Abstract
Background
The current study examined rates of comorbidity among children’s symptoms of posttraumatic stress (PTS) and depression after a natural disaster, Hurricane Ike. We also compared children with comorbid symptoms to children without comorbid symptoms, examining recovery, severity of symptoms, and risk factors.
Method
Children (n=277; 52% girls; 38% Hispanic, 28% White, 19% Black; grades 2–4) were assessed at 8 and 15 months postdisaster. Children completed measures of PTS and depressive symptoms at both time points and measures of exposure and recovery stressors at 8 months postdisaster.
Results
At 8 months postdisaster, 13% of children reported elevated PTS-only, 11% depression-only, and 10% comorbid symptoms of PTS and depression. At 15 months postdisaster, 7% of children reported elevated PTS-only, 11% depression-only, and 7% comorbid symptoms of PTS and depression. Children with comorbid symptoms of PTS and depression had poorer recovery, more severe symptoms, and they reported greater exposure and recovery stressors.
Limitations
We lacked information on children’s predisaster functioning and diagnostic interview of psychological distress symptoms.
Conclusions
Children with comorbid symptoms need to be identified early postdisaster. Levels of stressors should be monitored postdisaster, as highly stressed youth have difficulties recovering and may need help. Interventions should be tailored for children with comorbid symptoms of PTS and depression.
Keywords: Posttraumatic stress, Depression, Children, Disasters, Stressors
1. Introduction
Hurricanes and other disasters occur commonly around the world, affecting millions of youth annually (Seballos et al., 2011). Youth may be particularly vulnerable to the effects of disasters (Norris et al., 2010), and many children who are exposed to disasters report significant psychological distress symptoms, which can interfere with their functioning (Gurwitch et al., 2002; Kar and Bastia, 2006; La Greca et al., 2010; La Greca et al., 1996). In particular, symptoms of posttraumatic stress (PTS) have been widely reported in youth postdisaster (Furr et al., 2010). An increasing number of studies have begun to examine youths’ postdisaster depressive symptoms (Pina et al., 2008; Scheeringa and Zeanah, 2008) and have found that symptoms of PTS and depression are often comorbid (Eksi and Braun, 2009; Fan et al., 2011; Goenjian et al., 2001; Roussos et al., 2005). However, this comorbidity remains poorly understood.
Understanding children’s comorbid PTS and depressive symptoms is crucial for informing postdisaster mental health intervention efforts. Children with comorbid symptoms may be a high-risk group postdisaster, as the presence of comorbid disorders, even at subclinical levels, might influence recovery and recurrence of psychological distress (Richards, 2011). Identifying high-risk children is particularly important postdisaster, because resources available for postdisaster psychological interventions are limited (Jaycox et al., 2010). Further, information about comorbid symptoms can elucidate how psychopathology develops postdisaster (Angold et al., 1999). Thus, in the context of a destructive natural disaster, Hurricane Ike, we examined several issues including the occurrence and comorbidity of children’s PTS and depressive symptoms, recovery and severity of symptoms over time, and disaster-related risk factors associated with comorbid symptoms.
As our first aim, we examined rates of comorbidity at two time points (8 and 15 months) after a destructive hurricane. Based on existing evidence, it is not clear whether symptoms of PTS and depression are comorbid among children (i.e., preadolescents) postdisaster; it is also unclear these symptoms are comorbid after a disaster that is highly destructive, but involves little loss of life. These issues were addressed in the present study.
The majority of studies examining comorbid PTS and depressive symptoms in youth have focused on adolescents (Fan et al., 2011; Goenjian et al., 2009), even though preadolescents may display more severe PTS reactions postdisaster than older youth (Weems et al., 2010; Yelland et al., 2010). Also, postdisaster studies examining PTS and depressive symptoms have focused on disasters that involved substantial loss of life, such as earthquakes (Ekşi et al., 2007; Fan et al., 2011; Goenjian et al., 1995), supercyclones (Kar and Bastia, 2006), or terrorist attacks (Brown and Goodman, 2005). In fact, in those studies, loss of life was associated with both PTS and depressive symptoms in youth (Dell’Osso et al., 2011; Ekşi et al., 2007; Furr et al., 2010).
In evaluating children’s PTS and depressive symptoms (and their comorbidity), an important consideration was the postdisaster time frame. Our initial evaluation occurred eight months after Hurricane Ike, well into the disaster recovery period (Silverman and La Greca, 2002). Children’s PTS symptoms decrease significantly over the first six to seven months postdisaster (La Greca et al., 1996, 1998; see Bonanno Brewin et al., 2010 for a review), but appear more chronic by seven to nine months postdisaster (La Greca et al., 2010). We also assessed children’s symptoms at a second time-point, 15 months postdisaster. This prospective design enabled us to evaluate whether comorbid PTS and depressive symptoms were related to poorer recovery and more severe symptoms over time, and to evaluate the interplay of PTS and depressive symptoms over time.
Prospective studies of youths’ postdisaster reactions are rare (Furr et al., 2010); we could identify only two studies that evaluated youth’s PTS and depressive symptoms at multiple time points within the first year and a half postdisaster (Felix et al., 2011; Thienkrua et al., 2006). Neither of these studies evaluated the comorbidity of children’s PTS and depressive symptoms. Specifically, Thienkrua et al., 2006 assessed 371 Thai children (7–14 years), two months after the 2004 Asian Tsunami. Children affected by the tsunami and displaced from their homes (n=167) were compared to those who were affected but not displaced (n=99), and those who were neither affected nor displaced (n=105). The prevalence of clinically significant PTS was higher for the affected/displaced children (13%) than for those from unaffected villages (6%), although rates of depression did not differ across the groups (11% for affected/displaced, 5% for affected, and 8% for unaffected children). Most of the affected/displaced children were reassessed 9 months postdisaster and their rates of clinically significant PTS and depressive symptoms (10% and 12%, respectively) did not decline over time. Felix et al. (2011) followed a large sample of Puerto Rican youth 18 and 30 months after Hurricane Georges (1998). At 18 months, disaster exposure was associated with the prevalence of internalizing disorders among children (4–10 years) and depression among youth (4–17 years), although rates of disorder were low overall (<1% for PTSD, <4% for depression). While important, these studies did not evaluate the comorbidity of PTS and depressive symptoms, nor did they track comorbidity over time.
Thus, to extend the above work, our second study aim was to evaluate the comorbidity of children’s PTS and depressive symptoms during the first year and a half postdisaster. We examined whether comorbid elevations in PTS and depressive symptoms were associated with poorer recovery and more severe psychological symptoms over time than when either occurred alone. We also evaluated whether initial PTS contributed to subsequent depressive symptoms. These issues have not been examined prospectively in children postdisaster. However, based on work with adolescents (Fan et al., 2011; Fernando et al., 2010; Goenjian et al., 2011) and adults (North et al., 2004), one might expect poorer outcomes for children with comorbid PTS and depression. One might also expect that clinically significant PTS symptoms precede and lead to significant secondary depressive symptoms; this has been proposed by a number of researchers (Bolton et al., 2000; Karakaya et al., 2006), as the presence of PTS may interfere with youths’ engagement in activities, which could lead to depression over time (Goenjian et al., 2011).
