Abstract
Background
Extensive research has implicated inflammation as a necessary and causative factor in the development of peri-implant osteolysis, suggesting that such an inflammatory response is the sentinel event for the process. The potential to impact the clinical course of this condition is hampered by the lack of an effective medical therapy, as well as a limited ability for early detection prior to radiographically evident osteolysis. Advances in nanotechnology have allowed for the production of engineered water-soluble nanocarriers, which exploit changes in the microvascular architecture for selective distribution to inflamed tissues. Evaluation of the uptake of the nanocarriers in sites of inflammation has elucidated a novel mechanism of cellular uptake and retention of these particles.
Purpose
The current review discusses the development of a novel, biocompatible, water-soluble nanocarrier utilizing copolymers of N-(2-hydroxypropyl)methacrylamide (HPMA), conjugated to imaging and therapeutic agents for the detection and targeted treatment of inflammatory conditions.
Methods
We performed Medline searches for the terms “periprosthetic osteolysis,” “murine osteolysis model,” “HPMA osteolysis,” and “HPMA inflammation.” These searches identified 631, 306, 1, and 6 articles, respectively. These were then manually searched for articles relevant to the development of mouse models for inflammatory osteolysis and the use of HPMA copolymer technology in mouse models of inflammation.
Results
Promising results in a small animal model of osteolysis have demonstrated the capability for detection prior to the development of bone loss, and have highlighted the utility of nanocarriers for selective drug delivery to the affected tissues.
Conclusions
Challenges to the clinical translation of HPMA nanocarriers in peri-implant osteolysis remain, and the future research directions necessary for human clinical application are reviewed.
Keywords: periprosthetic osteolysis, nanocarrier, HPMA, optical imaging
Introduction
The phenomenal success of total joint replacement surgery (TJR) for restoring mobility and joint function in patients with end-stage arthritis has led to a rapid increase in demand for this procedure. Given the lack of medical therapies to alter the natural history of osteoarthritis, the most common indication for TJR, this trend is set to continue, with upwards of 4 million total hip and knee arthroplasty operations per year projected by 2030 in the USA alone [7]. An associated area of concern is the likelihood that as TJR rates increase, so too will the incidence of peri-implant osteolysis and aseptic loosening, which represent the leading long-term cause of implant failure and need for revision [1]. These revision arthroplasties are more technically challenging, and are associated with higher complication rates, inferior clinical outcomes, and an increased rate of additional surgeries, resulting in a significant social and economic burden to society [23, 28]. Despite the growing clinical importance of periprosthetic osteolysis, it remains a difficult condition to diagnose at early stages, when intervention might prevent pathological bone loss. Moreover, there are currently no approved medical therapies for this condition [17]. In light of these observations, there is clearly an unmet medical need for effective novel approaches for the early detection and treatment of patients with prosthetic joint implants who are developing osteolysis and associated implant loosening.
There is overwhelming evidence that periprosthetic osteolysis should be classified as an inflammatory bone loss disorder [4, 11]. A robust correlation has been made linking the development of peri-implant osteolysis with the generation of particulate debris emanating from the articulating surfaces or other regions of the prosthesis [5, 25]. Furthermore, using a variety of approaches, there is strong evidence that the wear debris initiates a cellular inflammatory reaction in the periprosthetic tissues, characterized by a macrophage foreign body reaction. In patients with peri-implant osteolysis, particulate wear debris is abundant in the surrounding soft tissues and within local phagocytes [16, 26], and multiple animal models have confirmed that orthopedic wear products can initiate inflammatory signaling that leads to pathological bone loss [10, 18, 24, 27]. Technology for early detection and therapeutic targeting of the inflammatory pathways activated by these products is necessary to avert osteolysis and the resulting loss of implant fixation that necessitates revision surgery.
Numerous intracellular pathways leading to the production of classical inflammatory mediators such as TNF and IL-1 have been implicated in the response to wear particles, including the NF-κB and MAPK signaling pathways [3, 13, 15], in addition to the recently identified involvement of the Nalp3 inflammasome [2, 19]. These results indicate that the inflammatory pathways and mediators involved in osteolysis are similar to those found in other inflammatory bone loss disorders, such as rheumatoid arthritis (RA). Many of the therapeutic approaches under development for the treatment of inflammatory arthritides, therefore, may have potential applications for the treatment of early osteolysis.
