Abstract
Background
In the previous studies, the rate of primary infertility was reported differently. It seems the main reasons are related to the different methods of data collection and information analysis. Therefore, introducing a precise method to determine the infertile couples and the population exposed to the risk of infertility is an important issue to study primary infertility.
Methods:
The proposed methodology for assessing primary infertility rate has been designed and applied by Avicenna Research Institute in a national survey. Sampling was conducted based on probability proportional to size cluster method. In this survey, after reviewing the former studies, the reproductive history was used as a basis for data collection. Every reproductive event was recorded with a code and a date in the questionnaire. To introduce a precise method, all possible events were considered thoroughly and for each situation, it was determined whether these cases should be considered in numerator, denominator or it should be eliminated from the study. Also in some situations where the correct diagnosis of infertility was not possible, a sensitivity analysis was recommended to see the variability of results under different scenarios.
Conclusion:
The proposed methodology can precisely define the infertile women and the population exposed to the risk of infertility. So, this method is more accurate than other available data collection strategies. To avoid bias and make a consistent methodology, using this method is recommended in future prevalence studies.
Keywords: Primary infertility rate, Reproductive history, Iran
Introduction
In the field of medical sciences which was used in the present study, primary infertility refers to a condition in which couples have never been able to conceive a child after one year of unprotected intercourse (1, 2). In demography, the term of primary infertility describes the proportion of childless women of reproductive age. From epidemiological point of view, the definition of primary infertility is based on “trying for” or “time to” a pregnancy among the women exposed to conception (3).
In study by Larson, using the question “How long have you tried to get pregnant?” is recommended in epidemiological and demographic studies of infertility using primary data (3). However, this question could not appropriately address the necessary information about the population at risk of pregnancy, which consist of sexually active, noncontracepting and nonlactating women. Individuals have different perception about “the ability to conceive”, “the duration of time they have tried to become pregnant”, “regular sexual activity” and usually forget to report previous abortions and stillbirths. The validity and reliability of such general self-reporting questions should be assessed and it seems this method is subject to recall bias.
In addition, infertility is a cultural sensitive issue. Incorrect information about induced and spontaneous abortion, stillbirth, abstinence from sexual relations, separation and divorce can affect the accuracy of the results. Therefore, the collection of reliable data for this subject should explicitly address these issues.
The general definition of infertility have been explained in many references such as NHS 2004 and WHO report 2000 (4, 5). These references introduce a formal definition of infertility and mention some limitations of this definition. They did not explain an applied way of data collection strategy that can minimize these limitations. For example, WHO report has mentioned this indicator is cultural sensitive, compromised by misclassification and is subject to response bias. However, these general definitions could not address the researcher need in a real survey and an applied data collection strategy is necessary.
Gurunach et al. suggested that differences in the definition of infertility and population exposed to the risk of infertility can causes selection bias which is a typical challenge in prevalence studies (6, 7). Remarkable differences in terms such as “duration of attempt for pregnancy”, “the age of sampled women” or “their marital or cohabitation status” lead to inconsistency in determining the numerator and denominator used to estimate infertility rate.
In several studies findings has been presented without any precise explanation of population at risk or infertility measurement method (8–15). In an article by Guzic and Swan (16), analyzing Chandra and Stephan Study (17), suggested that underestimation of infertility in the United States is a consequence of methodological limitations.
Reproductive calendar including birth date, pregnancies, not–live–birth pregnancy terminations and use of contraceptive methods was applied in 15 of the 47 surveys carried out in DHS comparative report. Although these approaches are appropriate to calculate infertility rate, details of data collection and calculation method have not been indicated (18). Likewise, in the study of Bhattacharya et al. the history of fertility was used as data collection method and the infertility rate was calculated based on different definitions. Nevertheless the method of calculation and referring to the history is not clear enough (19).
Lack of uniformity for the method of calculating primary infertility rate; hampers comparative studies between populations and over time. For example, primary infertility rate of Iranian couples has been reported 8% – 24.9% due to different method of data gathering. So, it seems introducing a precise method to determine the population exposed to infertility is a priority to study the primary infertility rate (20, 21). The present study aimed to introduce an applied data collection strategy with the minimum amount of bias to assess the primary infertility rate and make a consistent methodology for the future researches.
