Abstract
OBJECTIVES
The body adiposity index (BAI) is a proposed alternative to the body mass index (BMI) that has shown good cross-sectional agreement with percent body fat (%BF) in validation studies. The objective of this study was to examine the ability of BAI to track adiposity change over time in a biracial sample of midlife women.
METHODS
African-American (n=159) and Caucasian (n=206) women, aged 42–60 years, at the Chicago site of the Study of Women’s Health Across the Nation were followed from 2002–2008. BAI and BMI were calculated from measurements taken at annual assessments. %BF was quantified using whole-body dual-energy X-ray absorptiometry. Difference scores (BAIΔ, BMIΔ, and %BFΔ) quantified adiposity change over a mean of 1.6 (SD=0.7) years. Lin’s concordance correlation (ρc) and Bland-Altman limits-of-agreement assessed agreement between BAI and %BF.
RESULTS
In examining adiposity change, BAIΔ showed poor agreement with %BFΔ in the overall sample (ρc=.41), African-American women (ρc=.36), and Caucasian women (ρc=.43). BAIΔ estimated %BFΔ with minimal bias (+0.4%) but low precision (±6.3%BF limits-of-agreement). %BFΔ had weaker correlations with BAIΔ (r’s=.38 to .48) than with BMIΔ (r’s=.48 to .59). BAI and BMI showed similar cross-sectional associations with %BF in the overall sample and within each race (r’s>.74).
CONCLUSIONS
We conclude that BAI is less accurate than BMI in tracking adiposity change in midlife women, and would not be a suitable replacement for BMI in most research applications involving adiposity change.
Keywords: Anthropometric, Adiposity, Body Mass Index, Validation Studies, Dual-Energy X-Ray Absorptiometry
INTRODUCTION
Body mass index (BMI), the ratio of weight to height squared, is commonly used to quantify adiposity in research and clinical applications. However, BMI does not differentiate between lean and fat mass, and its relations with percent body fat (%BF) are sex- and ethnicity-dependent (Evans et al., 2006; Fernandez et al., 2003). Bergman et al. (2011) recently proposed the body adiposity index (BAI), which is based on hip circumference and height [hip(cm)/height(m)1.5−18], as an alternative metric to BMI. BAI is purported to have several advantages over BMI, including that it yields similar associations with %BF for men and women and may be more practical to assess in field studies because it does not require a weight measurement. Additionally, BAI was calibrated to provide a direct numerical estimate of %BF, whereas %BF can only be estimated from BMI using an equation that accounts for gender, age, and race (Deurenberg et al., 1998). BAI performed similarly or better than BMI in estimating %BF derived from dual-energy X-ray absorptiometry (DXA) in Hispanic, African-American, and Caucasian samples (Barreira et al., 2011; Bergman et al., 2011; Johnson et al., 2012).
Though BAI shows good cross-sectional agreement with %BF, its ability to capture change in adiposity is unknown. As visceral adipose tissue accumulates and diminishes more rapidly in response to changes in energy balance than subcutaneous adipose tissue (Hallgreen and Hall, 2008; Lara-Castro et al., 2002), adiposity measures linked to subcutaneous fat depots, such as BAI, may be less sensitive to change in adiposity than measures derived from total body weight, such as BMI. This study compared BAI to BMI in capturing change in DXA-derived %BF in African-American and Caucasian women at midlife, a period characterized by changes in weight and female body composition (Sowers et al., 2007).
METHODS
Participants were African-American and Caucasian women enrolled in the ancillary Fat Patterning Study at the Chicago site of the Study of Women’s Health Across the Nation (SWAN). The Fat Patterning Study occurred between 2002–2008, coincident with annual SWAN follow-up visits 4–11. Women who were already enrolled in the Chicago SWAN cohort, or who were screened as part of the original Chicago SWAN recruitment effort but were too young to participate in 1996, were recruited for the Fat Patterning Study. Eligible women weighed less than 300 lbs, did not have breast or hip implants, and had no history of diabetes, liver or renal disease, anorexia nervosa, or substance abuse. Fat Patterning Study procedures are described elsewhere (Janssen et al., 2010). Rush University Medical Center’s Institutional Review Board approved study procedures.
