Abstract
Background:
South Africa (SA) is experiencing a rapid epidemiologic transition as a consequence of political, economic and social changes. In this study we described, based on hospital data, the mortality patterns of Non communicable Diseases (NCD), Communicable Diseases (CD), the NCD/CD ratios, and the trends of deaths.
Methods:
We conducted a cross-sectional survey of all deaths occurring in several public hospitals in the Eastern Cape Province of SA between 2002 and 2006. Causes of deaths were coded according to the ICD 10 Edition.
Results:
A total of 107380 admissions responded to the inclusion criteria between 2002 and 2006. The crude death rate was 4.3% (n=4566) with a mean age of 46±21 years and a sex ratio of 3.1 men (n=3453): 1 woman (n=1113). Out of all deaths, there were 62.9% NCD (n=2872) vs. 37.1% CD (n=1694) with NCD/CD ratio of 1.7. The ratio NCD/CD deaths in men was 1.3 (n=1951/1502) vs. NCD/CD deaths in women of 1.9 (n=735/378). The peak of deaths was observed in winter season. The majority of NCD deaths were at age of 30–64 years, whereas the highest rate of CD deaths was at age< 30 years. The trend of deaths including the majority of NCD, increased from 2002 to 2006. There was a tendency of increase in tuberculosis deaths, but a tendency of decrease in HIV/AIDS deaths was from 2002 to 2006.
Conclusion:
Non-communicable diseases are the leading causes of deaths in rural Eastern Cape province of SA facing Post-epidemiologic transition stages. We recommend overarching priority actions for the response to the Non-communicable Diseases: policy change, prevention, treatment, international cooperation, research, monitoring, accountability, and re-orientation of health systems.
Keywords: Mortality, Epidemiologic transition, Non communicable diseases, South Africa
Introduction
There are changes for mortality, Communicable Diseases (CD), and Non communicable Diseases (NCD) worldwide (1–6).
Sub-Saharan Africa shows several studies about poverty, industrialization, urbanization, and epidemiologic transition (6–14). In particular, significant changes in the delivery of health care in the public sector occurred since the end of apartheid in 1994. South Africa (SA) has also embarked in redressing past inequalities and improving access to, and quality of health care to all citizen of the country (13–15).
Among other issues, the Eastern Cape of SA, faces significant challenges with NCD research, practice, and policy, basic equipment for effective diagnosis and treatment of NCD; and adequately trained health workers.
Therefore, the objective of this study was to identify, based on hospital data, the mortality rates of NCD and CD, as well the epidemiologic transition, and the trends of mortality.
Methods
Data in this study came from a survey of rural Eastern Cape Province-wide. Data for the tears 2002–2006 were considered.
The study protocol was approved by the Walter Sisulu University Ethics Committee.
The Eastern Cape Province is located in the south-eastern part of SA. The province shares borders with the Free State province and Lesotho Kingdom in the north, KwaZulu-Natal in the north-east, the Indian Ocean along its south-eastern borders, and Western and Northern–Cape provinces in the West.
A multistage random sampling procedure had 20 districts in the province wide. We conducted a cross-sectional survey between 2002 and 2006. We evaluated all cases of deaths in each district, not only for those who have come to the hospital. Officer responsible of statistics in the district is responsible for registration of both cases of death in the hospitals or also other cases of death especially those who had never came to hospital. Causes of deaths among the admissions were coded to the 10th Revision of International Classification of Diseases (ICD-10).
The variables of interest comprised of demographic (age and sex), months (season of Winter/June), NCD, CD, HIV/AIDS, tuberculosis, and years of 2002, 2003, 2004, 2005, and 2006. Data were extracted from deaths registration using standardized procedures published by other researchers (16–18).
Data and statistical analysis
Data were presented as frequencies (number), proportions (%) for qualitative variables, and mean± standard deviation for continuous variable. The trends of mortality were done across the months, ages, and the years 2002–2006. The coefficient determination (R2) was equal to the short projections of deaths. The software SPSS for Windows version 16.0(SPSS Inc, Chicago, IL, USA) was performed.
