Abstract
Proximal tibiofibular joint (PTFJ) instability is rare, but when encountered can be difficult to manage. Previously reported forms of treatment, including cast immobilization, soft tissue repairs and reconstructions, and fibular head resection have met with limited success. Another option is PTFJ arthrodesis—however, fusion can be difficult and ankle pain after surgery is not uncommon. In this report, we present a novel surgical technique used to treat PTFJ instability. It is a form of PTFJ arthrodesis that utilizes the osteoinductive agent recombinant human osteogenic protein (rhOP-1) to help achieve fusion, in conjunction with a fibular osteotomy to unload the PTFJ and to preserve normal rotator mobility of the distal fibula during ankle motion. We have used this technique in two patients with successful results; one of whom required revision after two previous failed attempts at PTFJ fusion and the other who had a previous diagnosis of underlying collagen disorder. Their case studies are presented in detail in this report.
Keywords: proximal tibiofibular joint, PTFJ, OP-1, osteogenic protein-1, knee
Introduction
Proximal tibiofibular joint (PTFJ) instability is rare, accounting for less than 1 % of knee injuries [1]. Closed reduction and cast immobilization, soft tissue repairs and reconstructions, and fibular head resection have all been reported as forms of treatment in the past, with variable results [2, 3]. Arthrodesis of the joint using screws and/or bone graft has also been advocated, particularly in cases of joint degeneration, intractable pain, and instability. However, earlier studies noted that arthrodesis can be limited by two problems: (1) a prolonged period to achieve fusion and (2) late development of ankle pain due to the loss of normal fibular rotation [4, 5].
In this report, we present a novel surgical technique that was developed to address both of these potential problems. We have used this protocol to treat two patients who presented with instability at the PTFJ with successful results. One patient suffered a traumatic injury to the joint during a motor vehicle accident resulting in proximal tibiofibular dislocation, while the other patient had a hypermobility syndrome that resulted in symptomatic instability of the joint. In both cases, the osteoinductive agent recombinant human osteogenic protein-1 (rhOP-1) was used to achieve successful arthrodesis of the PTFJ, which to our knowledge is the first reported instance of the use of an osteoinductive agent to augment fusion of this joint. Both patients were advised that details of their cases would be submitted for publication, and IRB approval was obtained.
Case 1
In February 2002, a 20-year-old athletic female, who regularly participated in outdoor activities including skateboarding and motocross bicycling, was injured in a motor vehicle accident in which she was struck directly on the anterior aspect of the fibular head of the right knee by the emergency parking brake on her truck. She developed persistent pain localized to the fibular head and paresthesias in the distribution of the peroneal nerve. The patient was diagnosed with a PTFJ dislocation and underwent surgery at an outside institution in December of 2002, at which time arthrodesis of the joint was attempted using a bioabsorbable screw. The patient was immobilized in a cast for 3 weeks. After removal of the cast, she reported continued pain in the lateral aspect of her right knee.
She was reevaluated in March 2003, at which time a CT scan showed minimal healing at the tibiofibular fusion site. The patient then underwent revision surgery for removal of the screw that was thought to be causing the patient's pain symptoms. At the time of surgery, it was noted that there was no evidence of fusion of the joint. The removal of hardware provided some relief of symptoms, but the pain largely persisted.
In August 2003, the patient presented to the senior author at the Hospital for Special Surgery with complaints of pain around the fibular head and crepitus in the knee. On examination of the right knee, there was slight motion at the PTFJ and mobilization of the fibular head caused pain. Knee ligament examination was normal. There was tenderness over the fibular head at the level of the tibiofibular joint. Knee alignment was normal. Peroneal muscle function and neurovascular status were normal. Radiographs and MRI demonstrated irregularity at the tibiofibular joint and normal morphology of the proximal fibula (Fig. 1). The diagnosis of post-traumatic arthrosis and instability at the PTFJ was made. At this time, it was decided that the best management strategy was arthrodesis of the tibiofibular joint.
Fig. 1.