Our third aim was to identify risk factors associated with comorbid symptoms. This information is needed for early identification of children at risk for developing comorbid symptoms. As noted above, postdisaster prospective studies have not examined comorbidity between PTS and depression. Therefore, it is unknown whether levels of risk factors may differ among children with comorbid symptoms and children with symptoms of PTS-only or depression-only. In this study, we examined several risk factors: disaster exposure (e.g., actual and perceived life threat), and stressors occurring during the disaster recovery period, which included immediate and ongoing loss/disruption (e.g., loss of home or possessions), and other stressful life events (e.g., parental separation, death in the family; see La Greca et al., 1996, 2010 and Vernberg et al., 1996 for the conceptual model underlying the risk factors).
Research evaluating risk factors for children’s postdisaster reactions has predominantly focused on PTS symptoms. Consistent with conceptual models, these studies generally demonstrate that disaster exposure variables, and especially perceived life threat, are important predictors of children’s PTS reactions (Blaze and Shwalb, 2009; La Greca et al., 2010; Weems et al., 2007; see Furr et al., 2010). In addition, stressors occurring during the disaster recovery period also have been identified as important risk factors for children’s persistent PTS symptoms (Comer et al., 2010; Fernando et al., 2010; La Greca et al., 2010). Despite the importance of these studies, the relationship between risk factors and comorbid PTS and depressive symptoms has not been considered.
Considerably less research has examined risk factors associated with children’s depressive symptoms postdisaster. Studies, conducted almost exclusively with adolescents, suggest that recovery stressors such as loss of family members, restrictions on travel, property damage, and financial difficulties, are associated with youths’ depressive symptoms postdisaster (Ekşi et al., 2007; Fernando et al., 2010; Giannopoulou et al., 2006; Goenjian et al., 2011; Kolaitis et al., 2003; Wickrama and Kaspar, 2007). Outside the context of natural disasters, evidence links both stressful life events and personal loss with depressive symptoms in youth (Brent et al., 2009; Rudolph and Flynn, 2007).
None of the above studies examined the relationship between various stressors and comorbid PTS and depressive symptoms, which was our third study aim. Overall, we expected that children with comorbid symptoms at Time 1 (8 months postdisaster) would report the highest levels of risk factors, when compared with children with symptoms of PTS-only, depression-only, or no elevated symptoms. Based on the literature reviewed above, we also expected that children with elevated PTS would report higher perceptions of life threat than children with no elevated PTS. Further, we expected that children with elevated depressive symptoms would report more stressors occurring during the postdisaster recovery period reflecting loss (of people, possessions) than children without elevated depressive symptoms.
The current study focused on children from Galveston, Texas. Galveston was in the direct path of Hurricane Ike, which hit Galveston in September 2008, taking 103 lives (Berg, 2008). Ike, a category 2 hurricane, is considered to be one of the most costly hurricanes in U.S. history (Blake, Landsea, & Gibney, 2011).
2. Method
2.1. Participants
Participants were 277 children (52% girls) recruited during the spring of 2009 from all six elementary schools in the Galveston Independent School District (GISD). Two schools were so badly damaged by Hurricane Ike that their buildings were closed for the entire year after the storm; students attending these schools “shared” facilities with two other elementary schools that were habitable.
Children were assessed at 8 months (Time 1, May 2009) and 15 months (Time 2, December 2009) postdisaster. At Time 1, 328 children (ages 7–11 years; M=8.70, SD=.95) were evaluated. Children were ethnically/racially diverse (38% Hispanic, 28% White, 19% Black, 11% Other, 4% Asian). Attrition at Time 2 was 16% (n=51). Only children who participated at both time points (n=277) were included in the current study. Children who participated at both time points did not differ from children who only participated at Time 1 on any demographic variables (age, gender, ethnicity) or on their initial PTS and depressive symptom levels.
2.2. Procedures
The Institutional Review Boards for the University of Miami, University of Texas Medical Branch, and GISD approved this study. Consent forms were distributed to students (Grades 2–4; n=1594), and 31% (n=494) returned consent forms to their teachers. Of forms returned, parental consent was obtained for 340 students (69%). Nine children were absent during testing and three children declined to participate. Prior to Time 2, parents of children who participated in Time 1 were re-contacted to remind them of their child’s participation in the study. The primary reason for attrition at Time 2 was moving out of the school district (n=43; 13%), which may have been hurricane-related. Further, five children (2%) were absent during testing and three children (1%) declined to participate.
For both time points, testing occurred in participating schools’ cafeteria, auditorium, or designated classrooms. Children were assessed in groups of 25 to 40 students. Six to eight research assistants and two study investigators were present to oversee testing and assist children. All questions were read aloud to children.
2.3. Measures
At Time 1, children completed all measures listed below. At Time 2, children reported PTS and depressive symptoms.
Demographics
Children reported their age, gender (1=Female, 0=Male), and race/ethnicity (1=Minority, 0=Caucasian).
Hurricane Exposure and Hurricane-Related Stressors
The Hurricane Related Traumatic Experiences-Revised (HURTE-R; La Greca et al., 2010; Vernberg et al., 1996) assessed hurricane stressors. One item (Yes/No) assessed perceived life threat (i.e., thinking you might die). Six items (Yes/No) assessed actual life threatening events (e.g., windows breaking in your home) and were summed (possible scores ranging from 0–6).
Ten items (Yes/No) reflecting immediate loss/disruption (e.g., moving to a new home) were summed (possible scores ranging from 0–10). Six items (Yes/No) related to ongoing loss/disruption (e.g., changing schools, homes) were summed (possible scores ranging from 0 to 6). The HURTE-R has been used with youth postdisaster (La Greca et al., 2010; Weems et al., 2010).
Major Life Events
A 14-item (Yes/No) version of the Life Events Checklist (LEC; Johnson & McCutcheon, 1980) assessed stressful major life events (e.g., parental divorce, family illness). Items were summed (possible scores ranging from 0 to 14). The LEC has been used in disaster research (La Greca et al., 2010), and shows adequate test-retest reliability (.72 in Greenberg et al., 1983).