Two critical barriers stand in the way of the development of therapeutics for the treatment of peri-implant osteolysis. First is the ability to identify TJR patients with inflammatory responses to wear debris at an early enough stage (i.e., prior to incipient osteolysis and prosthetic loosening), when therapeutic intervention may be able to prevent progression to clinically significant osteolysis. Second, even if the patients at risk of progression could be identified early, there are no currently available strategies to provide targeted drug delivery to the site of periprosthetic inflammation. Although there are anti-inflammatory therapeutic agents that may hold promise for the treatment of peri-implant osteolysis, many of these are associated with significant systemic and non-target organ toxicities that limit their clinical utility. Here, we review recent developments in a polymeric nanocarrier-based technology that simultaneously addresses both of these barriers and hence shows potential for significantly advancing the detection and treatment of periprosthetic osteolysis. We first describe recent conceptual breakthroughs in the use of a polymeric nanocarrier to image and treat inflammatory lesions, and then review the successful adaptation of these technologies to in vitro and small animal models of osteolysis.
Methods
We performed Medline searches for the terms “periprosthetic osteolysis,” “murine osteolysis model,” “HPMA osteolysis,” and “HPMA inflammation.” These searches identified 631, 306, 1, and 6 articles, respectively. These were then manually searched for articles relevant to the development of mouse models for inflammatory osteolysis and the use of HPMA copolymer technology in mouse models of inflammation.
Results
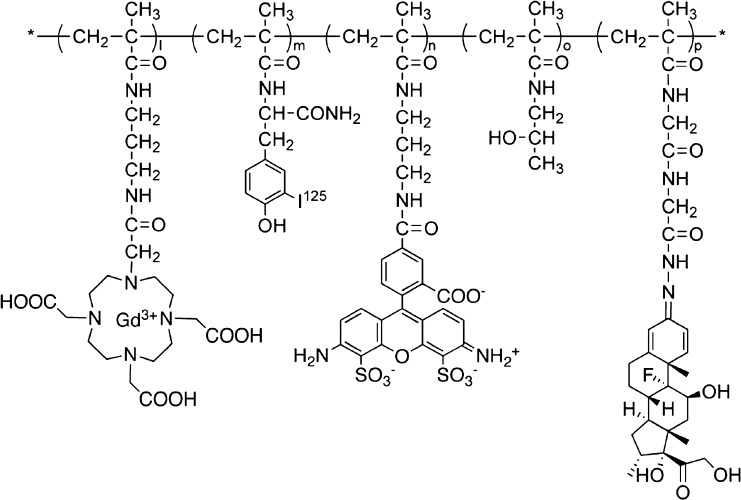
Distribution and Retention of Nanoparticles at Inflammatory Sites
Polymeric nanocarriers have a long history of utilization in the field of cancer chemotherapy. Many solid tumors possess abnormal microvascular architecture that allows for preferential extravasation of colloidal systems (including polymeric nanocarrier). This enhanced permeability is combined with impaired lymphatic outflow from the tumor, resulting in retention of the nanoparticles. This phenomenon has been characterized as the enhanced permeability and retention (EPR) effect [9], and it has been widely exploited to deliver therapeutic and imaging agents to the sites of malignancy. One popular strategy for the delivery system design has been the generation of water-soluble copolymers of N-(2-hydroxypropyl)methacrylamide (HPMA), which allow the conjugation of selected therapeutic or diagnostic agents (Fig. 1). HPMA copolymers can be engineered across a range of molecular weights and charge distributions to optimize their tissue distribution characteristics. Combined with their water solubility, low immunogenicity, and high stability, these properties have helped establish HPMA copolymers as a powerful platform for nanocarrier design and construction. Recently, an important new property of HPMA copolymers has been described. In our own studies, we have demonstrated the ability of these nanocarriers to specifically extravasate not only in tumor vasculature but also at sites of inflammation [12, 14, 21, 22]. The mechanism responsible for this phenomenon lies in the increased vascular permeability that accompanies local tissue responses to inflammatory stimuli, and we speculated that this pathophysiological mechanism might be exploited to allow delivery of HPMA copolymers to a wide range of inflammatory lesions.
Fig. 1.
General structure of HPMA copolymer conjugates showing a selection of conjugated imaging and therapeutic agents discussed in the text. HPMA-dexamethasone (P-Dex): l, m and n = 0; HPMA-Alexa-488: l, m and p = 0; HPMA-Gd3+: m, n and p = 0.
The first detailed exploration of the novel concept of targeting inflammatory disorders with HPMA copolymer conjugates utilized a well-established rat model of adjuvant-induced arthritis (AA) [12]. These studies established a number of important benchmark observations. Consistent with the documented increased vascular leakage associated with local tissue inflammation, HPMA copolymers labeled with the MRI contrast agent DOTA-Gd3+ administered via tail vein injection rapidly and specifically became associated with the inflamed synovium of the joints. Moreover, using HPMA coupled to AlexaFluor-488 under confocal microscopy, the joint tissue of arthritic rats demonstrated selectivity of the extravasation to the inflamed tissues, with rapid sequestration within synoviocytes. The cellular uptake of extravasated copolymer appeared to be fairly nonspecific with respect to cell type, with type A synoviocytes (macrophage-like) and type B cells (fibroblast-like) both showing substantial uptake. These findings have been corroborated and extended by flow cytometric analysis of cells isolated from the inflamed synovial tissues, reinforcing the concept that rapid uptake by multiple types of cells at sites of inflammation provides a mechanism for copolymer localization and retention. Importantly, this cell-based mechanism of tissue retention of extravasated copolymer within inflammatory tissues contrasts significantly with the proposed EPR mechanism for copolymer retention in tumors, which is largely attributable to defective lymphatic drainage. We have termed this novel passive targeting mechanism as “ELVIS,” which represents the polymeric nanocarriers’ Extravasation through Leaky Vasculature and the subsequent Inflammatory cell-mediated Sequestration [21]. Thus, in addition to the effects of altered lymphatic drainage at sites of inflammation, the cellular uptake allows for retention of the copolymer.