Participant age and self-reported race/ethnicity were documented at SWAN baseline.
BMI [weight(kg)/height2(m)] and BAI [hip circumference(cm)/height(m)1.5−18] were calculated annually at each of the four SWAN visits concurrent with the Fat Patterning Study.
Whole-body DXA scans (GE Lunar Prodigy, Madison, WI) were performed annually with subjects in a supine position. Scans were analyzed with GE-Lunar enCORE software, and %BF was calculated as total fat mass divided by fat mass + lean tissue.
As anthropometric measurements and %BF were collected in separate visits, analyses only included data from years in which a woman’s anthropometric measurements and DXA scans occurred ≤90 days apart. Cross-sectional agreement between %BF and BAI at baseline was examined with Lin’s concordance correlation (ρc) (Lin, 2000) and the Bland-Altman limits-of-agreement method (Bland and Altman, 1986). Lin’s concordance correlation assesses agreement between measures as a function their Pearson correlation and the deviation of their best-fit line from perfect concordance. The Bland-Altman limits-of-agreement yields a bias score reflecting the average difference between measures, and 95% confidence intervals reflecting precision of measurement. As agreement only pertains to variables utilizing the same scale of measurement (BAI and %BF), Pearson correlations tested associations of BMI with %BF and BAI.
For each woman, the two time points associated with the largest absolute change in body weight (kg) were selected for analysis to maximize the range of adiposity change in the analyzed sample. Agreement between BAIΔ and %BFΔ was assessed with Lin’s concordance correlation and Bland-Altman limits-of-agreement. Pearson correlations tested associations between the BAIΔ, %BFΔ, and BMIΔ. Analyses were conducted for the entire sample and stratified by race. Two-sample t-tests compared African-American and Caucasian women on adiposity metrics. Analyses were performed in SAS 9.2 (SAS Institute, Cary, NC) and Stata 11 (StataCorp, College Station, TX).
RESULTS
Analyses included 365 women. Women were 50.1 (SD=3.7) years old at Fat Patterning Study baseline. Usable baseline data were obtained from 352 women. BAIΔ, %BFΔ, and BMIΔ were calculated for 248 women using observations of change collected an average of 1.6 (SD=0.7) years apart. On average, anthropometric and DXA measures within a given year were collected ±26.6 (SD=20.4) days apart.
Table 1 presents baseline values and difference scores for adiposity metrics. African-American women had higher %BF (t(350)=4.11, p<.0001), BAI (t(350)=4.10, p<.001), and BMI (t(350)=6.28, p<.0001) than Caucasian women. The mean absolute difference in weight between the two years selected for difference score analyses was ±3.8 kg (SD=2.9 kg) for African-American women and ±3.6 kg (SD=3.3 kg) for Caucasian women (t(246)=0.46, p=.65). Groups did not differ on mean BAIΔ, %BFΔ, and BMIΔ (p’s>.50).
Table 1.
Agreement and correlations between BAI, percent body fat (%BF), and BMI baseline measurements and difference scores in African-American and Caucasian midlife women who completed anthropometric measurements and DXA scans ≤90 days apart in a given year.