Symptoms of Posttraumatic Stress Disorder
The Posttraumatic Stress Disorder-Reaction Index, Revision 1 (PTSD-RI-R; Steinberg et al., 2004) assessed children’s PTS symptoms over the past month. Eighteen items (rated 0=none of the time, to 4=most of the time) assessed 17 PTS disorder symptoms. Items were summed (possible scores ranging from 0 to 68). A cutoff score of 38 or greater was used to indicate clinically significant symptoms (Rodriguez et al., 2001; Steinberg et al., 2004). The PTSD-RI-R has adequate internal consistency (.83 in La Greca et al., 2010;.88 in Vernberg et al., 1996). Internal consistency in this study was. 88 (Time 1) and.88 (Time 2).
Depressive symptoms
Depressive symptoms were assessed with the Children’s Depression Inventory (CDI; Kovacs, 1981), which contains 27 items (children choose statements describing their symptoms over the past two-weeks, scored 0–2). One suicidality item was removed due to IRB concerns. Items were summed (possible scores ranging from 0 to 52). A cutoff score of 19 was used to indicate clinically significant depression (Cole et al., 1998). The CDI has been widely used and has good internal consistency (.91 in Cole et al., 1998). Internal consistency in this study was .83 (Time 1) and.87 (Time 2).
Comorbidity between PTS and depressive symptoms
Children were categorized into four clinical symptom groups: Group 1 met cutoffs for PTS and depression; Group 2 met cutoffs for PTSonly; Group 3 met cutoffs for depression-only; and Group 4 did not meet cutoffs for PTS or depression.
3. Results
3.1. Preliminary analyses
Descriptive statistics
Means and frequencies for study variables were examined. Regarding hurricane exposure, 35% of children reported perceived life threat and 53% reported at least one actual life-threatening event (M=.80). The most common event was seeing someone be badly hurt during the hurricane, reported by 27%. Most children (79%) reported that they evacuated during the hurricane. In terms of immediate loss/disruption, 92% reported at least one such event (M=3.49); the most common event was homes damaged or destroyed, reported by 53%. Regarding ongoing loss/disruption, 75% reported at least one such event (M=1.51); the most common event was having to move, reported by 35%. Finally, 71% reported at least one major life event since the hurricane (M=1.65); the most frequently reported event was change in a parent’s job, reported by 23%.
Mean levels of PTS symptoms were M=24.21 (Time 1) and M=19.18 (Time 2); these scores reflect moderate and mild levels of PTS symptom severity, respectively (using PTSD-RI-R criteria; Steinberg et al., 2004). Mean levels of depressive symptoms were M=11.90 (Time 1) and M=11.05 (Time 2), which are comparable to other postdisaster studies (e.g., M=11.23, 6 months post-earthquake among 4th–6th graders; Kolaitis et al., 2003).
Child characteristics
We evaluated whether child demographics (age, gender, ethnicity) were related to the probability of falling into elevated clinical symptom groups (i.e., Groups 1–3; Table 1). Age and minority status were not related to elevated clinical symptom groups at Time 1 or Time 2. Girls were more likely to fall in the PTS-only group at Time 1, x2(2)=6.91, p=.03, but no gender differences were found at Time 2.
Table 1.
Demographic characteristics and distribution of clinical symptom groups at Time 1 and Time 2.
| n (% of the sample) | Demographic Characteristics | ||
|---|---|---|---|
| Full Sample | Time 1 (n=275; 100%)a | M age=8.70 years; 52% female; 72% minority | |
| Time 2 (n=277; 100%) | M age=9.31 years; 52% female; 72% minority | ||
| Clinical Symptom Groups | Group 1: PTS & Depression | Time 1 (n=27; 10%) | M age=8.80 years; 44% female; 82% minority |
| Time 2 (n=18; 7%) | M age=9.28 years; 50% female; 89% minority | ||
| Group 2: PTS-Only | Time 1 (n=35; 13%) | M age=8.40 years; 74% female; 89% minority | |
| Time 2 (n=19; 7%) | M age=9.05 years; 74% female; 90% minority | ||
| Group 3: Depression-Only | Time 1 (n=29; 11%) | M age=8.57 years; 48% female; 90% minority | |
| Time 2 (n=31; 11%) | M age=8.90 years; 52% female; 81% minority | ||
| Group 4: No PTS or Depression | Time 1 (n=184; 67%) | M age=8.78 years; 50% female; 65% minority | |
| Time 2 (n=209; 76%) | M age=9.40 years; 50% female, 68% minority |
Two children from the full sample (n=277) did not complete the Time 1 measures of PTS symptoms (PTSD-RI-R) and depressive symptoms (CDI).
3.2. Aim 1: Comorbidity rates
Comorbid PTS and depressive symptoms were reported by 10% of children at Time 1, and 7% at Time 2 (Table 1). At Time 1, among children reporting clinically significant PTS (23% of the sample), almost half (43%) also reported clinically significant depressive symptoms. Among children reporting clinically significant depressive symptoms (21% of the sample), almost half (48%) also reported comorbid clinically significant PTS.
At Time 2, among the children reporting clinically significant PTS (14% of the sample), 50% also reported clinically significant depressive symptoms, whereas among children reporting clinically significant depressive symptoms (18% of the sample), 39% also reported clinically significant PTS. PTS and depressive symptoms significantly correlated at Times 1 and 2 (r=.57, p<.01 and r=.61, p<.01, respectively).