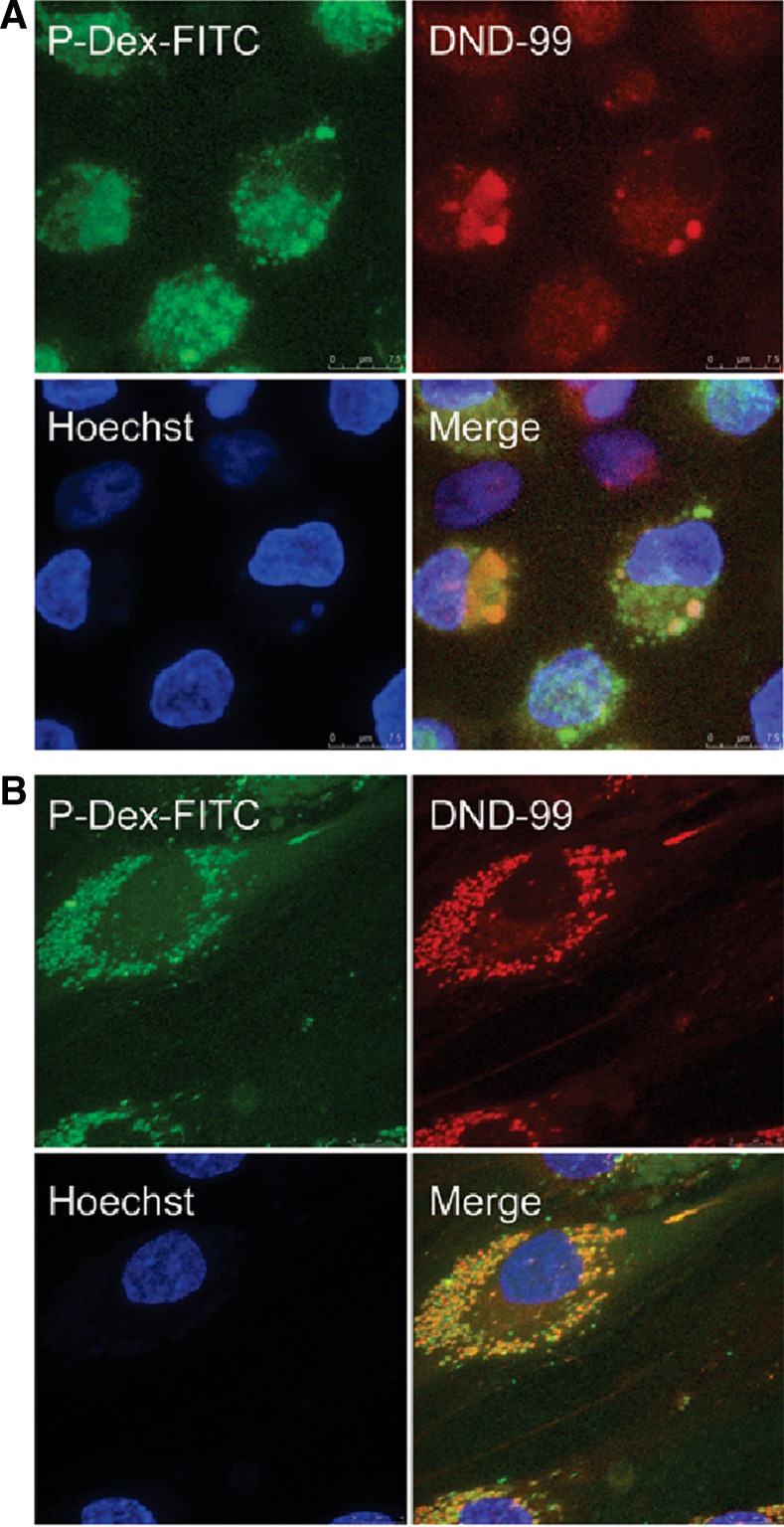
Inflammatory cell uptake of the extravasated copolymer not only provides a mechanism for retention of potential therapeutic agents at the sites of tissue inflammation but also provides a strategic approach to selectively delivery the anti-inflammatory prodrugs to the target cell populations responsible for the inflammation and tissue destruction. Understanding the mechanisms of uptake, intracellular partitioning, and copolymer processing is therefore crucial to the development of HPMA-based nanocarriers as anti-inflammatory therapeutics. Through a combination of immunofluorescence and flow cytometry approaches, we have shown that fluorescent probe-labeled copolymers are taken up both in vivo and in vitro by several types of inflammatory cells, including myeloid cells and fibroblasts, key players in the production and signaling of cytokines and other molecular mediators of inflammatory diseases. Confocal fluorescence microscopy has shown that HPMA copolymers are rapidly sequestered into the lysosomal/endosomal compartments of target cells, consistent with an endocytic mechanism of uptake (Fig. 2). This places the endocytosed copolymer in a highly acidic subcellular location, an observation that underpins a critical and novel feature of anti-inflammatory prodrug design, the engineering of a low-pH cleavable linker between the HPMA polymer and the therapeutic agent. Through the introduction of such a linker, release of the prodrug in the cell cytosol can be delayed until the prodrug has accumulated within the target inflammatory cells. Since the linker is cleaved gradually at low pH (with rates as low as 1% of the total every 24 h), this provides for a prodrug depot within target cells that can be cleaved and activated over a sustained period of time.
