Abstract
In this review, we hypothesized the importance of the interaction between the brain glutathione (GSH) system, the proteolytic tissue plasminogen activator (t-PA)/plasminogen/ plasmin system, regulated by plasminogen activator inhibitor (PAI-1), and neuroserpin in the pathogenesis of Alzheimer’s disease. The histopathological characteristic hallmark that gives personality to the diagnosis of Alzheimer’s disease is the accumulation of neurofibroid tangles located intracellularly in the brain, such as the protein tau and extracellular senile plaques made primarily of amyloidal substance. These formations of complex etiology are intimately related to GSH, brain protective antioxidants, and the proteolytic system, in which t-PA plays a key role. There is scientific evidence that suggests a relationship between aging, a number of neurodegenerative disorders, and the excessive production of reactive oxygen species and accompanying decreased brain proteolysis. The plasminogen system in the brain is an essential proteolytic mechanism that effectively degrades amyloid peptides (“beta-amyloidolysis”) through action of the plasmin, and this physiologic process may be considered to be a means of prevention of neurodegenerative disorders. In parallel to the decrease in GSH levels seen in aging, there is also a decrease in plasmin brain activity and a progressive decrease of t-PA activity, caused by a decrease in the expression of the t-PA together with an increase of the PAI-1 levels, which rise to an increment in the production of amyloid peptides and a lesser clearance of them. Better knowledge of the GSH mechanism and cerebral proteolysis will allow us to hypothesize about therapeutic practices.
Keywords: glutathione, Alzheimer’s disease, t-PA, PAI-1, plasminogen
Introduction
Sporadic or common Alzheimer’s disease (AD) is a chronic process of complex etiology, without any existing effective treatment, with aging being the main etiological factor of universal risk.
The histopathological characteristic that gives personality to the diagnosis of AD is the accumulation of neurofibroid tangles located intracellularly in the brain, such as protein tau1–6 and senile plaques with extracellular amyloid beta (Ab) substance.7–13 These deposits are produced as a consequence of a biological disorder in their production and elimination/clearance from the brain.10,13–17 These formations of complex etiology are intimately related to glutathione (GSH), brain protective antioxidants, and proteolysis, in which tissue plasminogen activator (t-PA) plays a key role.18,19
Our review suggests that GSH may play an essential role in the physiopathology of the different components of the proteolytic mechanisms in the brain, and focuses on its relation to t-PA and the plasminogen/plasmin system.
Brain GSH
GSH (L-gamma-glutamyl-L-cysteinylglycine) is a tripeptide present in large quantities in all mammal cells and in small amounts extracellularly,20–22 being mainly located in the cytosol, mitochondria, and endoplasmic reticulum.23 It plays a very important role in many biological processes involved in organism homeostasis, most notably, in neutralizing the free radicals that produce reactive oxygen species (ROS) (due to its great antioxidant activity),20,24–28 since oxidation is a basic process in the genesis of neurodegenerative disorders.29
GSH is the most important component of the antioxidant mechanism of the brain.30 It has a relatively homogeneous distribution in rat brains,31–33 reaching its highest levels in the brain cortex, corpus striatum, and the glia31,34 but it diminishes significantly with aging.32,34,35 GSH levels in neuronal cells are lower than in glia cells.36–38 This difference can be due to a smaller reserve of precursors for the GSH synthesis, especially of cysteine.
In studies of brain cells, the concentration of GSH in different neuronal cells has been found to vary considerably.39,40 Likewise, the GSH concentration in astroglia cell cultures has also been found to vary widely.39,41,42 Other studies have shown lower GSH concentration levels in neurons than in astrocytes,39,43 with the concentration of endogenous neuronal GSH ten times lower than in astrocytes.44 The separation of neurons and glia cells in cocultures and then their later culture has shown a significantly decreased level of neuronal GSH whereas this remained constant in astroglia cells.43 This difference in GSH levels between astrocytes and neurons was observed in the cortex; nevertheless, the concentrations are very similar in other parts of the brain, like the midbrain and the stratium.45 It is possible that this presence and distribution in the brain is due to cellular specialization that confers a great capacity to generate free radicals, as a consequence of being an organ with high oxygen requirement (20% of the total consumption of the organism, in spite of being less than 2% of the body weight in human adults).46
Astrocytes protect neurons against the toxicity of free radicals by increasing their GSH levels, by means of the transfer of sulfated amino acids or peptides as precursors (mainly cysteine and the dipeptide CysGly).30,44,47–49 An increase in cellular GSH concentration makes the neurons more resistant to cytotoxic injuries.50–52
Many cerebral functions are altered as a consequence of decrease in intra- and extracellular levels of GSH.53 This decrease can be due to either the inhibition of its synthesis or its consumption in the conjugation with exogenous compounds.24,54 The progressive decrease of GSH levels resulting from aging and related illnesses, is of great interest for investigators.55,56 The decrease of GSH levels has been detected not only in humans, but also in lesser animals, such as rodents and insects.57 The decrease found with aging is linked to an increase of ROS.58 There is scientific evidence of a relationship between aging and a number of neurodegenerative processes due to the excessive production of free radicals and the imbalance between the oxidant species and antioxidant defenses.59–61
Buthionine sulfoximine (S-(n-butyl) homocysteine sulfoximine) (BSO), a selective and potent inhibitor of the gamma-glutamylcysteine synthetase,24,62 has been administered in previous investigations. BSO inhibits GSH biosynthesis and causes depletion of cellular GSH levels.21,22 In rats, the same GSH decrease has also been achieved with the administration of diethyl maleate – the diethyl maleate reacts with GSH, causing the formation of conjugated GSH, which is then excreted.31,62–64
The effect of pharmacological depletion of cerebral GSH following exposure to BSO and diethyl maleate, in cellular cultures or after their administration to animals, has been studied over the last 20 years. From an experimental point of view, the administration of BSO by systemic route to adults has not been very effective in producing GSH depletion in the brain,65 being effective only in newborn rats or mice, where it was facilitated by the immaturity of the blood–brain barrier (BBB).66 Low levels in adult animals have been achieved using a direct intracerebroventricular65,67 administration of BSO by means of stereotaxic technique68 or by intrathecal administration.69
The decrease of GSH levels in the brain of newborn rats has been shown to frequently lead the animal to a fatal situation, as a consequence of the accumulation of hydrogen peroxide and subsequent mitochondrial lesion, thus showing the great metabolic importance of GSH.66,70 Decrease in the number of cerebral mitochondria has also been observed71 as well as the reduction in enzymatic activity of GSH reductase.72 In investigations of cerebral ischemia, it has been observed that GSH depletion exacerbates cortical infarction and edemas after ischemia, due to an increasing presence of ROS.73 In cultures of mesencephalic cells, incubation with BSO has caused a significant reduction of GSH, resulting in a loss of the integrity of the membrane and cellular death,74,75 after the loss of mitochondrial GSH.76 The depletion of cerebral GSH has also been found to modify the interaction between astrocytes and neurons, diminishing the neuronal protection against oxidant agents.44,77
Given the GSH decrease that is progressively produced with aging,57,60,78,79 we cannot discard the hypothesis that a defect in the mechanism of antioxidant cellular defense can be the silent trigger of the neurodegenerative process and neuronal death.72 It may be that an imbalance in the equilibrium between the formation of free radicals and their neutralization (oxidation–reduction) leads to a situation of oxidative stress with great organic risk that can be associated with neurodegenerative illnesses,73,79,80 including, most often, Parkinson’s disease25 and AD.33,74
Fibrinolytic activity and GSH
In 1959, Todd81 devised a histochemical fibrin slide technique with which he demonstrated the existence of areas of lysis in vascular walls that were related to the presence of the activators of fibrinolysis. Using immunohistochemical methods, it was revealed that t-PA was present in the blood vessels of most organs and that it was synthesized by endothelial cells.82,83
More than 20 years ago62 it was reported that the pharmacological effect of administration of BSO or diethyl maleate in rabbits is a significant decrease in GSH levels, accompanied by the inhibition of fibrinolytic activity important for the fibrin plate. This inhibition of plasmin activity results from a decrease in the liberation of t-PA at the cellular level and a significant increase in its inhibitor, plasminogen activator inhibitor (PAI-1), and occurs without any modification in the normal values of alpha-2 antiplasmin. These results lead us to consider that GSH could play an essential role in regulation of the different components of the fibrinolytic system.
