Abstract
Rationale
The high prevalence of smoking and low cessation rates among individuals with schizophrenia and similar conditions are not well understood. Behavioral economics has been extensively applied to studying addictive behavior and may contribute to understanding smoking in this subpopulation.
Objectives
This study compared smokers with schizophrenia or schizoaffective disorder (SS) and control smokers (CS) on indices of cigarette demand and delayed reward discounting, a behavioral economic index of impulsivity.
Materials and methods
The SS (n = 25) and CS (n = 24) groups participated in two sessions approximately one week apart. During the first session, delay discounting was assessed using the Monetary Choice Questionnaire. During the second session, participants smoked their usual brand ad libitum through a smoking topography assessment device, after which cigarette demand was assessed using a cigarette purchase task. Primary comparisons were of the hyperbolic discounting function, k, and indices of cigarette demand.
Results
Compared to the CS group, the SS group exhibited significantly higher intensity of demand, and significantly greater consumption and expenditure across the inelastic portion of the demand curve, but no differences were evident on the other demand indices. No differences were evident for delay discounting. The SS group also exhibited heavier smoking topography and two indices of smoking topography were significantly correlated with demand.
Conclusions
These results provide further evidence of higher incentive value of cigarettes among SS individuals, but not greater impulsivity, as measured by discounting. Considerations include potentially important methodological factors and the role of satiation/withdrawal.
Keywords: Nicotine, Tobacco, Cigarette, Schizophrenia, Behavioral Economics, Demand, Discounting
The prevalence of cigarette smoking is disproportionately high among people with schizophrenia, due to both unusually high rates of smoking initiation and low rates of smoking cessation (de Leon and Diaz 2005; Hughes et al. 1986; Lasser et al. 2000). In addition, smokers with schizophrenia tend to smoke more cigarettes per day, smoke more intensely and have higher serum nicotine and cotinine levels than other smokers (de Leon and Diaz 2005; Olincy et al. 1997; Tidey et al. 2005; Williams et al. 2005). The reasons for the markedly high smoking prevalence and degree of nicotine dependence among people with schizophrenia are not well understood but likely involve both environmental and biological factors. For example, people with schizophrenia tend to be inactive, unemployed and to live with other smokers (Granholm et al. 2008; Roick et al. 2007), which are significant environmental risk factors for smoking (Cummings et al. 2009; Shiffman et al. 2004). Nicotine also appears to alleviate some schizophrenia symptoms, cognitive functioning deficits and side effects of antipsychotic medications (for reviews, see Kumari and Postma 2005; Mobascher and Winterer 2008), suggesting that these beneficial effects may reinforce smoking behavior. Furthermore, abnormalities in dopamine neurotransmission associated with schizophrenia may sensitize these patients to the positive reinforcing effects of nicotine and other drugs (Chambers et al. 2001). Finally, smoking persistence in schizophrenia may be related to poor executive or other cognitive functioning in this population (O’Grada and Dinan 2007), which may undermine the extent to which smokers with schizophrenia can inhibit their impulses to smoke.
The field of behavioral economics has been extensively applied to understanding addictive behavior (Bickel et al. 2010; Vuchinich and Heather 2003) and has the potential to add insights into the reasons underlying smoking persistence in people with schizophrenia. As it is applied to addiction, behavioral economics is a hybrid of basic operant theory and microeconomics (Bickel et al. 2010; Vuchinich and Heather 2003). Of particular relevance are two experimental assays of motivation that may contribute to understanding smoking in individuals with schizophrenia: behavioral economic demand curve analysis and delayed reward discounting.
In addiction research, demand curve analysis refers to the examination of drug consumption under escalating conditions of financial or response cost and indicates the amount of money or effort that a person is willing to spend to obtain the drug. Demand curves, which can be generated via progressive ratio operant schedules (e.g., Johnson and Bickel 2003) or via self-report purchase tasks using monetary costs (e.g., Jacobs and Bickel 1999; MacKillop et al. 2008), yield several topographical features that reflect different dimensions of the relative value of cigarettes. These include intensity of demand (i.e., consumption at minimal price), Omax (i.e., maximum expenditure on cigarettes), elasticity (i.e., price sensitivity), Pmax (i.e., the price at which demand becomes proportionately sensitive to escalating prices [i.e., elastic], which corresponds with the price at which Omax is reached), and breakpoint (i.e., price that suppresses consumption to zero). Demand curve analysis has been used extensively in both basic and clinical addiction research to characterize drug motivation (e.g., Christensen et al. 2008; Greenwald and Hursh 2006; MacKillop et al. 2010; Winger et al. 2007). Only one study has conducted demand curve analyses in smokers with schizophrenia (Tidey et al. 1999). That study investigated choices between cigarette puffs and a monetary reinforcer across a range of response requirements and found that the response of smokers with schizophrenia were similar to those of non-psychiatric smokers who had been studied previously under identical conditions (Bickel et al. 1995). However, the Tidey et al. (1999) study did not include a concurrent control group. On the other hand, a study that used a related methodology to compare hypothetical dichotomous choices between smoking and a variety of alternative reinforcers in smokers with schizophrenia, smokers with major depression and smokers without psychiatric illness found that the two psychiatric groups chose smoking over the other reinforcers about twice as frequently as the non-psychiatric smokers (Spring et al. 2003). Thus, it is unclear whether smokers with schizophrenia over-value smoking compared to smokers without psychiatric illness.