Fig. 2.
Confocal images show the internalization and lysosomal localization of FITC-labeled acid-labile P-Dex by a cultured human monocytes and b fibroblasts. Adapted from Quan et al. Development of a macromolecular prodrug for the treatment of inflammatory arthritis: mechanisms involved in arthrotropism and sustained therapeutic efficacy. Arthritis Research & Therapy 2010, 12:R170.
In proof-of-concept studies, we have confirmed that HPMA copolymer-conjugated anti-inflammatory drugs (dexamethasone and the IKK inhibitor BMS 345541) are capable of suppressing cytokine production of myeloid cells in response to multiple inflammatory mediators, including LPS and particles of orthopedic wear responsible for periprosthetic osteolysis, even several days after dosing. These findings reinforce the concept that HPMA copolymer conjugates of therapeutic agents provide a sustained duration of efficacy not seen with free drugs. This represents a considerable advantage for the targeting of chronic inflammatory diseases. Validation of this conclusion has been provided by our demonstration of the therapeutic efficacy of an HPMA copolymer-dexamethasone conjugate (P-Dex) in the AA rat model, wherein a single dose of P-Dex provided protection from arthritis in this model over 4 weeks. In contrast, repeated dosing (×4) of equivalent free dexamethasone was only effective transiently, with disease scores rapidly rising after termination of the treatments [12]. Given the chronic nature of joint inflammation in this model, the sustained efficacy of a single dose of the copolymer prodrug form of this drug is particularly desirable.
Subsequent to our initial studies in the rat AA model, numerous other models of inflammatory disease have been investigated and shown to be equally well suited to polymeric nanocarrier-based approaches for disease imaging and treatment. These include the mouse model of collagen-induced arthritis and in the kidneys in NZB/W F1 mice, a prototypical mouse model of systemic lupus erythematosus nephritis. In each of these models, we successfully demonstrated the advantages of selective and sustained targeting of the sites of inflammation with the prodrug while sparing the systemic off-site toxicities of the free drug. Collectively, these studies strongly support the diagnostic sensitivity, therapeutic efficacy, and safety of the HPMA copolymer-based approaches for the treatment of inflammatory disorders.
Nanocarrier-Mediated Imaging and Treatment of Osteolysis
Aseptic loosening and peri-implant osteolysis secondary to TJR represent an inflammatory bone loss disorder with unique challenges for detection and treatment [20]. Although it is well established that the most important initiating event in this disorder is the inflammatory activation of myeloid cells following phagocytosis of particulates of orthopedic wear debris, symptomatic bone loss can occur many years or decades after the start of wear generation. At this point after development of extensive osteolysis, targeting the underlying inflammatory disease is of limited therapeutic benefit. Histopathological analysis of periprosthetic tissues at times of revision surgery has confirmed the presence of an ongoing macrophage-dominated inflammatory reaction, and gene expression analysis of these tissues has identified specific inflammatory mediators associated with this reaction [6, 11]. What is lacking is an effective means of detecting inflammatory disease at an early enough stage of development such that treatment with anti-inflammatory drugs can prevent incipient osteolysis.