Following an administration of BSO, to rabbits at a dose of 4.5 mmol/kg body weight liver, it was seen that GSH concentrations were reduced, with the greatest decrease (51%) occurring 7 hours after administration and with values that remained lowered after 24 hours; however, at 3 days posttreatment, GSH concentrations did not significantly differ from those in the control groups. Treatment with diethyl maleate, at a dose of 3.2 mmol/kg body weight, also induced a significant reduction in hepatic GSH levels that were 54% lower than those of the controls, after 45 minutes. GSH concentrations in the aortic arch were equally reduced (0.24 ± 0.05 μmol/g liver and 0.20 ± 0.04 μmol/g liver) 7 hours after BSO or 45 minutes after diethyl maleate were administered, respectively; concentration in the control group was 0.33 ± 0.04 μmol/g liver).62
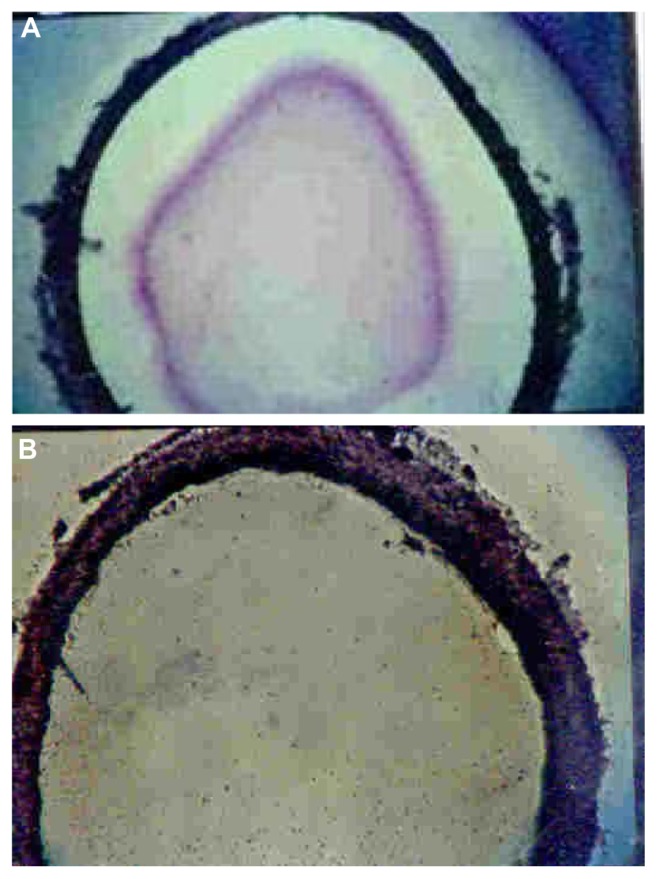
A study of the fibrinolytic activity in the aortic arch revealed an extensive area of lysis in the endothelial wall in the control rabbit groups.62 Following an administration of BSO, fibrinolysis was inhibited (Figure 1A and B) and only reappeared 3 days later. Intraperitoneal injection of diethyl maleate also induced significant inhibition activity in the aorta.
Figure 1.
Inhibition of fibrinolytic activity by BSO, on arterial walls in rabbits. Photomicrographs of 30 μm cross sections of the aortic arch that were incubated with fibrinogen, plasminogen, and human thrombin and stained with Harris’ hematoxylin (×40). (A) Fibrinolytic activity of the aortic arch reveals an extensive area of lysis under the endothelial wall. (B) Seven hours after BSO administration, the inhibited fibrinolysis activity could be attributed to a lower release of t-PA.
Note: Plasma t-PA levels were decreased following administration of BSO and only reappeared 3 days later, when the level of plasma glutathione was also normal.62
Abbreviations: BSO, buthionine sulfoximine; t-PA, tissue plasminogen activator.
Another similar study of the blood components in the fibrinolytic system revealed a significant reduction in t-PA activity (−29% and −22%) and a significant increase in PAI-1 activity (+61% and +27%), following a treatment with BSO or diethyl maleate, respectively. Alpha-2-antiplasmin was not significantly affected by the administration of either GSH-depleting agents.62
Plasminogen/plasmin systems in AD
The plasminogen system is a group of mechanisms whose interaction leads to the production of a protease involved in degrading substrates and avoiding their accumulation, and which is regulated by specific inhibitors.84 The cerebral plasminogen system does not differ from the systemic plasminogen system, as all the constituents of the systemic mechanism are present in the brain.85
Ab is the target for proteolytic degradation by several proteases known as the Ab-degrading proteases.86 Among the different, best-known Ab-degrading proteases are: neprilysin,12,87,92 insulin-degrading enzyme,93,94 endothelin converting enzyme,93,95,96 matrix metalloprotease,97–99 and plasmin.100–102 Of greatest interest to the study of Ab clearance and elimination through the BBB, are neprilysin79,88,89,103,104 and plasmin.105
The plasminogen system is an essential proteolytic mechanism that, by the action of plasmin, effectively degrades Ab peptides (beta-amyloidolysis), prompting us to consider this physiologic process as a preventive mechanism of neurodegenerative processes.19,106 Nevertheless, the primary substrate of degradation by plasmin in the brain is not very well known.107 Plasmin activity is diminished in the hippocampus and cortex of patients with AD.12,108 As mentioned earlier, the excessive production and lack of clearance of the peptide Ab creates the accumulation of senile plaques that define AD.18
A decrease in brain plasmin activity leads to a smaller clearance and an increase in the Ab deposits.15,16 Experimental studies in mice have shown an increase of Ab material deposits and an increase of PAI-1 in the process of AD.88,89 Therefore, the inhibition of the t-PA by the PAI-1 facilitates the accumulation of Ab material and slows its degradation and later clearance; very important mechanisms in the genesis of AD.18,102
For investigators, t-PA plays a significant role in the physiopathology of the central nervous system (CNS).109 At the CNS level, t-PA has a specific inhibitor, neuroserpin (NSP), which is found in those regions where t-PA is present. The coexpression of NSP and t-PA in the same regions of the brain suggests that NSP is a likely regulator of t-PA activity within the CNS. This complex t-PA/NSP contrasts with the formation of long-lasting, phyiologically irreversible complexes between t-PA and PAI-1 (due solely to differences in affinities of t-PA for PAI-1 versus NSP).110
In some studies, neurotoxicity has been attributed to the plasminogen system.111–120 In certain pathologies, such as in ischemia and cytotoxicity, activation of the plasminogen system occurs by t-PA, generating plasmin, which in turn, degrades the extracellular matrix by action on the laminin, producing neuronal loss.121 Other studies cast doubt on this action of t-PA, demonstrating that direct infusion does not lead to neuronal loss.114 Conversely, other results have conferred on t-PA a protective characteristic against cellular injury (both in vitro and in vivo)122 and considered it to be a regulator of vascular tone and permeability118 as well as a regulator of the BBB128 and a mediator in neuronal connection (synaptic plasticity).124,125 t-PA has been considered to have effects that are not related to its ability to activate plasminogen. For example, in mice lacking t-PA, neurons were found to be resistant to the damage caused by strokes.116 Further, t-PA increases microglia activation, without requiring any proteolytic activity.126 To sum up, t-PA is considered as a cerebral mediator, exercising both proteolytic and nonproteolytic actions, at a metabolic, functional, or morphological level.127
The relationship between GSH and the plasminogen system is of great importance for cerebral function. The pharmacological depletion of GSH produces a significant inhibition of the plasminogen mechanism, secondarily inhibiting the generation of plasmin. As indicated previously, the lack of plasminic activity in the brain leads to the accumulation of Ab peptides and to the formation of the extracellular plaques and intracellular tangles, found in AD.18,106 PAI-1 increases in different pathologies associated with GSH depletion and oxidative stress.128
Throughout aging, normal mice have been shown to experience a progressive decrease of t-PA activity.129,130 In parallel, lower levels of GSH have been found in the cortex, cerebellum, striatum, thalamus, and hippocampus (although hepatic levels remain normal).35,112,129 This decrease in t-PA activity found in normal mice, is due to a decrease in the expression of t-PA and to an increase in the production of PAI-1, carrying with this an increase in the production of Ab peptides.114,129,130 The same results have been found in the cerebral tissue of patients with sporadic AD, where a negative correlation between proteolytic activity and the levels of Ab peptides has been observed.15
Clinically, there is evidence to suggest that cognitive status can be improved with decreases in the concentration of Ab peptide in the cerebrospinal fluid, and that short- and long-term resistance to cognitive deterioration can be achieved with the administration of heparan sulfate-dermatan sulfate (sulodexide) (a glycosaminoglycan drug that crosses the BBB and acts by inhibiting PAI-1 and activating t-PA, with an accompanying increase in proteolytic activity).131–143 In a study conducted by us,144 two groups of patients were treated with sulodexide or with acenocoumarol. Follow up of these patients after 6 years revealed that patients treated with sulodexide experienced significantly less deterioration of cognitive status compared with the group treated with acenocumarol (Lasierra-Cirujeda, personal communication October, 2011).