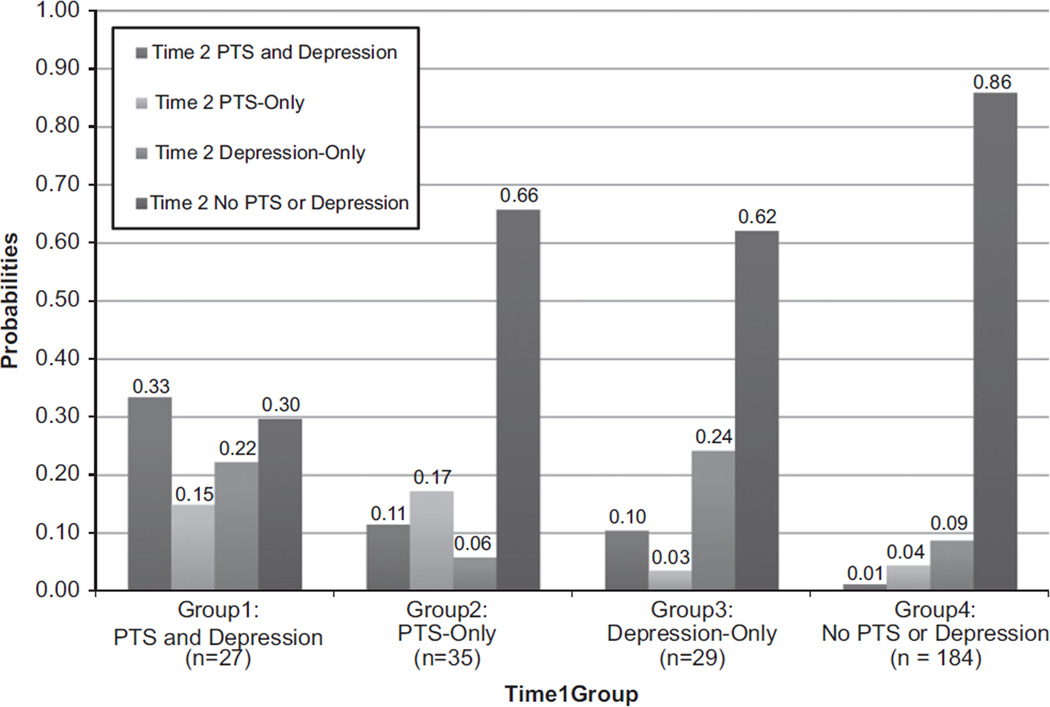
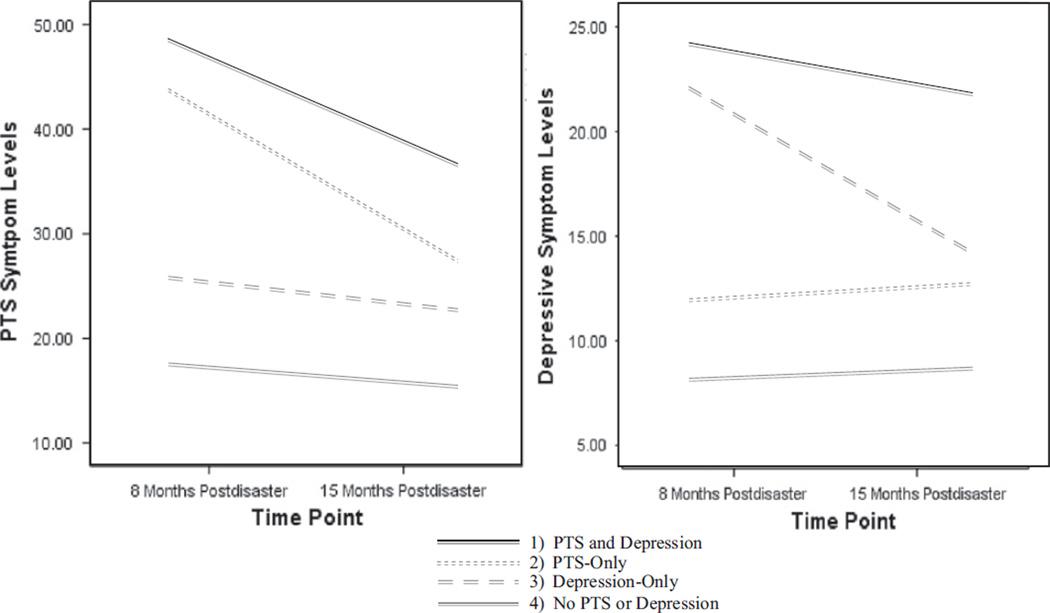
3.3. Aim 2: Comorbidity over time
We examined whether comorbidity at Time 1 contributed to poorer recovery at Time 2 (Fig. 1). Thirty-three percent of children with comorbid symptoms at Time 1 continued to report comorbid symptoms at Time 2. Further, only 30% of children with comorbid symptoms at Time 1 recovered (i.e., did not report elevated symptoms of PTS or depression) by Time 2. In comparison, 66% of children with PTS-only (Group 2) and 62% with depression-only (Group 3) recovered by Time 2. Thus, children with PTS-only and depression-only were 2.2 and 2.1 times more likely to recover than children with comorbid symptoms, respectively. Repeated measures ANOVAs revealed significant time by clinical symptom group interactions for PTS, F(3, 271)=18.13, p<.001, and depression, F(3, 271)=14.53, p<.001. The comorbidity group recovered more slowly than the PTS-only and depression-only groups (Fig. 2).
Figure 1.
Changes in children’s clinically significant symptom levels from Time 1 to Time 2.
Figure 2.
PTS and depressive symptoms levels over time by Time 1 clinical symptom groups.
Next, we examined whether children with comorbid symptoms reported more severe symptoms. ANOVAs (Table 2) and post-hoc analyses (Ryan procedure; Howell, 2007) revealed that children with comorbid symptoms at Time 1 had the highest mean levels of PTS and depressive symptoms at Time 2, M=36.30 and M=21.70, respectively. Time 2 PTS symptom levels for the comorbid group fell in the high-moderate range, just below the severe range (La Greca et al., 2010).
Table 2.
Mean scores for PTS and depressive symptoms and risk factors, by Time 1 clinical symptom groups.
| ANOVA | Group 1: | Group 2: | Group 3: | Group 4: | |
|---|---|---|---|---|---|
| PTS & depression (n=27) | PTS-only (n=35) | depression- only (n=29) | No PTS or depression (n=184) | ||
| PTS symptoms | |||||
| Time 1 | F (3, 271)=143.97*** | 47.41 (7.96)a | 43.37 (4.92)a | 25.59 (9.99)b | 16.92 (9.94)c |
| Time 2 | F (3, 271)=30.14*** | 36.30 (12.92)a | 26.80 (14.19)b | 21.86 (12.22)b, c | 14.67 (11.97)c |
| Depressive symptoms | |||||
| Time 1 | F (3, 271)=166.65*** | 24.37 (3.97)a | 12.43 (3.77)b | 23.34 (4.46)a | 8.17 (4.84)c |
| Time 2 | F (3, 271)=30.65*** | 21.70 (10.67)a | 12.66 (6.71)b | 14.76 (7.71)b | 8.61 (6.42)c |
| Risk factors | |||||
| Perceived life threat | F (3, 269)=6.62*** | .63 (.49)a | .51 (.51)a, b | .43 (.50)a, b | .27 (.45)b |
| Actual life threat | F (3, 271)=10.71*** | 1.59 (1.25)a | .97 (.98)b | 1.10 (1.14)a, b | .61 (.80)b |
| Initial L/D | F (3, 271)=20.52*** | 5.70 (1.64)a | 4.14 (1.88)b | 4.21 (1.72)b | 2.92 (1.96)c |
| Ongoing L/D | F (3, 271)=7.30*** | 2.22 (1.28)a | 1.97 (1.18)a | 1.69 (1.11)a, b | 1.29 (1.18)b |
| Major life events | F (3, 271)=17.69*** | 3.52 (2.44)a | 2.14 (1.83)b | 1.90 (1.72)b | 1.25 (1.35)b |
Note.
p <.001. L/D=Loss/Disruption. Superscripts within rows are different when means within the row are significantly different from one another (p<.05).