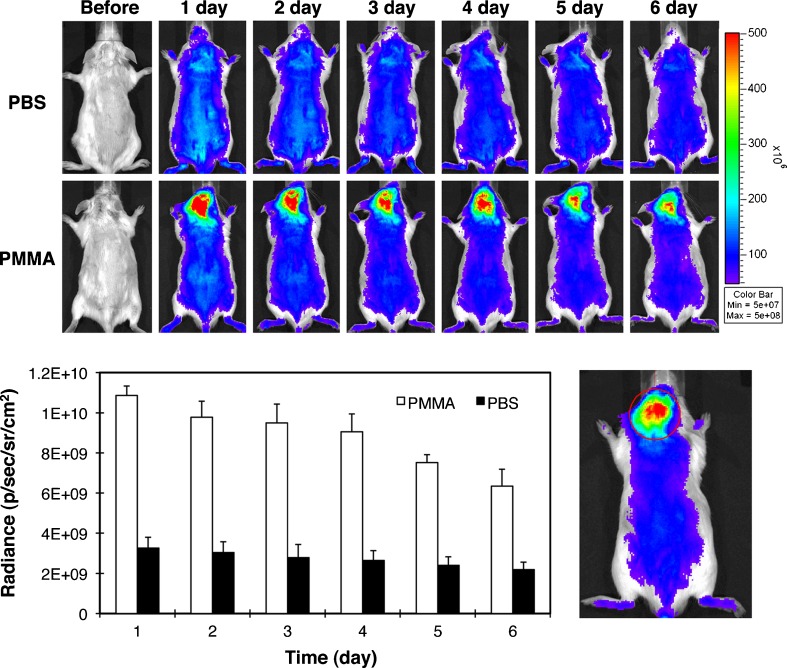
To explore the potential use of polymeric nanocarrier technologies in resolving these critical issues in the diagnosis and treatment of osteolysis, we have adapted a widely used mouse model for orthopedic wear-induced osteolysis [10, 18]. In this model, wear particles [generally consisting of ultra high molecular weight polyethylene (UHMWPE) and polymethylmethacrylate (PMMA) bone cement, common components of total joint replacements] are introduced over the surface of the mouse calvarium, from which the periosteum has been manually removed. The implanted particles initiate a granulomatous inflammatory reaction analogous to that observed in the human disease, leading to profound calvarial osteolysis within 7 days, which can be clearly delineated by microCT approaches. To assess potential copolymer localization and retention at sites of particle-induced inflammatory osteolysis, animals were injected with HPMA copolymer conjugated with either IRDye 800CW or Alexa Fluor-488 via tail vein injection 1 day following calvarial wear particle introduction. Strikingly, these copolymers rapidly and specifically accumulated within the same peri-calvarial tissues where the orthopedic wear particles had previously been applied (Fig. 3). However, in sham-operated animals without UHMWPE or PMMA particles, copolymer became distributed nonspecifically throughout the body. These encouraging findings suggest that HPMA copolymer-based nanocarriers are able to target to sites of orthopedic wear particle-induced inflammation. Immunohistochemical and flow cytometric approaches confirmed that, in keeping with the previous findings in other inflammatory disease models, polymeric nanocarrier retention at these sites was associated with ELVIS-mediated mechanisms of cellular uptake and partitioning. Perhaps the most significant aspect of these findings is that the injected nanocarriers were capable of specifically localizing to the sites of particle-driven inflammation at such an early phase of disease, days prior to the appearance of detectable osteolysis. This provides considerable encouragement that this type of approach has the potential to significantly augment current imaging modalities for early detection of inflammatory osteolysis.
Fig. 3.
Live optical imaging showing selective localization of copolymer to the site of early wear particle-induced inflammation. Upper panels: HPMA-IRDye was given via tail vein injection 1 day after PBS (a) or PMMA (b) implantation over the calvarium. The mice were imaged prior to and each day after the administration of the optical imaging agent for 6 days (n = 3). Compared to the PBS control, PMMA particle-implanted animals demonstrated more intense and longer-lasting HPMA-IRDye signals in the calvarial region where the PMMA particles were implanted. Lower panels: The HPMA-IRDye signal intensity was measured from a consistent region of interest (red circle) in the calvaria site for all the mice. The signal intensity differences in the two groups were statistically significant (p < 0.05). Reprinted with permission from Ren K, Purdue PE, Burton L, Quan LD, Fehringer EV, Thiele GM et al. Early detection and treatment of wear particle‐induced inflammation and bone loss in a mouse calvarial osteolysis model using HPMA copolymer conjugates. Mol Pharm. 2011;8(4):1043–51. doi:10.1021/mp2000555. Copyright 2011 American Chemical Society.
