Abstract
Background
Men who have sex with men (MSM) account for more than half of new HIV infections each year, and young Black MSM experience the highest incidence rates. Black MSM have not been found to engage in more HIV risk behaviors, and it has been proposed that sexual network factors (racially homophilous networks) and partnership characteristics (influence of older partners and familiarity with partners) may help account for this disparity.
Methods
143 ethnically diverse MSM were enrolled in an online prospective diary study of sexual behavior. Participants completed weekly diaries of sexual encounters and associated situational factors for 12 weeks. All analyses were conducted with Hierarchical Linear Modeling.
Results
Black MSM reported significantly less unprotected sex than other groups and were the most racially homophilous group in terms of sexual partnerships. Having older sexual partners and familiarity with partners were both associated with increased odds of sexual risk in Black MSM only. A three-way interaction between participant age, participant race, and sexual partner age revealed a strong association between having older partners and odds of sexual risk for young Black MSM, as well as a strong association between having younger partners and sexual risk for older non-Black MSM.
Conclusions
Findings expand upon previous theory and cross-sectional research. Results indicate that some of the driving forces behind the disproportionate HIV incidence in Black MSM may be the greater likelihood of racially homophilous sexual networks combined with the stronger influence of sexual partner age and familiarity with partners on condom use.
Keywords: HIV/AIDS, men who have sex with men, race, sexual risk
Black men who have sex with men (MSM) are disproportionately impacted by the HIV/AIDS epidemic in the United States1,2, and young Black MSM experience the highest HIV incidence of any group. Paradoxically, Black MSM have not been found to engage in more HIV risk behaviors3–5. Some have hypothesized that disparities in HIV incidence cannot be explained by individual risk behaviors alone, and racial differences in the characteristics of sexual networks (size and racial composition of networks) and partnerships (sexual partner age differences and types of relationships with partners) may underlie the racial disparity in HIV incidence6.
The sexual networks of Black MSM are thought to be much smaller than those of White MSM. There are significantly fewer Black than White MSM in the United States7, and evidence suggests that Black MSM are more likely to have same-race partnerships (sexual homophily) than other groups5,8,9. Furthermore, research has linked having older sexual partners to HIV risk among young Black MSM10,11, and familiarity with partners is associated with unprotected sex with casual partners in non-racially selected MSM samples12,13. Unprotected sex within these types of partnerships would provide a gateway through which HIV could enter a sexual network, after which it would more efficiently spread through the smaller and more racially homophilous networks of Black MSM. The higher prevalence of HIV in Black MSM, in concert with more in-group sexual partnering, would drive an increased incidence of new infections.
Using data from an ethnically diverse sample of MSM enrolled in a prospective sexual diary study, we tested the following hypotheses: 1) Black MSM are no more likely than other racial groups to report sexual risk; 2) Black MSM are more likely to have same-race partnerships than other racial groups (sexual homophily); and 3) sexual partner age and familiarity with partners are associated with sexual risk in MSM. Finally, we explored the moderating effects of age and race on the association between sexual partnership characteristics and sexual risk.
Methods
Participants
One hundred forty-three MSM were enrolled in a prospective diary study of sexual behavior. See Table 1 for full demographic description of the sample.
Table 1.