Axial proton density (PD) MRI image of proximal tibiofibular joint of patient in Case 1, prior to initial procedure at authors' institution and after two procedures at outside institution
In November of 2003, the patient underwent repeat attempt at fusion of the right PTFJ using a partially threaded cancellous lag screw and autogenous iliac crest bone graft interposed between the fibular head and tibia (Fig. 2a, b). Additionally, a fibular osteotomy of the right fibular midshaft was performed in order to unload the PTFJ and to preserve normal rotatory mobility of the distal fibula during ankle dorsiflexion. The patient was allowed toe-touch weight-bearing in a brace in full knee extension for the first 6 weeks, followed by progression to full weight-bearing by 8 weeks. Active knee flexion was avoided for the first 8 weeks to minimize excessive stress on the proximal fibula from the hamstrings. Following this surgery, the patient developed mild extensor hallucis longus weakness, likely due to traction on the common peroneal nerve branch to the muscle. Extensor hallucis longus function returned spontaneously by 8 weeks postoperatively.
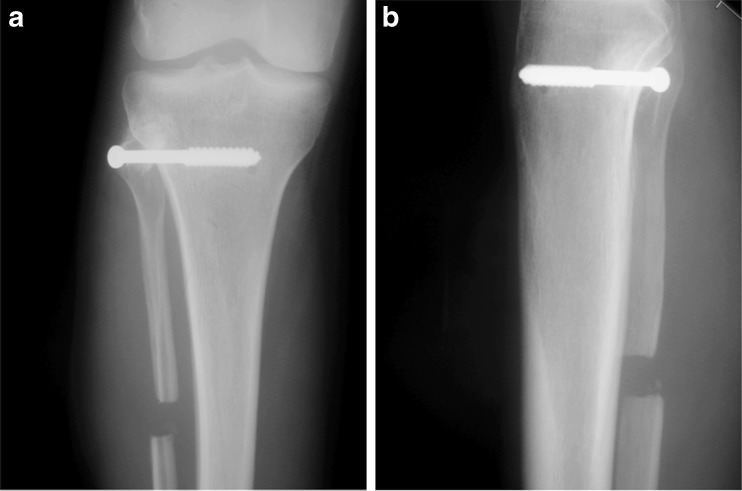
Fig. 2.
a Postoperative AP radiograph after first procedure at authors' institution. b Postoperative lateral radiograph after first procedure at authors' institution
At 5 months after surgery, a repeat CT scan showed incomplete fusion of the joint (Fig. 3). There was complete fusion between the bone graft and the fibular head; however, healing was only partially complete at the bone graft–tibia junction. Due to the fact that the patient still had pain, it was thus decided to re-explore the joint and revise the fusion using rhOP-1 (Stryker Biotech, Hopkington, MA). Exploration of the fusion during surgery demonstrated nonunion at the iliac crest graft–tibia junction. The fusion site at the PTFJ was debrided down to bleeding bone. A new autogenous iliac crest graft (approximately 1 cm × 1 cm in size) was obtained, along with cancellous bone graft from the iliac crest. The cancellous bone graft was mixed with rhOP-1 (0.875 mg/mL rhOP-1). The iliac crest graft was placed at the arthrodesis site and then the cancellous bone graft/rhOP-1 composite was applied to the fusion site. A 6.5-mm cancellous screw was again placed providing compression between the fibular head and proximal tibia. Prophylactic anterior compartment fasciotomy was performed to decrease the risk of development of compartment syndrome. The patient was placed in a postoperative hinged knee brace locked in full extension, and the patient was again allowed only toe-touch weight-bearing for the first 8 weeks, with progression to full weight-bearing after 8 weeks.
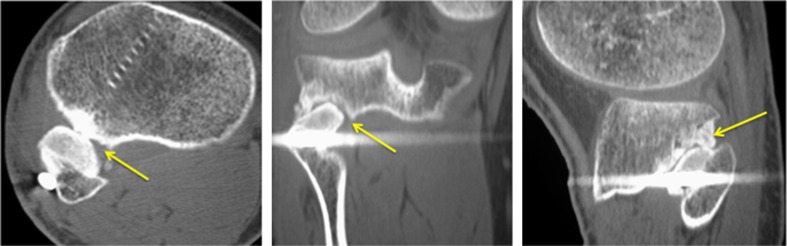
Fig. 3.