| Baseline measurements
| ||||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD)
|
BAI/%BFagreement
|
Pearson correlationd
|
|||||
| BAIa | BMIa | %BFa | ρc, (95% CI)b | Bias (95% CI)c | BAI/%BF | BMI/%BF | ||
| African-American | 156 | 35.9 (6.2) | 31.6 (6.7) | 45.1 (8.0) | .39 (.31, .46) | −9.2 (−19.8, 1.4) | .74 | .74 |
| Caucasian | 196 | 33.2 (5.9) | 27.4 (5.6) | 41.4 (8.7) | .45 (.38, .52) | −8.2 (−19.0, 2.7) | .78 | .81 |
| Total | 352 | 34.4 (6.2) | 29.3 (6.4) | 43.0 (8.6) | .44 (.39, .49) | −8.6 (−19.4, 2.1) | .77 | .78 |
|
| ||||||||
| Change scores
| ||||||||
| n | Mean (SD)
|
BAIΔ/%BFΔ agreement
|
Pearson correlationd
|
|||||
| BAIΔ | BMIΔ | %BFΔ | ρc, (95% CI)b | Bias (95% CI)c | BAIΔ/%BFΔ | BMIΔ/%BFΔ | ||
| African-American | 91 | .37 (2.44) | .23 (1.71) | .09 (3.36) | .36 (.19, .53) | .28 (−6.22, 6.78) | .38 | .48 |
| Caucasian | 157 | .27 (2.31) | .18 (1.91) | −.21 (3.50) | .43 (.32, .55) | .47 (−5.69, 6.64) | .48 | .59 |
| Total | 248 | .31 (2.35) | .20 (1.84) | −.10 (3.44) | .41 (.31, .50) | .40 (−5.88, 6.68) | .44 | .55 |
Significant group difference by t-test at p<.001.
Lin’s concordance correlation coefficient (ρc), which is a function of both the Pearson correlation between two measures, and the deviation of their best-fit line from perfect concordance (a 45-degree line through the origin).
The Bland-Altman limits-of-agreement method yields a bias score reflecting the mean difference between the BAI and %BF, as well as the 95% confidence interval (CI) around the mean difference.
All reported Pearson correlations are significant at p<.001
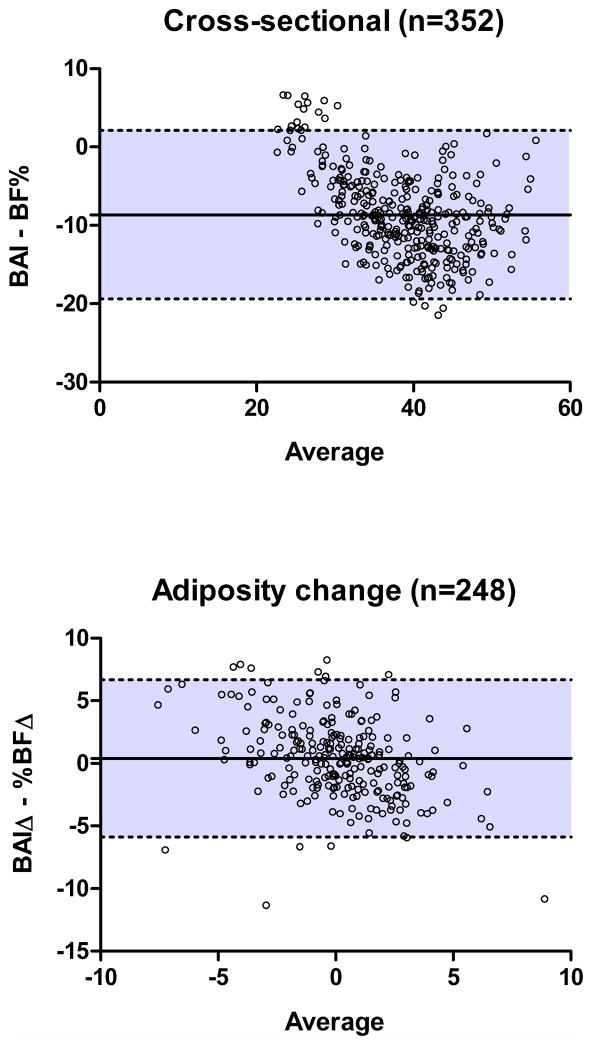
Cross-sectional agreement (ρc) between BAI and %BF was modest overall and within each race/ethnicity (Table 1). BAI underestimated %BF by 8.6%, 9.2%, and 8.2% overall and within African-American and Caucasian women, respectively. The 95% limits-of-agreement for differences between BAI and %BF were ±10.8 %BF overall, ±10.6 %BF for African-American women, and ±10.8 %BF for Caucasian women (Figure 1). BAI and BMI demonstrated similar correlations with %BF.