Participant Demographics: Men Who Have Sex with Men Recruited Online, 2011
| Variable | % of Full Sample N (%) | % of Analytic Sample N (%) |
|---|---|---|
| Age | ||
| 16–24 | 59 (41.3) | 57 (41.6) |
| 25–30 | 36 (25.2) | 33 (24.1) |
| 31–40 | 48 (33.5) | 47 (34.3) |
| Mean (SD) | 27.53 (7.33) | 27.54 (7.40) |
| Race/Ethnicity | ||
| White/Caucasian | 53 (37.1) | 50 (36.5) |
| Black/African American | 32 (22.4) | 31 (22.6) |
| Hispanic/Latino | 39 (27.3) | 37 (27.0) |
| Asian/Pacific Islander | 6 (4.2) | 6 (4.4) |
| Other/Multi-Racial | 13 (9.1) | 13 (9.5) |
| Sexual Orientation | ||
| Gay | 111 (77.6) | 106 (77.4) |
| Bisexual | 29 (20.3) | 28 (20.4) |
| Heterosexual (same-sex attracted) | 3 (2.1) | 3 (2.2) |
| Geographic Location | ||
| Northeast | 37 (25.9) | 36 (26.3) |
| Midwest | 40 (28.0) | 37 (27.0) |
| West Coast | 42 (29.4) | 40 (29.2) |
| South/Southeast | 24 (16.8) | 24 (17.5) |
Procedures & Design
Participants were recruited online via advertisements posted on Craigslist and Facebook. Inclusion criteria were: 1) oral/anal sex with a man during the previous six months, 2) between the ages of 16 and 40, 3) not in a sexually-monogamous relationship, and 4) HIV− or unknown serostatus. Inclusion criteria were utilized to increase the likelihood that participants would have multiple sexual encounters and to facilitate comparisons between age and racial groups that are currently at highest risk for HIV acquisition.
After completing baseline measures of between-subjects variables, participants completed online weekly diaries for 12 weeks. Each diary detailed the specific activities of up to three sexual encounters from the previous week and variables associated with these encounters. Participants had 48 hours to complete diaries and were paid up to 60 dollars, pro-rated for participation level. On average, participants completed 83.7% of all diary surveys. In order to avoid multiple enrollment of the same participant, contact information was cross-referenced against: date of birth, age, race/ethnicity, geographic location, contact information, and IP address. Online advertisements did not indicate eligibility requirements in order to minimize the potential for faking eligibility14.
Measures
Demographics
The demographic questionnaire assessed participant age, race/ethnicity, self-reported sexual orientation, and geographic location.
Sexual Behavior
A dichotomous risk score was calculated for each individual sexual encounter reported in weekly diaries (up to three per week). Unprotected anal or vaginal sex was coded 1, and protected anal or vaginal sex and any oral sex (protected or unprotected) were coded 0. All other encounters were excluded from analyses.
Sexual Partnership Characteristics
Sexual partner age was measured on a 7-point Likert scale (−3 = 10+ years younger, −2 = 5–10 years younger, −1 = 1–4 years younger, 0 = same age, 1 = 1–4 years older, 2 = 5–10 older, 3 = 10+ years older). Familiarity with partners was operationalized as the number of previous sexual encounters with a partner and was a numerical response (winsorized range 0–333). HIV status of partner was measured on a 5-point Likert scale (0 = I know this person is HIV negative, 1 = I think this person is HIV negative, 2 = I don’t know this person’s HIV status, 3 = I think this person is HIV+, 4 = I know this person is HIV+). Partner race was dichotomized into Black (1) and Other (0). Partner gender was dichotomized based on biological birth sex (1 = female, 0 = male).
Analyses
Analyses were conducted using Hierarchical Linear Modeling (HLM) 7.0 software15. A Bernoulli distribution was used to model the dichotomous sexual risk outcome. See our previous work for further discussion of analytic considerations for use of HLM with event-level data16,17.
Results
Sexual Behavior and Group Differences in Sexual Risk
Participants had approximately one sexual encounter per week (M = .94, SD = 1.26; range 0–15) and a total of 1,189 encounters observed in the data. Among these, 53.6% were repeat partners and 46.4% were new partners. On average, 27% of encounters were risk episodes (i.e., unprotected anal or vaginal sex). We first ran an unconditional (null) model of the odds of sexual risk with no predictor variables entered at Level 1 or Level 2 to evaluate the extent to which variability in sexual risk was due to individual/group differences (between-subjects characteristics) or change over time (within-persons factors), which can be expressed with a weighted Kappa for dichotomous outcomes18. Weighted Kappa was .26, indicating that participants were largely inconsistent in their unprotected sex behaviors across episodes.