(Left to right) axial, coronal, and sagittal CT images, respectively, of the patient in Case 1, demonstrating incomplete fusion at the proximal tibiofibular joint (arrows point to the site of incomplete fusion)
A CT scan performed at 5 months postsurgery showed successful fusion of the right PTFJ (Fig. 4). The screw was removed at 14 months postoperatively as there was clear evidence on imaging of complete fusion of the joint (Fig. 5a, b, c). At her latest visit, the patient reported no pain at the tibiofibular joint or the ankle and had full range of motion at the knee and ankle joint, along with normal peroneal nerve function.
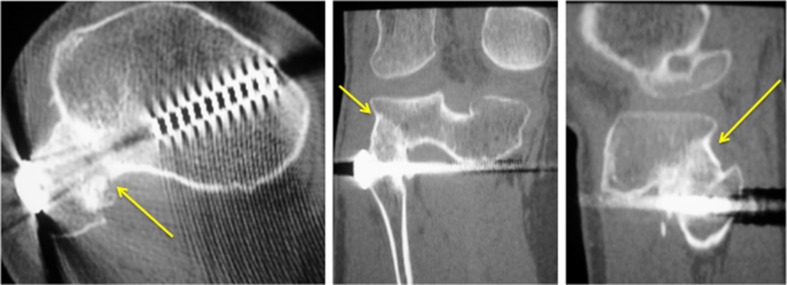
Fig. 4.
(Left to right) axial, coronal, and sagittal CT images, respectively, of the patient in Case 1 demonstrating successful bony fusion of proximal tibiofibular joint (arrows point to the fusion site)
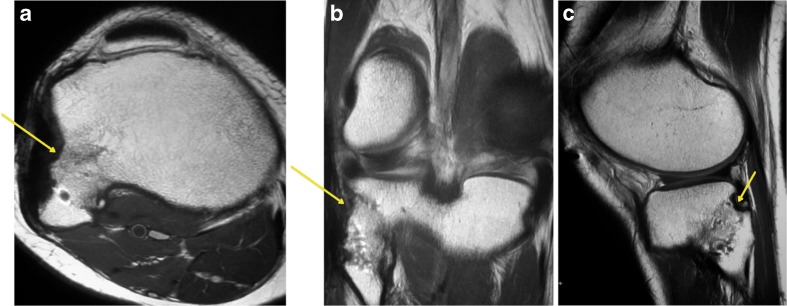
Fig. 5.
a, b, and c PD axial, coronal, and sagittal MRI images, respectively, of the patient in Case 1 after removal of hardware, demonstrating successful bony fusion of proximal tibiofibular joint (arrows point to the fusion site)
Case 2
The second case is a 34-year-old woman with a history of Ehlers–Danlos Syndrome and multiple-joint instability. In April 2005, the patient presented with complaints of instability, pain, and clicking about the right PTFJ that worsened with weight-bearing. She denied any known trauma to the tibiofibular joint; however, she did report three prior surgical procedures on the same knee including release of the iliotibial band, anterior cruciate ligament reconstruction using a patellar tendon autograft, and medial patellofemoral ligament reconstruction done elsewhere. On physical examination, there was tenderness to palpation of the fibular head, and slight anterior–posterior motion could be elicited, without any appreciable motion at the tibiofibular joint in the contralateral knee. This motion also reproduced her pain. The patient had normal motor and sensory function in the deep and superficial peroneal nerve distributions, and peroneal muscle function was normal. Comparison radiographs done supine versus standing did not demonstrate any obvious change in the position of the fibular head relative to the proximal tibia with weight-bearing. A CT scan and MRI demonstrated no evidence of subluxation of the right PTFJ. Previous corticosteroid injections into the affected PTFJ had provided temporary pain relief. The diagnosis of instability at the PTFJ was made and arthrodesis was recommended.