Delayed reward discounting refers to the analysis of the rate at which the value of a reward is discounted as it is delayed in time. It is considered a behavioral economic index of impulsivity and has been studied extensively in relation to drug addiction, including nicotine dependence. Individuals with excessive drug use or a substance use disorder have consistently been found to discount delayed monetary or drug rewards at a higher rate than controls, characteristic of more impulsive discounting (Bickel and Marsch 2001; Perry and Carroll 2008). In smoking research, smokers discount delayed rewards more steeply than non-smokers (Baker et al. 2003; Bickel et al. 1999). A recent study found that individuals with schizophrenia in general (i.e., not specifically smokers) discounted delayed monetary rewards more steeply than non-psychiatric controls (Heery et al. 2007). However, discounting has not been previously compared in smokers with and without schizophrenia.
In this study we compared cigarette demand and delayed reward discounting in a group of smokers with schizophrenia or schizoaffective disorder (SS) and control smokers (CS). Cigarette demand was assessed using a Cigarette Purchase Task, which assessed estimated cigarette consumption from zero cost to very high prices, and delayed reward discounting was assessed as preferences for smaller immediate amounts of money compared to larger delayed amounts for two magnitudes of rewards. Based on the findings of Spring et al. (2003), we predicted that the SS group would exhibit greater cigarette demand than the CS group, but specific predictions were not made with regard to which demand curve indices would be most sensitive. Based on higher nicotine dependence associated with schizophrenia and on the findings of Heerey et al. (2007), we predicted that the SS group would exhibit more impulsive delayed reward discounting than the CS group, but no prediction was made with regard to specific reward magnitudes. In addition, because individuals with schizophrenia exhibit a heavier smoking topography (e.g., Tidey et al., 2005; 2008) and no previous studies have examined topography in relation to either discounting or demand, we examined smoking topography between the two groups and in relation to the behavioral economic variables for exploratory purposes.
Method
Participants
Participants were required to be 18 or older, to have smoked 20–50 cigarettes per day for at least the past year and to have Fagerström Test for Nicotine Dependence (FTND; Heatherton et al. 1991) scores of at least 6. The FTND has good internal consistency and acceptable test-retest reliability in SS (Weinberger et al. 2007; Yang et al. 2003). The Structured Clinical Interview for DSM-IV (SCID; First et al. 1995) was used to confirm diagnoses of schizophrenia or schizoaffective disorder in SS and to rule out current Axis I disorders in CS. Participants were excluded for severe conceptual disorganization, disorientation or uncooperativeness, lack of competence to sign the informed consent, positive urine drug or pregnancy tests, positive breath alcohol at any visit, or use of medications that might affect smoking behavior or urges. Other medications were permitted as long as doses had been stable for at least 2 weeks.
Procedure
Participants were recruited from the community for a larger multi-session study of novel strategies for treating nicotine dependence in individuals with schizophrenia. The data for the current study were collected during the first two sessions, during which participants were not taking any medications and were not abstinent from smoking. During the first session, participants underwent informed consent, an individual differences assessment, including the measures of demographics, delayed reward discounting, and intellectual functioning (described in Assessment below), and information and training for the subsequent sessions. During the second session, participants were permitted to smoke their preferred cigarettes ad libitum for five hours through a smoking topography device (CReSS Lab; Borgwaldt KC, Richmond, VA) that recorded the number of cigarettes smoked, puffs/cigarette, inter-puff interval, average puff volume, average puff duration, and other smoking topography measures. Of note, the cigarettes smoked by participants were provided by the study at no cost. Participants were then assessed for cigarette demand, putatively under satiated conditions. Participants were not given any instructions about smoking before the sessions and were permitted to smoke until entering the research building, but were not assessed for time since last cigarette. All procedures were approved by the institutional review board involved.
Assessment
Information was collected on demographic variables, income and smoking histories. Psychiatric symptoms (SS only) were evaluated using the Positive and Negative Syndrome Scale (PANSS; Kay et al. 1987). The Shipley Institute of Living Scale (Shipley 1940) was administered to provide an estimate of Wechsler Adult Intelligence Scale (WAIS) intelligence quotient (IQ). Cigarette demand was assessed using a state Cigarette Purchase Task (Hitsman et al. 2008), which assessed estimated cigarette consumption at 19 prices from $0 to $1120. This measure is based on a progressive ratio operant schedule (Hodos 1961; Johnson and Bickel 2003), hence the approximately doubling response requirement. The specific intervals were based on those used in a CPT by Jacobs and Bickel (1999). The CPT used the following instructional set: “Imagine that you could smoke your favorite cigarettes RIGHT NOW. The following questions ask how many cigarettes you would smoke if they cost various amounts of money. Assume that you would smoke every cigarette you request; that is, you cannot stockpile cigarettes for a later date or bring cigarettes home with you.” Delayed reward discounting was assessed using the previously validated Monetary Choice Questionnaire (MCQ; Kirby et al. 1999), which is a trait-level measure. Only the large ($75–$85) and small ($25–$35) magnitude MCQ items were used to minimize burden but retain discounting at multiple magnitudes.
Data Analysis
Group comparisons on demographic and smoking history measures were conducted using independent-samples t-tests for continuous variables and chi-square tests for categorical variables. All demand curves were individually examined and all raw data and computed values were examined for outliers and distribution normality. Indices of demand were generated using an “observed values” approach (MacKillop et al. 2008; Murphy and MacKillop 2006), which generates the indices from raw values. Intensity of demand is defined as consumption at zero price; Omax is defined as the maximum amount of money allocated to cigarettes; breakpoint is defined as the first price at which a subject reports zero consumption; Pmax is defined as the price at Omax. In addition, quantitative demand curve modeling was conducted using the recently developed exponential approach (Hursh and Silberberg 2008). Specifically, nonlinear regression was used to fit and generate parameters for the following equation:
where Q = consumption at a given price, Q0 = maximum consumption (consumption at zero or minimal price), k = a constant across individuals that denotes the range of consumption values in log powers of ten (k was constrained as being between 0–4; Hursh, personal communication), C = the cost of the commodity (price), and α = the derived demand parameter reflecting the rate of decline of consumption in standardizd price (Hursh and Silberberg 2008). The derived parameter α is referred to as the “essential value” of the commodity (Hursh and Silberberg, 2008). It should be noted that the demand indices are considered distinct but related facets of motivation (Bickel et al., 2000) and are, in some cases, interdependent on one another. For example, intensity and breakpoint are entirely independent, but, using an observed values approach, Pmax, a price, is defined by Omax, an amount of expenditure. Thus, although Omax and Pmax are by no means collinear, they are related variables.