In animal models as well as in clinical trials in humans, an enteral or parenteral supply of nutrients, including cysteine, methionine, N-acetyl-cysteine (NAC), and L-2- oxo-thiazolidine, were found to be suitable precursors for the synthesis of GSH and subsequently led to an increase in the intracellular level of GSH.28,51,145–147 Normalization of GSH levels improves the proteolytic cerebral capacity. After the administration of GSH to patients with diabetes mellitus type 2, a significant reduction of plasma PA-1 levels, and an increment in the concentration of GSH in blood red cells were found. These results suggest the usefulness of GSH in the improvement of the plasminogen system.148–150
Finally, the supply of GSH precursors and the resulting increase in the antioxidant GSH has been found to promote cellular resistance to oxidative stress, by leading to an intra-and extracellular proteolytic improvement caused by both the decrease in PAI-1 and the increased clearance of the cerebral Ab proteins.150,151
In this review, we hypothesized the importance of the interaction between cerebral GSH and plasminogen systems in neurodegenerative diseases. In summary, the cerebral GSH and plasminogen systems are essential biological processes that combat the neurodegenerative processes that occur more significantly with advancing age. With knowledge of the physiopathology of neurodegenerative processes, both of these systems can be pharmacological targets, providing reason for hope of prevention of neurodegenerative diseases such as AD.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Delacourte A, Defossez A. Alzheimer’s disease: Tau proteins, the promoting factors of microtubule assembly, are major components of paired helical filaments. J Neurol Sci. 1986;76(2–3):173–186. doi: 10.1016/0022-510x(86)90167-x. [DOI] [PubMed] [Google Scholar]
- 2.Kosik KS, Joachim CL, Selkoe DJ. Microtubule-associated protein tau (tau) is a major antigenic component of paired helical filament in Alzheimer disease. Proc Natl Acad Sci U S A. 1986;83(11):4044–4048. doi: 10.1073/pnas.83.11.4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flament S, Delacourte A, Hémon B, Défossez A. Characterization of two pathological tau protein, variants in Alzheimer brain cortices. J Neurol Sci. 1989;92(2–3):133–141. doi: 10.1016/0022-510x(89)90131-7. [DOI] [PubMed] [Google Scholar]
- 4.Lee VM, Balin BJ, Otvos L, Jr, Trojanowski JQ. A68: a major subunit of paired helical filaments and derivatized forms of normal Tau. Science. 1991;251(4994):675–678. doi: 10.1126/science.1899488. [DOI] [PubMed] [Google Scholar]
- 5.Hasegawa M, Morishima-Kawashima M, Takio K, Suzuki M, Titani K, Ihara Y. Protein sequence and mass spectrometric analyses of tau in the Alzheimer’s disease brain. J Biol Chem. 1992;267(24):17047–17054. [PubMed] [Google Scholar]
- 6.Sergeant N, Bussière T, Vermersch P, Lejeune JP, Delacourte A. Isoelectric point differentiates PHF-tau from biopsy-derived human brain tau proteins. Neuroreport. 1995;6(16):2217–22120. doi: 10.1097/00001756-199511000-00028. [DOI] [PubMed] [Google Scholar]
- 7.Glenner GG, Wong CW. Alzheimer’s disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun. 1984;120(3):885–890. doi: 10.1016/s0006-291x(84)80190-4. [DOI] [PubMed] [Google Scholar]
- 8.Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natl Acad Sci U S A. 1985;82(12):4245–4249. doi: 10.1073/pnas.82.12.4245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selkoe DJ. Translating cell biology into therapeutic advances in Alzheimer’s disease. Nature. 1999;399(Suppl 6738):S23–S31. doi: 10.1038/399a023. [DOI] [PubMed] [Google Scholar]
- 10.Selkoe DJ. Towards a comprehensive theory for Alzheimer’s disease. Hypothesis: Alzheimer’s disease is caused by the cerebral accumulation and cytotoxicity of amyloid beta-protein. Ann N Y Acad Sci. 2000;924:17–25. doi: 10.1111/j.1749-6632.2000.tb05554.x. [DOI] [PubMed] [Google Scholar]
- 11.Selkoe DJ. Clearing the brain’s amyloid cobwebs. Neuron. 2001;32(2):177–180. doi: 10.1016/s0896-6273(01)00475-5. [DOI] [PubMed] [Google Scholar]
- 12.Iwata N, Tsubuki S, Takaki Y, et al. Metabolic regulation of brain Abeta by neprilysin. Science. 2001;292(5521):1550–1552. doi: 10.1126/science.1059946. [DOI] [PubMed] [Google Scholar]
- 13.Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 14.Saido TC. Alzheimer’s disease as proteolytic disorders: anabolism and catabolism of beta-amyloid. Neurobiol Aging. 1998;19(Suppl 1):S69–S75. doi: 10.1016/s0197-4580(98)00033-5. [DOI] [PubMed] [Google Scholar]
- 15.Zlokovic BV. Clearing amyloid through the blood-brain barrier. J Neurochem. 2004;89(4):807–811. doi: 10.1111/j.1471-4159.2004.02385.x. [DOI] [PubMed] [Google Scholar]
- 16.Tanzi RE, Moir RD, Wagner SL. Clearance of Alzheimer’s Abeta peptide: the many roads to perdition. Neuron. 2004;43(5):605–608. doi: 10.1016/j.neuron.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 17.Holtzman DM, Zlokovic B. Role of Aβ transport and clearance in the pathogenesis and treatment of Alzheimer’s disease. In: Sisodia SS, Tanzi RE, editors. Alzheimer’s Disease: Advances in Genetics, Molecular and Cellular Biology. New York: Springer; 2007. pp. 179–198. [Google Scholar]
- 18.Melchor JP, Pawlak R, Strickland S. The tissue plasminogen activator- plasminogen proteolytic cascade accelerates amyloid-beta (Abeta) degradation and inhibits Abeta-induced neurodegeneration. J Neurosci. 2003;23(26):8867–8871. doi: 10.1523/JNEUROSCI.23-26-08867.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Strooper B. Proteases and proteolysis in Alzheimer disease: a multifactorial view on the disease process. Physiol Rev. 2010;90(2):465–494. doi: 10.1152/physrev.00023.2009. [DOI] [PubMed] [Google Scholar]
- 20.Jones DP. Redox potential of GSH/GSSG couple: assay and biological significance. Methods Enzymol. 2002;348:93–112. doi: 10.1016/s0076-6879(02)48630-2. [DOI] [PubMed] [Google Scholar]
- 21.Griffith OW. Mechanism of action, metabolism, and toxicity of buthionine sulfoximine and its higher homologs, potent inhibitors of glutathione synthesis. J Biol Chem. 1982;257(22):13704–13712. [PubMed] [Google Scholar]
- 22.Meister A, Anderson ME. Glutathione. Annu Rev Biochem. 1983;52:711–760. doi: 10.1146/annurev.bi.52.070183.003431. [DOI] [PubMed] [Google Scholar]