At the time of surgery, the PTFJ was exposed, and the common peroneal nerve was identified and protected. The joint capsule was opened, and the bone was prepared to create bleeding cancellous surfaces. A 20 mm long segment of the midshaft of the fibula was harvested to use as bone graft. The bone graft was molded to fit between the proximal tibia and the fibular head. Cancellous bone graft was then harvested through a small drill hole in the lateral femoral epicondyle. Based on our experience in the first case where fusion was delayed, we elected to use OP-1 primarily. The bone graft was mixed with demineralized bone matrix (Grafton putty, Osteotech, Inc.; Eatontown, NJ) and rhOP-1 (0.875 mg/mL rhOP-1) that had been reconstituted in saline. The fibular bone graft was placed in the PTFJ, and the mixture of cancellous bone graft, Grafton putty, and rhOP-1 was applied to the fusion site. A 7.-0 mm cannulated screw was placed across the tibiofibular articulation to provide compression. The anterior and lateral compartment fascia was released prophylactically to minimize the risk of compartment syndrome. The patient was placed in a postoperative hinged knee brace locked in full extension with only toe-touch weight-bearing for the first 6 weeks, followed by progression to full weight-bearing by 8 weeks. At 12 months postoperatively, the patient reported no pain, feelings of instability or clicking at the joint. She had full range of knee and ankle motion. There were no peroneal nerve symptoms. A CT scan demonstrated complete fusion of the tibiofibular joint. She had normal ankle function and no ankle pain.
Discussion
PTFJ instability is a relatively rare pathologic entity that has received limited attention in the literature [1, 6]. Making the correct diagnosis can oftentimes be difficult, as the clinical presentation can be mistaken for other pathologies about the knee including biceps femoris tendonitis, meniscal tears, or posterolateral rotatory instability [6]. A careful history is critical in order to determine a mechanism of injury (if present) and its chronicity as well as to identify any predisposing factors. For example, patients with ligamentous laxity syndromes (such as Ehlers–Danlos) may be at greater risk for joint instability and may even be affected bilaterally [4, 5, 7].
On physical exam, a patient with an acute injury often presents with a prominent lateral mass if there is subluxation of the joint [4]. There may be tenderness along the biceps femoris tendon, and the tendon may be tense because of the increased stretch placed upon it [4]. Pain may be also be elicited by dorsiflexion and eversion of the ankle (because of the external rotation of the fibula associated with those movements) and also by knee extension [6]. With posteromedial dislocations, there can also be a transient peroneal nerve palsy, resulting in weakness of dorsiflexion of the ankle and/or decreased sensation in the distributions of the deep or superficial peroneal nerves [4, 5, 8–10]. Chronic PTFJ instability, on the other hand, may be associated with signs and symptoms that are often much less pronounced. In these cases, the fibular head can be manipulated in an anterior–posterior direction to determine if this reproduces the patient's symptoms [11]. The Radulescu sign may also be elicited [12]. A positive Radulescu sign is demonstrated by having the patient lie in the prone position with the knee flexed to 90° and dislocating the fibular head anteriorly with passive internal rotation of the leg. The patient should also be evaluated for other associated injuries at the knee and ankle including fracture of the tibial plateau, tibial shaft, and ankle and ligamentous injuries, particularly the posterolateral corner.
Radiographic assessment of the PTFJ should include supine and weight-bearing anterior–posterior and lateral radiographs of both the injured and noninjured knees in order to detect changes in the position of the proximal fibula relative to the tibia [13]. Both CT and MRI may also aid in the diagnosis, and we have found MRI particularly useful for its high-resolution depiction of the soft tissues as well as changes in the bone such as marrow edema patterns after trauma. Stress views of the PTFJ may also be considered in order to identify abnormal laxity. These are performed by applying manual stress on the fibula in an attempt to displace the fibular head in a posteromedial direction.
Treatment of Proximal Tibiofibular Instability
Treatment of PTFJ instability will depend upon the mechanism and chronicity of the injury as well any concomitant injuries. For nontraumatic subluxation, a nonsurgical approach is initially recommended, consisting of immobilization in a cast or brace for 2 to 3 weeks [4, 5]. These patients should also be advised to avoid knee hyperflexion, as this places additional strain at the joint and increases the risk of further injury [7, 14].