Delayed reward discounting was calculated as an inferred k value from the MCQ using previously established methods (Kirby et al. 1999); note that the k temporal discounting function from the MCQ is distinct from the k described above in exponential demand curve modeling. The MCQ generates three indices of discounting for small, medium, and large rewards, which are highly correlated (MacKillop et al. 2010), but only the small and large reward magnitude items were used in this study. In addition, consistency values were generated for each index, measuring how consistent the inferred k value was with the overall array of choices (i.e., the percentage of the participants’ choices that did not contradict the discounting function).
Initial analyses compared the two groups for potentially meaningful demographic and smoking differences and examined correlations with the demand indices and k values. The primary data analysis examined the preceding demand curve indices and k values. Exploratory individual price and expenditure comparisons were the conducted for clarification of which prices were sensitive to group differences. Comparisons between groups used t-tests and analysis of variance/covariance. Finally, based on previous evidence of significant correlations between demand indices and discounting (MacKillop et al. 2010), zero-order correlations were used to clarify overlap among the variables and were measured as Pearson’s r. Significance was defined as α ≤.05 for descriptive analyses, but lowered to α ≤.01 for the primary between-groups comparisons to adjust for multiple comparisons. Exponential demand curve modeling was conducted using GraphPad Prism 5 and all other analyses were conducted using SPSS 16.0.
Results
Preliminary Analyses
For two participants, no topographical data were collected and, for one, only number of cigarettes was collected. For cigarette demand, six of the 49 participants were not administered the CPT (four SS, two CS; χ2 = .67, p = .41). No missing data were imputed. In addition, three individuals provided invalid data (two SS, one CS; χ2 = .41, p = .52). These comprised two participants who provided erratic responding and one who provided too few responses for demand curve analysis. Individual demand curves were examined and revealed that five participants provided extreme values (two SS, three CS; χ2 = .18, p = .67). This was confirmed by formal outlier analysis using a standard score of 3.29, indicating that the vast majority of outlying values were provided by these individuals. Three isolated high-magnitude data points were also identified and recoded as one value above the next highest non-outlying value (Tabachnick and Fidell 2001). Thus, the final cell sizes for demand curve analysis were SS n = 17, and CS n = 18. The exponential demand equation generated a k constant of approximately 4 and provided a generally good fit to the data (median R2 = .86, IQR = .79 – .91, Range = .51–.99).
For delay discounting, two SS individuals were not administered the MCQ (χ2 = 2.00, p = .16), no missing data were imputed and no outliers were detected. Thus, the cell sizes for discounting analyses were SS, n = 23, and CS, n = 24. Consistency analysis revealed generally high levels of consistency for both small and large rewards, M = 94% (range = 78%–100%).
Skewness was examined using histograms and revealed positive skewness for all demand indices, except intensity, and discounting k values, which is common (Petry 2001). Logarithmic transformations were implemented and substantially improved the distributions.
Group Differences
Participants’ demographic, smoking, and psychiatric characteristics are presented in Table 1. The groups did not differ on gender, racial or ethnic distributions, age, years of education, income, estimated IQ, or FTND, however, the SS group smoked significantly more cigarettes per day than the CS group. Consistent with previous reports (Tidey et al., 2005; 2008), during the ad libitum period, the SS group smoked more cigarettes, took more puffs per cigarette, and exhibited shorter inter-puff intervals, although no differences were evident for puff volume or duration.
Table 1.
Participant characteristics (% or mean and standard deviation). Comparisons reflect independent samples t-tests.
| SS | Control | p | |
|---|---|---|---|
| Sex | 64% Male | 58% Male | |
| Race | 80% White, 12% African American, 4% Native, 4% Mixed | 58% White, 21 African American; 4% Native American; 4% Asian; 13% Mixed | |
| Hispanic | 4% Hispanic | 8% Hispanic | |
| Age | 45.48 (8.70) | 43.58 (12.35) | .54 |
| Education | 12.04 (2.35) | 11.8 (1.96) | .69 |
| Income | $14,389 (16,992) | $18,653 ($14,228) | .35 |
| Cigs/Day | 32.08 (10.90) | 24.17 (6.57) | <.01 |
| FTND | 7.60 (1.44) | 6.92 (1.38) | .10 |
| ad lib Cigarettes | 4.22 (1.41) | 2.96 (1.52) | <.01 |
| ad lib Puffs/Cig | 15.24 (4.69) | 11.29 (3.27) | <.01 |
| Puff Volume | 43.32 (16.47) | 43.08 (13.24) | .94 |
| Puff Duration | 1.30 (.49) | 1.37 (.43) | .87 |
| Inter Puff Interval | 23.13 (12.6) | 34.82 (13.59) | <.01 |
| Estimated IQ | 85.68 (12.08) | 84.42 (12.21) | .72 |
| PANSS-Positive | 12.52 (4.98) | -- | |
| PANSS-Negative | 14.84 (6.65) | -- | |
| PANSS-General | 28.16 (7.89) | -- |
Note: FTND = Fagerström Test of Nicotine Dependence; PANSS = Positive and Negative Syndrome Scale (not assessed in control subjects).
