Abstract
Objective
To evaluate the efficacy of cognitive rehabilitation therapies (CRTs) for mild cognitive impairment (MCI). Our review revealed a need for evidence-based treatments for MCI and a lack of a theoretical rehabilitation model to guide the development and evaluation of these interventions. We have thus proposed a theoretical rehabilitation model of MCI that yields key intervention targets - cognitive compromise, functional compromise, neuropsychiatric symptoms, and modifiable risk and protective factors known to be associated with MCI and dementia. Our model additionally defines specific cognitive rehabilitation approaches that may directly or indirectly target key outcomes - restorative cognitive training, compensatory cognitive training, lifestyle interventions, and psychotherapeutic techniques.
Methods
Fourteen randomized controlled trials met inclusion criteria and were reviewed.
Results
Studies markedly varied in terms of intervention approaches and selected outcome measures and were frequently hampered by design limitations. The bulk of the evidence suggested that CRTs can change targeted behaviors in individuals with MCI and that CRTs are associated with improvements in objective cognitive performance, but the pattern of effects on specific cognitive domains was inconsistent across studies. Other important outcomes (i.e., daily functioning, quality of life, neuropsychiatric symptom severity) were infrequently assessed across studies. Few studies evaluated long-term outcomes or the impact of CRTs on conversion rates from MCI to dementia or normal cognition.
Conclusions
Overall, results from trials are promising but inconclusive. Additional well-designed and adequately powered trials are warranted and required before CRTs for MCI can be considered evidence based.
Keywords: mild cognitive impairment, cognitive rehabilitation therapy, cognitive training, systematic review, neuropsychological, dementia
Introduction
Broadly speaking, the term mild cognitive impairment (MCI) is used to describe an older population with cognitive deficits not severe enough to warrant a diagnosis of dementia (Petersen 2004). It has been viewed as an intermediate stage between normal aging and dementia (Mariani et al. 2007) and as the prodromal stage for a variety of dementing neurodegenerative disorders, including Alzheimer’s disease (AD), frontotemporal dementia, dementia with Lewy bodies, and vascular dementia (Petersen 2004). Cognitive impairment associated with MCI can affect virtually all domains including memory, language, attention, visuospatial functioning, and executive functions (Arnaiz and Almkvist 2003). Depending on the study, prevalence rates of MCI within older adult populations have been estimated at 3-42% (Ward et al. 2012). Estimated conversion rates of MCI to dementia have ranged from 2-31%, with a mean annual conversion rate of 10.2% (Bruscoli and Lovestone 2004). Studies indicate that 14-40% of those with MCI return to normal cognitive function over time (Ganguli et al. 2004; Koepsell and Monsell 2012; Larrieu et al. 2002; Manly et al. 2008; Tschanz et al. 2006), and many individuals also exhibit a persistent form of MCI without converting to dementia (Manly et al. 2008; Schonknecht 2011).
Historically, many diagnostic criteria were proposed to describe the early cognitive changes that occur in older adults (Ward et al. 2012). Due to lack of adequate diagnostic criteria, approximately thirteen years ago Petersen et al. (1999) developed an MCI diagnostic and classification system which is now widely adopted. This classification system yields four MCI subtypes and categorizes cognitive deficits as either amnestic or non-amnestic, and as either single cognitive domain or multiple cognitive domains (Petersen 2004). More recently, the National Institute on Aging and the Alzheimer’s Association put together a workgroup that recommends two sets of criteria for MCI due to AD, one set of criteria for healthcare providers without access to neuroimaging or cerebrospinal fluid analysis, and another for researchers and clinical trials that incorporate these biomarkers (Albert et al. 2011). This workgroup recommends almost identical criteria as did Petersen et al. (1999) for the establishment of a clinical diagnosis of MCI: 1) a subjective cognitive complaint whereby the patient, an informant, or a clinician report a decline over time, 2) objective evidence of cognitive impairment in one or more cognitive domains using formal or bedside testing, 3) the impact of cognitive impairments on daily functioning does not preclude independence, 4) the person does not meet criteria for dementia. Based on whether biomarkers have been tested and whether results are informative, this workgroup’s proposed system also yields research diagnostic categories that indicate the likelihood of underlying AD (i.e., MCI - Core Clinical Criteria; MCI due to AD - Intermediate Likelihood; MCI due to AD - High Likelihood; MCI - Unlikely due to AD).
Although the cognitive impairments associated with MCI do not preclude independent functioning, research suggests that individuals with MCI nevertheless experience changes in their psychological and daily functioning as well as quality of life (QOL) (Albert et al. 2011; Gold 2012;Windblad et al. 2004; Teng et al. 2012). A recent review article noted that neuropsychiatric symptoms are very common in individuals with MCI, with prevalence rates of at least one neuropsychiatric symptom ranging from 35-85% (Monastero et al. 2009). The most common neuropsychiatric issues associated with MCI include depression, anxiety, irritability, agitation, apathy, euphoria, disinhibition, delusions, hallucinations, and sleep disorders (Apostolova and Cummings 2008; Bomboi et al. 2010; Ellison et al. 2008; Monastero et al. 2009). Areas of daily functioning most frequently impacted by MCI include appointment scheduling/attendance, transportation issues, and financial management (Gold 2012). Individuals with multi-domain MCI tend to demonstrate greater functional limitations than those with single domain MCI (Gold 2012). Individuals with MCI additionally report a reduced QOL relative to older adults without cognitive impairment, and this reduced QOL is associated with increased neuropsychiatric symptoms and reduced daily functioning (but not with objective cognitive performance) in older adults with MCI (Teng et al. 2012). The hypothesis that MCI is a transitional stage between normal aging and dementia implies that individuals with MCI are at risk for significant functional impairment and an eventual inability to live independently which would further decrease their QOL (Petersen et al. 2009).
MCI likely stems from multiple etiologies. In addition to neurodegenerative conditions like AD, Dementia with Lewy Bodies, and Parkinson’s disease, other possible etiologies for MCI include cardiovascular, metabolic, endocrine, traumatic, and psychiatric origins (Etgen et al. 2011; Mariani et al. 2007; Winblad 2004). Likewise, numerous demographic, genetic, disease, and lifestyle factors have been associated with increased or decreased risk for diagnosis with MCI. Although a thorough discussion of each of these risk and protective factors is beyond the scope of this paper, a non-exhaustive list has been provided in Table 1. Notably, the risk and protective factors associated with MCI are similar to those associated with conversion to dementia (Gomar et al. 2011; Li et al. 2011; Ravaglia et al. 2008; Schmand et al. 2012; Yu et al. 2012). The modifiable risk and protective factors that are associated with lifestyle habits are of particular interest to clinicians working with individuals with MCI since they can serve as the focus of preventative interventions and rehabilitation efforts. For example, some cognitive rehabilitation therapies (CRTs) for MCI involve lifestyle interventions, which for the purposes of this review, are defined as behavioral interventions designed to decrease the frequency of negative lifestyle behaviors (i.e., smoking, heavy alcohol consumption) and/or increase the frequency of positive lifestyle behaviors (i.e., Mediterranean diet, physical activity, cognitively-stimulating activities) known to impact risk of MCI.
Table 1.
Selected risk and protective factors that have been significantly associated with diagnosis of mild cognitive impairment (MCI)
Both pharmacological and non-pharmacological interventions have been recommended for the treatment of MCI. Although a number of pharmacological strategies have been evaluated (e.g., acetylcholinesterase inhibitors such as donepezil, rivastigmine, and galantamine, Vitamin E, rofecoxib, piracetam, memantine) or are under current investigation, these are reviewed elsewhere (Jelic et al. 2006; Karakaya et al. 2013; Popp and Arlt 2011) and are beyond the scope of the present paper. Instead, the current paper evaluates the efficacy of non-pharmacological interventions for MCI, specifically CRTs, by reviewing randomized controlled trials of such interventions (see Tables 2 and 3). Although terminology varies across settings and publications, for the purposes of this review, CRT is defined as any systematic behavioral therapy specifically designed to improve cognitive performance, help individuals to compensate for impaired cognitive performance, or enable individuals to adapt to impaired cognitive performance. As described in the next section, CRTs include lifestyle interventions, psychotherapy, and/or traditional cognitive training approaches as long as they are specifically implemented as a treatment to address cognitive impairments.
Table 2.
Summary of key findings from randomized controlled trials evaluating the efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI)1
| Study | R CT |
C CT |
LF S |
PT X |
D | Objective Cognitive Performance |
Self-Report Measures | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A/I | M | EF | GC | SCC | DF | QOL | PS | O | |||||||||||||||
| S T |
L T |
S T |
L T |
S T |
L T |
s T |
L T |
S T |
L T |
S T |
L T |
S T |
L T |
S T |
L T |
S T |
L T |
||||||
| Focused Lifestyle Interventions | |||||||||||||||||||||||
| Bakeret al.2010 | -- | -- | Y | -- | - - |
Y | -- | N | -- | Y | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Bayer-Carter et al. 2011 | -- | -- | Y | -- | - - |
N | -- | Y | -- | N | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Kwok et al. 2011 |
-- | -- | Y | -- | - - |
-- | -- | -- | -- | -- | -- | Y | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Lam et al. 2011 | -- | -- | Y | -- | N | Y | -- | -- | -- | N | -- | N | -- | N | -- | -- | -- | -- | -- | N | -- | -- | -- |
| Nagam atsu et al. 2012 | -- | -- | Y | -- | - - |
N | -- | Y | -- | Y | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Scherder et al. 2005 | -- | -- | Y | -- | - - |
N | N | N | N | Y | N | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| van Uffelen et al. 2008 | -- | -- | Y | -- | - - |
Y | -- | Y | -- | N | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Focused Restorative Cognitive Training Intervention – Single Domain, Attention/Information Processing | |||||||||||||||||||||||
| Barnes et al. 2009 | Y | -- | -- | -- | - - |
Y | -- | N | -- | N | -- | N | -- | -- | -- | -- | -- | -- | -- | U | -- | -- | -- |
| Focused Compensatory Cognitive Training Intervention – Single Domain, Memory | |||||||||||||||||||||||
| Greena way et al. 2012 | -- | Y | -- | -- | - - |
-- | -- | -- | -- | -- | -- | N | N | -- | -- | Y | Y | N | N | N | N | Y 2 |
Y 2 |
| Comprehensive Interventions – Single Domain, Memory | |||||||||||||||||||||||
| Rapp et al. 2002 | -- | Y | -- | Y | - - |
-- | -- | N | N | -- | -- | -- | -- | Y | Y | -- | -- | -- | -- | -- | -- | Y 3 |
N 3 |
| Troyer et al. 2008 | -- | Y | Y | Y | - - |
-- | -- | N | N | -- | -- | -- | -- | N | N | N | N | -- | -- | -- | -- | Y 4 |
Y 4 |
| Comprehensive Interventions – Multi-Modal | |||||||||||||||||||||||
| Buschert et al. 2011 | Y | Y | Y | -- | - - |
N | -- | N | -- | N | -- | Y | -- | -- | -- | -- | -- | N | -- | Y | -- | -- | -- |
| Kinsella et al. 2009 | -- | Y | Y | Y | - - |
-- | -- | Y | Y | -- | -- | -- | -- | N | N | -- | -- | -- | -- | -- | -- | Y 5 |
N 5 |
| Tsolaki et al. 2011 | Y | -- | -- | Y | - - |
N | -- | Y | -- | Y | -- | Y | -- | -- | -- | Y | -- | -- | -- | -- | -- | -- | -- |
Note: Note that some studies included treated and untreated groups with dementia in addition to the MCI groups; only information on the MCI groups are included in this table.