Results
For the 5-year period between 2002 and 2006, 107380 admissions had complete data. Of these hospital admissions, 4.3% (n=4566) died and had 46± 21 years.
Among all deaths, the sex ratio was almost 3.1 men (n=3453): 1 woman (n=1113). Out of all deaths, 62.9 % (n=2872) were attributable to NCD, while 37.1% ( n=1694) were attributable to CD: the ratio NCD/CD being 1.7. The NCD had 22 deaths in age<30 years, 2422 deaths in age 30–64 years, and 428 deaths in age>65 years. There was an inverse relationship between CD deaths and ages: 1345 deaths in age<30 years, 309 deaths in age 30–64 years, and 40 deaths in age>65 years.
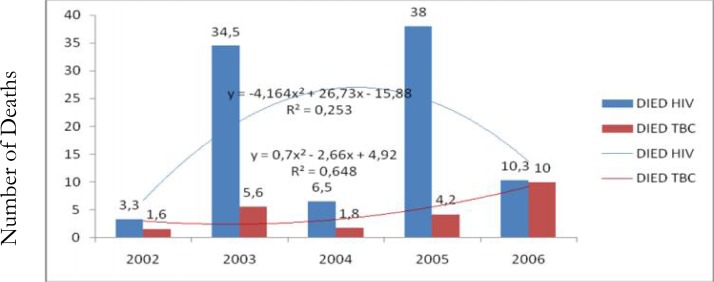
The ratio of NCD/CD deaths in men was 1.3(n=1951 NCD vs. 1502 CD). The ratio of NCD/CD deaths in women was 1.9 (n= 735 NCD vs. 378 CD). The peak of deaths was observed in June (winter season) between 2002 and 2006 (Fig. 1).
Fig. 1:
Relationship between deaths and winter season
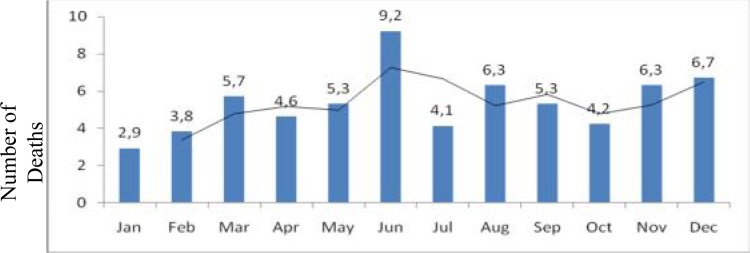
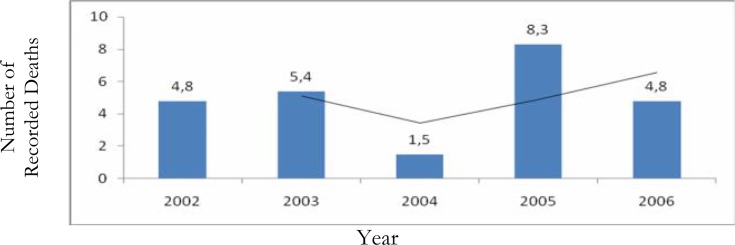
The trend of deaths including the majority of NCD, had an increase with R2= 30.1% from 2002 to 2006 (Fig. 2). There was a tendency of an increase of tuberculosis deaths (R2= 64.9%), but an inverted curve of HIV/AIDS deaths tended to decrease from 2002 to 2006(R2= 25.4%) (Fig. 3).
Fig. 2:
Trends of deaths from 2002 to 2006
Fig. 3:
Trends of HIV/AIDS deaths and Tuberculosis (TBC) deaths from 2002 to 2006
Discussion
The study investigated the extent and the changes of mortality patterns in Eastern Cape Province of SA with a profile of similar to that of countries facing epidemiological transition (19). However, the crude death rate in 2002 – 2006 from this study undertaken in hospitals was significantly lower than the double estimates for rural populations in India (20). NCD are currently the leading cause of death in rural India.