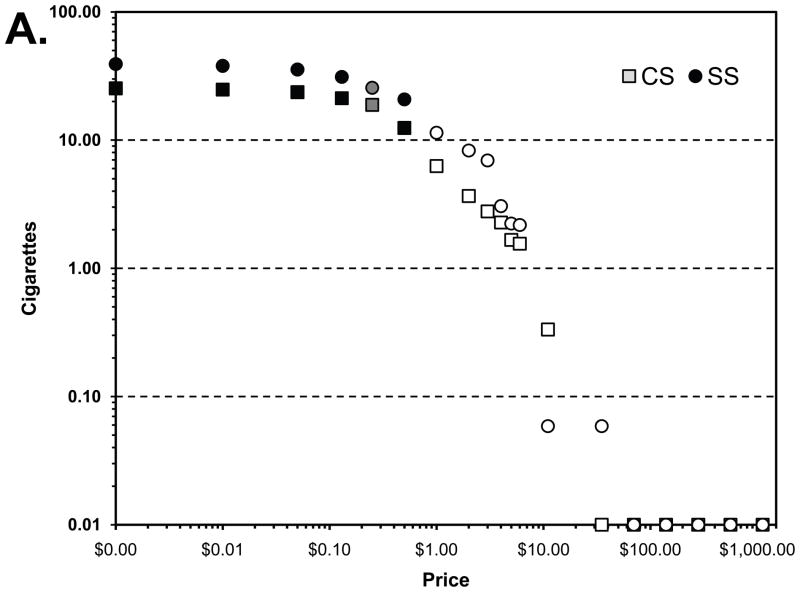
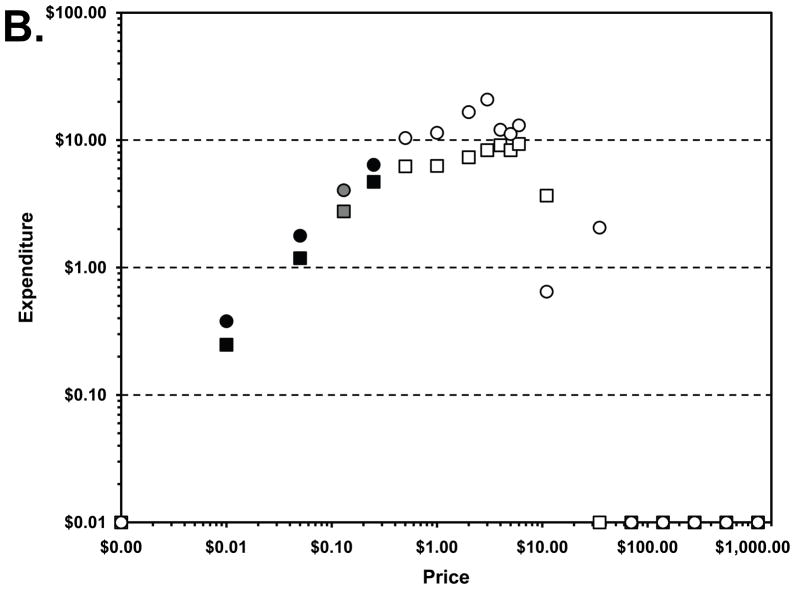
With regard to indices of cigarette demand, comparisons of the demand indices while covarying cigarettes/day revealed a significant difference for intensity of demand, but no other indices (Table 2). Raw demand and expenditure values are provided in Figure 1. In terms of demand at individual prices, significant differences were evident for consumption at five low prices, with corresponding effects present for expenditure (Figure 1). Adding cigarettes/per day as a covariate, significant differences continued to be evident for consumption and expenditure through the third price (not shown), although cigarettes per day was a significant in each case. In each case, SS smokers exhibited significantly greater demand for cigarettes and expenditure.
Table 2.
Estimated marginal means, standard errors, F ratios, and significance values for analyses of covariance of indices of cigarette demand and delay discounting between the schizophrenia-schizoaffective disorder smokers (SS) and control smokers (CS). Cigarettes/day was covaried for all analyses. Small and large discounting designations refer to delayed reward magnitudes (an average of $25 vs. $85). Note that untransformed means are provided for interpretational clarity. Degrees of freedom are 1, 34 for demand variables and 1, 36, for the discounting variables.
| Index | CS | SEM | SS | SEM | F | p |
|---|---|---|---|---|---|---|
| Intensity | 27.21 | 2.50 | 37.19 | 2.58 | 7.712 | .01 |
| Omax | 9.64 | 4.00 | 13.61 | 5.89 | .63 | .43 |
| Pmax | 1.22 | .66 | 1.19 | 1.32 | .001 | .97 |
| Breakpoint | 3.04 | .1.50 | 3.61 | 1.86 | .12 | .73 |
| α | .01 | .13 | .01 | .13 | .74 | .40 |
| Small k | .07 | .06 | .03 | .02 | 2.10 | .15 |
| Large k | .04 | .03 | .02 | .01 | 1.41 | .24 |
Figure 1.
Cigarette demand and expenditure curves for smokers with schizophrenia/ schizoaffective disorder (SS) and controls (CS). Panels A and B present the raw values by price in conventional log-log coordinates with between-groups analysis of variance comparisons. Black symbols reflect significant differences, p ≤ .05; gray symbols reflect trend-level effects, p≤.10; white symbols reflect nonsignificant group differences.
With regard to delayed reward discounting, a magnitude effect was present (F [1, 45] = 7.72, p <.01), with participants exhibiting greater impulsivity for smaller magnitude reward compared to larger magnitude rewards. For small magnitude rewards, no significant group difference was evident. Likewise, for large magnitude rewards, no significant difference was evident. For the preceding, untransformed means are presented in Table 2 for interpretational clarity. To clarify any possible role of the covariate, the analyses were re-run without covarying cigarettes/day and no group differences were evident (not shown).
