Abstract
Background
We estimated the prevalence of HIV, sexually transmitted infections (STIs), and risky behaviors among female sex workers (FSW) in Kerman City, Iran.
Methods:
Women, 18 years or older, who reported selling sex for at least 6 months during their lifetime and had at least one sexual contact with a client in the recent 12 months were sampled using Responding Driven Sampling (RDS). Participants were interviewed about their sexual behaviors and provided whole blood for HIV, syphilis, and Herpes simplex type 2 (HSV2) testing. Data were analyzed using RDSAT Version 6.0 software.
Results:
Among samples of 177 FSW, we did not find any HIV positive cases. The weighted prevalence of syphilis and HSV2 were 7.2% and 18.0%, respectively. The reported STI syndromes for the proceeding year of the survey were 36%. Unprotected sexual contact was about 17–22% and link to injecting drug users through injection was about 18%.
Conclusion:
While this survey found no HIV, there were findings of risky sexual behaviors and STI, markers for potential infection for HIV. The prevalence of STI and sexual risk behaviors for HIV is considerably high in this subpopulation that alarming for an urgent public health preventive measures and national control-plan to be developed and implemented.
Keywords: Sexual transmitted infections, Respondent-driven sampling, HIV, Female sex-workers, Iran
Introduction
The HIV epidemic in Iran is an aggregated linked epidemic among the subpopulations of injecting drug users (IDUs), prisoners, and recently sexual partners of IDUs and female sex workers (FSW). According to the latest report of HIV unit / Center for Disease Management (1), up to September 2011, near to 24000 cases have been identified in Iran whom 8.7% were female. Based on the reported cases in 2010, 20.8% have been infected through sexual contacts which are significantly higher in compare to the preceding years. The trend is toward the sexual routes of HIV infection and now the national HIV programme is targeting the new high risk groups like FSW. In the literature, the STI/HIV co-infection among the high-risk groups, MSM (2) and FSW (3), have been reported several times. Moreover, STI prevalence has been reported as a proxy of population vulnerability to HIV (3, 4) particularly where it has not been imported to the community yet. Among those who have STI, the risk of HIV transmission is three to four times more than those who are STI free (5, 6). All of these prompted to include the STI surveillance as one of the main components of new generation HIV surveillance. This has been considered in the new rounds of bio-behavioral surveys among the high-risk groups in Iran including FSW. Based on the last situation analysis of STI in Iran in 2008 (7), among the few prevalence studies, it was reported that the overall STI prevalence in general population is considerable and the trend is increasing. The overall prevalence of Gonococci is relatively low and in most studies the prevalence is limited to 0.2 and 0.6% but in one study, it was about 2% (8, 9). The same findings were seen on syphilis prevalence while it was about 0% to 0.06% (7, 10). Many studies, mostly among the pregnant women, indicated the high prevalence of Chlamydia infection at about 21 to 23% (11, 12). Among the 966 volunteer blood donors in Kerman, 2.7% had antibody for HSV2 (13). The key missing groups for the STI prevalence studies was the high-risk hard to reach subpopulations including female sex workers.
As a result, we designed this study to provide valid estimates of HIV, syphilis and HSV2 prevalence and their risky behaviors in female sex workers in Kerman, an urban setting, using respondent driven sampling.
Methods
We conducted a bio-behavioral survey among FSW that received an ethical approval from Kerman University of Medical Sciences from February to May 2010 in Kerman (a mid-size urban setting with a high level of stigma). We recruited 177 FSW by respondent driven sampling technique who met the inclusion criteria; having more than 18 years, selling sex for at least 6 months during their life and having at least one sexual contact with the clients in the recent 12 months.