Caregiver burden (ST - N; LT - N); Caregiver mood (ST-Y; LT – Y); Memory self-efficacy (ST-Y; LT - N).
Perceived impact of memory problems (ST - N; LT - N); compensatory memory strategy use (ST - N; LT - Y); perceived control over memory (ST - Y; LT - N).
Strategy use and knowledge (ST - Y; LT - Y); lifestyle importance (ST - N; LT - N).
Memory strategy use (ST – Y, LT - N), memory strategy knowledge (ST - Y; LT - Y), memory contentment (ST - N; LT - N).Abbreviations/Symbols: A/I = Attention/information processing. CCT = Did this study use a compensatory cognitive training approach? D = Were there statistically significant results that supported the efficacy of this intervention in terms of reducing the rate of conversion from MCI to dementia in the intervention group versus the control group? DF = Daily functioning/everyday functioning. EF = Executive function. GC = Global cognition. LFS = Did this study include lifestyle strategies? LT = Were there statistically significant results that supported the efficacy of this intervention in terms of the long-term benefits (>1 month since the intervention ended) in this outcome area? M = Memory. MCI = Mild cognitive impairment. N = No. O = Other relevant outcomes. PS = Psychiatric symptom severity. PTX = Does this intervention includes psychotherapeutic strategies such as relaxation training, stress management skills, mindfulness skills, cognitive restructuring, scheduling pleasurable activities, etc.? QOL = Quality of life. RCT = Did this study use a restorative cognitive training approach? SCC = Subject cognitive complaints. ST = Were there statistically significant results that supported the efficacy of this intervention in terms of the short-term benefits (≤1 month since the intervention ended) in this outcome area? U = Unclear/Although this outcome was measured, it is unclear from the methods or results whether this intervention was effective in this area. Y = Yes. -- = This study did not evaluate this outcome or use this approach.
Abbreviations/Symbols: A/I = Attention/information processing. CCT = Did this study use a compensatory cognitive training approach? D = Were there statistically significant results that supported the efficacy of this intervention in terms of reducing the rate of conversion from MCI to dementia in the intervention group versus the control group? DF = Daily functioning/everyday functioning. EF = Executive function. GC = Global cognition. LFS = Did this study include lifestyle strategies? LT = Were there statistically significant results that supported the efficacy of this intervention in terms of the long-term benefits (>1 month since the intervention ended) in this outcome area? M = Memory. MCI = Mild cognitive impairment. N = No. O = Other relevant outcomes. PS = Psychiatric symptom severity. PTX = Does this intervention includes psychotherapeutic strategies such as relaxation training, stress management skills, mindfulness skills, cognitive restructuring, scheduling pleasurable activities, etc.? QOL = Quality of life. RCT = Did this study use a restorative cognitive training approach? SCC = Subject cognitive complaints. ST = Were there statistically significant results that supported the efficacy of this intervention in terms of the short-term benefits (≤1 month since the intervention ended) in this outcome area? U = Unclear/Although this outcome was measured, it is unclear from the methods or results whether this intervention was effective in this area. Y = Yes. -- = This study did not evaluate this outcome or use this approach.
Table 3.
Summary of design characteristics and outcomes of randomized controlled trials evaluating the efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI)1
| Study | Inclusion and Exclusion Criteria |
Descriptio n of Control Group Condition (n) |
Description of Experiment al Group Intervention (n) |
Experiment al Group: Length of Sessions (L), # of Sessions (S), # of Weeks (W) |
ST Outcome Measures (SE?) |
LT Outcome Measures (SE?) |
F U |
|---|---|---|---|---|---|---|---|
| Focused Lifestyle Interventions | |||||||
| Baker et al. 2010 | Amnestic MCI (Petersen, 2004); no significant cardiac disease, cerebrovascular disease, musculoskeletal impairment, or medical conditions with psychiatric, neurologic, or metabolic sequela; sedentary adults with < 30 minutes 3×/wk of physical activity at baseline; no diabetic medications |
Stretching at intensity of below 50% of heart rate reserve (n = 10) |
High intensity aerobic exercise at intensity of 75% to 85% of heart rate reserve (n = 19) |
L = 45-60 S = 96 W = 24 |
SDMT (Y); verbal fluency (Y); stroop (Y); TMT B (Y); task switching (Y); story learning (N); list learning (N); delayed match to sample (N) |
-- | -- |
| Bayer-Carter et al. 2011 | Amnestic MCI (Roberts et al., 2008), delayed memory score 1.5 SD below expectation and consensus dx; no psychiatric disorders, alchoholism, neurologic disorders, renal/hepatic disease, diabetes, COPD, or cardiac issues; no cholesterol lowering medications |
Higher fat/glycemi c index diet (n = 15) |
Lower fat/glycemic index diet (n = 14) |
W=4 | Story recall (N); word list learning (N); BVMT (Y); TMT (N); stroop (N); verbal fluency (N) |
-- | -- |
| Kwok et al. 2011 |
MCI based on Chinese MMSE score of 20-25; ≥70 years old; no blindness, aphasia, or behavioral disturbance |
No- interventio n control (n=17) |
Chinese calligraphy training led by trained assistant (n=14) |
L = 30 S = 40 W = 8 |
MMSE (Y) | -- | -- |
| Lam et al. 2011 | Chinese subjects > 65 years old; CDR=0.5 or Mayo criteria for amnestic MCI; physically fit as judged by allied health professional; excluded if already regularly practicing Tai Chi |
Group stretching and toning (n=218) |
Simplified group Tai Chi (n=171) |
L = 30 S = 156 W = 52 |
CDR (Y); subjective memory complaints (N); ADAS-cog (N); digit span (N); visual span (Y); TMT (N); verbal fluency (N); Cantonese MMSE (N); Cornell Depression scale (N); Neuropsychiatr ic Inventory (N); Berg Balance Scale (Y) |
-- | -- |
| Nagamats u et al. 2012 | Women 70-80 years old; MOCA <26; subjective memory complaints |
Stretching, balance, toning exercises (n=28) |
Resistance training (n=28); aerobic training progressing to 70-80% heart rate reserve (walking; n=30) |
L = 60 S = 48 W = 24 |
Stroop (Y); TMT (N); verbal digits test (N); associative memory (Y); everyday problems test (N); short physical performance battery (Y); six- minutewalk test (Y) |
-- | -- |
| Scherder et al. 2005 | Frail elderly with MCI (Petersen et al., 1999); short version of MMSE ≥7; no AD, alcoholism, head trauma, hydrocephalus, neoplasm, epilepsy, disturbance of consciousness, focal brain disorders |
No interventio n control (n = 15) (8 received social visits and 7 were daily activities as usual) |
Walking (n=15); hand/face exercises (n=13) |
L = 30 for walking, 15 for hand/face S = 18 W = 6 |
Category fluency (Y); TMT (Y); digit span (N); visual memory span (N); dutch version of CVLT (N); Rivermead face recognition (N); Rivermead picture recognition (N) |
Category fluency (N); TMT (N); digit span (N); visual memory span (N); dutch version of CVLT (N); Rivermead face recognition (N); Rivermead picture recognition (N) |
6 wk |
| Van Uffelen et al. 2008 | MCI (Petersen et al., 1999); community dwelling; 70-80 years old; able to walk independently; no B-vitamin supplementation; no epilepsy, multiple sclerosis, Parkinson’s, hemodiaysis, or psychiatric impairment; GDS < 6; no alcohol abuse; no medications for rheumatoid arthritis or psoriasis |
Low intensity, nonaerobic activity (e.g., flexibility, balance, posture (n = 75) |
Moderate intensity walking (n=77) |
L = 60 S = 104 W = 52 |
RAVLT (Y); verbal fluency (N); digit symbol substitution test (N); stroop (Y) |
-- | -- |
| Focused Restorative Cognitive Training Intervention – Single Domain, Attention/Information Processing | |||||||
| Barnes et al. 2009 | MCI (Winblad et al., 2004); stable on medications |
Computer activities on provided laptop at home (games, audio books, reading) (n = 25) |
Posit Science auditory processing exercises on provided laptop at home (n = 22) |
L = 100 S = 30 W = 6 |
RBANS Attention (N); spatial span (Y); RBANS Immediate Memory (N); RBANS Delayed Memory (N); CVLT total learning (N); CVLT Delayed Recall (N); DKEFS Trails (N); DKEFS Design Fluency (N); Global cognition – RBANS (N); Geriatric Depression Scale (U) |
-- | -- |
| Focused Compensatory Cognitive Training Intervention – Single Domain, Memory | |||||||
| Greenaway et al. 2012 | Amnestic MCI (Petersen, 2004); informant with twice weekly contact; DRS-2 > 120; stable on medications |
Calendar provision (n = 20) |
Calendar provision plus Memory Support System training in appointment s, to do list, and journaling (n = 20) |
L = 60 S = 12 W = 6 |
DRS-2 (N); MMSE (N); eCOG (Y); QoL–AD (N); Depression – CESD (N); caregiver burden (N); caregiver mood (Y); memory |
DRS-2 (N); MMSE (N); eCOG (Y); QoL – AD (N); Depression – CESD (N); caregiver burden (N); self efficacy (Y |
6 m o caregiver mood (Y); memory self efficacy (N) |
| Comprehensive Interventions – Single Domain, Memory | |||||||
| Rapp et al. 2002 | MCI (Petersen et al., 1999) | No treatment (n = 10) |
Education about memory loss, relaxation training, compensator y memory strategy training, and cognitive restructuring for memory related beliefs (n = 9) |
L = 120 S = 6 W = 6 |
Word list memory task (N); grocery list memory task (N); names and faces memory task (N); paragraph recall task (N); perceived memory ability -MCIn and MFQ (Y); perceived control over memory - MCIn (Y); use of memory strategies - MFQ (N); perceived impact of memory problems - MFQ (N) |
Word list memory task (N); grocery list memory task (N); names and faces memory task (N); paragraph recall task (N); perceived memory ability - MCIn and MFQ (Y); perceived control over memory - MCIn (N); use of memory strategies - MFQ (N); perceived impact of memory problems - MFQ (N) |
-- |