Methods
The proposed methodology for assessing infertility rate has been designed and applied by Avicenna Research Institute (ARI) in an Iranian national survey. Sampling was conducted based on probability proportional to size cluster method. The data collection process was started in late 2010 and was mainly completed at the end of 2011. In this survey, after reviewing the former studies, the reproductive history was used as a basis for data collection. Based on an experts committee every reproductive event including marriage, contraception, contraceptive discontinuation, pregnancy, childbirth, abortion, infertility treatment, ending infertility treatment (discontinuation for any reason), separation (spousal abandonment for more than one year) and even divorce were specified. Each event was recorded with a code and a date in the questionnaire. A pilot study was conducted to ensure the transparency of queries and accuracy of responses. Afterwards, the reproductive history of 17000 married women of the ages 20–40 were recorded. This targeted group was chosen with the aim of avoiding recall bias.
Based on primary infertility rate definition, the number of infertile women represents the numerator and the population exposed to the risk of pregnancy represents the denominator. Defining infertile women and measuring continuous exposure to the risk of pregnancy over a period of one year is difficult and detailed information about reproductive history is necessary. The representativeness of primary infertility rate will be compromised if there is any selection bias either in the numerator or in denominator of this indictor.
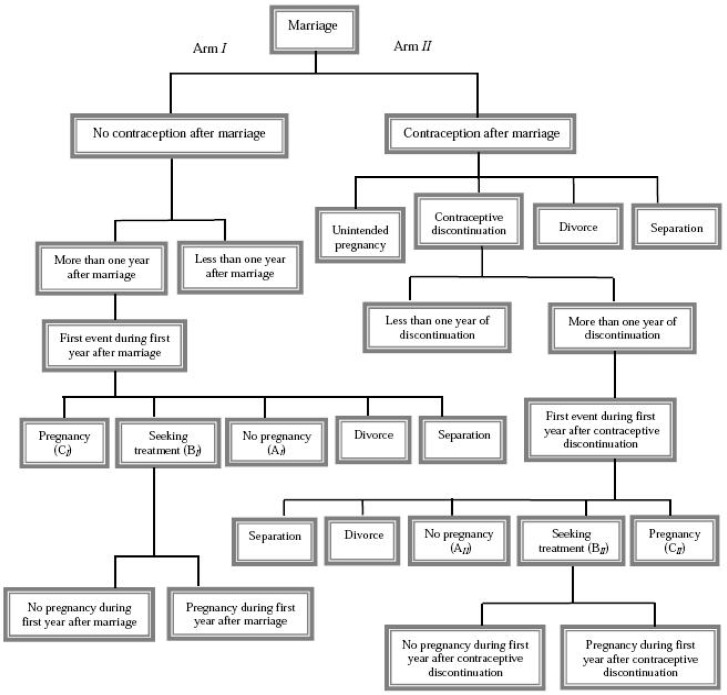
To explain the proposed method for calculating primary infertility rate, a flowchart was designed to pursue the individuals’ reproductive behavior after marriage (Fig. 1). Using contraceptive was the first question that was asked to follow the reproductive history in this flowchart. The arm I entails women who have not use contraceptive and the arm II are women who have used it after marriage. In the arm I, women were categorized in two group based on the duration of time from the marriage. If the duration is less than one year, the data should be discarded from the study because these women have the opportunity to get pregnant until one year. For noncontracepting women whose duration of time from marriage is more than one year the first event during the first year were asked. This event could be pregnancy, seeking treatment, no pregnancy, divorce and separation. If the next event is pregnancy, the woman is considered fertile. If a treatment is initiated during this period, the individuals are divided into fertile and infertile groups based on the occurrence of pregnancy in the first year. Those seeking treatment women who have not become pregnant in the first year after marriage were considered infertile. However, the fertility status of seeking treatment women who become pregnant in the first year remains unknown. Indeed potentially infertile women may become pregnant following treatment. In this situation, sensitivity analysis should be applied so that analysis is performed with and without information of this group in the numerator and the real infertility rate falls between these calculated values. Since infertile couples usually seek treatment at the end of the first year and the probability of fertility for these subjects in the first year are negligible, all seeking treatment couples were considered infertile and the number of these couples was used in numerator and denominator of primary infertility rate. It is noteworthy to mention that the accuracy of this assumption was assessed in this national survey and slight difference in the results of sensitivity analysis confirmed this assumption. In the future studies, interested researchers can assess the accuracy of this assumption similarly. Also, all women in “no pregnancy” group were considered infertile. Furthermore, the women who divorced or lived apart from their husband in the first year have been excluded from the denominator because they are not exposed to the risk of fertility for a period of one year. Since divorce or separation were occurred in the first year and the couples still has the opportunity to become pregnant, it doesn’t seem the infertile women were more likely to be divorced or separated. Therefore, exclusion of these subjects from the study produces no bias.