We next tested for reactivity (i.e., change due to study participation) by entering the week of data collection as a Level 1 variable. The results did not support reactivity in responding (OR = 1.00, p = .889). Demographic covariates (i.e., age, race/ethnicity) were then entered at Level 2 to evaluate group differences in sexual risk. Black MSM had 68% lower odds of reporting sexual risk behaviors compared to all other racial groups combined (OR = .32, p < .01). Likelihood of having unprotected anal or vaginal sex did not differ by participant age (OR = 1.00, p = .963).
Racial Composition of Sexual Partners
We conducted two analyses of within- and cross-race sexual partnerships to test our hypothesis that Black MSM would be more racially homophilous. First, we split the sample by participant race (i.e., Black, White and Latino) and evaluated the frequency of having sexual partners of differing racial groups. Among Black MSM, the plurality of sexual encounters occurred with Black partners (45.0%), followed by White (30.5%), Latino (17.6%) and Other (6.9%). For Latino MSM, the plurality of sexual encounters occurred with White partners (46.5%), followed by Latino (34.0%), Other (10.2%), and Black (9.3%). Finally, for White MSM, the majority of sexual encounters occurred with White partners (56.7%), followed by Latino (23.8%), Black (12.1%), and Other (7.4%). A Chi-square test indicated that these distributions were significantly different across participant racial groups, χ2 (9, N = 1189) = 261.69, p < .001.
Next, we ran an HLM model with sexual partner’s race (e.g., Black v. Other) as the outcome variable in order to evaluate racial differences in the likelihood of having partners who were Black, Latino, or White. Black MSM were the most sexually homophilous racial group; they were nearly 11 times more likely than other groups to have Black partners (OR = 10.94, p < .001). Conversely, Latino MSM were 72% less likely to have Black partners than other racial groups (OR = 0.28, p < .05) and White MSM were 66% less likely to have Black partners (OR = 0.34, p < .05). Latino MSM were nearly three times more likely than other racial groups to have Latino partners (OR = 2.81, p < .001), and White MSM were approximately twice as likely to have White partners compared to other racial groups (OR = 2.30, p < .01).
Sexual Partnership Characteristics and Sexual Risk
All analyses of the effects of sexual partnership characteristics on sexual risk were conducted while adjusting for the effects of demographic covariates (age, race/ethnicity, and self-reported sexual orientation) and additional sexual partnership characteristics (partner’s gender, HIV status, and race). Results for the final model are presented in Table 2. For the sample as a whole, only one main effect was significant: participants were more likely to have unprotected sex with female partners than males (OR = 4.59, p < .001). All other main effects were non-significant, including sexual partner’s age (OR = 1.00, p = .989), number of previous sexual encounters with the partner (OR = 1.00, p = .655), partner’s HIV status (OR = 1.09, p = .550), and partner’s race (Black v. Other; OR = 1.06, p = .806).
Table 2.