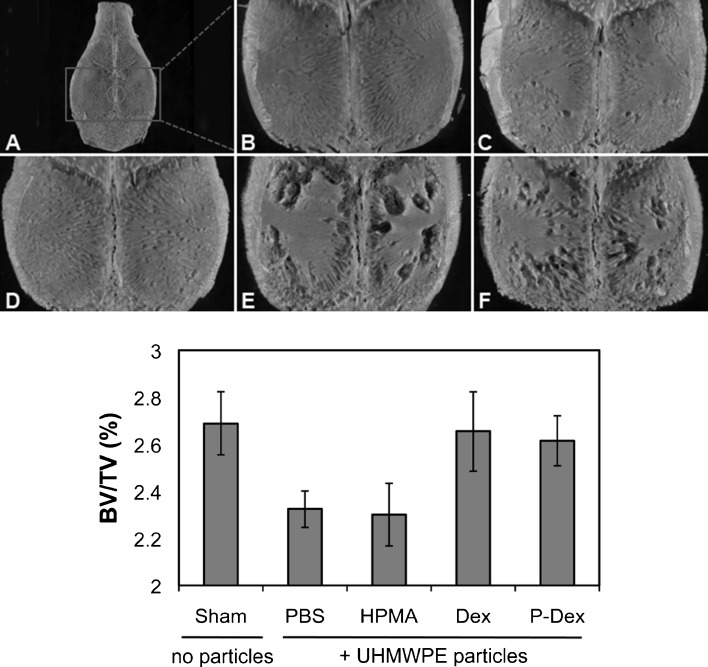
To establish whether the HPMA copolymer nanocarrier system could be applied to therapeutically target sites of wear particle-induced inflammation, we initially compared the abilities of free dexamethasone (Dex) and HPMA copolymer-conjugated Dex (P-Dex) to suppress inflammatory cytokine production in human monocytes challenged with PMMA wear particles in vitro. This revealed that conjugation of Dex to the HPMA copolymer did not interfere with its ability to dampen inflammatory signaling in response to particle phagocytosis. These results confirm that particle-activated cells are able to endocytose and activate P-Dex to generate an intracellular supply of active free drug. Importantly, these findings were validated in vivo since a single P-Dex tail vein injection 1 day after orthopedic UHMWPE particle implantation over the calvarium completely prevented particle-induced osteolysis (Fig. 4). Taken together, these findings provide strong in vivo and in vitro support for the concept that HPMA copolymer conjugates may hold great promise for early detection and treatment of peri-implant osteolysis.
Fig. 4.
Micro-CT analysis showing protection against UHMWPE-induced osteolysis by P-Dex copolymer. Upper panels: Mice calvaria were implanted with PBS (a, b) or UHMWPE particles (c–f). One day later, UHMWPE-treated mice were further treated via tail vein injection with four daily doses of free Dex (c) or a single injection of P-Dex (d), plain HPMA (e), or PBS (f). The negative controls (e, f) show no protection. P-Dex provides equivalent protection against osteolysis as multiple doses of free Dex. Lower panels: quantitation of BV/TV of the groups represented in the left panels. Reprinted with permission from Ren K, Purdue PE, Burton L, Quan LD, Fehringer EV, Thiele GM et al. Early detection and treatment of wear particle‐induced inflammation and bone loss in a mouse calvarial osteolysis model using HPMA copolymer conjugates. Mol Pharm. 2011;8(4):1043‐51. doi:10.1021/mp2000555. Copyright 2011 American Chemical Society.
As in other inflammatory disease models, calvarial inflammatory osteolysis induced by orthopedic wear particles could be targeted by HPMA copolymer-conjugated imaging and therapeutic agents with a high degree of sensitivity, selectivity, and durability. Our findings indicate that targeted HPMA copolymer-dexamethasone conjugates suppressed inflammatory responses to particles through an ELVIS-mediated mechanism and prevented progression of the inflammation to a stage of clinical osteolysis. Given the potential for significant “off-target” side effects and toxicity associated with systemic administration of dexamethasone, the capacity of the conjugate to selectivity target the site of inflammation without affects on non-target organs indicates the utility of this system for the delivery of therapeutic agents in inflammatory disorders.
Discussion
Remaining Challenges and Future Directions
As detailed above, the HPMA copolymer nanocarrier technology represents an effective and rational approach for imaging and treating inflammatory disorders. This represents a significant step forward in the therapeutic approach to these widespread and increasingly common disorders. By establishing a new paradigm for the mechanism of tissue retention of nanoparticles in inflammatory diseases related to the “ELVIS” principle, the groundwork has been prepared for translating this technology towards clinical utility. In addition to the strong preclinical data, the known biocompatibility of HPMA copolymer makes this translation a realistic goal. However, several important challenges remain:
Optimization of nanocarrier design strategies. The finding that inflammatory tissue sequestration of copolymers occurs through cellular uptake dictates that the effectiveness of these nanomedicines will be determined in large part by the kinetics and cellular profiles of the inflammatory response, variables that will differ significantly between different conditions. Thus, design parameters such as nanocarrier size, charge, and prodrug activation mechanism will have to be carefully optimized to ensure maximal effectiveness for each application.