To evaluate whether PTS preceded depressive symptoms, we examined probabilities of “new cases” of depression occurring at Time 2. Among children not meeting clinical cutoffs for depression at Time 1 (Groups 2 and 4; n=219), we evaluated their probabilities of reporting “new cases” of depression at Time 2. Referencing Fig. 1, 17% of Group 2 and 10% of Group 4 children reported “new cases” of depression at Time 2. Thus, children with PTS-only (Group 2) were 1.7 times more likely to report new cases of depression than were children with no PTS or depression (Group 4). A χ2 test revealed significant group differences, χ2(1)=7.41, p<.01.
Similarly, we examined whether depressive symptoms preceded PTS at Time 2. Among children who did not meet clinical cutoffs for PTS at Time 1 (Groups 3 and 4; n=213), 13% and 5%, respectively, reported new cases of PTS. Thus, children with depression-only at Time 1 (Group 3) were 2.6 times more likely to report new cases of PTS than children with no PTS or depression (Group 4) at Time 1; χ2 testing revealed significant group differences, χ2(1)=3.76, p=.05. Overall, PTS may precede depressive symptoms, but depressive symptoms may also precede PTS.
As a follow-up analysis, we examined scores of children presenting with new cases of PTS or depressive symptoms at Time 2 (n=36); most children were already close to clinical cutoffs at Time 1. At Time 1, 50% were within one standard deviation of PTS cutoffs, and 47% were within one standard deviation of depression cutoffs.
3.4. Aim 3: Risk factors associated with comorbidity
Finally, we examined whether children with comorbid symptoms at Time 1 reported higher levels of risk factors. Two-way ANOVAs (Time 1 clinical symptom group by gender) were conducted for hurricane exposure (perceived and actual life threat) and recovery stressors (initial and ongoing loss/disruption, major life events). Gender was included as a factor because it was significantly related to Time 1 clinical symptom groups; Time 1 clinical symptom group by gender interactions were nonsignificant. However, Time 1 symptom group effects were significant (Table 2).
Post-hoc analyses revealed that children with comorbid symptoms reported more initial loss/disruption andmajor life events than any other group. Compared to children with PTS-only (Group 2), children with comorbid symptoms also reported more actual life threatening events. Compared to children with no PTS or depression (Group 4), children with comorbid symptoms reported higher levels of all five risk factors. Children with PTS-only reported higher perceived life threat than children with no elevated symptoms (Group 4). Children with depression-only reported more initial loss/disruption events than children with no depression (Groups 2 and 4). No other significant between group differences were found.
4. Discussion
The current study addressed several gaps in our understanding of children’s psychological functioning postdisaster. Children exposed to a destructive disaster that incurred little loss of life, frequently reported comorbid symptoms of PTS and depression. Elevated rates of PTS and depressive symptoms, as well as their comorbidity, were relatively stable from 8 to 15 months postdisaster; this stability was largely due to poor recovery among children who reported comorbid symptoms at 8 months postdisaster. Children with comorbid symptoms also reported more severe symptoms over time. We found that PTS increases risk for subsequent depressive symptoms, but also found evidence to support the reverse process. Finally, we examined risk factors that may help identify children at risk for developing comorbid symptoms of PTS and depression postdisaster. These key issues are discussed below.
4.1. Comorbidity rates
To our knowledge, this is the first study to demonstrate the presence of comorbid symptoms among children after a disaster involving little loss of life. Disasters involving little loss of life are more common than disasters involving significant loss of life (e.g., Guha-Sapir et al., 2012). In our study, 10% and 7% of children reported comorbid PTS and depressive symptoms 8 and 15 months postdisaster, respectively.
Surprisingly, these comorbidity rates were comparable to rates found after disasters involving significant loss of life. Comorbid PTS and depressive symptoms were reported by 9% of Chinese adolescents (grades 7–8) six months after the Wenchuan earthquake (Fan et al., 2011), and 6% of Indian adolescents (grades 9–10) 14 months after a super cyclone (Kar & Bastia, 2006). These disasters took the lives of 70,000 and 10,000 people, respectively. However, Goenjian et al. (2001) have found much higher comorbidity rates among children postdisaster. Six months after Hurricane Mitch, which killed approximately 10,000 people, comorbid symptoms of PTS and depression were reported by 79% of adolescents (M age=13 years) from a severely devastated city. Their sample is likely not representative of most child disaster samples, as 90% of that sample reported elevated PTS, and 81% reported elevated depression. These rates are much higher than that found in most child disaster samples (Bonanno et al., 2010).
Given our findings, researchers and clinicians need to assess for both PTS and depressive symptoms after any type of disaster. It is not currently common practice to assess for depressive symptoms after disasters; the majority of postdisaster research focuses only on PTS symptoms (Furr et al., 2010; Silverman and La Greca, 2002).
4.2. Comorbidity over time
We examined comorbid symptoms of PTS and depression over the first year and a half postdisaster. This is a crucial time period, as children reporting elevated symptoms near the end of the first year postdisaster are at risk for chronic distress. PTS symptoms decline initially postdisaster but are relatively stable by approximately seven to nine months (La Greca et al., 2010; Shaw et al., 1996). Depressive symptoms also decline initially (Ekşi et al., 2007), but are stable after the first several months postdisaster (Felix et al., 2011; Goenjian et al., 2011; Thienkrua et al., 2006).
In this study, children with comorbid PTS and depressive symptoms recovered more poorly than any other group; only one third of these children recovered by 15 months postdisaster. Thus, children with comorbid symptoms are at high-risk for persistent distress after disasters. Although substantial research has demonstrated that earlier PTS symptoms are significantly related to later depressive symptoms postdisaster (Catani et al., 2008; Goenjian et al., 2001; Kolaitis et al., 2003), no studies have specifically tracked psychological distress of children with comorbid symptoms over time.
Further, children with comorbid PTS and depressive symptoms reported the most severe symptom levels. These findings are in line with research outside the field of disasters, which suggests that any comorbid symptoms may increase the severity of psychological distress (Richards, 2011; Trickey et al., 2012). Our findings underscore the importance of early treatment of children with comorbid PTS and depressive symptoms postdisaster. Trans-diagnostic treatments that target multiple symptoms of psychological distress are needed. Most postdisaster interventions focus exclusively on children’s PTS symptoms (La Greca and Silverman, 2011), suggesting that comorbid symptoms of depression are not formally addressed.
With regard to the potential interplay between PTS and depression over time, we found that PTS symptoms precede and may contribute to later depressive symptoms, but also that depressive symptoms appeared to precede PTS symptoms. Both findings are in line with theories suggesting that PTS precedes and influences depression after disasters (AACAP Official Action, 1998), as well as with research outside the field of disasters indicating that depressive symptoms are a significant psychological problem predicting severity of PTS symptoms (Trickey et al., 2012). However, most of the children presenting with new “cases” of PTS or depressive symptoms at 15 months postdisaster had elevated symptoms levels at 8 months postdisaster (although not quite as high). Thus, our results suggest it may be important to evaluate children on a continuum of distress and not only focus on those who exceed designated cutoff scores.