Sexual Partnership Effects and Odds of Sexual Risk: Full Model of Main and Moderating Effects
| Fixed Effect | Odds Ratio | Confidence Interval | Coefficient Value | Standard Error | t ratio | df | p value |
|---|---|---|---|---|---|---|---|
| Intercept | 0.26 | 0.17 – 0.41 | −1.338 | 0.221 | −6.063 | 123 | *<.001 |
| Age | 1.00 | 0.96 – 1.04 | −0.001 | 0.022 | −0.064 | 123 | .949 |
| Race (Black v. Other) | 0.32 | 0.15 – 0.69 | −1.141 | 0.387 | −2.945 | 123 | *.004 |
| Sexual Orientation (bisexual) | 1.29 | 0.65 – 2.56 | 0.252 | 0.348 | 0.723 | 123 | .471 |
| Partner Age | 1.00 | 0.86 – 1.17 | 0.001 | 0.078 | 0.014 | 5010 | .989 |
| Age | 0.99 | 0.97 – 1.01 | −0.011 | 0.009 | −1.292 | 5010 | .197 |
| Race (Black v. Other) | 1.34 | 1.04 – 1.73 | 0.292 | 0.129 | 2.255 | 5010 | *.024 |
| Age X Race** | 0.96 | 0.93 – 0.97 | −0.038 | 0.018 | −2.214 | 5015 | *.034 |
| Num. Previous Encounters | 1.00 | 0.98 – 1.01 | −0.003 | 0.007 | −0.447 | 5010 | .655 |
| Age | 1.00 | 1.00 – 1.00 | <0.001 | 0.001 | 0.263 | 5010 | .792 |
| Race (Black v. Other) | 1.04 | 1.01 – 1.06 | 0.036 | 0.012 | 2.949 | 5010 | *.003 |
| Age X Race** | 1.00 | 0.99 – 1.01 | 0.002 | 0.002 | 1.248 | 5015 | .212 |
| Partner Gender | 4.59 | 2.12 – 9.94 | 1.523 | 0.395 | 3.859 | 5010 | *<.001 |
| Partner HIV Status | 1.09 | 0.82 – 1.44 | 0.086 | 0.144 | 0.598 | 5010 | .550 |
| Partner Race (Black v. Other) | 1.06 | 0.68 – 1.66 | 0.056 | 0.229 | 0.246 | 5010 | .806 |
NOTE:
Asterisks denote statistical significance at p < .05.
Double asterisks denote effects run as follow-up analyses that were not included in the full multivariate model.
Next, we conducted our exploratory analyses of age and racial differences in the effects of partnership factors. Participant race (Black vs. Other) moderated the effect of sexual partner’s age on sexual risk (OR = 1.34, p < .05). Having an older sexual partner was associated with increased odds of unprotected sex amongst Black MSM. Participant age did not moderate this relationship (OR = 0.99, p = .197). In a follow-up analysis, we entered an interaction term (participant race X participant age) as a moderator of the main effect of participant age on sexual risk. This three-way interaction was significant (Figure 1; OR = 0.96, p < .05). The positive association between sexual partner age and sexual risk in Black MSM became stronger as participant age decreased (i.e., younger Black MSM were the most likely to have unprotected sex with older partners). Conversely, older non-Black MSM were more likely to have unprotected sex with younger partners.
Figure 1. Three-Way Interaction Between Participant Race, Participant Age, and Sexual Partner Age in Predicting Odds of Unprotected Anal or Vaginal Intercourse.
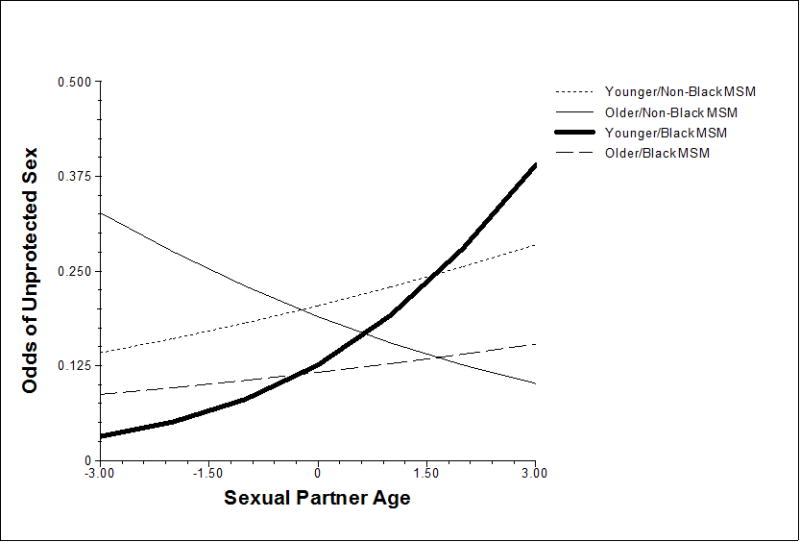
*NOTE: Age x Race x Partner Age interaction is illustrated by splitting participants into four groups. “Younger” and “older” age groups were created by averaging the lower and upper quartiles of participant age. This is done solely for illustrative purposes. Sexual partner age values were −3 = 10+ years younger, −2 = 5–10 years younger, −1 = 1–4 years younger, 0 = about same age as participant, 1 = 1–4 years older, 2 = 5–10 years older, and 3 = 10+ years older.
