japan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:91–6. doi: 10.1016/j.tripleo.2003.12.029. [DOI] [PubMed] [Google Scholar]
- 89.Smith EM, Ritchie JM, Yankowitz J, Wang D, Turek LP, Haugen TH. HPV prevalence and concordance in the cervix and oral cavity of pregnant women. Infect Dis Obstet Gynecol. 2004;12:45–56. doi: 10.1080/10647440400009896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am J Epidemiol. 2003;157:218–26. doi: 10.1093/aje/kwf180. [DOI] [PubMed] [Google Scholar]
- 91.Kreimer AR, Bhatia RK, Messeguer AL, Gonzalez P, Herrero R, Giuliano AR. Oral human papillomavirus in healthy individuals: a systematic review of the literature. Sex Transm Dis. 2010;37:386–91. doi: 10.1097/OLQ.0b013e3181c94a3b. [DOI] [PubMed] [Google Scholar]
- 92.Dodson TB. The frequency of human papilloma virus (HPV) is higher in premalignant and malignant oral mucosal lesions than normal mucosa. J Evid Based Dent Pract. 2010;10:174–5. doi: 10.1016/j.jebdp.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 93.Szarka K, Tar I, Feher E, Gall T, Kis A, Toth ED, et al. Progressive increase of human papillomavirus carriage rates in potentially malignant and malignant oral disorders with increasing malignant potential. Oral Microbiol Immunol. 2009;24:314–8. doi: 10.1111/j.1399-302X.2009.00516.x. [DOI] [PubMed] [Google Scholar]