Development of suitable imaging agents for detection of early disease in humans. To have clinical utility, the optical imaging tools developed for nanoparticle imaging in rodent models will have to be adapted to the imaging protocols currently available for clinical assessment in human subjects. A logical candidate approach in this regard would be HPMA conjugated to a SPECT, PET, or MRI contrast agent. These instruments represent the most useful imaging systems for detection of osteolysis. The sensitivity and specificity of these imaging systems could be significantly enhanced by use of nanocarriers that preferentially localize to sites of early inflammatory disease. This would be of particular value in patients at high risk of implant failure who have been recommended for routine serial imaging, such as patients with contralateral early osteolysis and certain patients with metal-on-metal bearing surfaces.
Selection of the drug candidate for polymeric nanocarrier conjugation. The drug candidate must be selected according to its intended application. For each inflammatory disease, there will be optimal drug candidates that are uniquely suited to the underlying disease pathology, and this principle must rationally guide the design strategy of the prodrug. Molecular and genetic screening have defined the tissue distribution and specificity of the individual kinases that comprise the major signal pathway families associated with inflammatory and autoimmune processes, including the MAP, JAK, SYK, and NF-κB pathways. High-throughput screening and drug design methodologies have identified small molecule inhibitors to target specific protein kinases within these pathways, and studies in animal models of inflammation and in early human trials have validated their clinical efficacy [8]. However, the requirements for high dosages, frequent administration, and undesirable pharmacokinetic/biodynamic biodistribution and toxicity profiles associated with adverse effects on “off-target” tissues remain a major barrier to the advancement of these therapeutic agents into actual human clinical application. For example, p38, one of the terminal kinases that regulate the cellular response in the MAP signaling pathway, was proposed as a therapeutic target in RA therapy. However, the first generation of p38 inhibitors failed in clinical trials due to liver, brain, and skin toxicities [8]. These limitations would make the polymeric nanocarrier conjugation of kinase inhibitors a very promising direction to pursue since the HPMA copolymers allow for a more selective and durable response with improvement in “off-target” safety profiles. However, successful optimization of this approach will require continued efforts towards identification of therapeutic targets and strategies.
Disclosures
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1):128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 2.Caicedo MS, Desai R, McAllister K, Reddy A, Jacobs JJ, Hallab NJ. Soluble and particulate Co-Cr-Mo alloy implant metals activate the inflammasome danger signaling pathway in human macrophages: a novel mechanism for implant debris reactivity. J Orthop Res. 2009;27(7):847–854. doi: 10.1002/jor.20826. [DOI] [PubMed] [Google Scholar]
- 3.Clohisy JC, Hirayama T, Frazier E, Han SK, Abu-Amer Y. NF-kB signaling blockade abolishes implant particle-induced osteoclastogenesis. J Orthop Res. 2004;22(1):13–20. doi: 10.1016/S0736-0266(03)00156-6. [DOI] [PubMed] [Google Scholar]
- 4.Cobelli N, Scharf B, Crisi GM, Hardin J, Santambrogio L. Mediators of the inflammatory response to joint replacement devices. Nat Rev Rheumatol. 2011;7(10):600–608. doi: 10.1038/nrrheum.2011.128. [DOI] [PubMed] [Google Scholar]
- 5.Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17(5):649–661. doi: 10.1054/arth.2002.33664. [DOI] [PubMed] [Google Scholar]
- 6.Koulouvaris P LK, Ivashkiv LB, Bostrom MP, Nestor BJ, Sculco TP, Purdue PE. Expression profiling reveals alternative macrophage activation and impaired osteogenesis in periprosthetic osteolysis. J Orthop Res. 2008;26(1):106–16. [DOI] [PubMed]
- 7.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lindstrom TM, Robinson WH. A multitude of kinases—which are the best targets in treating rheumatoid arthritis? Rheum Dis Clin North Am. 2010;36(2):367–383. doi: 10.1016/j.rdc.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsumura Y, Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986;46(12 Pt 1):6387–6392. [PubMed] [Google Scholar]