Participant race also moderated the effect of the number of previous sexual encounters with partners on sexual risk (OR = 1.04, p < .01). For Black MSM, there was a positive association between number of previous sexual encounters with a partner and the odds of sexual risk that was not present among non-black MSM (Figure 2). Neither participant age (OR = 1.00, p = .792) nor the interaction between participant age and race (OR = 1.00, p = .212) were significant moderators of this same main effect. In order to test the robustness of these findings, we further restricted the range of number of previous sexual encounters with a partner to 100 and re-ran the full model. The overall pattern and significance of all effects were unchanged.
Figure 2. Moderating Effect of Participant Race on the Association Between the Number of Previous Sexual Encounters with a Partner and Odds of Unprotected Anal or Vaginal Intercourse.
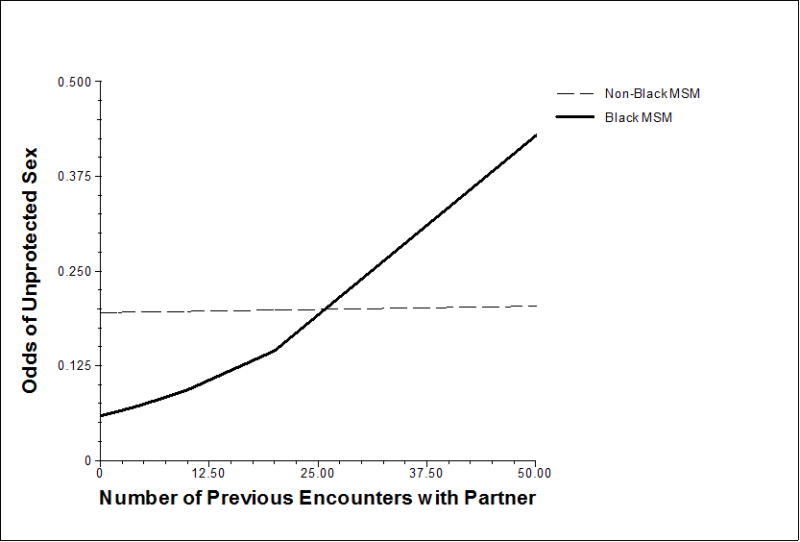
*Note: Number of previous encounters with partner was winsorized at three standard deviations from the mean to reduce the influence of outliers.
Discussion
The current study aimed to empirically test the likelihood of same-race partnerships (sexual homophily) and the influence of sexual partnership characteristics on sexual risk in an ethnically diverse sample of MSM. Black MSM reported significantly less unprotected sex throughout the course of the study. Black MSM were the most racially homophilous group in terms of sexual partnerships, and they were almost 11 times more likely than other racial groups to have Black partners. Given that Black MSM have higher HIV prevalence1, sex within their more homophilous networks confers higher risk compared to the less homophilous and lower HIV prevalent networks of other racial groups. Such a pattern leads to a higher per act risk of infection. If the per act risk is high enough, it could overcome the protective effect of fewer transmission risk acts, therefore leading to increased incidence of infection among Black MSM.