This study also confirmed NCD to be the leading causes of death in Eastern Cape. The data reported globally (2–6), in all South Africa (11) and in other developing countries (20) also incriminated NCD as the leading causes of mortality. According to WHO, NCD were responsible of 60% (35/58 million) of all global deaths in 2005 (21).
In this study conducted in one of the poorest province of SA (15), 62.9% of deaths were attributed to NCD and 37.1% to CD. These findings were similar with 53.8% of all deaths attributed to NCD and 36.4% due to CD in the all developing countries (5).
In its report, the WHO identified a long time ago observed the “growing prevalence of NCDs accounting for the largest proportion of the global burden of disease and even outpacing infectious diseases in all developing countries with the exception of sub-Saharan Africa” (22).
There however remains a constant challenge that even in the light of body of evidence, public health policies and practices globally have consistently been either non-existent or slow in responding to NCDs, with the priority continuing to be on communicable diseases control. Two main reasons for this trend were identified by Glasgow (23) viz. compared to communicable diseases, NCDs play a non-significant role in both high and low politics, no immediate security thread is posed by NCDs compared with HIV?AIDS and hemorrhagic fevers that have been seen destroying even security forces. Secondly, the rising prevalence of NCDs in low and middle income countries is viewed as attributable to western lifestyle globalization including consumption of unhealthy western diets. This latter theory thus supports non-public health view that NCDs are individuals’ responsibility because they are self created (24–25).
The present study showed that this province has witnessed a dramatic change from a burden of disease dominated by mortality from infectious causes to degenerative and chronic causes. This epidemiologic transition (26) as reported in other low- and middle-income countries (27–29), has been experienced in shorter time frame (10 years after 1994, end of Apartheid) than that experienced historically in rich countries (26). In this study, Intra- Midst-, immediate Post-, and advanced Post-epidemiologic transition stages were defined in all patients, in men, and in women. Eastern Cape province is in stage of receding pandemics, which was characterized by CVD and its risk factors predominated by hypertension, congestive heart failure, renal failure, cancer, and stroke. CVD was commoner in men, while cancer was more frequent in women.
The important determinants of mortality in Eastern Cape Province during the 2002 – 2006 period were male gender, aging, rural area, and winter.
In our survey of 2002 – 2006, males were more vulnerable than females as reported by several studies from the literature (30).
Aging in this population facing demographic transition was associated with higher risk of mortality. The improvement of sanitation in South Africa after 1994 (end of apartheid) may explain the control of perinatal deaths, maternal mortality and death related to infection diseases (13). 80% of CVD deaths occur in developing countries, mainly individuals aged 30–69 years (6).
Winter was associated with higher risk of mortality among the patients from Eastern Cape as well observed in other settings. Heunis et al. investigated the short-term relationship between winter temperatures and cardiac diseases mortality in Cape Town, Western Cape province of South Africa (31). They found a strong lagged relationship between extreme temperatures/large daily variations of temperatures and above-average mortality rates. Data from Spain showed the effect of extreme winter temperature on mortality in Madrid for people aged>60 years (32). Poor people from Eastern Cape Province live in huts or shuck without windows neither heater. Cold temperatures give rise to bronchoconstriction, which can enhance previously existing pulmonary diseases. Cold temperatures increase blood pressure, cholesterol, fibrinogen and erythrocyte numbers (33). These mechanisms may explain the outbreaks of deaths observed in this study with CVD and respiratory diseases as leading causes of death.
This study showed a significant social gradient in which patients living in the poor rural areas had higher rates of mortality than advantaged patients from urban areas. The same social gradient was previously demonstrated by Grunewald et al. in the poor sub district of Khayelitsha from Cape Town, Western Cape Province of South Africa (34).
These findings will play an important role in managing patients and shaping public-health policy in Eastern Cape Province and in other resources limited settings in and outside South Africa.
Training of health professionals with a new approach to primary health-care system, adequate management of NCD, and priority actions for the response to the NCD crisis are urgently needed in this poor province and globally. These changes in mortality patterns will provide insight into the evolving course of health transition in Easter Cape province. Public-health Leadership, prevention, treatment, international cooperation, monitoring and accountability are thus at a crossroads of Eastern Cape Province.