Fig. 1:
Fallowing the individual’s reproductive behavior through the flowchart
The arm II of the flowchart devoted to women who have used contraceptives after marriage. The first event could be contraceptive discontinuation, separation, divorce and unintended pregnancy. Women whose first event after contraception was separation or divorce were discarded because they were not exposed to the risk of pregnancy. The couples who discontinued contraception were categorized in two groups. If the duration of time from contraceptive discontinuation is less than one year, the data should be excluded from calculation of primary infertility rate because no judgment is acceptable about their fertility status. Otherwise, their subsequent event after contraceptive discontinuation was asked. If pregnancy occurs during the first year, the women are considered fertile. Similar to the reasons that were explained for the arm I, all seeking treatment women were considered infertile. If pregnancy does not occur during the first year after contraceptive discontinuation, the women are considered infertile. Likewise, women who has divorced or separated in the first year after contraceptive discontinuation were excluded from denominator since they were not at risk of fertility for a period of one year.
As indicated in the flowchart, unintended pregnancy is one of the events that can occur after using contraception. This group usually should have used ineffective contraceptive methods. It should be noted unintended pregnancy is a subgroup of ineffective contraceptive cohort while the infertile subgroup of this cohort will not be distinguished easily. Although, some part of this infertile subgroup will appear in box AII (no pregnancy) and BII (seeking treatment), it seems the major part of them will continue using contraceptives or have not experienced at least one year after contraceptive discontinuation (and as a result they will be discarded from calculations). Therefore, both including and excluding unintended pregnancy in the denominator of primary infertility will impose biases but in two different directions. We believe that excluding this group will cause less bias than including them. But as a sensitivity analysis, the interested researcher can consider both of these decisions to check the variability of results.
Note that for simplicity only important situations were considered in this study. It is possible to extend this method to consider other situations, but this extension will complicate the results. In summary, the following formula was used in the calculation:
Where AI, BI, CI, AII, BII, CII were defined in the flowchart. Indeed the numerator of these fraction consist of the number of individuals in “no pregnancy” and “seeking treatment” groups as the first event after one year of unprotected intercourse and the denominator consist of individuals in “no pregnancy”, “seeking treatment” and “pregnancy” groups as a first event after one year of unprotected intercourse. Although at the first glance this is a simple formula, the logic that was used in determining its numerator and denominator is very important and usually this scrutiny is ignored in other available data collection strategies.
Result
There are many factors influencing the infertility rate calculation. Hence, our focus in current paper is only to explain the methodological aspects and corresponding flow-chart specifically to minimize common biases in such studies. With this prerequisite paper, there is indeed no need to explain this method in the future papers where we would like to focus on the results and analyses of the infertility rate calculations.
Conclusion
Infertility is a key criterion to measure the health. It is essential for health care providers to know the prevalence of infertility, assess the need for treatment and indentify the causes of infertility. The increasing use of assisted reproductive techniques (ARTs) and growing number of infertility clinics necessitate a thorough evaluation of infertility and its causes in the country. To achieve this goals the accurate calculation of primary infertility rate is significantly important.
Unfortunately some definitions of primary infertility are too general to precisely determine infertile women and the population exposed to the risk of fertility. Defining the population at risk of infertility is difficult and without extra details, it is not possible for responder or even interviewers to find the true answer.
As mentioned in introduction, lack of uniformity for the method of calculating primary infertility rate hamper comparative studies between populations and over time. Although, some of the differences may be justifiable due to the effect of time, sampling and physiological changes; but it seems the main reasons are related to the methods of data collection and information analysis.
In the present study, using the reproductive history was recommended as an appropriate data collection method for calculating this rate. In this method all possible events is explicitly defined and infertile women and the population at risk of infertility is precisely determined. So, this method is more accurate than other alternatives. The other advantage of this method is classification of subjects in different groups. The researcher has the opportunity to adjust the calculation based on available information about each of these groups; In situations where correct diagnosis of infertility is not possible, this method offers a sensitivity analysis that considers different possible scenarios and shows the variability of results across this scenarios. Therefore, the proposed method can minimize the usual biases and is recommended for applying in the future prevalence studies.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
We thank our colleagues Maryam Farahani, Sara Aliyazdi, Shima Shahamat Manesh, Shadi Amani and somayeh abouzar in the Avicenna Research Institute for their full cooperation during this study. The authors declare that there is no conflict of interest.