Sexual partner age was a significant predictor of sexual risk, but only for Black MSM. Our analyses found a significant three-way interaction between participant race, participant age, and sexual partner age in predicting odds of sexual risk, such that young Black MSM were the most likely to have unprotected sex with older partners. This is a particularly important finding because young Black MSM are the demographic group that currently experiences the highest HIV incidence2. Odds of having unprotected sex with partners also increased significantly with repeated sexual encounters for Black MSM. It may be that Black MSM are aware that they are at increased risk for acquiring HIV. Subsequently, they may be using certain sexual partnership characteristics, including familiarity with partners, as indicators of HIV risk, which could influence choices about condom use. However, the majority of new HIV infections occur in the context of these types of main, serious or repeated partners19. This strategy of using familiarity with partners to make condom use decisions, were it adopted by Black MSM, could increase their risk for HIV acquisition. It may be advisable for interventions targeting Black MSM to address partner familiarity as a poor indicator when making decisions about condom use.
Our findings indicate that some of the driving forces behind the elevated HIV incidence in Black MSM may be the greater likelihood of racially homophilous sexual networks combined with the stronger influence of sexual partner age and familiarity on condom use. The influence of these partnership variables on condom use would allow HIV to penetrate the networks of Black MSM. The virus would then be able to travel through the smaller more racially homophilous sexual networks of Black MSM more efficiently than its ability to do so in the larger less homophilous networks of non-black MSM. Further investigation is needed to understand the processes underlying these patterns of risk behavior, including interpersonal power dynamics, stigma and discrimination in partner selection, and limited access to community resources.
Findings must be considered in the context of several important limitations. While we adhered to rigorous procedures to minimize risk of multiple enrollment and faking eligibility, it is not possible to rule out these possibilities with online recruitment. Additionally, the sample was relatively small and had limited representation of Black MSM, which may have limited our ability to detect certain interactions between race and partnership characteristics. Finally, the current study excluded MSM who were in sexually-monogamous relationships, were HIV+, or who had not had oral or anal sex with a man in the six months prior to enrollment. Not including these groups means that our results cannot be generalized to the MSM community as a whole.
The current study represents an important advance in understanding the seemingly paradoxical rise in HIV incidence in young Black MSM. Through our analyses, we were able to empirically test several sexual partnership characteristics and network factors that help to explain this disparity using a prospective study of multiple sexual encounters within-persons. With these results in mind, future research must strive to understand the mechanisms underlying these predictors of sexual risk in order to develop efficacious intervention strategies that address the unique needs of Black MSM and reduce the profound effect of HIV/AIDS on this community.
Acknowledgments
This project was funded by a National Research Service Award (NRSA) provided by the National Institute of Mental Health (F31MH088942; PI: Newcomb). Additional funding for participant incentives came from a supplemental dissertation grant from the Chicago Developmental Center for AIDS Research (D-CFAR; PI: Newcomb). Christian Grov, Ph.D. (of Center for HIV/AIDS Educational Studies and Training and Brooklyn College, City University of New York) and Jon Kassel, Ph.D., Robin Mermelstein, Ph.D., and Stewart Shankman, Ph.D. (all of University of Illinois at Chicago) provided helpful comments on earlier drafts of this manuscript.
Sources of support:
National Institute of Mental Health (F31MH088942; PI: Newcomb)
Chicago Developmental Center for AIDS Research (D-CFAR; PI: Newcomb)
Footnotes
Conference presentation of this data:
Newcomb, M. E., & Mustanski, B. (2012, February). What’s driving racial disparities in HIV incidence? The role of sexual partnership characteristics in predicting sexual risk in Black MSM. Paper presented at the international invited meeting Gay Men’s Sexual Health: A Focus on Couples, San Juan, PR.