- 23.Lu SC. Regulation of glutathione synthesis. Curr Top Cell Regul. 2000;36:95–116. doi: 10.1016/s0070-2137(01)80004-2. [DOI] [PubMed] [Google Scholar]
- 24.Griffith OW, Meister A. Potent and specific inhibition of glutathione synthesis by buthionine sulfoximine (S-n-butyl homocysteine sulfoximine) J Biol Chem. 1979;254(16):7558–7560. [PubMed] [Google Scholar]
- 25.Bains JS, Shaw CA. Neurodegenerative disorders in humans: the role of glutathione in oxidative stress-mediated neuronal death. Brain Res Brain Res Rev. 1997;25(3):335–358. doi: 10.1016/s0165-0173(97)00045-3. [DOI] [PubMed] [Google Scholar]
- 26.Lu SC. Regulation of hepatic glutathione synthesis: current concepts and controversies. FASEB J. 1999;13(10):1169–1183. [PubMed] [Google Scholar]
- 27.Griffith OW. Biologic and pharmacologic regulation of mammalian glutathione synthesis. Free Radic Biol Med. 1999;27(9–10):922–935. doi: 10.1016/s0891-5849(99)00176-8. [DOI] [PubMed] [Google Scholar]
- 28.Wu G, Fang YZ, Yang S, Lupton JR, Turner ND. Glutathione metabolism and its implications for health. J Nutr. 2004;134(3):489–492. doi: 10.1093/jn/134.3.489. [DOI] [PubMed] [Google Scholar]
- 29.Butterfield DA, Perluigi M, Sultana R. Oxidative stress in Alzheimer’s disease brain: new insights from redox proteomics. Eur J Pharmacol. 2006;545(1):39–50. doi: 10.1016/j.ejphar.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 30.Dringen R, Gutterer JM, Hirrlinger J. Glutathione metabolism in brain metabolic interaction between astrocytes and neurons in the defense against reactive oxygen species. Eur J Biochem. 2000;267(16):4912–4916. doi: 10.1046/j.1432-1327.2000.01597.x. [DOI] [PubMed] [Google Scholar]
- 31.Philbert MA, Beiswanger CM, Waters DK, Reuhl KR, Lowndes HE. Cellular and regional distribution of reduced glutathione in the nervous system of the rat: histochemical localization by mercury orange and o-phthaldialdehyde-induced histofluorescence. Toxicol Appl Pharmacol. 1991;107(2):215–227. doi: 10.1016/0041-008x(91)90204-r. [DOI] [PubMed] [Google Scholar]
- 32.Zhu Y, Carvey PM, Ling Z. Age-related changes in glutathione and glutathione- related enzymes in rat brain. Brain Res. 2006;1090(1):35–44. doi: 10.1016/j.brainres.2006.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu H, Wang H, Shenvi S, Hagen TM, Liu RM. Glutathione metabolism during aging and in Alzheimer disease. Ann N Y Acad Sci. 2004;1019:346–349. doi: 10.1196/annals.1297.059. [DOI] [PubMed] [Google Scholar]
- 34.Hjelle OP, Chaudhry FA, Ottersen OP. Antisera to glutathione: characterization and immunocytochemical application to the rat cerebellum. Eur J Neurosci. 1994;6(5):793–804. doi: 10.1111/j.1460-9568.1994.tb00990.x. [DOI] [PubMed] [Google Scholar]
- 35.Ravindranath V, Shivakumar BR, Anandatheerthavarada HK. Low glutathione levels in brain regions of aged rats. Neurosci Lett. 1989;101(2):187–190. doi: 10.1016/0304-3940(89)90528-4. [DOI] [PubMed] [Google Scholar]
- 36.Makar TK, Nedergaard M, Preuss A, Gelbard AS, Perumal AS, Cooper AJ. Vitamin E ascorbate, glutathione, glutathione disulfide, and enzymes of glutathione metabolism in cultures of chick astrocytes and neurons: evidence that astrocytes play an important role in antioxidative processes in the brain. J Neurochem. 1994;62(1):45–53. doi: 10.1046/j.1471-4159.1994.62010045.x. [DOI] [PubMed] [Google Scholar]
- 37.Cooper AJL. Glutathione in the brain: disorders of glutathione metabolism. In: Rosenberg RN, Prusiner SB, DiMauro S, Barchi RL, Kunk LM, editors. The Molecular and Genetic Basis of Neurological Disease. Boston: Butterworth-Heinemann; 1997. pp. 1195–1230. [Google Scholar]
- 38.Keelan J, Allen NJ, Antcliffe D, Pal S, Duchen MR. Quantitative imaging of glutathione in hippocampal neurons and glia in culture using monochlorobimane. J Neurosci Res. 2001;66(5):873–884. doi: 10.1002/jnr.10085. [DOI] [PubMed] [Google Scholar]
- 39.Raps SP, Lai JC, Hertz L, Cooper AJ. Glutathione is present in high concentrations in cultured astrocytes but not in cultured neurons. Brain Res. 1989;493(2):398–401. doi: 10.1016/0006-8993(89)91178-5. [DOI] [PubMed] [Google Scholar]
- 40.Pileblad E, Eriksson PS, Hansson E. The presence of glutathione in primary neuronal and astroglial cultures from rat cerebral cortex and brain stem. J Neural Transm Gen Sect. 1991;86(1):43–49. doi: 10.1007/BF01250374. [DOI] [PubMed] [Google Scholar]
- 41.Devesa A, O’Connor JE, Garciá C, Puertes IR, Viña JR. Glutathione metabolism in primary astrocyte cultures: flow cytometric evidence of heterogeneous distribution of GSH content. Brain Res. 1993;618(2):181–189. doi: 10.1016/0006-8993(93)91264-s. [DOI] [PubMed] [Google Scholar]
- 42.Dringen R, Hamprecht B. Glutathione content as an indicator for the presence of metabolic pathways of amino acids in astroglial cultures. J Neurochem. 1996;67(4):1375–1382. doi: 10.1046/j.1471-4159.1996.67041375.x. [DOI] [PubMed] [Google Scholar]
- 43.Sagara JI, Miura K, Bannai S. Maintenance of neuronal glutathione by glial cells. J Neurochem. 1993;61(5):1672–1676. doi: 10.1111/j.1471-4159.1993.tb09802.x. [DOI] [PubMed] [Google Scholar]
- 44.Byrd AS, Sikorska M, Walker PR, Sandhu JK. Effects of glutathione depletion on the viability of human NT2-derived neuronal and astroglial cultures. Neuron Glia Biol. 2004;1(4):317–326. doi: 10.1017/S1740925X05000207. [DOI] [PubMed] [Google Scholar]
- 45.Langeveld CH, Schepens E, Jongenelen CA, et al. Presence of glutathione immunoreactivity in cultured neurones and astrocytes. Neuroreport. 1996;7(11):1833–1836. doi: 10.1097/00001756-199607290-00029. [DOI] [PubMed] [Google Scholar]
- 46.Clarke DD, Sokoloff L. Circulation and energy metabolism of the brain. In: Siegel GJ, Agranoff BW, Albers RW, Fisher SK, Uhler MD, editors. Basic Neurochemistry: Molecular, Cellular and Medical Aspects. 6th ed. Philadelphia: Lippincott-Raven; 1999. pp. 637–669. [Google Scholar]
- 47.Kranich O, Dringen R, Sandberg M, Hamprecht B. Utilization of cysteine and cysteine precursors for the synthesis of glutathione in astroglial cultures: preference for cystine. Glia. 1998;22(1):11–18. [PubMed] [Google Scholar]