4.3. Risk factors associated with comorbidity
A major strength of the current study was our recruitment of a diverse, economically distressed sample. In our study, 23% of children reported their parents changed jobs after Hurricane Ike. Minority children with few resources may experience high levels of recovery stressors (Furr et al., 2010; Weems et al., 2010). Compared to other disasters samples, children in our sample reported more recovery stressors than children assessed after Hurricanes Charley (La Greca et al., 2010) and Andrew (La Greca et al., 1996).
When we examined the relationship between risk factors and comorbidity, we found that the highest levels of risk factors were reported by children with comorbid symptoms. These risk factors were drawn from conceptual models designed to understand postdisaster PTS symptoms (e.g., La Greca et al., 1996, 2010; Yelland et al., 2010). Our findings indicate that these models may be useful for understanding comorbid symptoms of PTS and depression. This is important, because no clear models have yet been developed to understand comorbid symptoms postdisaster.
In the context of postdisaster interventions, our findings indicate that screening for and monitoring children experiencing high levels of postdisaster stressors may aid early identification of children at risk for developing comorbid symptoms. In addition, interventions should include strategies to help children and families cope with or reduce stressors.
In terms of whether risk factors might differentially relate to PTS or depressive symptoms, we found that children with PTS-only reported higher perceived life threat than children with no symptoms. Our findings are in keeping with research demonstrating that perceived life threat is one of the largest risk factors for children developing PTS after disasters (Blaze and Shwalb, 2009; Furr et al., 2010; La Greca et al., 2010; Weems et al., 2007). Thus, children’s perceptions of life threat may serve as a useful screener for children likely to develop PTS postdisaster.
In contrast, children with depression-only reported higher initial loss/disruption than children with no symptoms, but did not differ in terms of other recovery stressors (i.e., ongoing loss/disruption, major life events). Thus, recovery stressors more proximal to the event (i.e., initial loss/disruption) may serve to distinguish children who may develop elevated depressive symptoms postdisaster. These results are in keeping with models of depression (Abramsonet al., 1989; Beck, 1991), which emphasize the role of stressors and negative life events in the development of depression.
4.4. Limitations and future directions
Several limitations should be considered when interpreting results. First, we lacked data on children’s predisaster functioning, as is typical of most child disaster research, due to the unpredictable nature of disasters. Thus, it was not possible to determine whether preexisting difficulties contributed to symptom presentation postdisaster.
Second, we relied upon children’s self-reports, as have most postdisaster studies (e.g., La Greca et al., 2010; Weems et al., 2010). Nevertheless, children are considered the best informants of their postdisaster internalized distress. Parents underestimate children’s postdisaster distress symptoms, and their ratings are largely influenced by their own distress levels (Kassam-Adams et al., 2006).
Third, we did not use structured clinical interviews, as they are logistically difficult to administer with large samples of children postdisaster. Future research could extend our findings by using structured clinical interviews to obtain more precise diagnostic information, even if only conducted with a subset of youth (e.g., those who exceed symptom cutoff levels). Finally, our findings may not generalize to less diverse or more affluent samples of children.
In conclusion, our study presents crucial public health information. Children may present with comorbid symptoms of PTS and depression, even after disasters that involve little loss of life. Assessing for comorbid symptoms postdisaster is important, as these children are likely to experience persistent, severe symptoms across time. These youth may need strategies for coping with or reducing stressors, and they may need tailored interventions that will simultaneously address both PTS and depressive symptoms.
Acknowledgments
We kindly thank the families and schools who participated in this study. We would also like to thank Victoria Novinger, Allison Hoyle, and Sofia Cabrera, who assisted with the proof-reading of this manuscript.
Role of funding source
The data collection was partially funded by awards from the Flipse Funds and Cooper Fellowship from the University of Miami to Annette La Greca. In addition, data collection was partially funded by general funds from the University of Texas Medical Branch. Research time for the preparation of this manuscript was supported by the National Institute of Child Health and Human Development (NICHD; T32 HD07510). The University of Miami, the University of Texas Medical Branch, and the NICHD had to no further role in study design; in the collection, analysis and interpretation of data; in the writing of the paper; and in the decision to submit the paper for publication.
Footnotes
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- AACAP Official Action. Summary of the practice parameters for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:997–1001. doi: 10.1097/00004583-199809000-00025. [DOI] [PubMed] [Google Scholar]
- Abramson L, Metalsky G, Alloy L. Hopelessness depression: a theory-based subtype of depression. Psychological Review. 1989;96(2):358–372. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. The Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Beck A. Cognitive therapy: a 30-year retrospective. American Psychologist. 1991;46(4):368–375. doi: 10.1037//0003-066x.46.4.368. [DOI] [PubMed] [Google Scholar]
- Berg R. Tropical Cyclone Report: Hurricane Ike. National Hurricane Center, National Oceanic and Atmospheric Administration. 2008 < http://www.nhc.noaa.gov/pdf/TCR-AL092008_Ike_3May10.pdf>Retrieved August 14, 2008.
- Blake E, Landsea C, Gibney E. The Deadliest, Costliest, and Most Intense United States Tropical Cyclones From 1851 to 2010 (and other Frequently Requested Hurricane Facts) 2011 Retrieved from< http://www.nhc.noaa.gov/pdf/nws-nhc-6.pdf>.