References
- 1.Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HWG, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231–45. doi: 10.1093/humupd/dmp048. [DOI] [PubMed] [Google Scholar]
- 2.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. The international committee for monitoring assisted reproductive technology (ICMART) and the world health organization (WHO) revised glossary on ART terminology. Hum Reprod. 2009;20(11):2683–7. doi: 10.1093/humrep/dep343. [DOI] [PubMed] [Google Scholar]
- 3.Larsen U. Research on infertility: Which definition should we use? Fertil Steril. 2005;83(4):846–52. doi: 10.1016/j.fertnstert.2004.11.033. [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Clinical Excellence. Fertility: assessment and treatment for people with fertility problems, Clinical Guidline11. 2004. Available from: www.nice.org.uk.
- 5.World Health Organization. Reproductive health indicators for global monitoring: report of the second interagency meeting. 2000. Department of Reproductive Health and Research, Geneva. Available from: www.google.com.
- 6.Stephen EH, Chandra A. Estimating infertility: not the last word. Fertil Steril. 2006;86(3):534. doi: 10.1016/j.fertnstert.2006.02.129. [DOI] [PubMed] [Google Scholar]
- 7.Gurunath S, Pandian Z, Anderson RA, Bhattacharya S. Defining infertility-a systematic review of prevalence studies. Hum Reprod Update. 2011;17(5):575–88. doi: 10.1093/humupd/dmr015. [DOI] [PubMed] [Google Scholar]
- 8.Savitz DA, Hertz-Picciotto I, Poole C, Olshan AF. Epidemiologic measures of the course and outcome of pregnancy. Epidemiol Rev. 2002;24(2):91–101. doi: 10.1093/epirev/mxf006. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Reproductive Health Indicators, Guidelines for their generation, interpretation and analysis for global monitoring. 2006. Department of Reproductive Health and Research, Geneva. Available from www.google.com.
- 10.Thonneau P, Spira A. Prevalence of infertility: international data and problems of measurement. Eur J Obstet Gynecol Reprod Biol. 1991;38(1):43–52. doi: 10.1016/0028-2243(91)90206-z. [DOI] [PubMed] [Google Scholar]
- 11.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat. 2005;(25) series 23. [PubMed] [Google Scholar]
- 12.Kumar D. Prevalence of female infertility and its socio-economic factors in tribal communities of Central India. Rural Remote Health. 2007;7(2):456. [PubMed] [Google Scholar]
- 13.Ericksen K, Brunette T. Patterns and predictors of infertility among African women: A cross-national survey of twenty-seven nations. Soc Sci Med. 1996;42(2):209–20. doi: 10.1016/0277-9536(95)00087-9. [DOI] [PubMed] [Google Scholar]
- 14.World Fertility Report. United Nations, department of economic and social affairs, Population Division. 2007. Available from: www.google.com.
- 15.Lunenfeld B, Van Steirteghem A. Infertility in the third millennium: implications for the individual, family and society: condensed meeting report from the Bertarelli Foundation’s second global conference. Hum Reprod Update. 2004;10(4):317–26. doi: 10.1093/humupd/dmh028. [DOI] [PubMed] [Google Scholar]
- 16.Guzick DS, Swan S. The decline of infertility: apparent or real? Fertil Steril. 2006;86(3):524–6. doi: 10.1016/j.fertnstert.2006.05.027. [DOI] [PubMed] [Google Scholar]
- 17.Stephen EH, Chandra A. Declining estimates of infertility in the United States: 1982–2002. Fertil Steril. 2006;86(3):516–23. doi: 10.1016/j.fertnstert.2006.02.129. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Infecundity, infertility, and childlessness in developing countries. Demographic and Health Surveys (DHS) Comparative reports No. 9. 2004. Available from: www.google.com. [Google Scholar]
- 19.Bhattacharya S, Porter M, Amalraj E, Templeton A, Hamilton M, Lee AJ, et al. The epidemiology of infertility in the North East of Scotland. Hum Reprod. 2009;24(12):3096–107. doi: 10.1093/humrep/dep287. [DOI] [PubMed] [Google Scholar]
- 20.Safarinejad MR. Infertility among couples in a population-based study in Iran: prevalence and associated risk factors. Int J Androl. 2008;31(3):303–14. doi: 10.1111/j.1365-2605.2007.00764.x. [DOI] [PubMed] [Google Scholar]
- 21.Vahidi S, Ardalan A, Mohammad K. Prevalence of Primary Infertility in the Islamic Republic of Iran in 2004–2005. Asia Pac J Public Health. 2009;21(3):287–93. doi: 10.1177/1010539509336009. [DOI] [PubMed] [Google Scholar]