- 48.Dringen R, Pfeiffer B, Hamprecht B. Synthesis of the antioxidant glutathione in neurons: supply by astrocytes of CysGly as precursor for neuronal glutathione. J Neurosci. 1999;19(2):562–569. doi: 10.1523/JNEUROSCI.19-02-00562.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dringen R, Hirrlinger J. Glutathione pathways in the brain. Biol Chem. 2003;384(4):505–516. doi: 10.1515/BC.2003.059. [DOI] [PubMed] [Google Scholar]
- 50.Barkats M, Millecamps S, Abrioux P, Geoffroy MC, Mallet J. Overexpression of glutathione peroxidase increases the resistance of neuronal cells to Abeta-mediated neurotoxicity. J Neurochem. 2000;75(4):1438–1446. doi: 10.1046/j.1471-4159.2000.0751438.x. [DOI] [PubMed] [Google Scholar]
- 51.Pocernich CB, La Fontaine M, Butterfield DA. In-vivo glutathione elevation protects against hydroxyl free radical-induced protein oxidation in rat brain. Neurochem Int. 2000;36(3):185–191. doi: 10.1016/s0197-0186(99)00126-6. [DOI] [PubMed] [Google Scholar]
- 52.James SJ, Slikker W, 3rd, Meinyk S, New E, Pogribna M, Jernigan S. Thimerosal neurotoxicity is associated with glutathione depletion: protection with glutathione precursors. Neurotoxicology. 2005;26(1):1–8. doi: 10.1016/j.neuro.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 53.Aoyama K, Suh SW, Hamby AM, et al. Neuronal glutathione deficiency and age-dependent neurodegeneration in the EAAC1 deficient mouse. Nat Neurosci. 2006;9(1):119–126. doi: 10.1038/nn1609. [DOI] [PubMed] [Google Scholar]
- 54.Zhu M, Bowden GT. Molecular mechanism(s) for UV-B irradiationinduced glutathione depletion in cultured human keratinocytes. Photochem Photobiol. 2004;80(2):191–196. doi: 10.1562/2004-02-26-RA-091. [DOI] [PubMed] [Google Scholar]
- 55.Halliwell B, Gutteridge J. Free Radicals in Biology and Medicine. 4th ed. Oxford: Oxford University Press; 2007. [Google Scholar]
- 56.Hartman D. Free radical theory of aging: Alzheimer’s disease pathogenesis. Age. 1995;18(3):97–119. [Google Scholar]
- 57.Sohal RS, Weindruch R. Oxidative stress, caloric restriction, and aging. Science. 1996;273(5271):59–63. doi: 10.1126/science.273.5271.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ames BN, Shigenaga MK, Hagen TM. Oxidants, antioxidants, and the degenerative diseases of aging. Proc Natl Acad Sci U S A. 1993;90(17):7915–7922. doi: 10.1073/pnas.90.17.7915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schulz JB, Lindenau J, Seyfried J, Dichgans J. Glutathione, oxidative stress and neurodegeneration. Eur J Biochem. 2000;267(16):4904–4911. doi: 10.1046/j.1432-1327.2000.01595.x. [DOI] [PubMed] [Google Scholar]
- 60.Mecocci P, MacGarvey U, Kaufman AE, et al. Oxidative damage to mitochondrial DNA shows marked age-dependent increases in human brain. Ann Neurol. 1993;34(4):609–616. doi: 10.1002/ana.410340416. [DOI] [PubMed] [Google Scholar]
- 61.Mecocci P, Beal MF, Cecchetti R, et al. Mitochondrial membrane fluidity and oxidative damage to mitochondrial DNA in aged and AD human brain. Mol Chem Neuropathol. 1997;31(1):53–64. doi: 10.1007/BF02815160. [DOI] [PubMed] [Google Scholar]
- 62.Lasierra J, Aza MJ, Collado PS, González J, Esteller A. Inhibition of fibrinolysis by cellular glutathione depletion in the rabbit. Thromb Res. 1989;53(4):347–355. doi: 10.1016/0049-3848(89)90313-7. [DOI] [PubMed] [Google Scholar]
- 63.Aza MJ, Gonzalez J, Esteller A. Effect of diethyl maleate pretreatment on biliary excretion and choleretic action of sulfobromophthalein in rats. Arch Int Pharmacodyn Ther. 1986;281(2):321–330. [PubMed] [Google Scholar]
- 64.Kaplowitz N, Aw TY, Ookhtens M. The regulation of hepatic glutathione. Annu Rev Pharmacol Toxicol. 1985;25:715–744. doi: 10.1146/annurev.pa.25.040185.003435. [DOI] [PubMed] [Google Scholar]
- 65.Masukawa T, Sai M, Tochino Y. Methods for depleting brain glutathione. Life Sci. 1989;44(6):417–424. doi: 10.1016/0024-3205(89)90266-x. [DOI] [PubMed] [Google Scholar]
- 66.Jain A, Mårtensson J, Stole E, Auld PA, Meister A. Glutathione deficiency leads to mitochondrial damage in brain. Proc Natl Acad Sci U S A. 1991;88(5):1913–1917. doi: 10.1073/pnas.88.5.1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pileblad E, Magnusson T. Intracerebroventricular administration of L-buthionine sulfoximine: a method for depleting brain glutathione. J Neurochem. 1989;53(6):1878–1882. doi: 10.1111/j.1471-4159.1989.tb09256.x. [DOI] [PubMed] [Google Scholar]
- 68.Pellegrino LJ, Pellegrino AS, Cushman AJ. A Stereotaxic Atlas of the Rat Brain. 2nd ed. New York: Plenum Press; 1979. [Google Scholar]
- 69.Shivakumar BR, Ravindranath V. Selective modulation of glutathione in mouse brain regions and its effect on acrylamide-induced neurotoxicity. Biochem Pharmacol. 1992;43(2):263–269. doi: 10.1016/0006-2952(92)90287-s. [DOI] [PubMed] [Google Scholar]
- 70.Lee M, Cho T, Jantaratnotai N, Wang YT, McGeer E, McGeer PL. Depletion of GSH in glial cells induces neurotoxicity: relevance to aging and degenerative neurological diseases. FASEB J. 2010;24(7):2533–2545. doi: 10.1096/fj.09-149997. [DOI] [PubMed] [Google Scholar]
- 71.Mãrtensson J, Meister A. Glutathione deficiency decreases tissue ascorbate levels in newborn rats: ascorbate spares glutathione and protects. Proc Natl Acad Sci U S A. 1991;88(11):4656–4660. doi: 10.1073/pnas.88.11.4656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barker JE, Heales SJ, Cassidy A, Bolaños JP, Land JM, Clark JB. Depletion of brain glutathione results in a decrease of glutathione reductase activity; an enzyme susceptible to oxidative damage. Brain Res. 1996;716(1–2):118–122. doi: 10.1016/0006-8993(96)00003-0. [DOI] [PubMed] [Google Scholar]
- 73.Mizui T, Kinouchi H, Chan PH. Depletion of brain glutathione by buthionine sulfoximine enhances cerebral ischemic injury in rats. Am J Physiol. 1992;262(2 Pt 2):H313–H317. doi: 10.1152/ajpheart.1992.262.2.H313. [DOI] [PubMed] [Google Scholar]
- 74.Mytilineou C, Leonardi EK, Radcliffe P, et al. Deprenyl and desmethylselegiline protect mesencephalic neurons from toxicity induced by glutathione depletion. J Pharmacol Exp Ther. 1998;284(2):700–706. [PubMed] [Google Scholar]
- 75.Li Y, Maher P, Schubert D. A role for 12-lipoxygenase in nerve cell death caused by glutathione depletion. Neuron. 1997;19(2):453–463. doi: 10.1016/s0896-6273(00)80953-8. [DOI] [PubMed] [Google Scholar]
- 76.Meister A. Glutathione deficiency produced by inhibition of its synthesis, and its reversal; applications in research and therapy. Pharmacol Ther. 1991;51(2):155–194. doi: 10.1016/0163-7258(91)90076-x. [DOI] [PubMed] [Google Scholar]