Acute dislocation of the PTFJ can often by treated by simple closed reduction. Once the fibular head is reduced, it is important to evaluate all soft tissue structures of the knee, particularly the lateral collateral ligament and posterolateral corner structures as well as peroneal nerve function. This is followed by a period of protected weight-bearing using crutches with progression to full weight-bearing over 6 weeks. Consideration may be made for a period of immobilization in a brace. Ankle motion should be restricted for 4–6 weeks if there is pain with ankle dorsiflexion or eversion.
For chronic instability at the PTFJ, treatment options include fibular head resection, soft tissue stabilization, and arthrodesis. Partial or complete fibular head resection may be considered if a patient develops pain due to post-traumatic arthrosis of the PTFJ [4, 5, 15]. A partial resection removing the portion that articulates with the tibia (essentially a resection arthroplasty) would be favored over complete fibular head resection. Potential complications include chronic knee pain, lateral knee instability, and ankle pain [14, 16]. If a complete resection is performed, the soft tissue attachments to the fibular head (lateral collateral ligament, biceps tendon, and popliteofibular ligament) need to be repaired to the proximal tibia or remaining proximal fibula after fibular head resection. Fibular head resection is not recommended in athletes due to limitations in function [6].
Soft tissue reconstructions using the biceps tendon, deep fascia, and iliotibial band have also been described [3, 17–19]. However, they are technically demanding and success may be limited in cases where osteoarthritis is already present.
For cases of chronic instability with or without post-traumatic arthrosis of the tibiofibular joint, we believe arthrodesis can be a good option. However, an ideal fusion method has been elusive. Since the proximal fibula, in its normal anatomic position, has motion in both the anterior–posterior and rotatory axes, increased stress may be transferred to the ankle following PTFJ arthrodesis, potentially leading to pain at the ankle [4, 5, 12]. To reduce the risk of this complication, we chose to uncouple the proximal fibula and ankle by resecting a small segment of the fibula at the junction of the proximal and middle thirds, thereby preventing the transmission of abnormal stresses to the distal fibula and ankle [4, 12]. The fibular resection also served to unload the PTFJ during weight-bearing. Fusion itself can also be difficult to achieve, as demonstrated in the first case study. After the subject in Case 1 failed three prior attempts at fusion and based on previous reports of difficulty achieving fusion [4], we resorted to using OP-1. (We do acknowledge use of OP-1 in this manner is off label). Numerous basic and clinical studies have demonstrated the ability of bone morphogenetic protein (BMP) to induce the cellular events leading to the formation of new bone [20–25]. BMP-2, BMP-4, and BMP-7 (also known as OP-1) are the principal osteoinductive BMPs. When implanted with a collagen matrix preparation, OP-1 was shown to heal large critical-sized diaphyseal segmental defects in rabbits, dogs, and nonhuman primates [24]. In human clinical trials, similar positive results have been seen. When OP-1, placed on a type 1 collagen carrier, was used to treat tibial fracture nonunions in combination with intramedullary rods, OP-1 was shown to be as effective both clinically and radiographically, as autogenous iliac crest bone graft with no donor site complications, less blood loss, and a shorter operative time [25]. In a study of noninstrumented posterolateral fusions in patients with degenerative spondylolisthesis and spondylosis, OP-1 putty was comparable to autograft controls in terms of radiographic fusion and clinical improvement at minimum 4-year follow up [21].
Despite good results in these two cases and though no untoward events occurred, a larger sample size is needed before definitive recommendations can be made. We also recognize that the effects of OP-1 on fetal development and pregnancy are unclear and would recommend that patients avoid pregnancy near the time of exposure to OP-1 [26].