Exploratory Continuous Analyses
To characterize overlap among variables, a correlation matrix including smoking-related variables, behavioral economic variables, and topographical variables that significantly differed between groups is provided in Table 3. Nicotine dependence (FTND) score was significantly associated with intensity and Omax, cigarettes/day was also significantly associated with intensity, and significant, high magnitude associations were evident among Omax, Pmax, and breakpoint, as well as between the large and small k values. Interestingly, ad libitum smoking was significantly associated with both intensity and Omax, and puffs/cigarette was significantly associated with and all demand indices other than intensity. Of note, income and IQ were not significantly correlated with any of the smoking or behavioral economic measures.
Table 3.
Zero order correlations among variables. Base 10 transforms were used for the temporal discounting functions (k) and demand indices, with the exception of intensity.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. FTND | 1 | ||||||||||
| 2. C/D | .55** | 1 | |||||||||
| 3. Intensity | .34* | .54** | 1 | ||||||||
| 4. Omax | .35* | .14 | .24 | 1 | |||||||
| 5. Pmax | .13 | −.09 | .14 | .74** | 1 | ||||||
| 6. BP | .09 | −.11 | −.23 | .70** | .89** | 1 | |||||
| 7. α | −.28 | −.15 | −.17 | −.93** | −.83** | −.87** | 1 | ||||
| 8. k (Small) | .05 | −.02 | .13 | .36* | .35* | .29 | −.38* | 1 | |||
| 9. k (Large) | −.07 | −.05 | .19 | .17 | .18 | .17 | −.25 | .75** | 1 | ||
| 10. ad lib Cigarettes | .23 | .56** | .59** | .34* | −.09 | −.06 | −.23 | .11 | .08 | 1 | |
| 11. ad lib Puffs/Cig | .04 | .17 | .14 | .40** | .36* | .37* | −.41* | −.15 | .01 | .21 | 1 |
| 12. IPI | .01 | −.17 | −.17 | −.25 | −.10 | −.09 | .17 | .12 | .03 | .03 | −.70** |
C/D = cigarettes/day; IPI = Inter-puff Interval;
p <.05,
p <.01.
Discussion
To better understand the strong association between smoking and schizophrenia, the current study examined two behavioral economic measures of motivation, cigarette demand and delayed reward discounting, in nicotine-dependent individuals with and without schizophrenia or schizoaffective disorder. Consistent with our prediction, significant differences in demand were observed between the two groups. Specifically, the SS group exhibited significantly higher intensity of demand (unconstrained consumption) and exploratory analyses revealed significantly greater consumption and expenditure across the inelastic portion of the demand curve. The two groups differed in terms of smoking rate (number of cigarettes smoked per day), but these differences largely remained present in follow-up analyses after covarying that variable. Notably higher Omax and expenditure in general was evident in the SS group, but given the high within-group variability, the difference between the two groups was not significant. No differences were evident in terms of Pmax, breakpoint, or essential value. A recent factor analysis of indices of demand suggested two underlying factors, amplitude (value for greater amounts of a commodity) and persistence (insensitivity to escalating price) (MacKillop et al. 2009). Applying this in the context of the current study, the pattern of findings suggested greater amplitude, but not greater persistence of demand in the SS group. Taken together, these findings converge with Tidey et al. (1999) insofar as they reveal that smokers with schizophrenia are sensitive to increases in the costs of cigarettes and extend those findings to reveal significantly greater volumetric demand for cigarettes at low prices compared to a control sample. In addition, although the methods are not directly comparable, the current results are generally consistent with findings of Spring et al. (2003) who reported greater reward value for cigarettes in smokers with schizophrenia or major depression compared non-psychiatric smokers. These findings are also generally consistent with evidence that smokers with schizophrenia allocate large portions of their income to smoking (Steinberg et al. 2004).
With regard to delayed reward discounting, there were no significant differences between the two groups and, directionally, the control group actually exhibited more impulsive discounting than the SS group. Given its conceptual relevance and association with a number of dimensions of nicotine dependence (Baker et al. 2003; Bickel et al. 1999; MacKillop and Kahler 2009; Yoon et al. 2007), excessive discounting is a plausible explanatory variable for the high nicotine dependence associated with schizophrenia, but that hypothesis was not supported in the current study. In the context of the larger field, this suggests that although precipitous discounting may be associated with nicotine dependence in general (Bickel et al., 1999; Baker et al., 2003), it does not contribute to the greater rates of smoking and greater levels of nicotine dependence among SS individuals. That is, impulsive discounting may be a more general nicotine dependence risk factor and alternative motivational mechanisms are responsible for the unusually high levels of smoking within SS individuals.
There are reasons, however, to be cautious about ruling out a role of delay discounting on the basis of this study alone. In the first place, one possibility is that because both the SS and control samples were nicotine dependent and smoked more than 20 cigarettes/day, there may have been a ceiling effect. Second, although the measure used has been sensitive to group differences in case-control studies comparing drug abusers to controls (Kirby et al., 1999), it may not be optimal for detecting differences between subsamples of smokers or other drug users. There are a number of alternative discounting assessments that may be more sensitive to group differences, such as adaptive adjusting choice tasks, in vivo tasks, and tasks using cigarettes or health as commodities (e.g., Baker et al. 2003; Bickel et al. 1999; Odum et al., 2002; Reynolds 2006). A third possiblity is that either the CS or the SS subjects may not have been representative of their respective populations. Given that the participants in the current study were generally of below average intellectual functioning and that individuals with schizophrenia are known to have deficits in cognitive functioning (O’Grada and Dinan 2007), the abstraction involved in the measure may have been challenging and a delay discounting task for actual outcomes would avoid that problem. Given these possibilities and the fact this is the first study to test this hypothesis (to our knowledge), although the current findings give no indication of significantly greater discounting in SS individuals, it would be imprudent to consider this definitive at this point.