| Troyer et al. 2008 | MCI (Petersen, 2004) | Waitlist control (n = 24) |
Compensato ry memory strategies in attention; intensive lifestyle education including relaxation and stress management skills, nutrition skills, community resources, importance of recreational activities, physical exercise, and cognitive activities (n = 24) |
L = 120 S = 10 W = 26 |
Memory strategy use – MMQ (Y), memory task (Y); memory strategy knowledge (Y); self-reported memory ability – MMQ (N); memory contentment - MMQ (N); perceived impact of memory on daily functioning (N); perceived importance of lifestyle factors’ impact on memory (N); face name learning (N); number learning N); wordlist learning (N) |
Memory strategy use – MMQ (Y), memory task (Y); memory strategy knowledge (Y); selfreported memory ability - MMQ (N); memory contentme nt - MMQ (N); perceived impact of memory on daily functioning (N); perceived importance of lifestyle factors’ impact on memory (N); face name learning (N); number learning (N); wordlist learning (N) |
3 m o |
| Comprehensive Interventions – Multi-Modal | |||||||
| Buschert et al. 2011 | Amnestic MCI (Petersen et al., 2001); MMSE ≥ 23; ≥ 50 years; adequate vision and hearing for participation; no major medical or psychiatric disorder or disability precluding participation; stable on medications ≥ 3 months; no cognitive intervention in past year |
Monthly group meetings with paper pencil cognitive activities (n = 12) |
Restorative cognitive training exercises and compensator y cognitive strategies in attention, memory, and executive function; reminiscence , psychomotor , recreational, creative, and social activities; discussion groups;aging education (n = 12) |
L = 120 S = 20 W = 26 |
MMSE (Y); ADAS-cog (Y); RBANS – immediate story recall (N), delayed story recall (N); TMT A (N); TMT B (N); depression - MADRS (Y); QoL-AD (N) |
-- | -- |
| Kinsella et al. 2009 | Amnestic MCI (Petersen, 2004; Winblad et al., 2004); no cormorbidities associated with functional decline or cognition; no major psychiatric disorders; no significant cerebrovascular disease; no significant hearing, vision, or communication impairments; English speaking |
Waitlist control (n = 22) |
Training in compensator y memory strategies and external memory aids; training in strategies to improve organization al and attention skills in approaching learning and remembering ; discussion of coping strategies; education about lifestyle strategies including physical exercise and cognitive activities (n = 22) |
L = 90 S = 5 W = 5 |
Prospective memory tasks (Y); MMQ – perceived memory ability (N), contentment associated with memory (N), memory strategy usage (Y); SKR - memory strategy knowledge (Y) |
Prospectiv e memory tasks (Y); MMQ – perceived memory ability (N), contentment associated with memory (N), memory strategy usage (N); SKR - memory strategy knowledge (Y) |
4 m o |
| Tsolaki et al. 2011 | MCI (Petersen et al., 2001); free of neuropsychiatric symptoms per the Neuropsychologic al Inventory; no history of stroke or ischemic lesions; No cholinesterase inhibitors; no dementia; no lack of insight into deficits; no visual/hearing impairments or reading/writing disability that would preclude cognitive training |
No therapy (n = 72) |
Practice of paper-pencil and oral tasks of attention and executive function with ecological validity; practice of tasks aimed at enhancing memory; cognitivebehavioral techniques such as autogenic relaxation and progressive muscle relaxation (n = 104) |
L = 60 S = 60 W = 26 |
Visual or verbal memory - RBMT (N), RAVLT (N), ROCFT Delayed Recall (N), MoCA memory subtest (Y); Attention – TEA (N), WAIS-R Digit Symbol (N); Executive Function – FUCAS (Y), TMT B (N), FAS (N); Language – BNT (N), BDAE (N); Visual Construction – ROCFT Copy (Y), MoCA Clock Drawing (Y); Daily Functioning – FRSSD (Y); MMSE (Y); MoCA (Y) |
-- | -- |
Note: Note that some studies included treated and untreated groups with dementia in addition to the MCI groups; only information on the MCI groups are included in this table. Abbreviations: AD = Alzheimer’s disease. ADAS – cog = Alzheimer’s Disease Assessment Scale – cognitive subscale. ADL = Activities of daily living. BADL = Basic Activities of Daily Living. BDAE = Boston Diagnostic Aphasi Examination. BNT = Boston Naming Test. CCMB = Cote-des-Neiges Computerized Memory Battery. CDR = Clinical Dementia Rating. COPD = Chronic obstructive pulmonary disease. CR = Clinical Dementia Rating. DRS = Dementia Rating Scale. dx = Diagnosis. FRSSD = Functional Rating Scale of Symptoms of Dementia. FU = Long-term follow-up period, in months. FUCAS = Functional Cognitive Assessment Scale. GDS = Geriatric Depression Scale. IADL = Instrumental Activities of Daily Living. ICQ = Illness Cognition Questionnaire. L = Length of sessions, in minutes. LT = Long-term (>1 month since the intervention ended). MADRS = Montgomery Asberg Depression Rating Scale. MCI = Mild cognitive impairment. MCIn = Memory Controllability Inventory. MFQ = Memory Functioning Questionnaire. MMQ = Multifactorial Metamemory Questionnaire. MMSE = Mini Mental Status Exam. mo = months. MoCA = Montreal Cognitive Assessment. n = Group sample size. N = No. NPI = Neuropsychiatric Symptom Inventory. PMS = Profile of Mood States. PPT = Physical Performance Test. QoL-AD = Quality of Life-Alzheimer’s Disease. RAVLT = Rey Auditory Verbal Learning Test. RBMT = Rivermead Behavioral Memory Test. ROCFT = Rey Osterrieth Complex Figure Test. SE? = Were there statistically significant results indicating that the intervention was associated with improvement on this measure, above and beyond any that were observed in the control group, OR that the intervention was associated with significantly less decline on this measure than what was seen in the control group? S = Number of sessions. SD = standard deviation. SKR = Strategy Knowledge Repertoire. ST = Short-term (≤ 1 month since the intervention ended). STAI = State Trait Anxiety Inventory. TEA = Test of Everyday Attention. TMT = Trail Making Test. W = Number of weeks over which the intervention was conducted. WAIS-R = Wechsler Adult Intelligence Scale, Revised. Wk = weeks. Y = Yes.
Theoretical Rehabilitation Model of MCI: Course, Risk and Protective Factors, and Treatment Targets
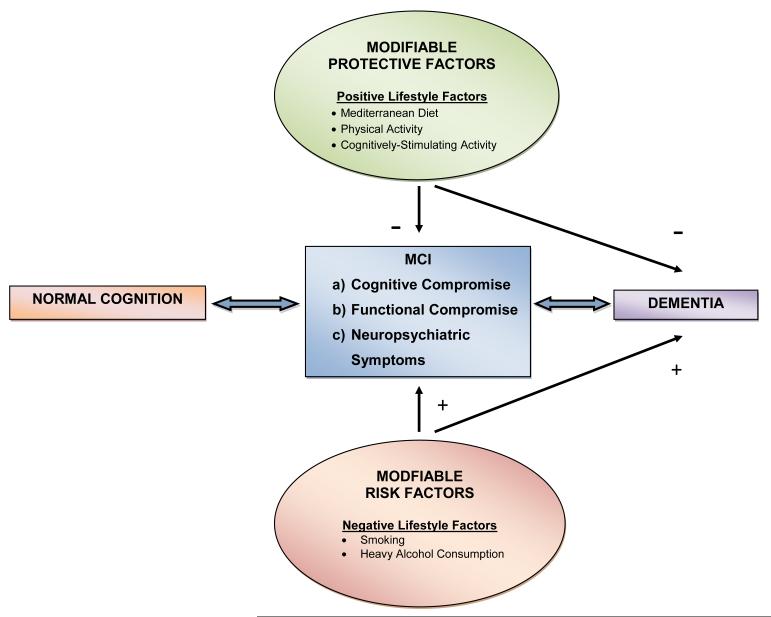
A theoretical rehabilitation model of MCI can provide a conceptual framework to inform development of CRTs for MCI as well as to guide selection of appropriate outcome measures for clinical trials that evaluate the impact of these interventions. Here we offer a provisional theoretical rehabilitation model based on the available literature that was reviewed and summarized in the Introduction, as well as the clinical trials that were systematically reviewed in the Results section below. In this model (Fig. 1), MCI is viewed as an intermediate stage between healthy age related cognitive decline (i.e., normal cognition) and dementia, though potential outcomes of MCI can also include chronic MCI without conversion to dementia or a return to normal cognition. The etiology of MCI and dementia are viewed as multifactorial; risk factors contribute toward an increased risk of MCI and dementia, while protective factors contribute toward a reduced risk. Thus, brain function and dysfunction are mediated and moderated by multiple risk and protective factors, including those listed in Table 1. In some individuals, the cumulative and interactive impact of these factors on the brain results in the behavioral manifestation known as MCI which, as depicted in Fig. 1, is characterized by three types of symptoms : (a) mild cognitive compromise (measured by objective neuropsychological tests), (b) mild functional compromise not yet precluding independent living (evaluated by measures of daily functioning and QOL), and (c) commonly associated neuropsychiatric symptoms such as depression, anxiety, fatigue, and sleep difficulties (measured by neuropsychiatric symptom severity scales).
Fig. 1. Theoretical rehabilitation model of mild cognitive impairment (MCI) to guide the development and evaluation of cognitive rehabilitation therapies (CRTs) for MCI.
In this provisional rehabilitation model, MCI is viewed as an intermediate stage between normal cognition and dementia. Individuals with MCI may alternatively return to normal cognition or present with a persistent MCI that does not convert to dementia. The etiology of MCI and dementia are viewed as multifactorial, and a range of risk and protective factors, including those listed in Table 1, contribute toward increased or decreased risk, respectively. In some individuals, the cumulative and interactive impact of these factors on the brain results in the behavioral manifestation known as MCI which is characterized by three types of symptoms: (a) mild cognitive compromise (measured by objective neuropsychological tests), (b) mild functional compromise not yet precluding independent living (evaluated by measures of daily functioning and quality of life), and (c) commonly associated neuropsychiatric symptoms such as depression, anxiety, fatigue, and sleep difficulties (measured by neuropsychiatric symptom severity scales). Based on this model, the figure identifies the key intervention targets that CRTs for MCI are likely to address. Specifically, CRTs can target the symptoms of MCI (i.e., cognitive compromise, functional compromise, or associated neuropsychiatric symptoms). Or, they may target modifiable risk and protective factors, particularly the lifestyle factors that are highlighted in the figure because they are known to increase (depicted as arrows with plus signs) or decrease (depicted as arrows with negative signs) risk for MCI and dementia. In a clinical trial, appropriate intervention outcomes would include reducing MCI symptoms (i.e., symptom management), reducing the conversion rate from MCI to dementia (i.e., preventing dementia), or increasing the conversion rate from MCI to normal cognition (i.e., curing MCI).