Summary
Proximal tibiofibular instability is an uncommon pathologic entity. Patients may present with only complaints of pain rather than instability. Although soft tissue reconstruction of the joint can be considered, arthrodesis may be the most reliable treatment option, especially for chronic instability, post-traumatic arthrosis, or failed prior surgery. We have presented two cases where tibiofibular arthrodesis was augmented using the osteoinductive factor osteogenic protein-1 (rhBMP-7) in combination with bone autograft. We were able to achieve a successful fusion of the PTFJ with minimal morbidity. The potential advantage of using a potent osteoinductive factor is the speed with which fusion may be achieved, leading to earlier rehabilitation and earlier return to normal function. While we acknowledge that many factors may have contributed to fusion, including improved fixation and the use of autogenous graft and/or demineralized bone matrix, we do believe that OP-1 played a significant role, especially in Case 1 where the patient failed two prior attempts at fusion without OP-1 augmentation. Not all cases may require augmentation with OP-1 or BMP-2, but we recommend strongly considering it in revision cases as well as in patients who may have comorbidities that may adversely affect bone healing (such as diabetes, collagen disorder, etc). Our technique included resection of the midfibula in order to unload the PTFJ during weight-bearing and to also prevent abnormal stresses on the ankle following fibular arthrodesis. Long-term follow-up is required to determine any consequences of such a fusion on ankle and knee function.
Disclosures
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
References
- 1.Harvey GP, Woods GW. Anterolateral dislocation of the proximal tibio-fibular joint: case report and literature review. Todays OR Nurse. 1992;14(3):23–7. [PubMed] [Google Scholar]
- 2.Ogden JA. The anatomy and function of the proximal tibio-fibular joint. Clin Orthop Relat Res. 1974;101(101):186–91. [PubMed] [Google Scholar]
- 3.Giachino AA. Recurrent dislocations of the proximal tibio-fibular joint. Report of two cases. J Bone Joint Surg Am. 1986;68(7):1104–6. [PubMed] [Google Scholar]
- 4.Ogden JA. Subluxation and dislocation of the proximal tibio-fibular joint. J Bone Joint Surg Am. 1974;56(1):145–54. [PubMed] [Google Scholar]
- 5.Ogden JA. Subluxation of the proximal tibio-fibular joint. Clin Orthop Relat Res. 1974;101(101):192–7. [PubMed] [Google Scholar]
- 6.Sekiya JK, Kuhn JE. Instability of the proximal tibio-fibular joint. J Am Acad Orthop Surg. 2003;11(2):120–8. doi: 10.5435/00124635-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Semonian RH, Denlinger PM, Duggan RJ. Proximal tibio-fibular subluxation relationship to lateral knee pain: a review of proximal tibio-fibular joint pathologies. J Orthop Sports Phys Ther. 1995;21(5):248–57. doi: 10.2519/jospt.1995.21.5.248. [DOI] [PubMed] [Google Scholar]
- 8.Parkes JC, 2nd, Zelko RR. Isolated acute dislocation of the proximal tibio-fibular joint. Case report. J Bone Joint Surg Am. 1973;55(1):177–83. [PubMed] [Google Scholar]
- 9.Veth RP, Klasen HJ, Kingma LM. Traumatic instability of the proximal tibio-fibular joint. Injury. 1981;13(2):159–64. doi: 10.1016/0020-1383(81)90052-8. [DOI] [PubMed] [Google Scholar]
- 10.Dennis JB, Rutledge BA. Bilateral recurrent dislocations of the superior tibio-fibular joint with peroneal-nerve palsy. J Bone Joint Surg Am. 1958;40-A(5):1146–8. [PubMed] [Google Scholar]
- 11.Sijbrandij S. Instability of the proximal tibio-fibular joint. Acta Orthop Scand. 1978;49(6):621–6. doi: 10.3109/17453677808993250. [DOI] [PubMed] [Google Scholar]