As the stages of epidemiologic transition occur ongoing, modification of the Eastern Cape health system is required to ensure that the services provided address the main diseases suffered by the population (20). Among the communicable causes of death that were still widespread in Eastern Cape Province, tuberculosis was prominent because of drug resistance. HIV/AIDS may well have been a contributor to other cases of deaths in infectious diseases such as tuberculosis and meningitis as well as in NCD such as CVD, metabolic syndrome, diabetes mellitus and cancers (8, 11). Antiretroviral therapy (HAART) may impact on decline in HIV/AIDS deaths.
WHO recommends State Members to pay attention to formulating and testing frameworks for chronic care systems, and to the skill-set that is required of multipurpose health professionals to support long-term patient-centered care. For this reason, Cambodia has demonstrated the feasibility of integrating care for HIV/AIDS with NCD in chronic diseases clinics (35).
The first step to combat the NCD epidemic should encompass an extensive and comprehensive research on the dimensions and actual burden of NCD in Eastern Cape. Thorough understanding of the dynamics of epidemiologic transition is important to achieve a serious appraisal of primary health-care systems in this province. Research to establish the Cost, value and feasibility of implementation of the framework will have the way for international support (36).
The Lancet NCD Action Group and the NCD Alliance propose the delivery of the following priority interventions: tobacco control, salt reduction, improved diets and physical activity, reduction in hazardous alcohol intake, essential drugs and technologies.
Although in Eastern Cape province, the burden of mortality due to CD and HIV/AIDS has often overshadowed that due to NCD, there is evidence now of a shift of attention to NCD by identifying and addressing modifiable risk factors(lifestyle changes), screening, diagnosing, treating and follow-upping patients with NCD. Primordial prevention by educating the general population may promote health. Essential components of these Implications include: effective surveillance mechanisms supplemented by focused research; generating broad interest and consensus; mobilizing Leadership and commitment at all levels; involving local and international Expertise; building on existing efforts; and seeking integrated, multidisciplinary and multi-sector approaches (37).
Limits of the study
This study is limited to some degree because of its setting, design and methods. The findings from this hospital-based survey are difficult to be generalized to the Eastern Cape general population. In limited resources settings, hospital data may guide the public policy and research. The cross-sectional design is not able to demonstrate a causal association in the findings.
Several settings use hospital –wide mortality rates to evaluate the quality of hospital care (38), although the usefulness of this metric has been questioned (39).
Conclusion
This study contributes to understand the changes of mortality patterns in a poor setting facing Post-epidemiologic transition stages. There is a positive and significant association between male gender, aging, winter season, rural residence, and higher rates of all deaths.
NCD are the leading causes of mortality pn this poorest and rural province of South Africa. Health policies and programs should learn from the observed and unique pattern of mortality with a rapid progression of epidemiologic transition in general and in women in particular. Clinical Implications and Perspectives for Public Health (Prevention, Health Promotion, and Interventions) should be adequately based on comprehensive information about the extent and nature of mortality in Eastern Cape.
An urgent reorganization of the Eastern Cape Health delivery is needed to enable the implementation of Evidence-Based activities that can curb the rising of NCD.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
The authors declare that they have no competing interests.