- Blaze JT, Shwalb DW. Resource loss and relocation: a follow-up study of adolescents two years after Hurricane Katrina. Psychological Trauma: Theory, Research, Practice, and Policy. 2009;4:312–322. [Google Scholar]
- Bolton D, O’Ryan D, Udwin O, Boyle S, Yule W. The long-term psychological effects of a disaster experienced in adolescence: II: General psychopathology. The Journal of Child Psychology and Psychiatry. 2000;41(4):513. [PubMed] [Google Scholar]
- Bonanno G, Brewin C, Kaniasty K, La Greca A. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest. 2010;11(1):1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- Brent D, Melhem N, Donohoe B, Walker M. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. American Journal of Psychiatry. 2009;166(7):786–794. doi: 10.1176/appi.ajp.2009.08081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown EJ, Goodman RF. Childhood traumatic grief: an exploration of the construct in children bereaved on September 11. Journal of Clinical Child and Adolescent. 2005;34(2):248. doi: 10.1207/s15374424jccp3402_4. [DOI] [PubMed] [Google Scholar]
- Catani C, Jacob N, Schauer E, Kohila M, Neuner F. Family violence, war, natural disasters: a study of the effect of extreme stress on children’s mental health in Sri Lanka. BMC Psychiatry. 2008;8(1):33. doi: 10.1186/1471-244X-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole D, Peeke L, Martin J, Truglio R, Seroczynski A. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology. 1998;66(3):451–460. doi: 10.1037//0022-006x.66.3.451. [DOI] [PubMed] [Google Scholar]
- Comer J, Fan B, Duarte C, Wu P, Musa G, Mandell D, Hoven C. Attackrelated life disruption and child psychopathology in New York city public schoolchildren 6-months post-9/11. Journal of Consulting and Clinical Psychology. 2010;39(4):460–469. doi: 10.1080/15374416.2010.486314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell’Osso L, Carmassi C, Massimetti G, Conversano C, Daneluzzo E, Riccardi I, Stratta P, Rossi A. Impact of traumatic loss on post-traumatic spectrum symptoms in high school students after the L’Aquila 2009 earthquake in Italy. Journal of Affective Disorders. 2011;134:59–64. doi: 10.1016/j.jad.2011.06.025. [DOI] [PubMed] [Google Scholar]
- Ekşi A, Braun K, Ertem-Vehid H, Peykerli G, Saydam R, Toparlak D, Alyanak B. Risk factors for the development of PTSD and depression among child and adolescent victims following a 7.4 magnitude earthquake. International Journal of Psychiatry in Clinical Practice. 2007;11(3):190–199. doi: 10.1080/13651500601017548. [DOI] [PubMed] [Google Scholar]
- Eksi A, Braun K. Over-time changes in PTSD and depression among children surviving the 1999 Istanbul earthquake. European Child and Adolescent Psychiatry. 2009;18(6):384–391. doi: 10.1007/s00787-009-0745-9. [DOI] [PubMed] [Google Scholar]
- Fan F, Zhang Y, Yang Y, Mo L, Liu X. Symptoms of posttraumatic stress disorder, depression, and anxiety among adolescents following the 2008 Wenchuan earthquake in China. Journal of Traumatic Stress. 2011;24(1):44–53. doi: 10.1002/jts.20599. [DOI] [PubMed] [Google Scholar]
- Felix E, Hernández LA, Bravo M, Ramirez R, Cabiya J, Canino G. Natural disaster and risk of psychiatric disorders in Puerto Rican children. Journal of Abnormal Child Psychology. 2011;39(4):589–600. doi: 10.1007/s10802-010-9483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernando GA, Miller KE, Berger DE. Growing pains: the impact of disaster-related and daily stressors on the psychological and psychosocial functioning of youth in Sri Lanka. Child Development. 2010;81(4):1192–1210. doi: 10.1111/j.1467-8624.2010.01462.x. [DOI] [PubMed] [Google Scholar]
- Furr JM, Comer JS, Edmunds JM, Kendall PC. Disasters and youth: A meta-analytic examination of posttraumatic stress. Journal of Consulting and Clinical Psychology. 2010;78(6):765–780. doi: 10.1037/a0021482. [DOI] [PubMed] [Google Scholar]
- Giannopoulou I, Strouthos M, Smith P, Dikaiakou A, Galanopoulou V, Yule W. Post-traumatic stress reactions of children and adolescents exposed to the Athens 1999 earthquake. European Psychiatry. 2006;21(3):160–166. doi: 10.1016/j.eurpsy.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Goenjian AK, Molina L, Steinberg AM, Fairbanks LA, Alvarez ML, Goenjian HA, Pynoos RS. Posttraumatic stress and depressive reactions among Nicaraguan adolescents after Hurricane Mitch. American Journal of Psychiatry. 2001;158(5):788–794. doi: 10.1176/appi.ajp.158.5.788. [DOI] [PubMed] [Google Scholar]
- Goenjian A, Pynoos R, Steinberg A, Najarian L, Asarnow J, Karayan I, Fairbanks L. Psychiatric comorbidity in children after the 1988: earthquake in Armenia. The Journal of the American Academy of Child and Psychiatry’s. 1995;34(9):1174. doi: 10.1097/00004583-199509000-00015. [DOI] [PubMed] [Google Scholar]
- Goenjian A, Roussos A, Steinberg A, Sotiropoulou C, Walling D, Kakaki M, Karagianni S. Longitudinal study of PTSD, depression, and quality of life among adolescents after the Parnitha earthquake. Journal of Affective Disorders. 2011;133(3):509–515. doi: 10.1016/j.jad.2011.04.053. [DOI] [PubMed] [Google Scholar]
- Goenjian AK, Walling D, Steinberg AM, Roussos A, Goenjian HA, Pynoos RS. Depression and PTSD symptoms among bereaved adolescents 6 1/2 years after the 1988 Spitak earthquake. Journal of Affective Disorders. 2009;112(1–3):81–84. doi: 10.1016/j.jad.2008.04.006. [DOI] [PubMed] [Google Scholar]
- Greenberg M, Siegle J, Leitch C. The nature and importance of attachment relationships to parents and peers during adolescence. Journal of Youth and Adolescence. 1983;12(5):373–386. doi: 10.1007/BF02088721. [DOI] [PubMed] [Google Scholar]
- Guha-Sapir D, Vos F, Below R, Ponserre S. Annual Disaster Statistical Review 2011: The Numbers and Trends. CRED. Louvain, Belgium: Catholic University of Louvain; 2012. Available online. [Google Scholar]
- Gurwitch R, Kees M, Becker S. In the face of tragedy: placing children’s reaction to trauma in a new context. Cognitive and Behavioral Practice. 2002;9:286–295. [Google Scholar]
- Howell D. Statistical Methods for Psychology. 6th ed. Belmont: Thomson Wadsworth; 2007. [Google Scholar]
- Jaycox L, Cohen J, Mannarino A, Walker D, Langley A, Gegenheimer K, Scott M, Schonlau M. Children’s mental health care following Hurricane Katrina: a field trail of trauma-focused psychotherapies. Journal of Traumatic Stress. 2010;23(2):223–231. doi: 10.1002/jts.20518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J, McCutcheon S. In: Assessing life stress in older children and adolescents: preliminary findings with the life events checklist. SER Clin. C.. Hemisphere. Sarason I, Spielberger C, editors. Washington, DC: 1980. pp. 111–125. [Google Scholar]