A strength of the current study was the inclusion of an ad libitum smoking topography behavioral assessment. In this case, the results converged with previous reports of heavier smoking topography in individuals with schizophrenia (Tidey et al., 2005; 2008), with the SS group smoking more cigarettes, puffing more, and leaving less time between puffs compared to the control group. Moreover, ad libitum cigarette consumption was significantly positively correlated with both intensity of demand and Omax. The former association is particularly important because it provides further validation for intensity as measured by a purchase task as an index of consumption under conditions of zero cost, which were the self-administration conditions here. Thus, the two were essentially measures of the same thing – unconstrained consumption – albeit with the laboratory assessment taking place over a shorter period of time under controlled conditions and with a topography device. Interestingly, puffs/cigarette was also significantly associated with all the demand indices, but with the exception of intensity. These relationships all reflected a correspondence between puffing behavior and greater relative value of cigarettes. However, the correlational nature of the findings means it is unclear whether participants who puffed more did so because cigarettes have a greater incentive value, or whether these participants value cigarettes more because they experience stronger reinforcing effects from the sensorimotor activity of puffing.
The implications of these findings are a function of the study’s strengths and limitations. Strengths include a well characterized sample of SS and control smokers, and groups that were highly similar to each other. From an experimental psychopathology standpoint, this is critical for stringently determining whether meaningful differences are present between the groups. Future studies will be important for replicating and refining these findings to better understand the nature of these differences in terms of smoking patterns or motives. From a clinical standpoint, these findings suggest that smokers with schizophrenia will need more aggressive treatments to compete with their greater general motivation for nicotine. This might plausibly come in the form of, among a number of possibilities, multiple concurrent forms of nicotine replacement therapy, relatively rich schedules of contingency management, or both. In any case, this study further suggests that applying the general treatment recommendations in a ‘one-size-fits-all’ way will be insufficient for these individuals.
However, limitations of the study include the relatively small sample size, which made only large effect size differences detectable between the two groups and a number of additional measurement issues. With regard to statistical power, as an initial study in this area, the cell sample sizes were relatively small and the observed demand findings suggest that performance was relatively variable. Thus, these initial findings suggest that in a study with a larger sample size, several additional demand indices would be likely to be statistically significant. This in turn would have the potential to provide greater clarity and precision on the nature of the differences between the two groups. Related to this issue, the open response format of the CPT yielded invalid values from a number of participants from both groups and in general participants were relatively heterogeneous in their performance on the task. This problem has not been evident in previous studies using a CPT in individuals with comorbid nicotine dependence and opiate dependence (Jacobs and Bickel 1999) and young adult smokers (MacKillop et al. 2008). However, as noted above, the current study’s participants were relatively low in terms of intellectual functioning and the level of abstraction required may have been a limitation. It is possible a paradigm using actual outcomes or more concrete response options would eliminate these issues and reduce the probability of extreme or erratic data. A more general issue pertains to the price intervals used, which may have been suboptimal. The price intervals used were based on an initial study of the purchase task methodology (Jacobs and Bickel 1999) and used doubling response requirements, akin to a progressive ratio schedule. However, some of the prices were limited by market implausibility and the relatively large increases between intervals. A CPT using smaller price intervals and fewer prices of very high cost might prove more sensitive to differences between groups. These factors suggest caution in interpreting these results and the need for further investigation in this area to clarify these relationships further.
Other factors to consider for future studies are the roles of physiological and affective states. The current study examined variables under conditions of satiation, which is a reasonable starting point, but it is possible that individuals with schizophrenia may be differentially sensitive to withdrawal from nicotine. First, acute withdrawal has been shown to affect discounting (Field et al. 2006; Mitchell 2004) and smokers with schizophrenia have been found to exhibit a larger rebound in smoking following a period of acute abstinence (Tidey et al. 2008), in spite of no differences in subjective withdrawal and craving. Moreover, differential effects of protracted abstinence on smokers with schizophrenia have not been studied to date. Equally, it is possible that individuals with schizophrenia are more sensitive to or less able to cope with stressful situations, which is one of most common relapse precipitants (Kassel et al., 2003). In both the cases of withdrawal and stress, these possibilities are necessarily speculative but nonetheless represent plausible domains that may explain the differences between smokers with schizophrenia and general smokers.
Taken together, these findings are potentially important as initial evidence that demand curve analysis may be a useful experimental paradigm for unraveling the differences in smoking prevalence between smokers with and without schizophrenia-spectrum disorders. In addition, although no differences in delay discounting were detected, these findings represent only an initial test of this hypothesis and point to future strategies in this domain. Subsequent studies employing some of the preceding suggestions will be important for affirming the observed differences and clarifying the motivational factors that lead to overvaluation of cigarettes in individuals with schizophrenia.
Acknowledgments
Funding support from NIH grants grants K23AA016936 (JM), 5R01DA014002 (JT), 1R21DA026829 (JT). The authors are grateful for excellent technical assistance from Laura Dionne.
Footnotes
The authors have no conflicts of interest with these findings.