References
- 1.World Bank . World Development Report 1993: Investing in health. Oxford University Press; New-York: 1993. [Google Scholar]
- 2.Ehrmann Feldman D, Thivierge C, Guérard L, Déry V, Kapetanakis C, Lavoie G, Beck EJ. Changing trends in mortality and admissions to hospital for elderly patients with congestive heart failure in Montreal. CMAJ. 2001;165:1033–1036. [PMC free article] [PubMed] [Google Scholar]
- 3.Kestellof H, Yuan XY, Jooseens JV. Changing mortality patterns in men. Acta Cardical. 1998;43:133–139. [PubMed] [Google Scholar]
- 4.Murray CJL, Chan LC. Dynamics and patterns of mortality change. In: Chen LC, Kleinman A, Ware NC, editors. Health and social change in international perspective. Harvard University Press; Boston, MA: 1994. pp. 3–23. Sanitary transition. [Google Scholar]
- 5.Lopez AD, Mathers CD, Ezzath M, Jamison DT, Marry CJ. Global and regional burden of diseases and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 6.WHO . Preventing Chronic Disease. Genera: WHO; 2010. A vital investment. [Google Scholar]
- 7.De-Graft Aikens A, Unwin N, Agyemang C, Allotey P, Campell C, Arhinful D. Tacking Africa’s chronic diseases burden : from the local to the global. Global Health. 2010;6:1–7. doi: 10.1186/1744-8603-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Longo-Mbenza B, Ngoma DV, Nahimana D, et al. Screen detection and the WHO STEPwise of arterial hypertention in Kinshasa. Eur J Cardiovasc Prev Rehabil. 2008;15:503–8. doi: 10.1097/HJR.0b013e3282f21640. [DOI] [PubMed] [Google Scholar]
- 9.Young F, Critchly JA, Jonhstone LK, Unwin NC. A review of co-morbility between infections and chronic diseases in Sub-Saharian Africa : TB and Diabetes Mellitus, HIV and Metabolic syndrome, and the impact of globalization. Globalization and Health. 2009:5–9. doi: 10.1186/1744-8603-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bradshaw D, Groenewald P, Laubscher R, et al. Initial burden of disease estimates for South Africa. S Afr Med J. 2003;93:682–688. [PubMed] [Google Scholar]
- 11.Tollman SM, Kahn K, Sartorius B, Collinson MA, Clark SJ, Garenne ML. Implications of mortality transion for primary health care in rural South Africa : a population – based surveillance study. Lancet. 2008;372:893–901. doi: 10.1016/S0140-6736(08)61399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bourne LT, Lambert EV, Styn K. Where does the black population of South Africa stand on the nutrition transition? Public Health Nutr. 2002;5:157–162. doi: 10.1079/PHN2001288. [DOI] [PubMed] [Google Scholar]
- 13.Mayosi BM, Flisher AJ, Lallo VG, Sitas F, Tollman SM, Bradshaw D. The burden of non-communicable diseases in South Africa. Lancet. 2009;374:934–947. doi: 10.1016/S0140-6736(09)61087-4. [DOI] [PubMed] [Google Scholar]
- 14.Chopra M, Lawn JE, Sanders D, et al. Achieving the health Millennium Development Goals for South Africa: challenges and priorities. Lancet. 2008;374:1023–31. doi: 10.1016/S0140-6736(09)61122-3. [DOI] [PubMed] [Google Scholar]
- 15.Statistic South Africa Mortality and causes of death in South Africa. 2005. Findings from death notification.
- 16.Kiielonski D, Stuinberg M, Barron PM. Life after death – mortality statistics and the public health. S Afr Med J. 1989;76:672–75. [PubMed] [Google Scholar]
- 17.Bradshaw D, Kiekowski D, Sitas New birth and death registration forms a foundation for the future, a challenge for health workers? S Afr Med J. 1998;88:971–74. [PubMed] [Google Scholar]
- 18.Murray CJ, Lopez AD. Global burden of Diseases and Injury Series. Vol. 1. Harvard School of Public Health; Boston: 1996. The global burden of disease: a comprehensive assessment of mortality and disability from diseases injuries and risk factors in 1990 and projected to 2020. [Google Scholar]