- Kar N, Bastia B. Post-traumatic stress disorder, depression and generalised anxiety disorder in adolescents after a natural disaster: a study of comorbidity. Clinical Practice and Epidemiology in Mental Health. 2006;2(1):17. doi: 10.1186/1745-0179-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakaya I, Agaoglu B, Coskun A, Sismanlar S, Memik N, Yildizoc O. Post-traumatic stress reaction symptoms among Turkish students: assessments one and six months after a terrorist attack in Istanbul. Hong Kong Journal of Psychiatry. 2006;16(2):65–70. [Google Scholar]
- Kassam-Adams N, Garcia-Espana J, Miller V, Winston F. Parent-child agreement regarding children’s acute stress. The Journal of the American Academy of Child and Psychiatry’s. 2006;45(12):1485–1493. doi: 10.1097/01.chi.0000237703.97518.12. [DOI] [PubMed] [Google Scholar]
- Kolaitis G, Kotsopoulos J, Tsiantis J, Haritaki S, Rigizou F, Zacharaki L, Riga E, Augoustatou A, Bimbou A, Kanari N, Liakopoulou M, Katerelos P. Posttraumatic stress reactions among children following the Athens earthquake of September, 1999. European Child & Adolescent Psychiatry. 2003;12(6):273–280. doi: 10.1007/s00787-003-0339-x. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica. 1981;46:305–315. [PubMed] [Google Scholar]
- La Greca A, Silverman W. Interventions for youth following disasters and acts of terrorism. In: Kendall P, editor. Child and Adolescent Therapy: Cognitive-Behavioral Procedures. 4th ed. New York: Guilford Press; 2011. [Google Scholar]
- La Greca AM, Silverman WK, Lai BS, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: concurrent and prospective impact on children’s persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology. 2010;78(6):794–805. doi: 10.1037/a0020775. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Vernberg EM, Prinstein MJ. Symptoms of posttraumatic stress in children after Hurricane Andrew: a prospective study. Journal of Consulting and Clinical Psychology. 1996;64(4):712–723. doi: 10.1037//0022-006x.64.4.712. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Wasserstein SB. Children’s predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. Journal of Consulting & Clinical Psychology. 1998;66(6):883–892. doi: 10.1037//0022-006x.66.6.883. [DOI] [PubMed] [Google Scholar]
- Norris F, Sherrieb K, Galea S. Prevalence and consequences of disasterrelated illness and injury from Hurricane Ike. Rehabilitation Psychology. 2010;55(3):221–230. doi: 10.1037/a0020195. [DOI] [PubMed] [Google Scholar]
- North C, Kawasaki A, Spitznagel E, Hong B. The course of PTSD, major depression, substance abuse, and somatization after a natural disaster. The Journal of Nervous and Mental Disease. 2004;192:823–829. doi: 10.1097/01.nmd.0000146911.52616.22. [DOI] [PubMed] [Google Scholar]
- Pina A, Villalta I, Ortiz C, Gottschall A, Costa N, Weems C. Social support, discrimination, and coping as predictors of posttraumatic stress reactions in youth survivors of Hurricane Katrina. Journal of Clinical Child & Adolescent. 2008;37(3):564–574. doi: 10.1080/15374410802148228. [DOI] [PubMed] [Google Scholar]
- Richards D. Prevalence and course of depression: a review. Clinical Psychology Review. 2011;31:1117–1125. doi: 10.1016/j.cpr.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Rodriguez N, Steinberg A, Saltzman W, Pynoos R. Symposium conducted at the Annual Meeting of the International Society for Traumatic Stress Studies. New Orleans, LA: 2001. Dec, PTSD Index: Preliminary psychometric analyses of child and parent versions. [Google Scholar]
- Roussos A, Goenjian A, Steinberg A, Sotiropoulou C, Kakaki M, Kabakos, Karagianni S, Manouras V. Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia, Greece. The American Journal of Psychiatry. 2005;162(3):530–537. doi: 10.1176/appi.ajp.162.3.530. [DOI] [PubMed] [Google Scholar]
- Rudolph K, Flynn M. Childhood adversity and youth depression: influence of gender and pubertal status. Development and Psychopathology. 2007;19:497–521. doi: 10.1017/S0954579407070241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seballos F, Tanner T, Tarazona M, Gallegos J. Children in a Changing Climate Research Report. Brighton: IDS; 2011. Children and Disasters: Understanding Impact and Enabling Agency. [Google Scholar]
- Scheeringa MS, Zeanah CH. Reconsideration of harm’s way: Onsets and comorbidity patterns of disorders in preschool children and their caregivers following Hurricane Katrina. Journal of the American Academy of Child and Adolescent. 2008;37(3):508–518. doi: 10.1080/15374410802148178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw J, Applegate B, Schorr C. Twenty-one-month follow-up study of school-age children exposed to Hurricane Andrew. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(3):359–364. doi: 10.1097/00004583-199603000-00018. [DOI] [PubMed] [Google Scholar]
- Silverman W, La Greca AM. Children experiencing disasters: definitions, reactions, and predictors of outcomes. In: LaGreca AM, Silverman W, Vernberg EM, Roberts MC, editors. Helping Children Cope with Disasters. Washington, DC: American Psychological Association; 2002. pp. 11–34. [Google Scholar]
- Steinberg A, Brymer M, Decker K, Pynoos R. The University Of California At Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports. 2004;6(2):96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Thienkura W, Cardozo B, Chakkraband M, Guadamuz T, Pengjuntr W, Tantipiwatanaskul P, Sakornsatian S, van Griensven F. Symptoms of posttraumatic stress disorder and depression among children in tsunamiaffected areas in southern Thailand. The Journal of the American Medical Association. 2006;296(5):549–559. doi: 10.1001/jama.296.5.549. [DOI] [PubMed] [Google Scholar]
- Trickey D, Siddaway A, Meiser-Stedman R, Serpell L, Field A. A metaanalysis of risk factors of post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012;32:122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Vernberg E, La Greca A, Silverman W, Prinstein M. Prediction of posttraumatic stress symptoms in children after Hurricane Andrew. Journal of Abnormal Psychology. 1996;105(2):237–248. doi: 10.1037//0021-843x.105.2.237. [DOI] [PubMed] [Google Scholar]
- Weems C, Pina A, Costa N, Watts S, Taylor L, Cannon M. Predisaster trait anxiety and negative affect predict posttraumatic stress in youths after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2007;75:154–159. doi: 10.1037/0022-006X.75.1.154. [DOI] [PubMed] [Google Scholar]
- Weems CF, Taylor L, Cannon M, Marino R, Romano D, Scott B, Perry A, Triplett V. Post traumatic stress, context, and the lingering effects of the Hurricane Katrina disaster among ethnic minority youth. Journal of Abnormal Child Psychology. 2010;38:49–56. doi: 10.1007/s10802-009-9352-y. [DOI] [PubMed] [Google Scholar]
- Wickrama KAS, Kaspar V. Family context of mental health risk in tsunami-exposed adolescents: findings from a pilot study in Sri Lanka. Social Science & Medicine. 2007;64(3):713–723. doi: 10.1016/j.socscimed.2006.09.031. [DOI] [PubMed] [Google Scholar]
- Yelland C, Robinson P, Lock C, La Greca AM, Kokegei B, Ridgway V, Lai BS. Bushfire impact on youth. Journal of Traumatic Stress. 2010;23(2):274–277. doi: 10.1002/jts.20521. [DOI] [PubMed] [Google Scholar]