References
- Baker F, Johnson MW, Bickel WK. Delay discounting in current and never-before cigarette smokers: similarities and differences across commodity, sign, and magnitude. J Abnorm Psychol. 2003;112:382–92. doi: 10.1037/0021-843x.112.3.382. [DOI] [PubMed] [Google Scholar]
- Bickel WK, DeGrandpre RJ, Higgins ST. The behavioral economics of concurrent drug reinforcers: a review and reanalysis of drug self-administration research. Psychopharmacology (Berl) 1995;118:250–9. doi: 10.1007/BF02245952. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction. 2001;96:73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA, Carroll ME. Deconstructing relative reinforcing efficacy and situating the measures of pharmacological reinforcement with behavioral economics: a theoretical proposal. Psychopharmacology (2000) 2000;153:44–56. doi: 10.1007/s002130000589. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Mueller ET, MacKillop J, Yi R. Behavioral economic and neuroeconomic perspectives on addiction. In: Sher K, editor. Oxford Handbook of Substance Use Disorders. Oxford University Press; Oxford, UK: 2010. [Google Scholar]
- Bickel WK, Odum AL, Madden GJ. Impulsivity and cigarette smoking: delay discounting in current, never, and ex-smokers. Psychopharmacology (Berl) 1999;146:447–54. doi: 10.1007/pl00005490. [DOI] [PubMed] [Google Scholar]
- Chambers RA, Krystal JH, Self DW. A neurobiological basis for substance abuse comorbidity in schizophrenia. Biol Psychiatry. 2001;50:71–83. doi: 10.1016/s0006-3223(01)01134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen CJ, Silberberg A, Hursh SR, Huntsberry ME, Riley AL. Essential value of cocaine and food in rats: tests of the exponential model of demand. Psychopharmacology (Berl) 2008;198:221–9. doi: 10.1007/s00213-008-1120-0. [DOI] [PubMed] [Google Scholar]
- Cummings KM, Fong GT, Borland R. Environmental influences on tobacco use: evidence from societal and community influences on tobacco use and dependence. Annu Rev Clin Psychol. 2009;5:433–58. doi: 10.1146/annurev.clinpsy.032408.153607. [DOI] [PubMed] [Google Scholar]
- de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res. 2005;76:135–57. doi: 10.1016/j.schres.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Field M, Santarcangelo M, Sumnall H, Goudie A, Cole J. Delay discounting and the behavioural economics of cigarette purchases in smokers: the effects of nicotine deprivation. Psychopharmacology (Berl) 2006;186:255–63. doi: 10.1007/s00213-006-0385-4. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer R, Williams J. DSM-IV Axis I disorders (SCID-I, Version 2.0.) New York State Psychiatric Institute, Biometrics Research Department; New York: 1995. User’s guide for the Structured Clinical Interview for. [Google Scholar]
- Granholm E, Loh C, Swendsen J. Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophr Bull. 2008;34:507–14. doi: 10.1093/schbul/sbm113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald MK, Hursh SR. Behavioral economic analysis of opioid consumption in heroin-dependent individuals: effects of unit price and pre-session drug supply. Drug and Alcohol Dependence. 2006;85:35–48. doi: 10.1016/j.drugalcdep.2006.03.007. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heery EA, Robinson BM, McMahon RP, Gold JM. Delay discounting in schizophrenia. Cognitive Neuropsychiatry. 2007;12:213–221. doi: 10.1080/13546800601005900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitsman B, MacKillop J, Lingford-Hughes A, Williams TM, Ahmad F, Adams S, Nutt DJ, Munafo MR. Effects of acute tyrosine/phenylalanine depletion on the selective processing of smoking-related cues and the relative value of cigarettes in smokers. Psychopharmacology (Berl) 2008;196:611–21. doi: 10.1007/s00213-007-0995-5. [DOI] [PubMed] [Google Scholar]
- Hodos W. Progressive ratio as a measure of reward strength. Science. 1961;134:943–4. doi: 10.1126/science.134.3483.943. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA. Prevalence of smoking among psychiatric outpatients. Am J Psychiatry. 1986;143:993–7. doi: 10.1176/ajp.143.8.993. [DOI] [PubMed] [Google Scholar]
- Hursh SR, Silberberg A. Economic demand and essential value. Psychol Rev. 2008;115:186–98. doi: 10.1037/0033-295X.115.1.186. [DOI] [PubMed] [Google Scholar]
- Jacobs EA, Bickel WK. Modeling drug consumption in the clinic using simulation procedures: demand for heroin and cigarettes in opioid-dependent outpatients. Exp Clin Psychopharmacol. 1999;7:412–26. doi: 10.1037//1064-1297.7.4.412. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. The behavioral economics of cigarette smoking: The concurrent presence of a substitute and an independent reinforcer. Behav Pharmacol. 2003;14:137–44. doi: 10.1097/00008877-200303000-00005. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Kumari V, Postma P. Nicotine use in schizophrenia: the self medication hypotheses. Neurosci Biobehav Rev. 2005;29:1021–34. doi: 10.1016/j.neubiorev.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA. 2000;284:2606–10. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug Alcohol Depend. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Miranda JR, Monti PM, Ray LA, Tidey JW, Rohsenow DJ, Gwaltney GJ, McGeary JE, Swift RM. Alcohol demand, delayed reward discounting, and craving in relation to drinking and alcohol use disorders. J Abnorm Psychol. 2010;119:115–125. doi: 10.1037/a0017513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Ray LA, Eisenberg DT, Lisman SA, Lum JK, Wilson DS. Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Exp Clin Psychopharmacol. 2008;16:57–65. doi: 10.1037/1064-1297.16.1.57. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Tidey JW, Kahler CW, Ray LA, Bickel WK. Latent structure of facets of alcohol reinforcement from a behavioral economic demand curve. Psychopharmacology (Berl) 2009;203:33–40. doi: 10.1007/s00213-008-1367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SH. Effects of short-term nicotine deprivation on decision-making: delay, uncertainty and effort discounting. Nicotine and Tobacco Research. 2004;6:819–28. doi: 10.1080/14622200412331296002. [DOI] [PubMed] [Google Scholar]