- 12.Baciu CC, Tudor A, Olaru I. Recurrent luxation of the superior tibio-fibular joint in the adult. Acta Orthop Scand. 1974;45(5):772–7. doi: 10.3109/17453677408989688. [DOI] [PubMed] [Google Scholar]
- 13.Resnick D, Newell JD, Guerra J, Jr, Danzig LA, Niwayama G, Goergen TG. Proximal tibio-fibular joint: anatomic–pathologic–radiographic correlation. AJR Am J Roentgenol. 1978;131(1):133–8. doi: 10.2214/ajr.131.1.133. [DOI] [PubMed] [Google Scholar]
- 14.Halbrecht JL, Jackson DW. Recurrent dislocation of the proximal tibio-fibular joint. Orthop Rev. 1991;20(11):957–60. [PubMed] [Google Scholar]
- 15.Turco VJ, Spinella AJ. Anterolateral dislocation of the head of the fibula in sports. Am J Sports Med. 1985;13(4):209–15. doi: 10.1177/036354658501300401. [DOI] [PubMed] [Google Scholar]
- 16.Draganich LF, Nicholas RW, Shuster JK, Sathy MR, Chang AF, Simon MA. The effects of resection of the proximal part of the fibula on stability of the knee and on gait. J Bone Joint Surg Am. 1991;73(4):575–83. [PubMed] [Google Scholar]
- 17.Shapiro GS, Fanton GS, Dillingham MF. Reconstruction for recurrent dislocation of the proximal tibio-fibular joint. A new technique. Orthop Rev. 1993;22(11):1229–32. [PubMed] [Google Scholar]
- 18.Horst PK, Laprade RF. Anatomic reconstruction of chronic symptomatic anterolateral proximal tibio-fibular joint instability. Knee Surg Sports Traumatol Arthrosc 2010 Feb 3. [DOI] [PubMed]
- 19.Tanner SM, Brinks KF. Reconstruction of the proximal tibio-fibular joint: a case report. Clin J Sport Med. 2007;17(1):75–7. doi: 10.1097/JSM.0b013e31802b4feb. [DOI] [PubMed] [Google Scholar]
- 20.Sampath TK, Maliakal JC, Hauschka PV, Jones WK, Sasak H, Tucker RF, et al. Recombinant human osteogenic protein-1 (hOP-1) induces new bone formation in vivo with a specific activity comparable with natural bovine osteogenic protein and stimulates osteoblast proliferation and differentiation in vitro. J Biol Chem. 1992;267(28):20352–62. [PubMed] [Google Scholar]
- 21.Vaccaro AR, Whang PG, Patel T, Phillips FM, Anderson DG, Albert TJ, et al. The safety and efficacy of OP-1 (rhBMP-7) as a replacement for iliac crest autograft for posterolateral lumbar arthrodesis: minimum 4-year follow-up of a pilot study. Spine J. 2008;8(3):457–65. doi: 10.1016/j.spinee.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Vaccaro AR, Anderson DG, Patel T, Fischgrund J, Truumees E, Herkowitz HN, et al. Comparison of OP-1 Putty (rhBMP-7) to iliac crest autograft for posterolateral lumbar arthrodesis: a minimum 2-year follow-up pilot study. Spine (Phila Pa 1976) 2005;30(24):2709–16. doi: 10.1097/01.brs.0000190812.08447.ba. [DOI] [PubMed] [Google Scholar]
- 23.Vaccaro AR, Patel T, Fischgrund J, Anderson DG, Truumees E, Herkowitz H, et al. A pilot safety and efficacy study of OP-1 putty (rhBMP-7) as an adjunct to iliac crest autograft in posterolateral lumbar fusions. Eur Spine J. 2003;12(5):495–500. doi: 10.1007/s00586-003-0561-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cook SD, Wolfe MW, Salkeld SL, Rueger DC. Effect of recombinant human osteogenic protein-1 on healing of segmental defects in non-human primates. J Bone Joint Surg Am. 1995;77(5):734–50. doi: 10.2106/00004623-199505000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Friedlaender GE, Perry CR, Cole JD, Cook SD, Cierny G, Muschler GF, et al. Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions. J Bone Joint Surg Am. 2001;83-A Suppl 1(Pt 2):S151–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Desai BM. Osteobiologics. Am J Orthop (Belle Mead NJ) 2007;36(4 Suppl):8–11. [PubMed] [Google Scholar]