This theoretical rehabilitation model yields a number of plausible intervention targets for individuals with MCI, which are highlighted in Fig. 1 and include the symptoms of MCI (i.e., cognitive compromise, functional compromise, and neuropsychiatric symptoms) as well as modifiable risk and protective factors, particularly the lifestyle factors known to be associated with risk of MCI. Although CRTs are heterogeneous in terms of content and methods, integration of the literature with our model indicates that they can be designed to include any combination of four broad approaches, each directly or indirectly targeting different aspects of the model. Regardless of the combination of approaches used, all CRTs aim to reduce the symptoms of MCI (i.e., symptom management), delay or prevent progression to dementia (i.e., prevention of dementia), or increase the rate of conversion to normal cognition (i.e., curing MCI): 1) Restorative cognitive training most directly targets cognitive compromise (a). It aims to enhance or restore cognitive abilities, potentially through neuroplastic mechanisms. A common restorative approach utilizes structured and repeated practice of specific cognitive tasks and mental exercises that may or may not be computerized as a means of improving abilities in specific cognitive domains. 2) Compensatory cognitive training most directly targets functional compromise (b). It teaches individuals skills and strategies to compensate for cognitive impairments so that the impact of these deficits on daily function and QOL can be reduced. Compensatory strategies can include internal strategies (e.g., using visual imagery, chunking or acronyms to compensate for memory difficulties, using structured problem-solving and planning methods to compensate for executive dysfunction), external strategies (e.g., using day planners, timers, and navigation devices), or environmental strategies (e.g., setting up a quiet work space devoid of visually distracting stimuli). 3) Lifestyle interventions most directly target modifiable risk and protective factors, namely the positive and negative lifestyle factors highlighted in Fig. 1, that are associated with MCI or dementia. Lifestyle interventions educate individuals about the cognitive benefits of healthy lifestyle practices and the negative consequences of unhealthy lifestyle practices and encourage individuals to make changes to their life to improve the balance of these risk and protective factors. Lifestyle strategies can include regular physical exercise, healthy nutrition (i.e., Mediterranean diet), frequent participation in cognitively-stimulating activities, and reduction of other modifiable risk factors such as smoking and heavy alcohol consumption. Lifestyle approaches either directly engage individuals in healthy lifestyle practices (e.g., through an exercise, diet, or leisure time program) or they aim to change lifestyle practices and behaviors through education, encouragement, and other behavioral strategies (e.g., motivational interviewing) with the goal of improving MCI outcomes. Lifestyle interventions do not include interventions that are restricted to basic MCI psychoeducation (e.g., definitions of MCI, prognosis, etiology) or administration of specific dietary supplements (e.g., Vitamin B, folic acid, omega-3 fatty acids) or medications. 4) Psychotherapeutic interventions most directly target neuropsychiatric symptoms (c) that are common among individuals with MCI (e.g., depression, anxiety, fatigue, poor sleep). Unlike lifestyle interventions, this approach incorporates more traditional psychotherapy techniques to address accompanying neuropsychiatric symptoms and thus can include relaxation exercises, mindfulness techniques, skills to manage stress, fatigue, and poor sleep, and cognitive behavioral techniques such as cognitive restructuring to address negative thoughts and feelings related to MCI.
It should be noted that comprehensive treatment for MCI is likely to include services other than CRTs. Indeed, based on this rehabilitation model, other risk factors not highlighted in Fig. 1, such as many of the disease factors listed in Table 1, are likely best addressed through referral to other specialty providers for medications and/or other interventions besides CRT (e.g., diabetes, renal failure, polypharmacy). Some risk factors like cardiovascular disease or sleep disorders could benefit from both medical and behavioral interventions, and some risk factors may be addressed through both elements of CRT as well as other specialty providers (e.g., depression, smoking).
Lastly, it is worth acknowledging that there can be some overlap between the four CRT approaches described above. For example, restorative cognitive training contrasts with compensatory cognitive training by focusing on extensive repetition of carefully designed cognitive tasks (usually specific to an individual’s deficits, such as N-back tasks to enhance attention) as a way of strengthening neural circuits and improving performance on similar tasks through generalization. Compensatory cognitive training instead focuses on teaching a range of compensatory strategies (i.e., internal, external, and environmental) that an individual then practices throughout their daily life (e.g., using a planning worksheet to facilitate completion of important home and work projects). An individual may nevertheless employ certain compensatory skills while engaging in restorative exercises (e.g., chunking information). Moreover, while compensatory cognitive training focuses on application of strategies to improve daily functioning, use of these skills may also improve an individual’s objective cognitive performance on certain tests (e.g., categorizing during list learning tests). Similarly, although a lifestyle intervention aims to increase or decrease the frequency of a lifestyle behavior associated MCI risk (i.e., exercise, cognitively-stimulating activities, heavy alcohol consumption), certain psychotherapeutic strategies could be employed to achieve this aim (e.g., motivational interviewing). Likewise, although psychotherapeutic interventions use more traditional psychotherapeutic techniques to target neuropsychiatric symptoms associated with MCI (e.g., mindfulness to address depression and anxiety), lifestyle interventions can also reduce neuropsychiatric symptoms (e.g., exercise). Despite this overlap, the distinctions are offered as part of the proposed provisional rehabilitation model to aid in the development, evaluation, and comparisons of future CRTs. While some providers clearly identify with and employ only one approach, others integrate several. Thus, these distinctions may help the field ultimately determine which elements most effectively treat which aspects of MCI.
Objectives
The primary objective of this review is to evaluate the evidence for the efficacy of CRTs for older adults with MCI. As with other forms of rehabilitation (e.g., physical, occupational), CRTs aim to enhance an individual’s daily functioning and QOL, rather than to treat disease per se. Thus, our review will evaluate the efficacy of CRTs for older adults with MCI in terms of their short-term (< 1 month following the intervention) and long-term (≥ 1 month following the intervention) impact on objective cognitive performance, with a focus on attention/information processing, memory, executive function, and global cognition. Additionally, we will evaluate efficacy in terms of CRTs impact on subjective cognitive complaints, daily functioning/everyday functioning, QOL, neuropsychiatric symptom severity, and other related constructs. Lastly, we will evaluate whether CRTs reduce conversion rates to dementia.
Based on our theoretical model and in an attempt to elucidate which approaches are most effective, we will distinguish between interventions that are Focused on one approach (i.e., restorative cognitive training, compensatory cognitive training, lifestyle interventions, psychotherapeutic interventions) versus Comprehensive interventions that entail multiple approaches. Because interventions that entail either restorative or compensatory cognitive training approaches can target one or more cognitive domains, we will also distinguish between Single Domain and Multi-Modal CRTs.
Methods
A systematic review of peer-reviewed journal articles was conducted on 10/25/12 using Pub Med. The following search terms were applied to all fields: (mild cognitive disorder OR MCI OR mild cognitive decline) AND (cognitive rehabilitation OR cognitive intervention OR cognitive training OR cognitive stimulation OR attention rehabilitation OR attention training OR information process training OR memory rehabilitation OR memory intervention OR memory training). Filters included publication dates between 1/1/1990 and 10/25/12, clinical trial, and published in English.
Articles included in the final review met the following criteria: 1) The study primarily evaluated the effects of a CRT intervention for MCI. 2) The study was a randomized controlled trial that quantitatively assessed outcomes at both pre- and post-intervention. 3) The study included at least one intervention group meeting criteria for MCI, and at least one demographically similar group of non-treated adults meeting criteria for MCI, AND the study employed adequate statistical analyses to compare change from pre- to post intervention across groups (e.g., repeated measures ANOVA, mixed effects model, slope analysis). If the study did not employ a repeated measures between group analysis or slope analysis, at a minimum the study compared change across time within each group, and then also compared results across groups at both pre- and post- intervention. 4) If individuals with dementia were included in the study, the results from individuals with MCI were reported separately from those with dementia. 5) Samples included community dwelling adults. 6) Sample sizes were ≥ 5/group. 7) The study included pre- and post-intervention outcome measures that evaluated objective cognitive performance using neuropsychological tests AND/OR self-report outcome measures that assessed subjective cognitive complaints, daily functioning/everyday functioning, QOL, neuropsychiatric symptom severity, or another related construct. We excluded studies which primarily focused on neuroimaging results.
Results: Efficacy of CRTs for MCI
293 articles were initially identified through PubMed using the search terms described. After scanning titles and abstracts from these 293 articles, 34 articles were identified as potentially meeting our review criteria. The other 259 articles were rejected because it was clear from the abstracts that they did not meet one or several of the seven review criteria outlined in the Methods. The most common exclusions were that the study did not include a CRT intervention (e.g., the study was a medication trial) or that it did not include a group with MCI (e.g., the groups included only healthy older adults or adults with dementia). The complete manuscripts of the 34 remaining articles were then reviewed, and 20 additional articles were rejected because they did not meet all seven criteria outlined in the Methods. The most common exclusion at this stage was that the study was not a randomized controlled trial. In the end, 14 articles were found eligible for final review based on all seven criteria described in our Methods.
A summary of key findings and design characteristics/outcomes from the studies that were selected for final review can be found in Tables 2 and 3, respectively. Results are also described by intervention type below. Only results from studies with p ≤ 0.050 were deemed significant and are described as such in the tables and text. In terms of focused interventions (i.e., using only one approach), we identified seven lifestyle interventions, and one compensatory cognitive training intervention (single-domain, focused on memory). In terms of comprehensive interventions that utilized multiple approaches, we identified two single-domain interventions focused on memory, and three multi-modal interventions focused on multiple domains.
Focused Lifestyle Interventions
Over the past decade there has been a substantial increase in the scientific literature examining lifestyle interventions as a means to stave off negative cognitive aging outcomes. The bulk of the evidence suggests that exercise and cognitively stimulating activities are effective behavioral interventions for improving cognition and lowering risk of dementia (Jak 2012). However, to date, most 10 evidence has come from epidemiological and cross sectional studies (Sofi et al. 2011; Verghese et al. 2006; Wilson et al. 2002; Wilson et al. 2007; Wilson et al. 2012); randomized trials have been less common. Furthermore, most existing studies have targeted normally aging populations while fewer have evaluated the ability of these strategies to positively impact outcomes in those who already have MCI.