- 77.Sandhu JK, Gardaneh M, Iwasiow R, et al. Astrocyte-secreted GDNF and glutathione antioxidant system protect neurons against 6OHDA cytotoxicity. Neurobiol Dis. 2009;33(3):405–414. doi: 10.1016/j.nbd.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 78.Cudkowicz ME, Sexton PM, Ellis T, et al. The pharmacokinetics and pharmaco-dynamics of Procysteine in amyotrophic lateral sclerosis. Neurology. 1999;52(7):1492–1494. doi: 10.1212/wnl.52.7.1492. [DOI] [PubMed] [Google Scholar]
- 79.Christen Y. Oxidative stress and Alzheimer disease. Am J Clin Nutr. 2000;71(2):621S–629S. doi: 10.1093/ajcn/71.2.621s. [DOI] [PubMed] [Google Scholar]
- 80.Lovell MA, Xie C, Markesbery WR. Decreased glutathione transferase activity in brain and ventricular fluid in Alzheimer’s disease. Neurology. 1998;51(6):1562–1566. doi: 10.1212/wnl.51.6.1562. [DOI] [PubMed] [Google Scholar]
- 81.Todd AS. The histological localisation of fibrinolysin activator. J Pathol Bacteriol. 1959;78:281–283. doi: 10.1002/path.1700780131. [DOI] [PubMed] [Google Scholar]
- 82.Loskutoff DJ, Edgington TE. Synthesis of a fibrinolytic activator and inhibitor by endothelial cells. Proc Natl Acad Sci U S A. 1977;74(9):3903–3907. doi: 10.1073/pnas.74.9.3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Larsson A, Astedt B. Immunohistochemical localisation of tissue plasminogen activator and urokinase in the vessel wall. J Clin Pathol. 1985;38(2):140–145. doi: 10.1136/jcp.38.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Collen D. The plasminogen (fibrinolytic) system. Thromb Haemost. 1999;82(2):259–270. [PubMed] [Google Scholar]
- 85.Hino H, Akiyama H, Iseki E, et al. Immunohistochemical localization of plasminogen activator inhibitor-1 in rat and human brain tissues. Neurosci Lett. 2001;297(2):105–108. doi: 10.1016/s0304-3940(00)01679-7. [DOI] [PubMed] [Google Scholar]
- 86.Saido T, Leissring MA. Proteolytic degradation of amyloid b-protein. Cold Spring Harb Perspect Med. 2012;2(6):a006379. doi: 10.1101/cshperspect.a006379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Howell S, Nalbantoglu J, Crine P. Neutral endopeptidase can hydrolyze beta-amyloid(1–40) but shows no effect on beta-amyloid precursor protein metabolism. Peptides. 1995;16(4):647–652. doi: 10.1016/0196-9781(95)00021-b. [DOI] [PubMed] [Google Scholar]
- 88.Shirotani K, Tsubuki S, Iwata N, et al. Neprilysin degrades both amyloid beta peptides 1–40 and 1–42 most rapidly and efficiently among thiorphan- and phosphoramidon-sensitive endopeptidases. J Biol Chem. 2001;276(24):21895–21901. doi: 10.1074/jbc.M008511200. [DOI] [PubMed] [Google Scholar]
- 89.Marr RA, Rockenstein E, Mukherjee A, et al. Neprilysin gene transfer reduces human amyloid pathology in transgenic mice. J Neurosci. 2003;23(6):1992–1996. doi: 10.1523/JNEUROSCI.23-06-01992.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Eckeman EA, Eckman CB. Abeta-degrading enzymes: modulators of Alzheimer’s disease pathogenesis and targets for therapeutic intervention. Biochem Soc Trans. 2005;33(Pt 5):1101–1105. doi: 10.1042/BST20051101. [DOI] [PubMed] [Google Scholar]
- 91.Hersh LB, Rodgers DW. Neprilysin and amyloid beta peptide degradation. Curr Alzheimer Res. 2008;5(2):225–231. doi: 10.2174/156720508783954703. [DOI] [PubMed] [Google Scholar]
- 92.Eckman EA, Adams SK, Troendle FJ, et al. Regulation of steady- state beta-amyloid levels in the brain by neprilysin and endothelin- converting enzyme but not angiotensin-converting enzyme. J Biol Chem. 2006;281(41):30471–30478. doi: 10.1074/jbc.M605827200. [DOI] [PubMed] [Google Scholar]
- 93.Authier F, Posner BI, Bergeron JJ. Insulin-degrading enzyme. Clin Invest Med. 1996;19(3):149–160. [PubMed] [Google Scholar]
- 94.de Tullio MB, Morelli L, Castaño EM. The irreversible binding of amyloid peptide substrates to insulin-degrading enzyme: a biological perspective. Prion. 2008;2(2):51–56. doi: 10.4161/pri.2.2.6710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Eckman EA, Reed DK, Eckman CB. Degradation of the Alzheimer’s amyloid beta peptide by endothelin-converting enzyme. J Biol Chem. 2001;276(27):24540–24548. doi: 10.1074/jbc.M007579200. [DOI] [PubMed] [Google Scholar]
- 96.Eckman EA, Watson M, Marlow L, Sambamurti K, Eckman CB. Alzheimer’s disease beta-amyloid peptide is increased in mice deficient in endothelin-converting enzyme. J Biol Chem. 2003;278(4):2081–2084. doi: 10.1074/jbc.C200642200. [DOI] [PubMed] [Google Scholar]
- 97.Yan P, Hu X, Song H, et al. Matrix metalloproteinase-9 degrades amyloid-beta fibrils in vitro and compact plaques in situ. J Biol Chem. 2006;281(34):24566–24574. doi: 10.1074/jbc.M602440200. [DOI] [PubMed] [Google Scholar]
- 98.Liao MC, Van Nostrand WE. Degradation of soluble and fibrillar amyloid beta-protein by matrix metalloproteinase (MT1-MMP) in vitro. Biochemistry. 2010;49(6):1127–1136. doi: 10.1021/bi901994d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hernandez-Guillamon M, Mawhirt S, Fossati S, et al. Matrix metalloproteinase 2 (MMP-2) degrades soluble vasculotropic amyloid-beta E22Q and L34V mutants, delaying their toxicity for human brain microvascular endothelial cells. J Biol Chem. 2010;285(35):27144–27158. doi: 10.1074/jbc.M110.135228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Van Nostrand WE, Porter M. Plasmin cleavage of the amyloid beta- protein: alteration of secondary structure and stimulation of tissue plasminogen activator activity. Biochemistry. 1999;38(35):11570–11576. doi: 10.1021/bi990610f. [DOI] [PubMed] [Google Scholar]
- 101.Tucker HM, Kihiko M, Caldwell JN, et al. The plasmin system is induced by and degrades amyloid-beta aggregates. J Neurosci. 2000;20(11):3937–3946. doi: 10.1523/JNEUROSCI.20-11-03937.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jacobsen JS, Comery TA, Martone RL, et al. Enhanced clearance of Abeta in brain by sustaining the plasmin proteolysis cascade. Proc Natl Acad Sci U S A. 2008;105(25):8754–8759. doi: 10.1073/pnas.0710823105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Leissring MA, Farris W, Chang AY, et al. Enhanced proteolysis of beta- amyloid in APP transgenic mice prevents plaque formation, secondary pathology, and premature death. Neuron. 2003;40(6):1087–1093. doi: 10.1016/s0896-6273(03)00787-6. [DOI] [PubMed] [Google Scholar]