The interview site was a health facility in downtown appointed to provide services to FSW in a secure and safe setting in Kerman. We started the recruitment process with 8 seeds while later expanded to 12 seeds. Seeds had the strong social networks with the population of FSW in the city and had good collaboration with the interview site staff. The seeds provided the verbal informed consent, participated in face-to-face interview that was conducted by one of two trained interviewers to complete the standardized behavioral questionnaire. The laboratory staff collected venous blood draw for HIV (ELISA), syphilis testing (Treponema pallidum hemagglutination –(TPHA IgG and IgM) and HSV2 (IgM test) after pre-test counseling. Each seed was given primary incentive (40000 Rails as equal to 4 USD) and also three recruitment coupons to recruit other FSW in the study if they completed all parts of survey. They could receive secondary incentive if they presented the valid payment coupon (20000 Rails as equal to 2 USD). By following the referral chain, seeds recruited next participants (wave 1) to the survey and this recruitment continued with further chains to reach to required sample size. The chains were traceable with the coupon serial numbers. The site supervisor was screening the referred FSW for the valid coupon number and for the eligibility criteria. After that they completed the process same as the seeds. The behavioral questionnaire, derived from FHI(Family Healthy Indicators), WHO, UNAIDS, and UNGASS criteria consisted of questions related to demographic information, sexual history and marriage, partners and clients, drug history, condom use, knowledge for HIV transmission and prevention, STI symptoms and HIV testing history. The questionnaire also had 5 questions to collect the network size of each FSW and applied this for weighted analysis. All parts of survey were anonymous and the questionnaires and blood samples were linked together by the coupon number of each participant. They could refuse to continue whenever they wanted.
All the data were entered and cleaned in EpiData v.3.1. We drew the referral chain of recruited FSW using NetDraw. We calculated the point and interval estimates for the categorical behaviors using RDSAT Version 6.0. We used the survey command package in STATA V.11 to calculate point and interval estimates for the continuous variables and assess the related risks of STIs.
Results
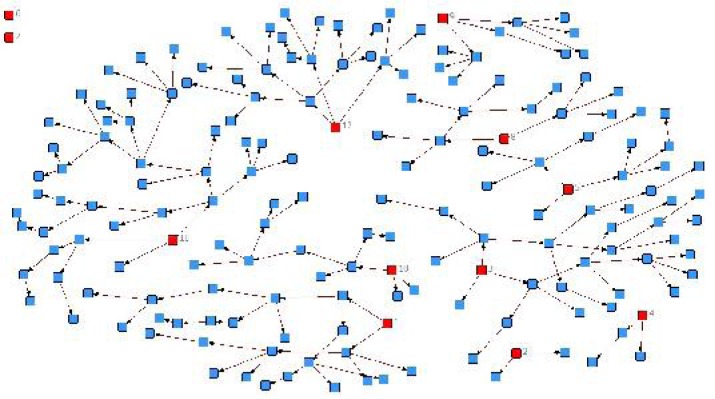
The survey lasted 4 months in Kerman City. Two seeds did not recruit additional participants. Finally, 10 remained seeds recruited 165 FSW and the final sample comprised of 177 FSW participants and the maximum chain length were 6 (Fig.1).
Fig. 1:
Referral chain of recruited FSW in the RDS Kerman. The 12 red boxes stand for seeds while two of them could not recruited any eligible cases to the study
Thirty eight participants refused biologic testing. The average network size of the participants was 7.28.
The weighted mean age of participants were 30.8 (95% CI: 28.9 – 32.7) years (minimum, maximum and median age were 18, 53 and 29 respectively). Approximately 65% of FSW were under 30 years old (Table 1). The weighted mean age of participants who had ever been married were 17.06 (95% CI: 16.1 – 17.9) when they first got married. About 90% of participants were not single at the time of study (Table 1). The demographic characteristics of participants are shown in Table 1.
Table 1:
Weighted estimators and 95% confidence intervals for demographic characteristics of female sex workers, Kerman, Iran 2010
| Demographic factors | Sample Size* | Weighted % (95% CI) |
|---|---|---|
| Age category | ||
| <20 yr | 8 | 4.5 (1.3–8.8) |
| 20–29 yr | 85 | 60.2 (51.3–71.3) |
| +30 yr | 63 | 35.3 (23.6–44.9) |
| Education | ||
| Illiterate | 9 | 5.3 (1.1–9.8) |
| Primary School | 30 | 12.7 (6.1–19.8) |
| Middle School | 48 | 27.5(20.3–37.4) |
| High School | 68 | 41.3 (32.7–54.1) |
| University | 9 | 13.1 (3.4–20.1) |
| Ever been married | 141 | 86.3 (78.3–92.8) |
| Current Marital Status | ||
| Single | 23 | 11.8 (6.4–17.1) |
| Married | 27 | 8.9 (4.4–15.5) |
| Divorced | 63 | 42.5 (31.7–52.6) |
| In a temporary | 12 | 9.5 (3.9–16.2) |
| Relationship | 38 | 27.2 (18.0–38.0) |
| Widow |
Excluded seeds
While the mean age of participants at first sex were 17.35 (95%CI: 16.6 – 18.1), they were 24.88 (95%CI: 22.75 – 27.0) years old when they received money for sex for the first time and more than 70% of them were under 20 years old (Table 2).