Our search produced seven randomized controlled trials investigating lifestyle interventions in individuals with MCI. Rather than relying on lifestyle education and encouragement, all of these studies directly engaged participants in a program of cognitively stimulating activity (Kwok et al. 2011), physical activity (Baker et al. 2010; Lam et al. 2011; Nagamatsu et al. 2012; Scherder et al. 2005; van Uffelen et al. 2008), or diet (Bayer-Carter et al. 2011). As a whole, these studies demonstrated that lifestyle interventions can significantly improve objective cognitive performance in those with MCI. Specifically, significant (p ≤ 0.050) improvements in executive functioning were noted following aerobic exercise interventions of at least 30 minutes per day, at least three days per week for a minimum of six weeks (Scherder et al. 2005). Aerobic activity for at least 45 minutes per day, four to five days per week for at least 12 weeks produced significant improvements in more than one cognitive domain (Baker et al. 2010; van Uffelen et al. 2008). Non-aerobic activity, namely resistance training and tai chi, was significantly associated with improvements in executive functioning and memory (Nagamatsu et al. 2012) and attention (Lam et al. 2011) in individuals with MCI. Following a lower fat and glycemic index diet for four weeks resulted in significant increases in visual memory (Bayer-Carter et al. 2011). Practicing a single cognitively stimulating activity, namely calligraphy with a trained instructor, 30 minutes daily, five days a week for 8 weeks led to significant increases in global cognition as compared to a no-intervention control (Kwok et al. 2011).
These studies in aggregate had several significant limitations. Only one of the seven studies included extended follow-up and did not identify sustained benefits of lifestyle interventions (Scherder et al. 2005). Only one study evaluated the risk of progression to AD and did not find a significant effect (Lam et al., 2011). Other weaknesses of this literature included questionable diagnosis of MCI, relying strongly or exclusively on cognitive screening measures (e.g., Kwok et al. 2011; Nagamatsu et al. 2012), poor compliance with the prescribed intervention (e.g., Nagamatsu et al. 2012; van Uffelen et al. 2008), and too much of the intervention period working toward criterion and therefore fewer weeks exercising at the prescribed intensity level. The neuropsychological measures examined in the lifestyle intervention trials were largely time-based with no adjustment for processing speed; it is therefore difficult to tease apart whether gains on executive functioning measures were simply increased speed or actual improvements in higher level thinking. The use of no-intervention control groups (e.g., Kwok et al. 2011) was a significant methodological weakness of several of the studies and limited confidence that any cognitive gains were due to the specific lifestyle intervention (e.g., physical exercise) rather than added social contact or a general increase in daily activity. Finally, objective cognitive performance was the predominant outcome measure in this literature. There was little examination of daily functioning, QOL, or neuropsychiatric symptom changes following lifestyle interventions.
Focused Restorative Cognitive Training Intervention - Single Domain, Attention/Information Processing
Only one trial (Barnes et al. 2009) focused on improving attention through restorative cognitive training, with the notion that improvements in auditory attention and discrimination would yield downstream effects on other cognitive domains, such as memory. Using an intensive computerized cognitive training intervention (100 mins/day, 5 days/week for 6 weeks), compared to a robust computer activities control group, the authors found that the experimental group significantly improved on a spatial span task, but not on any other cognitive tests from a comprehensive battery. It is unclear from their design if significant treatment effects would have been found relative to a no intervention or a less cognitively stimulating control group. This study did not examine long-term outcomes or impact on conversion rates from MCI to cognitive normalization or dementia.
Focused Compensatory Cognitive Training Intervention - Single Domain, Memory
One study focused on improving memory through compensatory cognitive training (Greenaway et al. 2012). Greenaway et al. (2012) emphasized training in calendars and notebooks 2 hours/week for 6 weeks, including setting appointments, adding “to do” items, and journaling. Compared to controls, the experimental group significantly improved in their daily functioning and memory self-efficacy, and the improvements in daily functioning (but not memory self-efficacy) were sustained six months post-intervention. Treatment-associated changes on measures of objective global cognition, QOL, or neuropsychiatric symptom severity did not reach significance, perhaps because these were not the targets of treatment. This study did not examine impact on conversion rates to cognitive normalization or dementia.
Comprehensive Interventions - Single Domain, Memory
The two comprehensive interventions that targeted memory as a single domain (Rapp et al. 2002; Troyer et al. 2008) both provided training in compensatory memory skills, and both employed no-contact control groups. Rapp and colleagues’ (2002) intervention entailed six 2-hour sessions spaced across six weeks and included training in compensatory memory skills along with psychoeducation and relaxation (breathing) training. Compared to controls, experimental subjects showed no significant improvement on objective memory test performance, but they did endorse significantly better memory abilities at post-test and 6-month follow-up, as well as significantly increased control over memory at post-test and significantly greater use of mnemonic strategies at follow-up. Troyer and colleagues’ (2008) intervention entailed ten 120-minute sessions spaced across six months, one hour devoted primarily to compensatory memory training, and the other hour devoted to intensive lifestyle education as well as psychotherapeutic techniques. Although aspects of the intervention were commendable (e.g., inclusion of specialists such as dieticians in the lifestyle component, connecting participants with community resources to increase their activity level, spacing the sessions over many months to potentially extend the benefits of the intervention), most results were non-significant. Compared to the control group, the experimental group reported significantly increased knowledge and use of compensatory memory strategies as well as a significantly stronger belief in the importance of lifestyle factors, which were sustained three months post-intervention; however, the experimental group did not evidence significant improvement on measures of objective memory performance, subjective memory complaints, or daily functioning. Because the outcome measures were created by the authors and the psychometric properties of the objective memory measures have not been previously reported, the non-significant results are difficult to interpret (i.e., was the intervention ineffective or were the measures inadequate?). Neither study examined conversion rates to cognitive normalization or dementia.
Comprehensive Interventions - Multi-Modal
Three eligible studies were identified (Kinsella et al. 2009; Buschert et al. 2011; Tsolaki et al. 2011). Two studies included restorative training (Buschert et al. 2011; Tsolaki et al. 2011), two compensatory training (Kinsella et al. 2009; Buschert et al. 2011), two lifestyle approaches (Kinsella et al. 2009; Buschert et al. 2011), and two psychotherapeutic techniques (Kinsella et al. 2009; Tsolaki et al. 2011). Kinsella and colleagues’ (2009) intervention entailed five 90-minute sessions spaced across five weeks. Like Troyer and colleagues’ (2008) intervention, sessions primarily focused on compensatory memory training and included lifestyle education as well as psychotherapeutic techniques; the intervention also included some training in organization and attention skills to improve learning and memory. Using the same measures as used in the Troyer et al. (2008) study, this intervention was similarly associated with significantly increased knowledge and use of compensatory memory strategies but not with significant improvements in subjective memory complaints, calling into question the sensitivity of this latter measure. Compared with the control group, the experimental group evidenced significant improvements on two objective measures of prospective memory [different from the memory measures used in the Troyer et al. (2008) study] that were sustained three months post-intervention.
Buschert and colleagues’ (2011) intervention entailed twenty 120-minute sessions spaced over six months and employed restorative and compensatory cognitive training in attention, memory and executive function as well as intensive lifestyle interventions that increased participants’ cognitive and physical activity levels through inclusion of reminiscence, psychomotor, recreational, creative, and social activities in class. Relative to the non-treated control group, this intensive intervention was associated with only modest to questionable improvements on well-validated measures of objective cognitive performance, though these results are difficult to interpret because of insufficient statistical power (n = 12/group). Specifically, relative to the control group, the experimental group evidenced improvements on measures of memory (i.e., RBANS story recall) and attention/executive function (i.e., TMT B) that appeared promising but only trended near significance (p < 0.100). Moreover, relative to the experimental group, the control group evidenced significant decline on one measure of global cognition (ADAS-cog), but this pattern only trended toward significance on another measure of global cognition (i.e., MMSE). Although the intervention was not associated with improvements on a QOL measure designed for individuals with AD, it is conceivable that this measure was not sensitive to the issues that individuals with MCI (rather than dementia) encounter. Interestingly, this was the only comprehensive intervention to include a measure of neuropsychiatric symptom severity (i.e., MADRS); the intervention was associated with significant improvements on this measure, suggesting that comprehensive CRTs may effectively target MCI-associated neuropsychiatric symptoms. This study did not evaluate long-term outcomes.
Tsolaki and colleagues’ (2011) intervention entailed sixty 60-minute sessions spaced across six months, focused on restorative cognitive training in attention, memory, and executive function, and also included psychotherapeutic techniques. Whereas previously described multi-modal studies had sample sizes < 25/group, this study was notable for its large sample size (treatment group, n = 104; control group, n = 72). Significant improvements from pre- to post-intervention were observed in the experimental group on objective measures of global cognition, attention, memory, executive function, visuomotor construction, language and daily functioning, whereas the only significant change noted in the control group was a decline in daily functioning. Groups did not differ on any measures pre-intervention, and between group comparisons post-intervention reached significance on one measure of daily functioning and on some but not all objective measures of cognition. However, interpretation of results was limited by a failure to include a repeated measures between group analysis of change over time (e.g., repeated measures ANOVA, mixed effects model, slope analysis). This study did not evaluate long-term outcomes.
Discussion: Summary and Future Directions
Overall, the results of randomized controlled trials evaluating the efficacy of CRTs for MCI can be categorized as encouraging but inconclusive. Perhaps because research on interventions for MCI is only in a very early stage, common design limitations (e.g., small sample size, inclusion of measures without established psychometric properties, less than optimal statistical analyses, failure to include long-term outcomes) hamper interpretation of study findings, particularly non-significant results. Although larger, well-designed randomized controlled trials are required before CRTs for MCI can be considered evidence-based, relevant trends from existing randomized controlled trials are discussed below.
Importantly, the three studies that included measures of compensatory strategy use and knowledge (Troyer et al. 2008; Kinsella et al. 2008; Rapp et al. 2002) and the one study that included a measure of the degree to which individuals rate lifestyle strategies as important (Troyer et al. 2008) found that interventions were associated with significant improvements on these measures. Consistent with research showing that individuals with MCI show learning potential and cognitive plasticity (Akhtar et al. 2006; Schreiber and Schneider 2007), these findings indicate that CRTs can effectively change targeted behaviors, knowledge, and beliefs in older adults with MCI, that adults with MCI are teachable, and that additional CRT trials are warranted with this population.
In terms of effects on objective cognitive performance, all of the seven focused lifestyle interventions and the three comprehensive multi-modal interventions were associated with significant improvements in at least one cognitive domain, suggesting that these approaches are perhaps the most promising (yet difficult to implement). The one single domain intervention that used restorative training to focus on attention found significant improvements in attention. None of the three single domain interventions that focused on memory found significant improvements in any cognitive domain, including memory. However, these latter three studies included only very brief neuropsychological batteries assessing either memory or global cognition. In contrast, most of the other studies employed comprehensive batteries and found one or more effects. Thus, the bulk of the evidence indicates that CRTs for MCI are associated with some improvements in objective cognitive performance, but the pattern of effects on specific cognitive domains is inconsistent across studies.