- 19.Huicho L, Trelles M, Gonzales F, Mendoza W, Mirand J. Mortality profiles in a country facing epidemiological transition: An analysis of registered data. BMC Public Health. 2009;9:47. doi: 10.1 186 / 147 – 2458 – 9 – 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joshi R, Cardona M, Iyengar S, et al. Chronic diseases now a leading cause of death in rural India – mortality data from the Andhra Pradesh Rural Health Initiative. Int J Epidemiological. 2006;35:1522–9. doi: 10.1093/ije/dyl168. [DOI] [PubMed] [Google Scholar]
- 21.Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA. 2004;291:2616–2622. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization . Reducing Risks, Promoting Healthy Life. Geneva: WHO; 2002. The World Health Report 2002. [Google Scholar]
- 23.Glasgow SM. The private life of public health; managing chronic disease in an era of neoliberal governmentality. 2005. [PhD diss], Univ. Maryland, USA;
- 24.O’Manique C. Globalisation’s Pandemic. Houndmill, UK: Palgrave Macmillan; 2004. Neoliberalism and AIDS Crisis in sub-Saharan Africa. [Google Scholar]
- 25.O’Manique C. The securitization of HIV/AIDS in sub-Saharan Africa; a critical feminist lens. Policy Soc. 2005;24:24–47. [Google Scholar]
- 26.Omran AR. The epidemiologic transition : A theory of the epidemiology of population change. Milbank Memorial Fund Q. 1971;49:509–38. [PubMed] [Google Scholar]
- 27.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: Part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–64. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 28.Reddy YN, Murthy SV, Krishna DR, Prabhakar MC. Role of free radicals and antioxidants in tuberculosis patients. Indian J Tuberc. 2004;51:213–8. [Google Scholar]
- 29.Perel P, Casas JP, Ortiz Z, Miranda JJ. Non communicable diseases and injuries in Latin America and the Caribbean: time for action. PLoS Med. 2006;3:e344. doi: 10.1371/journal.pmed.0030344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tollman SM, Kahn K, Garenne M, Gear JS. Reserved in mortality trends : evidence from the Agincourt field site, South African, 1992 – 1995. AIDS. 1999;13:1091–7. doi: 10.1097/00002030-199906180-00013. [DOI] [PubMed] [Google Scholar]
- 31.Heunis JC, Oliver J, Bourns DE. Short-term relationships between winter temperatures and cardiac disease mortality in Cape Town. S Afr Med J. 1995;85:1016–9. [PubMed] [Google Scholar]
- 32.Diaz J, Garcia R, Lopez C, Linares C, Tobias L. Mortality impact of extreme winter temperatures. In J Biometeorol. 2005;49:179–83. doi: 10.1007/s00484-004-0224-4. [DOI] [PubMed] [Google Scholar]
- 33.Thakur CP, Anand MP, Shahi MP. Cold weather and myocardial infarction. Int J Cardiol. 1987;16:19–25. doi: 10.1016/0167-5273(87)90266-x. [DOI] [PubMed] [Google Scholar]
- 34.Groenewald P, Bradshaw D, Daniels J, et al. Cause of death and premature mortality, Cape Town 2002–2006: South African Medical Research Council. 2008. 2008. http://www.mrc.ac.za/bod/premort_cpt.pdf (accessed October 16).
- 35.Janssens B, Damme WV, Raleigh B, et al. Offering integrated care for HIV/AIDS, diabetes and hypertension within chronic disease clinics in Cambodia. Bull World Health Organ. 2007;85:880–885. doi: 10.2471/BLT.06.036574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maher D, Harries AD, Zachariah R, Enarson D. A global framework for action to improve the primary care response to chronic non-communicable diseases: a solution to a neglected problem. BMC Public Health. 2009;9:355. doi: 10.1186/1471-2458-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bovet P, Viswanathan B, Shamlaye C, Romain S, Gedeon J. Addressing non-communicable diseases in the Seychelles: towards a comprehensive plan of action. Global Health Promotion. 2010;(Supp(2)):37–40. doi: 10.1177/1757975910363930. [DOI] [PubMed] [Google Scholar]
- 38.Krakauer H, Bailey RC, Skellan KJ, et al. Evaluation of the HCFA model for the analysis of mortality following hospitalization. Health Serv Res. 1992;27:317–335. [PMC free article] [PubMed] [Google Scholar]
- 39.Shahian DM, Wolf RE, Iezzoni LI, Kirle L, Normand S-LT. Variability in the Measurement of Hospital-wide Mortality Rates. N Engl J Med. 2010;363:2530–2539. doi: 10.1056/NEJMsa1006396. [DOI] [PubMed] [Google Scholar]