- 10.Merkel KD, Erdmann JM, McHugh KP, Abu-Amer Y, Ross FP, Teitelbaum SL. Tumor necrosis factor-alpha mediates orthopedic implant osteolysis. Am J Pathol. 1999;154(1):203–210. doi: 10.1016/S0002-9440(10)65266-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Purdue PE, Koulouvaris P, Potter HG, Nestor BJ, Sculco TP. The cellular and molecular biology of periprosthetic osteolysis. Clin Orthop Relat Res. 2007;454:251–261. doi: 10.1097/01.blo.0000238813.95035.1b. [DOI] [PubMed] [Google Scholar]
- 12.Quan LD, Purdue PE, Liu XM, Boska MD, Lele SM, Thiele GM, et al. Development of a macromolecular prodrug for the treatment of inflammatory arthritis: mechanisms involved in arthrotropism and sustained therapeutic efficacy. Arthritis Res Ther. 2010;12(5):R170. doi: 10.1186/ar3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rakshit DS, Ly K, Sengupta TK, Nestor BJ, Sculco TP, Ivashkiv LB et al. Wear Debris Inhibition of Anti-Osteoclastogenic Signaling by Interleukin-6 and Interferon-{gamma} Mechanistic Insights and Implications for Periprosthetic Osteolysis. J Bone Joint Surg Am. 2006;88(4):788–99. [DOI] [PubMed]
- 14.Ren K, Purdue PE, Burton L, Quan LD, Fehringer EV, Thiele GM, et al. Early detection and treatment of wear particle-induced inflammation and bone loss in a mouse calvarial osteolysis model using HPMA copolymer conjugates. Mol Pharm. 2011;8(4):1043–1051. doi: 10.1021/mp2000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ren W, Li XH, Chen BD, Wooley PH. Erythromycin inhibits wear debris-induced osteoclastogenesis by modulation of murine macrophage NF-kappaB activity. J Orthop Res. 2004;22(1):21–29. doi: 10.1016/S0736-0266(03)00130-X. [DOI] [PubMed] [Google Scholar]
- 16.Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am. 1992;74(6):849–863. [PubMed] [Google Scholar]
- 17.Schwarz EM. What potential biologic treatments are available for osteolysis? J Am Acad Orthop Surg. 2008;16(Suppl 1):S72–S75. doi: 10.5435/00124635-200800001-00015. [DOI] [PubMed] [Google Scholar]
- 18.Schwarz EM, Benz EB, Lu AP, Goater JJ, Mollano AV, Rosier RN, et al. Quantitative small-animal surrogate to evaluate drug efficacy in preventing wear debris-induced osteolysis. J Orthop Res. 2000;18(6):849–855. doi: 10.1002/jor.1100180602. [DOI] [PubMed] [Google Scholar]
- 19.St Pierre CA, Chan M, Iwakura Y, Ayers DC, Kurt-Jones EA, Finberg RW. Periprosthetic osteolysis: characterizing the innate immune response to titanium wear-particles. J Orthop Res. 2010;28(11):1418–1424. doi: 10.1002/jor.21149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walde TA, Weiland DE, Leung SB, Kitamura N, Sychterz CJ, Engh CA, Jr, et al. Comparison of CT, MRI, and radiographs in assessing pelvic osteolysis: a cadaveric study. Clin Orthop Relat Res. 2005;437:138–144. doi: 10.1097/01.blo.0000164028.14504.46. [DOI] [PubMed] [Google Scholar]
- 21.Wang D, Goldring SR. The bone, the joints and the Balm of Gilead. Mol Pharm. 2011;8(4):991–993. doi: 10.1021/mp200328t. [DOI] [PubMed] [Google Scholar]
- 22.Wang D, Miller SC, Liu XM, Anderson B, Wang XS, Goldring SR. Novel dexamethasone-HPMA copolymer conjugate and its potential application in treatment of rheumatoid arthritis. Arthritis Res Ther. 2007;9(1):R2. doi: 10.1186/ar2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ward JR, West PW, Ariaans MP, Parker LC, Francis SE, Crossman DC, et al. Temporal interleukin-1beta secretion from primary human peripheral blood monocytes by P2X7-independent and P2X7-dependent mechanisms. J Biol Chem. 2010;285(30):23147–23158. doi: 10.1074/jbc.M109.072793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warme BA, Epstein NJ, Trindade MC, Miyanishi K, Ma T, Saket RR, et al. Proinflammatory mediator expression in a novel murine model of titanium-particle-induced intramedullary inflammation. J Biomed Mater Res B Appl Biomater. 2004;71(2):360–366. doi: 10.1002/jbm.b.30120. [DOI] [PubMed] [Google Scholar]
- 25.Wilkinson JM, Hamer AJ, Stockley I, Eastell R. Polyethylene wear rate and osteolysis: critical threshold versus continuous dose-response relationship. J Orthop Res. 2005;23(3):520–5. [DOI] [PubMed]
- 26.Willert HG. Reactions of the articular capsule to wear products of artificial joint prostheses. J Biomed Mater Res. 1977;11(2):157–164. doi: 10.1002/jbm.820110202. [DOI] [PubMed] [Google Scholar]
- 27.Wooley PH, Morren R, Andary J, Sud S, Yang SY, Mayton L, et al. Inflammatory responses to orthopaedic biomaterials in the murine air pouch. Biomaterials. 2002;23(2):517–526. doi: 10.1016/S0142-9612(01)00134-X. [DOI] [PubMed] [Google Scholar]
- 28.www.orthoinfo.com. Official Website of the American Academy of Orthopaedic Surgeons: www.orthoinfo.org. Accessed March 2012.