Other important outcomes were only infrequently assessed across studies and require further investigation. Three of the four studies that included measures of subjective cognitive complaints did not find significant treatment-associated improvements, and results on subjective cognitive complaint measures did not correspond with results on objective cognitive performance measures (i.e., one study found subjective improvement but not objective improvement, two found objective improvement but not subjective improvement, and one found neither objective nor subjective improvement). Although patients’ subjective cognitive complaints are important to understand and warrant further investigation in future trials, the present results suggest that general measures of subjective cognitive complaints may not prove optimal or sensitive to change (e.g., “To what extent would you rate your memory as poor?”). In contrast, two of the three studies that included measures of daily functioning found significant treatment-associated improvements on these measures. This suggests that that individuals with MCI may be better able to perceive changes in their ability to perform daily tasks related to cognition than to assess general cognitive ability per se, and that these more specific self-report measures may be more appropriate for clinical trials (e.g., “How often do memory problems interfere with your ability to follow through with important responsibilities, tasks, or roles in your family life?”). The only study that included a collateral measure of daily functioning (Greenaway et al. 2012) found a significant treatment-associated effect on this measure, raising the possibility that collateral measures of daily functioning might prove more sensitive and reliable than self-report measures. Only two studies examined QOL and neither found significant treatment-associated effects on these measures. Because both of these studies employed QOL measures designed for individuals with AD, it is possible these measures were not sensitive to MCI specific concerns. Of the studies that examined neuropsychiatric symptom severity, two did not find significant treatment-associated effects on these measures, one did, and one did not employ adequate analyses to determine effects. However, since none of the studies that incorporated psychotherapeutic techniques as part of their intervention assessed neuropsychiatric symptom severity, it is unclear whether inclusion of such an approach would more effectively target this outcome. Only two studies examined long-term outcomes, one finding sustained effects, the other not. Only one study evaluated conversion rates to dementia and found non-significant treatment effects.
The studies that were reviewed varied markedly in terms of their intervention design and selected outcome variables, with no clear pattern regarding which intervention approaches were more or less effective. One of the obstacles contributing to the variation in approaches to this research has likely been the lack of a theoretical rehabilitation model of MCI to guide the development of these interventions and the selection of appropriate outcome measures. We have thus proposed a theoretical rehabilitation model (see Introduction and Fig. 1) based on the literature that yields four key treatment targets - cognitive compromise, functional compromise, associated neuropsychiatric symptoms, and modifiable risk and protective factors. Based on this model, well-designed clinical trials would, therefore, include outcome measures that assess objective cognitive performance, daily functioning, and neuropsychiatric symptom severity. It will also be important for future studies to ultimately evaluate whether interventions are associated with a reduced conversion rate to dementia or an increased conversion rate to normal cognition, as it remains to be seen whether CRTs have more potential as an intervention to maintain cognitive status (i.e., prevention of dementia) versus an intervention to reverse cognitive decline (i.e., treatment of MCI). Similar to research on other chronic or progressive diseases, it will be difficult and expensive to adequately power such analyses given a mean annual conversion rate from MCI to dementia of 10.2% (Bruscoli and Lovestone 2004) and the need to follow patients many years, even decades, to establish whether conversion occurs. Because reduced daily functioning and increased neuropsychiatric symptoms have been associated with reduced QOL in adults with MCI (Teng et al. 2012), trials should also include QOL measures, as has been previously recommended (Scholzel-Dorenbos et al. 2007). Given the potentially progressive nature of MCI, concerns have been raised that cognitive impairment might eventually impact an individual’s ability to complete or fully comprehend self-report questionnaires while lack of insight might lead to an inaccurate representation of an individual’s experience (Frank et al. 2011). Thus, clinical trials should include a combination of objective measures, collateral report measures, and self-report measures. They should evaluate both short-term as well as long-term treatment outcomes (e.g., three to six months post intervention), including an evaluation of whether individuals continue to implement or adhere to a treatment once the intervention has been discontinued (e.g., use of compensatory strategies, use of lifestyle strategies). They should also examine whether, relative to untreated control groups, interventions are associated with improvements on outcome measures or less decline on outcome measures.
Our provisional theoretical rehabilitation model (see Introduction and Fig. 1) also defines specific cognitive rehabilitation approaches that may directly or indirectly target key outcomes - restorative cognitive training, compensatory cognitive training, lifestyle interventions, and psychotherapeutic techniques. If well-designed studies are first able to definitively establish the overall efficacy of CRTs for MCI, more detailed studies can later be conducted to evaluate which approaches are associated with the largest effects on which outcomes (even though they may impact several outcomes), and which specific mechanisms operate to produce these improvements. For example, one could hypothesize that in a restorative cognitive training intervention, neuroimaging changes [e.g., increased cortical activation during functional magnetic resonance imaging (fMRI) tasks, increased white matter integrity on diffusion tensor imaging (DTI)] would mediate improvements in objective cognitive performance, and, in a compensatory cognitive training intervention, increased use of compensatory strategies would mediate improvements in daily functioning. Moreover, use of psychotherapeutic techniques in one’s daily life (e.g., relaxation exercises, sleep hygiene principles, cognitive restructuring) could be hypothesized to mediate improvements in neuropsychiatric symptom severity, and increased use of lifestyle strategies (e.g., increased physical activity or cognitively stimulating activity levels, healthier diet, reduced use of tobacco and alcohol) could be hypothesized to mediate cognitive improvements. Future studies could also evaluate the extent to which other intervention characteristics (e.g., number, length and frequency of sessions; lifestyle education versus in-class activities that increase cognitive and physical activity levels; educating about the benefits of external aids versus providing participants with these aids) and patient characteristics (e.g., demographics; premorbid IQ/cognitive reserve; baseline cognitive performance, daily functioning, and neuropsychiatric symptom severity; current and lifetime health and psychiatric status, engagement in cognitively stimulating activities, physical activity level, diet, tobacco and alcohol use) moderate outcomes.
In summary, our review of the literature on CRTs for MCI revealed the need for evidence-based treatments for MCI and the lack of a theoretical model to guide both the development and evaluation of such interventions. Data from existing studies are promising but inconclusive and indicate that additional trials are warranted if they are adequately powered and well-designed. Lastly, the development of standardized “manualized” cognitive rehabilitation interventions are recommended as they would facilitate replication studies, as well as the establishment and dissemination of evidence-based CRTs for MCI.
Acknowledgements
This material is the result of work supported with resources and the use of facilities at the Portland Veterans Affairs Medical Center, Portland, Oregon and Oregon Health & Science University, Portland Oregon. This work is in part supported by VA Merit Review awards to DS and JK, a grant from the National Institute on Drug Abuse to MH (2P50DA018165-06A1), and grants from the National Institute on Aging to JK (P30AG08017; P30AG024978). All authors read and approved the final contents of the manuscript.
Footnotes
Conflict of interest statement: The authors have declared that there are no conflicts of interest.
References
- Akhtar S, Moulin CJA, Bowie PCW. Are people with mild cognitive impairment aware of the benefits of errorless learning? Neuropsychological Rehabilitation. 2006;16(3):329–346. doi: 10.1080/09602010500176674. [DOI] [PubMed] [Google Scholar]
- Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2011;7(3):270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson-Hanley C, Arciero PJ, Brickman AM, Nimon J.P, Okuma, N., Western SC, et al. Exergaming and older adult cognition. American Journal of Prevention Medicine. 2012;42(2):109–119. doi: 10.1016/j.amepre.2011.10.016. [DOI] [PubMed] [Google Scholar]
- Anttila T, Helkala E, Viitanen M, Kareholt I, Fratiglioni L, Winblad B, et al. Alcohol drinking in middle age and subsequent risk of mild cognitive impairment and dementia in old age: A prospective population based study. British Medical Journal. 2004;329(7465):539. doi: 10.1136/bmj.38181.418958.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apostolova LG, Cummings JL. Neuropsychiatric manifestations in mild cognitive impairment: A systematic review of the literature. Dementia and Geriatric Cognitive Disorders. 2008;25(2):115–126. doi: 10.1159/000112509. [DOI] [PubMed] [Google Scholar]
- Arnaiz E, Almkvist O. Neuropsychological features of mild cognitive impairment and preclinical Alzheimer’s disease. Acta Neurologica Scandinavica. 2003;107(s19):34–41. [PubMed] [Google Scholar]
- Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Impact of cardiovascular risk factors on cognitive function: The Tromso study. European Journal of Neurology. 2011;18(5):737–743. doi: 10.1111/j.1468-1331.2010.03263.x. [DOI] [PubMed] [Google Scholar]