- 104.Caccamo A, Oddo S, Sugarman MC, Akbari Y, LaFerla FM. Age-and region-dependent alterations in Abeta-degrading enzymes: implications for Abeta-induced disorders. Neurobiol Aging. 2005;26(5):645–654. doi: 10.1016/j.neurobiolaging.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 105.Tucker HM, Kihiko-Ehmann M, Wright S, Rydel RE, Estus S. Tissue plasminogen activator requires plasminogen to modulate amyloid-beta neurotoxicity and deposition. J Neurochem. 2000;75(5):2172–2177. doi: 10.1046/j.1471-4159.2000.0752172.x. [DOI] [PubMed] [Google Scholar]
- 106.Ledesma MD, Da Silva JS, Crassaerts K, Delacourte A, De Strooper B, Dotti CG. Brain plasmin enhances APP alpha-cleavage and Abeta degradation and is reduced in Alzheimer’s disease brains. EMBO Rep. 2000;1(6):530–535. doi: 10.1093/embo-reports/kvd107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yepes M, Lawrence DA. New functions for an old enzyme: nonhemostatic roles for tissue-type plasminogen activator in the central nervous system. Exp Biol Med (Maywood) 2004;229(11):1097–1104. doi: 10.1177/153537020422901103. [DOI] [PubMed] [Google Scholar]
- 108.Ledesma MD, Abad-Rodriguez J, Galvan C, et al. Raft disorganization leads to reduced plasmin activity in Alzheimer’s disease brains. EMBO Rep. 2003;4(12):1190–1196. doi: 10.1038/sj.embor.7400021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Strickland S. Tissue plasminogen activator in nervous system function and dysfunction. Thromb Haemost. 2001;86(1):138–143. [PubMed] [Google Scholar]
- 110.Barker-Carlson K, Lawrence DA, Schwartz BS. Acyl-enzyme complexes between tissue-type plasminogen activator and neuroserpin are short-lived in vitro. J Biol Chem. 2002;277(49):46852–46857. doi: 10.1074/jbc.M207740200. [DOI] [PubMed] [Google Scholar]
- 111.Davies BJ, Pickard BS, Steel M, Morris RG, Lathe R. Serine proteases in rodent hippocampus. J Biol Chem. 1998;273(36):23004–23011. doi: 10.1074/jbc.273.36.23004. [DOI] [PubMed] [Google Scholar]
- 112.Tsirka SE, Rogove AD, Bugge TH, Degen JL, Strickland S. An extracellular proteolytic cascade promotes neuronal degeneration in the mouse hippocampus. J Neurosci. 1997;17(2):543–552. doi: 10.1523/JNEUROSCI.17-02-00543.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Siao CJ, Fernandez SR, Tsirka SE. Cell type-specific roles for tissue plasminogen activator released by neurons or microglia after excitotoxic injury. J Neurosci. 2003;23(8):3234–3242. doi: 10.1523/JNEUROSCI.23-08-03234.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chen ZL, Strickland S. Neuronal death in the hippocampus is promoted by plasmin-catalyzed degradation of laminin. Cell. 1997;91(7):917–925. doi: 10.1016/s0092-8674(00)80483-3. [DOI] [PubMed] [Google Scholar]
- 115.Tsirka SE, Rogove AD, Strickland S. Neuronal cell death and tPA. Nature. 1996;384(6605):123–124. doi: 10.1038/384123b0. [DOI] [PubMed] [Google Scholar]
- 116.Wang YF, Tsirka SE, Strickland S, Stieg PE, Soriano SG, Lipton SA. Tissue plasminogen activator (tPA) increases neuronal damage after focal cerebral ischemia in wild-type and tPA-deficient mice. Nat Med. 1998;4(2):228–231. doi: 10.1038/nm0298-228. [DOI] [PubMed] [Google Scholar]
- 117.Nagai N, De Mol M, Lijnen HR, Carmeliet P, Collen D. Role of plasminogen system components in focal cerebral ischemic infarction: a gene targeting and gene transfer study in mice. Circulation. 1999;99(18):2440–2444. doi: 10.1161/01.cir.99.18.2440. [DOI] [PubMed] [Google Scholar]
- 118.Nicole O, Docagne F, Ali C, et al. The proteolytic activity of tissue- plasminogen activator enhances NMDA receptor-mediated signaling. Nat Med. 2001;7(1):59–64. doi: 10.1038/83358. [DOI] [PubMed] [Google Scholar]
- 119.Yepes M, Sandkvist M, Coleman TA, et al. Regulation of seizure spreading by neuroserpin and tissue-type plasminogen activator is plasminogen-independent. J Clin Invest. 2002;109(12):1571–1578. doi: 10.1172/JCI14308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Medina MG, Ledesma MD, Domínguez JE, et al. Tissue plasminogen activator mediates amyloid-induced neurotoxicity via Erk1/2 activation. EMBO J. 2005;24(9):1706–1716. doi: 10.1038/sj.emboj.7600650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lijnen HR, Silence J, Lemmens G, Frederix L, Collen D. Regulation of gelatinase activity in mice with targeted inactivation of components of the plasminogen/plasmin system. Thromb Haemost. 1998;79(6):1171–1176. [PubMed] [Google Scholar]
- 122.Kim YH, Park JH, Hong SH, Koh JY. Nonproteolytic neuroprotection by human recombinant tissue plasminogen activator. Science. 1999;284(5414):647–650. doi: 10.1126/science.284.5414.647. [DOI] [PubMed] [Google Scholar]
- 123.Yepes M, Sandkvist M, Moore EG, Bugge TH, Strickland DK, Lawrence DA. Tissue-type plasminogen activator induces opening of the blood-brain barrier via the LDL receptor-related protein. J Clin Invest. 2003;112(10):1533–1540. doi: 10.1172/JCI19212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Madani R, Hulo S, Toni N, et al. Enhanced hippocampal long- term potentiation and learning by increased neuronal expression of tissue-type plasminogen activator in transgenic mice. EMBO J. 1999;18(11):3007–3012. doi: 10.1093/emboj/18.11.3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Calabresi P, Napolitano M, Centonze D, et al. Tissue plasminogen activator controls multiple forms of synaptic plasticity and memory. Eur J Neurosci. 2000;12(3):1002–1012. doi: 10.1046/j.1460-9568.2000.00991.x. [DOI] [PubMed] [Google Scholar]
- 126.Rogove AD, Siao C, Keyt B, Strickland S, Tsirka SE. Activation of microglia reveals a non-proteolytic cytokine function for tissue plasminogen activator in the central nervous system. J Cell Sci. 1999;112( Pt 22):4007–4016. doi: 10.1242/jcs.112.22.4007. [DOI] [PubMed] [Google Scholar]
- 127.Pawlak R, Rao BS, Melchor JP, Chattarji S, McEwen B, Strickland S. Tissue plasminogen activator and plasminogen mediate stress-induced decline of neuronal and cognitive functions in the mouse hippocampus. Proc Natl Acad Sci U S A. 2005;102(50):18201–18206. doi: 10.1073/pnas.0509232102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dimova EY, Samoylenko A, Kietzmann T. Oxidative stress and hypoxia: implications for plasminogen activator inhibitor-1 expression. Antioxid Redox Signal. 2004;6(4):777–791. doi: 10.1089/1523086041361596. [DOI] [PubMed] [Google Scholar]