Figure 1.
Bland-Altman plots depicting cross-sectional agreement between BAI and %BF at Fat Patterning Study Baseline (top) and agreement between BAIΔ and %BFΔ over an average of 1.6 (SD=0.7) years of follow-up (bottom). Plots show the mean and 95% confidence intervals of the differences between measures across the distribution of scores.
In analyses involving adiposity change, agreement (ρc) between BAIΔ and %BFΔ was low (Table 1). Though BAIΔ overestimated change in %BF by only a small degree (0.40% overall, 0.28% in African-American women, and 0.47% in Caucasian women), the 95% limits-of-agreement were wide (±6.3 %BF overall, ±6.5 %BF for African-American women, ±6.2 for Caucasian women; Figure 1). Correlations between BAIΔ and %BFΔ were lower than those between BMIΔ and %BFΔ. BAIΔ and BMIΔ correlated less strongly with %BFΔ in African-American women than Caucasian women.
DISCUSSION
Among African-American and Caucasian women at midlife, BAIΔ estimated adiposity change without significant bias, but showed weaker associations with %BFΔ than BMIΔ. BMI is more strongly associated with visceral adipose mass than BAI (Hung et al., 2012), which may explain its stronger association with adiposity change than BAI in the current study. Visceral fat is more labile in response to changes in energy balance, and increases or decreases in volume approximately 30% faster than total body fat (Hallgreen and Hall, 2008; Lara-Castro et al., 2002) during weight gain and weight loss, respectively. BAI quantifies height-adjusted adiposity solely based on variation in hip circumference, which largely reflects subcutaneous gluteal fat stores, pelvic width, and gluteal muscle mass. BAI may therefore be relatively insensitive to changes in central adiposity, which reflects visceral and subcutaneous abdominal fat.
Both BAIΔ and BMIΔ demonstrated slightly weaker associations with %BFΔ in African-American women compared to Caucasian women, despite similar levels of adiposity change during follow up and similar cross-sectional associations of BMI and BAI with %BF in both groups. As the proportion of fat to fat-free mass lost or gained with changes in energy balance does not vary by race (Broyles et al., 2011), additional research is needed to determine if this finding stems from known racial/ethnic differences in body composition (Wagner et al., 2000).
We extended prior studies by examining cross-sectional agreement between BAI and %BF in African-American and Caucasian women at midlife, a time associated with significant changes in female body composition (Sowers et al., 2007). The observed cross-sectional associations between BAI and %BF were strong, similar for African-American and Caucasian women, and roughly equivalent to those involving BMI. BAI underestimated %BF by about 8.6%, which may be due to true bias in the BAI’s estimation of %BF in midlife women, bias in the measurement of %BF, or both. Prior studies examining cross-sectional agreement between BAI and DXA-derived %BF in different groups have found no bias, overestimation, and underestimation (Barreira et al., 2011; Bergman et al., 2011; Johnson et al., 2012). Findings suggest BAI is useful for ranking midlife women on adiposity, but would need recalibration to accurately estimate %BF.
Study limitations include the temporal lag between anthropometric measurements and DXA scans and brief follow-up period. Limiting analysis to years in which measurements were collected ≤90 days apart and utilizing the pair of observations associated with the largest absolute weight change may not have completely overcome these limitations. The sample was relatively large, but fewer African-American women were included in adiposity change analyses than Caucasian women. Additionally, the sample size did not provide adequate power to conduct subgroup analyses by level of adiposity. Findings may not generalize to men, individuals ≥300 lbs, or women of different ages or races/ethnicities.