- Baker LD, Frank LL, Foster-Schubert K, Green PS, Wilkinson CW, McTiernan A, et al. Effects of aerobic exercise on mild cognitive impairment. Archives of Neurology. 2010;67(1):71–79. doi: 10.1001/archneurol.2009.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes DE, Alexopoulos GS, Lopez OL, Williamson JD, Yaffe K. Depressive symptoms, vascular disease, and mild cognitive impairment: Findings from the Cardiovascular Health Study. Archives of General Psychiatry. 2006;63(3):273–279. doi: 10.1001/archpsyc.63.3.273. [DOI] [PubMed] [Google Scholar]
- Barnes DE, Yaffe K, Belfor N, Jagust WJ, DeCarli C, Reed BR, et al. Computer based cognitive training for mild cognitive impairment: Results from a pilot randomized, controlled trial. Alzheimer’s Disease & Associated Disorders. 2009;23(3):205–210. doi: 10.1097/WAD.0b013e31819c6137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer-Carter JL, Green PS, Montine TJ, VanFossen B, Baker LD, Watson S, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Neurology. 2011;68(6):743–752. doi: 10.1001/archneurol.2011.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beydoun MA, Beason-Held LL, Kitner-Triolo MH, Beydoun HA, Ferrucci L, Resnick SM, et al. Statins and serum cholesterol’s associations with incident dementia and mild cognitive impairment. Journal of Epidemiology and Community Health. 2011;65(11):949–57. doi: 10.1136/jech.2009.100826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel H. Smoking, alcohol consumption, and dementia. Zeitschrift fur Wissenshcaft und Praxis. 2006;52(1):48–59. [Google Scholar]
- Bomboi S, Derambure P, Pasquier F, Monaca C. Sleep disorders in aging and dementia. Journal of Nutrition, Health, & Aging. 2010;14(3):212–217. doi: 10.1007/s12603-010-0052-7. [DOI] [PubMed] [Google Scholar]
- Boot BP, Boeve BF, Roberts RO, Ferman TJ, Geda YE, Pankratz VS, et al. Probably rapid eye movement sleep behavior disorder increases risk for mild cognitive impairment and Parkinson disease: A population-based study. Annals of Neurology. 2012;71(1):49–56. doi: 10.1002/ana.22655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruscoli M, Lovestone S. Is MCI really just early dementia? A systematic review of conversion studies. International Psychogeriatrics. 2004;16:129–140. doi: 10.1017/s1041610204000092. [DOI] [PubMed] [Google Scholar]
- Buschert VC, Friese U, Teipel SJ, Schneider P, Merensky W, Rujescu D, et al. Effects of a newly developed cognitive intervention in amnestic mild cognitive impairment and mild Alzheimer’s disease: a pilot study. Journal of Alzheimer’s Disease. 2011;25:679–694. doi: 10.3233/JAD-2011-100999. [DOI] [PubMed] [Google Scholar]
- Buchman AS, Tanne D, Boyle PA, Shah RC, Leurgans SE, Bennett DA. Kidney function is associated with the rate of cognitive decline in the elderly. Neurology. 2009;73(12):920–927. doi: 10.1212/WNL.0b013e3181b72629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceresini G, Lauretani G, Maggio M, Ceda GP, Morganti S, Usberti E, et al. Thyroid function abnormalities and cognitive impairment in elderly people: Results of the Invecchiare in Chianti study. Journal of the American Geriatrics Society. 2009;57(1):89–93. doi: 10.1111/j.1532-5415.2008.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: A meta analysis. Internal Medicine Journal. 2012;42(5):484–491. doi: 10.1111/j.1445-5994.2012.02758.x. [DOI] [PubMed] [Google Scholar]
- Cipriani G, Bianchetti A, Trabucchi M. Outcomes of a computer-based cognitive rehabilitation program on Alzheimer’s disease patients compared with those on patients affected by mild cognitive impairment. Archives of Gerontology and Geriatrics. 2006;43:327–335. doi: 10.1016/j.archger.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Clarke R, Birks J, Nexo E, Ueland PM, Schneede J, Scott J, et al. Low vitamin B-12 status and risk of cognitive decline in older adults. The American Journal of Clinical Nutrition. 2007;86(5):1384–1391. doi: 10.1093/ajcn/86.5.1384. [DOI] [PubMed] [Google Scholar]
- Doody RS, Ferris SH, Salloway S, Sun Y, Goldman R, Watkins WE, Xu Y, Murthy AK. Donepezil treatment of patients with MCI: A 48-week randomized, placebo-controlled trial. Neurology. 2009;72(18):1555–1561. doi: 10.1212/01.wnl.0000344650.95823.03. [DOI] [PubMed] [Google Scholar]
- Ellison JM, Harper DG, Berlow Y, Zeranski L. Beyond the “C” in MCI: Noncognitive symptoms in amnesic and non-amnestic mild cognitive impairment. CNS Spectrums. 2008;13(1):66–72. doi: 10.1017/s1092852900016175. [DOI] [PubMed] [Google Scholar]
- Etgen T, Bronner M, Sander D, Bickel H, Sander K, Forstl H. Somatic factors in cognitive impairment. Fortschritte der Neurologie - Psychiatrie. 2009;77(2):72–82. doi: 10.1055/s-0028-1109116. [DOI] [PubMed] [Google Scholar]
- Etgen T, Sander D, Bickel H, Forstl H. Mild cognitive impairment and dementia: The importance of modifiable risk factors. Deutches Arzteblatt International. 2011;108(44):743–750. doi: 10.3238/arztebl.2011.0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank L, Lenderking WR, Howard K, Cantillon M. Patient self-report for evaluating mild cognitive impairment and prodromal Alzheimer’s disease. Alzheimer’s Research & Therapy. 2011;3(6):35. doi: 10.1186/alzrt97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguli M, Dodge HH, Shen C, DeKosky ST. Mild cognitive impairment, amnestic type: an epidemiologic study. Neurology. 2004;63(1):115. doi: 10.1212/01.wnl.0000132523.27540.81. [DOI] [PubMed] [Google Scholar]
- Gardener S, Gu Y, Rainey-Smit SR, Keogh JB, Clifton PM, Mathieson SL. Adherence to a Mediterranean diet and Alzheimer’s disease risk in an Australian population. Translational psychiatry. 2012;2:e164. doi: 10.1038/tp.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold DA. An examination of instrumental activities of daily living assessment in older adults and mild cognitive impairment. Journal of Clinical and Experimental Neuropsychology. 2012;34(1):11–34. doi: 10.1080/13803395.2011.614598. [DOI] [PubMed] [Google Scholar]
- Goldstein FC, Levey AI, Steenland NK. High blood pressure and cognitive decline in mild cognitive impairment. Journal of the American Geriatric Society. 2013;61(1):67–73. doi: 10.1111/jgs.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomar JJ, Bobes-Bascaran MT, Conejero-Goldberg C, Davies P, Goldberg TE. Utility of combinations of biomarkers, cognitive markers, and risk factors to predict conversion from mild cognitive impairment to Alzheimer disease in patients in the Alzheimer’s disease neuroimaging initiative. Archives of General Psychiatry. 2011;68(9):961–969. doi: 10.1001/archgenpsychiatry.2011.96. [DOI] [PubMed] [Google Scholar]
- Greenaway MC, Duncan NL, Smith GE. The memory support system for mild cognitive impairment: randomized trial of a cognition rehabilitation intervention. International Journal of Geriatric Psychiatry. 2012 doi: 10.1002/gps.3838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hai S, Dong B, Liu Y, Zou Y. Occurrence and risk factors of mild cognitive impairment in the older Chinese population: A 3-year follow-up study. International Journal of Geriatric Psychiatry. 2012;27(7):703–708. doi: 10.1002/gps.2768. [DOI] [PubMed] [Google Scholar]
- Hin H, Clarke R, Sherliker P, Atoyebi W, Emmens K, Kirks J, et al. Clinical relevance of low serum vitamin B-12 concentrations in older people: The Banbury B12 Study. Age and Ageing. 2006;35(4):416–422. doi: 10.1093/ageing/afl033. [DOI] [PubMed] [Google Scholar]
- Jak AJ. The impact of physical and mental activity on cognitive aging. Current Topics in Behavioral Neurosciences. 2012;10:273–291. doi: 10.1007/7854_2011_141. [DOI] [PubMed] [Google Scholar]
- Jelic V, Kivipelto M, Winblad B. Clinical trials in mild cognitive impairment: Lessons for the future. Journal of Neurology, Neurosurgery, and Psychiatry. 2006;77:429–438. doi: 10.1136/jnnp.2005.072926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmijn S, Mehta KM, Pols HA, Hofman A, Drexhage HA, Breteler MM. Subclinical hyperthyroidism and the risk of dementia: The Rotterdam study. Clinical Endocrinology. 2000;53(6):733–737. doi: 10.1046/j.1365-2265.2000.01146.x. [DOI] [PubMed] [Google Scholar]
- Karakaya T, Fusser F, Schroder J, Pantel J. Pharmacological treatment of mild cognitive impairment as a prodromal syndrome of Alzheimer’s disease. Current Neuropharmacology. 2013;11(1):102– 108. doi: 10.2174/157015913804999487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatri M, Nickolas T, Moon YP, Paik MC, Rundek T, Elkind MS, Sacco RL, Wright CB. CKD associates with cognitive decline. Journal of the American Society of Nephrology. 2009;20(11):2427–2432. doi: 10.1681/ASN.2008101090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsella GJ, Mullaly E, Rand E, Ong B, Burton C, Price S, et al. Early intervention for mild cognitive impairment: a randomised controlled trial. Journal of Neurology, Neurosurgery, and Psychiatry. 2009;80:730–736. doi: 10.1136/jnnp.2008.148346. [DOI] [PubMed] [Google Scholar]
- Koepsell TD, Monsell SE. Reversion from mild cognitive impairment to normal or near-normal cognition: Risk factors and prognosis. Neurology. 2012;79(15):1591–1598. doi: 10.1212/WNL.0b013e31826e26b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurella M, Chertow GM, Fried LF, Cummings SR, Harris T, Simonsick E, et al. Chronic kidney disease and cognitive impairment in the elderly: the health, aging, and body composition study. Journal of the American Society of Nephrology. 2005;16(7):2127–2133. doi: 10.1681/ASN.2005010005. [DOI] [PubMed] [Google Scholar]
- Kwoz TC, Bai X, Kao HS, Li JC, Ho FK. Cognitive effects of calligraphy therapy for older people: A randomized controlled trial in Hong Kong. Clinical Interventions in Aging. 2011;6:269–273. doi: 10.2147/CIA.S25395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam LCW, Chau RCM, Wong BML, Fung AWT, Lui VWC, Tam CCW, et al. Interim follow-up of a randomized controlled trial comparing Chinese style mind body (Tai Chi) and stretching exercises on cognitive function in subjects as risk of progressive cognitive decline. International Journal of Geriatric Psychiatry. 2011;26:733–740. doi: 10.1002/gps.2602. [DOI] [PubMed] [Google Scholar]
- Larrieu S, Letenneur L, Orgogozo JM, Fabriquole C, Amieva H, Le Carret N, et al. Incidence and outcome of mild cognitive impairment in a population-based prospective cohort. Neurology. 2002;59(10):1594–1599. doi: 10.1212/01.wnl.0000034176.07159.f8. [DOI] [PubMed] [Google Scholar]
- Lee HB, Richardson AK, Black BS, Shore AD, Kasper JD, Rabins PV. Race and cognitive decline among community-dwelling elders with mild cognitive impairment: findings from the Memory and Medical Care Study. Aging and Mental Health. 2012;16(3):372–7. doi: 10.1080/13607863.2011.609533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Wang YJ, Zhang M, Xu ZQ, Gao CY, Fang CQ, et al. Vascular risk factors promote conversion from mild cognitive impairment to Alzheimer disease. Neurology. 2011a;76(17):1485–1491. doi: 10.1212/WNL.0b013e318217e7a4. [DOI] [PubMed] [Google Scholar]