References
- 1.CDC. HIV in the United States. United States Department of Health and Human Services; 2011. [Google Scholar]
- 2.CDC. HIV and AIDS among gay, bisexual and other men who have sex with men (MSM) United States Department of Health and Human Services; 2010. [Google Scholar]
- 3.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007 Oct 1;21(15):2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 4.Rosenberger JG, Reece M, Schick V, et al. Condom Use during Most Recent Anal Intercourse Event among a U.S. Sample of Men Who Have Sex with Men. J Sex Med. 2012 Feb 21; doi: 10.1111/j.1743-6109.2012.02650.x. [DOI] [PubMed] [Google Scholar]
- 5.Clerkin EM, Newcomb ME, Mustanski B. Unpacking the racial disparity in HIV rates: the effect of race on risky sexual behavior among Black young men who have sex with men (YMSM) J Behav Med. 2011 Aug;34(4):237–243. doi: 10.1007/s10865-010-9306-4. [DOI] [PubMed] [Google Scholar]
- 6.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006 Jun;96(6):1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gates GJ. Sexual minorities in the 2008 General Social Survey: Coming out and demographic characteristics. University of California; Los Angeles: The Williams Institute; 2010. [Google Scholar]
- 8.Raymond HF, McFarland W. Racial mixing and HIV risk among men who have sex with men. AIDS Behav. 2009 Aug;13(4):630–637. doi: 10.1007/s10461-009-9574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry M, Raymond HF, McFarland W. Same race and older partner selection may explain higher HIV prevalence among black men who have sex with men. AIDS. 2007 Nov 12;21(17):2349–2350. doi: 10.1097/QAD.0b013e3282f12f41. [DOI] [PubMed] [Google Scholar]
- 10.Joseph HA, Marks G, Belcher L, et al. Older partner selection, sexual risk behaviour and unrecognised HIV infection among black and Latino men who have sex with men. Sex Transm Infect. 2011 Aug;87(5):442–447. doi: 10.1136/sextrans-2011-050010. [DOI] [PubMed] [Google Scholar]
- 11.Bingham TA, Harawa NT, Johnson DF, Secura GM, MacKellar DA, Valleroy LA. The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men’s Survey, Los Angeles, 1999–2000. AIDS Educ Prev. 2003 Feb;15(1 Suppl A):39–52. doi: 10.1521/aeap.15.1.5.39.23613. [DOI] [PubMed] [Google Scholar]
- 12.Zablotska IB, Grulich AE, De Wit J, Prestage G. Casual sexual encounters among gay men: familiarity, trust and unprotected anal intercourse. AIDS Behav. 2011 Apr;15(3):607–612. doi: 10.1007/s10461-010-9675-2. [DOI] [PubMed] [Google Scholar]
- 13.Prestage G, Van De Ven P, Grulich A, Kippax S, McInnes D, Hendry O. Gay men’s casual sex encounters: discussing HIV and using condoms. AIDS Care. 2001 Jun;13(3):277–284. doi: 10.1080/09540120120043928. [DOI] [PubMed] [Google Scholar]
- 14.Mustanski BS. Getting wired: Exploiting the Internet for the collection of valid sexuality data. J Sex Res. 2001 Nov;38(4):292–301. [Google Scholar]
- 15.HLM 7: Hierarchical linear and nonlinear modeling. [computer program] Chicago, IL: Scientific Software International; 2011. [Google Scholar]
- 16.Mustanski B. The influence of state and trait affect on HIV risk behaviors: a daily diary study of MSM. Health Psychol. 2007 Sep;26(5):618–626. doi: 10.1037/0278-6133.26.5.618. [DOI] [PubMed] [Google Scholar]
- 17.Newcomb ME, Clerkin EM, Mustanski B. Sensation seeking moderates the effects of alcohol and drug use prior to sex on sexual risk in young men who have sex with men. AIDS Behav. 2011 Apr;15(3):565–575. doi: 10.1007/s10461-010-9832-7. [DOI] [PubMed] [Google Scholar]
- 18.Fleiss JL, Cohen J. The equivalence of weighted Kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33(3):613–619. [Google Scholar]
- 19.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009 Jun;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]