- 129.Popa-Wagner A, Fischer B, Platt D, Schmoll H, Kessler C. Delayed and blunted induction of mRNA for tissue plasminogen activator in the brain of old rats following pentylenetetrazole-induced seizure activity. J Gerontol A Biol Sci Med Sci. 2000;55(5):B242–B248. doi: 10.1093/gerona/55.5.b242. [DOI] [PubMed] [Google Scholar]
- 130.Cacquevel M, Launay S, Castel H, et al. Ageing and amyloid- beta peptide deposition contribute to an impaired brain tissue plasminogen activator activity by different mechanisms. Neurobiol Dis. 2007;27(2):164–173. doi: 10.1016/j.nbd.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 131.Perego M, Palmieri G, Nazzari M. Effects of oral and parenteral 3-GS administration on blood lipids and haemostatic parameters in atherosclerotic hyperlipaemic patients. In: Lenzi S, Descovich CG, editors. Atherosclerosis: Etiopathogenesis, Clinical Evaluation and Therapy. Bologna: Editrice Compositori; 1982. pp. 457–463. [Google Scholar]
- 132.Bonacci C, Crolle G, Olivi A, et al. Effetti del sulodexide in pazienti anziani con vasculopatia arteriosclerotica cerebrale. [Effects of sulodexide in elderly patients with artherosclerotic cerebral vascular disease]. Acta Gerontol. 1986;36(3–4):228–235. Italian. [Google Scholar]
- 133.Capone-Braga M, Tellini L, Boncompagni L, Bettoni M, Burali A, Bensi A. Approccio terapeutico con sulodexide in pazienti con vasculopatia aterosclerotica a varia localizzazione. [Sulodexide treatment approach in patients with atherosclerotic vascular disease with various localizations]. Clin Ter. 1987;120(1):25–31. Italian. [PubMed] [Google Scholar]
- 134.Cospite M, Milio G, Ferrara F, et al. Double-blind study of the pharmacological effect of sulodexide in patients with multiple atherosclerotic vascular disease. Eur Rev Med Pharmacol Sci. 1985;7:97–106. [Google Scholar]
- 135.Bonanno G, Bonaccorso R, Dell’ali C, Salanitri G. Sulodexide in the treatment of atherosclerosis: a controlled clinical trial. Acta Therapeutica. 1985;11:87–98. [Google Scholar]
- 136.Postiglione F, Pisani P, Gisonni P, et al. Il sulodexide nella terapia delle vasculopatie. [Sulodexide in the therapy of vasculopathies]. Clin Ter. 1986;117(3):223–231. Italian. [PubMed] [Google Scholar]
- 137.Santus G, Sottini G, Lombardi G, Rozzini R, Inzoli R. L’uso del sulodexide nei vasculopatici cerebrali con dislipidemia e/o diabete:contributo clinico statistico. [Role of sulodexide in cerebral vasculopathy with dyslipidemia and/or diabetes: clinical statistical contribution]. Atherosclerosis and Cardiovascular Diseases. 1984;415:20. French. [Google Scholar]
- 138.Conti L, Re F, Lazzerini F, et al. Glycosaminoglycan polysulfate (Ateroid) in old-age dementias: effects upon depressive symptomatology in geriatric patients. Prog Neuropsychopharmacol Biol Psychiatry. 1989;13(6):977–981. doi: 10.1016/0278-5846(89)90048-1. [DOI] [PubMed] [Google Scholar]
- 139.Ban TA, Morey LC, Aguglia E, et al. Glycosaminoglycan polysulfate in the treatment of old age dementias. Prog Neuropsychopharmacol Biol Psychiatry. 1991;15(3):323–342. doi: 10.1016/0278-5846(91)90064-8. [DOI] [PubMed] [Google Scholar]
- 140.Ban TA, Morey LC, Fjetland OK, et al. Early manifestations of dementing illness: treatment with glycosaminoglycan polysulfate. Prog Neuropsychopharmacol Biol Psychiatry. 1992;16(5):661–676. doi: 10.1016/0278-5846(92)90023-8. [DOI] [PubMed] [Google Scholar]
- 141.Pollack SJ, Sadler II, Hawtin SR, Tailor VJ, Shearman MS. Sulfated glycosaminoglycans and dyes attenuate the neurotoxic effects of beta-amyloid in rat PC12 cells. Neurosci Lett. 1995;184(2):113–116. doi: 10.1016/0304-3940(94)11182-i. [DOI] [PubMed] [Google Scholar]
- 142.Parnetti L, Mari D, Abate G, et al. Vascular dementia Italian sulodexide study (VA.D.I.S.S.). Clinical and biological results. Thromb Res. 1997;87(2):225–233. doi: 10.1016/s0049-3848(97)00122-9. [DOI] [PubMed] [Google Scholar]
- 143.Aisen PS, Saumier D, Briand R, et al. A Phase II study targeting amyloid-beta with 3APS in mild-to-moderate Alzheimer disease. Neurology. 2006;67(10):1757–1763. doi: 10.1212/01.wnl.0000244346.08950.64. [DOI] [PubMed] [Google Scholar]
- 144.Lasierra-Cirujeda J, Coronel Granado P. A study on the safety, efficacy, and efficiency of sulodexide compared with acenocoumarol in secondary prophylaxis in patients with deep venous thrombosis. Angiology. 2006;57(1):53–64. doi: 10.1177/000331970605700108. [DOI] [PubMed] [Google Scholar]
- 145.Chung TK, Funk MA, Baker DH. L-2-oxothiazolidine-4-carboxylate as a cysteine precursor: efficacy for growth and hepatic glutathione synthesis in chicks and rats. J Nutr. 1990;120(2):158–165. doi: 10.1093/jn/120.2.158. [DOI] [PubMed] [Google Scholar]
- 146.Jahoor F, Jackson A, Gazzard B, et al. Erythrocyte glutathione deficiency in symptom-free HIV infection is associated with decreased synthesis rate. Am J Physiol. 1999;276(1 Pt 1):E205–E211. doi: 10.1152/ajpendo.1999.276.1.E205. [DOI] [PubMed] [Google Scholar]
- 147.Lyons J, Rauh-Pfeiffer A, Yu YM, et al. Blood glutathione synthesis rates in healthy adults receiving a sulfur amino acid-free diet. Proc Natl Acad Sci U S A. 2009;97(10):5071–5076. doi: 10.1073/pnas.090083297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Anderson ME, Luo JL. Glutathione therapy: from prodrugs to genes. Semin Liver Dis. 1998;18(4):415–424. doi: 10.1055/s-2007-1007174. [DOI] [PubMed] [Google Scholar]
- 149.Badaloo A, Reid M, Forrester T, Heird WC, Jahoor F. Cysteine supplementation improves the erythrocyte glutathione synthesis rate in children with severe edematous malnutrition. Am J Clin Nutr. 2002;76(3):646–652. doi: 10.1093/ajcn/76.3.646. [DOI] [PubMed] [Google Scholar]
- 150.Martina V, Bruno GA, Zumpano E, Origlia C, Quaranta L, Pescarmona GP. Administration of glutathione in patients with type 2 diabetes mellitus increases the platelet constitutive nitric oxide synthase activity and reduces PAI-1. J Endocriol Invest. 2001;24(1):37–41. doi: 10.1007/BF03343806. [DOI] [PubMed] [Google Scholar]
- 151.Hsu CH-CH, Yen H, Yin M, Tsai CH, Hsieh CH. Five cysteine-containing compounds delay diabetic deterioration in Balb/cA mice. J Nutr. 2004;134(12):3245–3249. doi: 10.1093/jn/134.12.3245. [DOI] [PubMed] [Google Scholar]