Though BAI appears comparable to BMI in assessing current adiposity in African-American and Caucasian women, it is less accurate than BMI in tracking adiposity change. Despite the limitations of BMI, BAI would not be a suitable replacement for BMI in most research or clinical applications involving adiposity change at midlife.
Acknowledgments
The Study of Women’s Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women’s Health (ORWH) (Grants NR004061; AG012505, AG012535, AG012531, AG012539, AG012546, AG012553, AG012554, AG012495). The SWAN Fat Patterning Study is supported by the National Heart, Lung, and Blood Institute (NHLBI) (Grant HL067128) and the Charles J. and Margaret Roberts Trust. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH or the NIH.
Footnotes
CONFLICT OF INTEREST
The authors declared no conflict of interest.
References
- Barreira TV, Harrington DM, Staiano AE, Heymsfield SB, Katzmarzyk PT. Body adiposity index, body mass index, and body fat in white and black adults. JAMA. 2011;306:828–830. doi: 10.1001/jama.2011.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity (Silver Spring) 2011;19:1083–1089. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- Broyles ST, Bouchard C, Bray GA, Greenway FL, Johnson WD, Newton RL, et al. Consistency of fat mass--fat-free mass relationship across ethnicity and sex groups. Br J Nutr. 2011;105:1272–1276. doi: 10.1017/S0007114510004794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord. 1998;22:1164–1171. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- Evans EM, Rowe DA, Racette SB, Ross KM, McAuley E. Is the current BMI obesity classification appropriate for black and white postmenopausal women? Int J Obes (Lond) 2006;30:837–843. doi: 10.1038/sj.ijo.0803208. [DOI] [PubMed] [Google Scholar]
- Fernandez JR, Heo M, Heymsfield SB, Pierson RN, Jr, Pi-Sunyer FX, Wang ZM, et al. Is percentage body fat differentially related to body mass index in Hispanic Americans, African Americans, and European Americans? Am J Clin Nutr. 2003;77:71–75. doi: 10.1093/ajcn/77.1.71. [DOI] [PubMed] [Google Scholar]
- Hallgreen CE, Hall KD. Allometric relationship between changes of visceral fat and total fat mass. Int J Obes (Lond) 2008;32:845–852. doi: 10.1038/sj.ijo.0803783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung CS, Yang CY, Hsieh HJ, Wei JN, Ma WY, Li H-Y. BMI correlates better to visceral fat and insulin sensitivity than BAI. Obesity (Silver Spring) 2012;20(6):1141. doi: 10.1038/oby.2012.86. [DOI] [PubMed] [Google Scholar]
- Janssen I, Powell LH, Kazlauskaite R, Dugan SA. Testosterone and visceral fat in midlife women: the Study of Women’s Health Across the Nation (SWAN) Fat Patterning Study. Obesity (Silver Spring) 2010;18:604–610. doi: 10.1038/oby.2009.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson W, Chumlea WC, Czerwinski SA, Demerath EW. Concordance of the recently published body adiposity index with measured body fat percent in European-American adults. Obesity (Silver Spring) 2012;20:900–903. doi: 10.1038/oby.2011.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara-Castro C, Weinsier RL, Hunter GR, Desmond R. Visceral adipose tissue in women: longitudinal study of the effects of fat gain, time, and race. Obes Res. 2002;10:868–874. doi: 10.1038/oby.2002.119. [DOI] [PubMed] [Google Scholar]
- Lin LI. A note on the concordance correlation coefficient. Biometrics. 2000;56:324–325. [Google Scholar]
- Sowers M, Zheng H, Tomey K, Karvonen-Gutierrez C, Jannausch M, Li X, et al. Changes in body composition in women over six years at midlife: ovarian and chronological aging. J Clin Endocrinol Metab. 2007;92:895–901. doi: 10.1210/jc.2006-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner DR, Heyward VH. Measures of body composition in blacks and whites: a comparative review. Am J Clin Nutr. 2000;71:1392–1402. doi: 10.1093/ajcn/71.6.1392. [DOI] [PubMed] [Google Scholar]