- Mobascher A, Winterer G. The molecular and cellular neurobiology of nicotine abuse in schizophrenia. Pharmacopsychiatry. 2008;41(Suppl 1):S51–9. doi: 10.1055/s-2008-1081463. [DOI] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J. Relative reinforcing efficacy of alcohol among college student drinkers. Exp Clin Psychopharmacol. 2006;14:219–27. doi: 10.1037/1064-1297.14.2.219. [DOI] [PubMed] [Google Scholar]
- O’Grada C, Dinan T. Executive function in schizophrenia: what impact do antipsychotics have? Hum Psychopharmacol. 2007;22:397–406. doi: 10.1002/hup.861. [DOI] [PubMed] [Google Scholar]
- Odum AL, Madden GJ, Bickel WK. Discounting of delayed health gains and losses by current, never- and ex-smokers of cigarettes. Nicotine Tob Res. 2002;4:295–303. doi: 10.1080/14622200210141257. [DOI] [PubMed] [Google Scholar]
- Olincy A, Young DA, Freedman R. Increased levels of the nicotine metabolite cotinine in schizophrenic smokers compared to other smokers. Biol Psychiatry. 1997;42:1–5. doi: 10.1016/S0006-3223(96)00302-2. [DOI] [PubMed] [Google Scholar]
- Perry JL, Carroll ME. The role of impulsive behavior in drug abuse. Psychopharmacology (Berl) 2008;200:1–26. doi: 10.1007/s00213-008-1173-0. [DOI] [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology (Berl) 2001;154:243–50. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Reynolds B. The Experiential Discounting Task is sensitive to cigarette-smoking status and correlates with a measure of delay discounting. Behavioural Pharmacology. 2006;17:133–42. doi: 10.1097/01.fbp.0000190684.77360.c0. [DOI] [PubMed] [Google Scholar]
- Roick C, Fritz-Wieacker A, Matschinger H, Heider D, Schindler J, Riedel-Heller S, Angermeyer MC. Health habits of patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2007;42:268–76. doi: 10.1007/s00127-007-0164-5. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gwaltney CJ, Dang Q. Immediate antecedents of cigarette smoking: an analysis of unrestricted smoking patterns. J Abnorm Psychol. 2004;113:166–71. doi: 10.1037/0021-843X.113.1.166. [DOI] [PubMed] [Google Scholar]
- Shipley WC. A self-administering scale for measuring intellectual impairment and deterioration. Journal of Psychology. 1940;9:371–377. [Google Scholar]
- Spring B, Pingitore R, McChargue DE. Reward value of cigarette smoking for comparably heavy smoking schizophrenic, depressed, and nonpatient smokers. Am J Psychiatry. 2003;160:316–22. doi: 10.1176/appi.ajp.160.2.316. [DOI] [PubMed] [Google Scholar]
- Steinberg M, Williams J, Ziedonis D. Financial implications of cigarette smoking among individuals with schizophrenia. Tob Control. 2004;13:206. [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4. Allyn & Bacon, Allyn & Bacon; 2001. [Google Scholar]
- Tidey JW, O’Neill SC, Higgins ST. Effects of abstinence on cigarette smoking among outpatients with schizophrenia. Exp Clin Psychopharmacol. 1999;7:347–53. doi: 10.1037//1064-1297.7.4.347. [DOI] [PubMed] [Google Scholar]
- Tidey JW, Rohsenow DJ, Kaplan GB, Swift RM. Cigarette smoking topography in smokers with schizophrenia and matched non-psychiatric controls. Drug Alcohol Depend. 2005;80:259–65. doi: 10.1016/j.drugalcdep.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Tidey JW, Rohsenow DJ, Kaplan GB, Swift RM, Adolfo AB. Effects of smoking abstinence, smoking cues and nicotine replacement in smokers with schizophrenia and controls. Nicotine Tob Res. 2008;10:1047–56. doi: 10.1080/14622200802097373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuchinich RE, Heather N. Choice, behavioural economics and addiction. Pergamon/Elsevier Science; Amsterdam, The Netherlands: 2003. [Google Scholar]
- Weinberger AH, Reutenauer EL, Allen TM, Termine A, Vessicchio JC, Sacco KA, Easton CJ, McKee SA, George TP. Reliability of the Fagerstrom Test for Nicotine Dependence, Minnesota Nicotine Withdrawal Scale, and Tiffany Questionnaire for Smoking Urges in smokers with and without schizophrenia. Drug Alcohol Depend. 2007;86:278–82. doi: 10.1016/j.drugalcdep.2006.06.005. [DOI] [PubMed] [Google Scholar]
- Williams JM, Ziedonis DM, Abanyie F, Steinberg ML, Foulds J, Benowitz NL. Increased nicotine and cotinine levels in smokers with schizophrenia and schizoaffective disorder is not a metabolic effect. Schizophr Res. 2005;79:323–35. doi: 10.1016/j.schres.2005.04.016. [DOI] [PubMed] [Google Scholar]
- Winger G, Galuska CM, Hursh SR. Modification of ethanol’s reinforcing effectiveness in rhesus monkeys by cocaine, flunitrazepam, or gamma-hydroxybutyrate. Psychopharmacology (Berl) 2007;193:587–98. doi: 10.1007/s00213-007-0809-9. [DOI] [PubMed] [Google Scholar]
- Yang YK, McEvoy JP, Wilson WH, Levin ED, Rose JE. Reliabilities and intercorrelations of reported and objective measures of smoking in patients with schizophrenia. Schizophr Res. 2003;60:9–12. doi: 10.1016/s0920-9964(02)00208-6. [DOI] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, Badger GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Exp Clin Psychopharmacol. 2007;15:176–86. doi: 10.1037/1064-1297.15.2.186. [DOI] [PubMed] [Google Scholar]