- Li H, Li J, Li N, Li B, Wang P, Ting Z. Cognitive interventions for persons with mild cognitive impairment: A meta-analysis. Ageing Research Reviews. 2011b;10:285–296. doi: 10.1016/j.arr.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Lopez OL, Jagust WJ, Dulberg C, Becker JT, DeKosky ST, Fitzpatrick A, et al. Risk factors for mild cognitive impairment in the Cardiovascular Health Study Cognition Study: Part 2. Archives of Neurology. 2003;60(10):1394–1399. doi: 10.1001/archneur.60.10.1394. [DOI] [PubMed] [Google Scholar]
- Luck T, Luppa M, Briel S, Matschinger H, Konig HH, Bleich S, et al. Mild cognitive impairment: Incidence and risk factors: Results of the Leipzig Longitudinal Study of the aged. Journal of American Geriatrics Society. 2010;58(10):1903–1910. doi: 10.1111/j.1532-5415.2010.03066.x. [DOI] [PubMed] [Google Scholar]
- Luck T, Luppa M, Briel S, Riedel-Heller SG. Incidence of mild cognitive impairment: A systematic review. Dementia and Geriatric Cognitive Disorder. 2010;29(2):164–175. doi: 10.1159/000272424. [DOI] [PubMed] [Google Scholar]
- Manly JJ, Tang MX, Schupf N, Stern Y, Ronsattel JP, Mayeux R. Frequency and course of mild cognitive impairment in a multiethnic community. Annals of Neurology. 2008;63(4):494–506. doi: 10.1002/ana.21326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani E, Monastero R, Mecocci P. Mild cognitive impairment: A systematic review. Journal of Alzheimer’s Disease. 2007;12:23–35. doi: 10.3233/jad-2007-12104. [DOI] [PubMed] [Google Scholar]
- Monastero R, Mangialasche F, Camarda C, Ercolani, Camarda R. A systematic review of neuropsychiatric symptoms in mild cognitive impairment. Journal of Alzheimer’s Disease. 2009;18(1):11–30. doi: 10.3233/JAD-2009-1120. [DOI] [PubMed] [Google Scholar]
- Monastero R, Palmer K, Qiu C, Winblad B, Fratiglioni L. Heterogeneity in risk factors for cognitive impairment, no dementia: Population-based longitudinal study from the Kungsholmen Project. The American Journal of Geriatric Psychiatry. 2007;15(1):60–69. doi: 10.1097/01.JGP.0000229667.98607.34. [DOI] [PubMed] [Google Scholar]
- Nagamatsu LS, Handy TC, Hsu CL, Voss M, Liu-Ambrose T. Resistance training promotes cognitive and functional brain plasticity in seniors with probable mild cognitive impairment. Archives of Internal Medicine. 2012;172(8):666–668. doi: 10.1001/archinternmed.2012.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen RC. Mild cognitive impairment as a diagnostic entity. Journal of Internal Medicine. 2004;256:183–194. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- Petersen RC. Clinical practice: Mild cognitive impairment. The New England Journal of Medicine. 2011;364(23):2227–2234. doi: 10.1056/NEJMcp0910237. [DOI] [PubMed] [Google Scholar]
- Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, Ritchie K, Roosor M, Thal L, Winbald B. Current concepts in mild cognitive impairment. Archives of Neurology. 2001;58(12):1985–1992. doi: 10.1001/archneur.58.12.1985. [DOI] [PubMed] [Google Scholar]
- Petersen RC, Knopman DS, Boeve BF, Geda YE, Ivnik RJ, Smith GE, et al. Mild cognitive impairment: Ten years later. Archives of Neurology. 2009;66(120):1447–1455. doi: 10.1001/archneurol.2009.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: Clinical characterization and outcome. Archives of Neurology. 1999;56(3):303–308. doi: 10.1001/archneur.56.3.303. [DOI] [PubMed] [Google Scholar]
- Popp J, Arlt S. Pharmacological treatment of dementia and mild cognitive impairment due to Alzheimer’s disease. Current Opinion in Psychiatry. 2011;24(6):556–561. doi: 10.1097/YCO.0b013e32834b7b96. [DOI] [PubMed] [Google Scholar]
- Rapp S, Brenes G, Marsh AP. Memory enhancement training for older adults with mild cognitive impairment: A preliminary study. Aging & Mental Health. 2002;6(2):5–11. doi: 10.1080/13607860120101077. [DOI] [PubMed] [Google Scholar]
- Ravaglia G, Forti P, Lucicesare A, Rietti E, Pisacane N, Mariani E, et al. Prevalent depressive symptoms as a risk factor for conversion to mild cognitive impairment in an elderly Italian cohort. American Journal of Geriatric Psychiatry. 2008;16(10):834–843. doi: 10.1097/JGP.0b013e318181f9b1. [DOI] [PubMed] [Google Scholar]
- Roberts RO, Geda YE, Knopman DS, et al. The Mayo Clinic Study of Aging: design and sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. 2008;30(1):58–69. doi: 10.1159/000115751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachdev PS, Lipnicki DM, Crawford J, Reppermund S, Kochan NA, Trollor JN, et al. Risk profiles of subtypes of mild cognitive impairment: the sydney memory and ageing study. Journal of the American Geriatric Society. 2012;60(1):24–33. doi: 10.1111/j.1532-5415.2011.03774.x. [DOI] [PubMed] [Google Scholar]
- Scarmeas N, Stern Y, Mayeux R, Mannly JJ, Schupf N, Luchsinger JA. Mediterranean diet and mild cognitive impairment. Archives of Neurology. 2009;66(2):216–225. doi: 10.1001/archneurol.2008.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherder EJA, Van Paaschen J, Deijen JB, Van Der Knokke S, Orlebeke K, Burgers I, et al. Physical activity and executive functions in the elderly with mild cognitive impairment. Aging & Mental Health. 2005;9(3):272–280. doi: 10.1080/13607860500089930. [DOI] [PubMed] [Google Scholar]
- Schmand B, Eikelenboom P, van Gool WA. Value of diagnostic tests to predict conversion to Alzheimer’s disease in young and old patients with amnestic mild cognitive impairment. Journal of Alzheimer’s Disease. 2012;29(3):641–648. doi: 10.3233/JAD-2012-111703. [DOI] [PubMed] [Google Scholar]
- Scholzel-Dorenbos CJ, van der Steen MJ, Engels LK, Olde Rikkert MG. Assessment of quality of life as outcome in dementia and MCI intervention trials: A systematic review. Alzheimer’s Disease & Associated Disorders. 2007;21(2):172–178. doi: 10.1097/WAD.0b013e318047df4c. [DOI] [PubMed] [Google Scholar]
- Schonknecht P. Neurobiological and psychological aspects of mild cognitive impairment – bridging the gap. GeroPsych. 2011;24(2):63–64. [Google Scholar]
- Schreiber M, Schneider R. Cognitive plasticity in people at risk for dementia: Optimising the testing the-limits-approach. Aging & Mental Health. 2007;11(1):75–81. doi: 10.1080/13607860600735887. [DOI] [PubMed] [Google Scholar]
- Sofi F, Valecchi D, Bacci D, Abbate R, Gensini GF, Casini A, Macchi C. Physical activity and risk of cognitive decline: A meta-analysis of prospective studies. Journal of Internal Medicine. 2011;269(1):107–117. doi: 10.1111/j.1365-2796.2010.02281.x. [DOI] [PubMed] [Google Scholar]
- Steenland K, Karnes C, Seals R, Carnevale C, Hermida A, Levey A. Late-life depression as a risk factor for mild cognitive impairment or Alzheimer’s disease in 30 US Alzheimer’s disease centers. Journal of Alzheimer’s Disease. 2012;31(2):265–275. doi: 10.3233/JAD-2012-111922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng E, Tassniyom K, Lu PH. Reduced quality of life ratings in mild cognitive impairment: Analyses of subject and informant responses. American Journal of Geriatric Psychiatry. 2012;20(12):1016–25. doi: 10.1097/JGP.0b013e31826ce640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troyer AK, Murphy KJ, Anderson ND, Moscovitch M, Craik FIM. Changing everyday memory behavior in amnestic mild cognitive impairment: A randomised controlled trial. Neuropsychological Rehabilitation: An International Journal. 2008;18(1):65–88. doi: 10.1080/09602010701409684. [DOI] [PubMed] [Google Scholar]
- Tschanz JT, Welsh-Bohmer KA, Lyketsos CG, Corcoran C, Green RC, Hayden K, et al. Conversion to dementia from mild cognitive disorder: the Cache County Study. Neurology. 2006;67(2):229–234. doi: 10.1212/01.wnl.0000224748.48011.84. [DOI] [PubMed] [Google Scholar]
- Tsolaki M, Kounti F, Agogiatou C, Popsti E, Bakoglidou E, Zafeiropoulou M, et al. Effectiveness of nonpharmacological approaches in patients with mild cognitive impairment. Neurodegenerative Diseases. 2011;8:138–145. doi: 10.1159/000320575. [DOI] [PubMed] [Google Scholar]
- Unverzagt FW, Ogunniyi A, Taler V, Gao S, Lane KA, Baiyewu O, et al. Incidence and risk factors for cognitive impairment no dementia and mild cognitive impairment in African Americans. Alzheimer’s Disease and Associated Disorders. 2011;25(1):4–10. doi: 10.1097/WAD.0b013e3181f1c8b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Uffelen JGZ, Chinapaw MJM, van Mechelen W, Hopman-Rock M. Walking or vitamin B for cognition in older adults with mild cognitive impairment? A randomised controlled trial. British Journal of Sports Medicine. 2008;42:344–351. doi: 10.1136/bjsm.2007.044735. [DOI] [PubMed] [Google Scholar]
- Varela S, Ayan C, Cancela JM, Martin V. Effects of two different intensities of aerobic exercise on elderly people with mild cognitive impairment: a randomized pilot study. Clinical Rehabilitation. 2011;26(5):442–450. doi: 10.1177/0269215511425835. [DOI] [PubMed] [Google Scholar]
- Verghese J, LeValley A, Derby C, Kuslansky G, Katz M, Hall C, et al. Neurology. 2006;66(6):821–827. doi: 10.1212/01.wnl.0000202520.68987.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward A, Arrighi HM, Michels S, Cedarbaum JM. Mild cognitive impairment: Disparity of incidence and prevalence estimates. Alzheimer’s & Dementia. 2012;8(1):14–21. doi: 10.1016/j.jalz.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes De Leon CF, Barnes L.L, Schneider, J.A., Bienias JL, Evans DA, Bennett DA. Participation in cognitive stimulating activities and risk of incident Alzheimer disease. Journal of the American Medical Association. 2002;287(6):742–748. doi: 10.1001/jama.287.6.742. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Scherr PA, Schneider JA, Tang Y, Bennett DA. Relation of cognitive activity to risk of developing Alzheimer disease. Neurology. 2007;69(20):1911–20. doi: 10.1212/01.wnl.0000271087.67782.cb. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Segawa E, Boyle PA, Bennett DA. Influence of late-life cognitive activity on cognitive health. Neurology. 2012;78(15):1123–29. doi: 10.1212/WNL.0b013e31824f8c03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winblad B, Machado JC. Use of rivastigmine transdermal patch in the treatment of Alzheimer’s disease. Expert Opinion on Drug Delivery. 2008;5(2):1377–1386. doi: 10.1517/17425240802542690. [DOI] [PubMed] [Google Scholar]
- Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, et al. Mild cognitive impairment – beyond controversies, towards a consensus: Report of the International Working Group on mild cognitive impairment. Journal of Internal Medicine. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- Yaffe K, Vittinghoff E, Lindquist K, Barnes D, Covinsky KE, Neylan T, et al. Posttraumatic stress disorder and dementia: What is the origin of the association? Archives of General Psychiatry. 2010;67(6):608–613. doi: 10.1001/archgenpsychiatry.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu P, Dean RA, Hall SD, Qi Y, Sethuraman G, Willis BA, et al. Enriching amnestic mild cognitive impairment populations for clinical trials: Optimal combination of biomarkers to predict conversion to dementia. Journal of Alzheimer’s Disease. 2012;32(2):373–385. doi: 10.3233/JAD-2012-120832. [DOI] [PubMed] [Google Scholar]