Table 2:
Weighted estimators and 95% CI for Risky Behaviors of female sex workers, Kerman, Iran 2010
| Risky Behaviors | Sample Size* | Weighted % (95% CI) |
|---|---|---|
| Age at first commercial sex | ||
| <=20 yr | 101 | 70.2 (56.7–81.1) |
| >20 yr | 62 | 29.8 (18.9–43.3) |
| Attending in group sex in last week | ||
| Yes | 13 | 10.0 (4.3–16.7) |
| No | 161 | 90.0 (83.3–95.7) |
| Ever linked to a place/home for sex | ||
| Yes | 105 | 78.9 (59.7–92.5) |
| No | 59 | 21.1 (7.5–40.3) |
| Using condom in the last sex with paying partner | ||
| Yes | 145 | 83.1 (71.8–91.7) |
| No | 19 | 16.9 (8.3–28.2) |
| Using condom in the last sex with non-paying partner | ||
| Yes | 111 | 78.3 (64.7–89.4) |
| No | 28 | 21.7 (10.6–35.3) |
| History of Broken Condom in the last month | ||
| Yes | 87 | 67.2 (57.1–78.9) |
| No | 71 | 32.8 (21.1–42.9) |
| History of STI syndrome in the last year | ||
| Yes | 64 | 35.9 (26.8–45.7) |
| No | 101 | 64.1 (54.4–73.2) |
| Ever injected drugs | ||
| Yes | 21 | 18.0 (10.3–27.4) |
| No | 117 | 82.0 (72.7–89.7) |
| Consistency of high risk injection | ||
| Unusually | 3 | ------ |
| Never | 16 | ------ |
| Having enough knowledge about HIV transmission¥ | 63 | 45.7 (33.1–58.2) |
Excluded seeds
A knowledgeable person was the one who answered three questions on prevention and rejected two misconceptions on this area, correctly
The average working years as FSW were 3.05 (95%CI: 2.3 – 3.8) among participants. The mean number of clients that participants had in the last week was 2.64 (95%CI: 2.18 – 3.10). Non condom use in the last sexual act with paying and non-paying partners was reported by 17% and 22% of FSW, respectively.
Near to 18% of FSW had ever injected drugs and the mean age at first injection was 18.76 (95%CI: 16.76 – 20.77). This means, 18% of FSW in Kerman has a link to the population of injecting drug users. The characteristic of risky behaviors are shown in Table 2.
None of the participants were HIV positive, while the prevalence of syphilis and HSV2 were 7.2% and 18% respectively (Table 3).
Table 3:
Weighted estimators and 95% CI for HIV, VDRL, HSV2 of female sex workers, Kerman, Iran 2010
| HIV, VDRL, HSV2 | Sample Size* | Weighted % (95%CI) |
|---|---|---|
| Total sample size | 139 | |
| HIV Positive | 0 | ----- |
| VDRL Positive | 8 | 7.2 (2.5 – 13.5) |
| HSV2 Positive | 28 | 18.0 (8.2 – 28.3) |
Excluded seeds
Discussion
Based on the findings, the HIV infection still is not introduced in the female sex worker population in Kerman. However, they are very prone to obtain the infection and transmit to other high risk groups such as male clients and injecting drug users. Group sex was reported by one tenth of the FSW and we believe that this socially stigmatized behavior would be much higher in reality.
In a recent published paper on size of high-risk populations for HIV in Kerman, the population size of men who have extramarital sex with women (not sex workers) was estimated as of 15937 (95% CI 13293–18581). Also, it was estimated that 9314 (95%CI 7710–10916) of men have sexual contact with FSW in Kerman (14).
Considering in mind what we found in the study results; the prevalence of STI infection (7–18%) and STI syndromes (36% during last year) and unsafe sexual act (17–22%) and broken condom during sexual act (67%), it seems that there is an urgent need for implementing effective public health interventions for increasing the behavioral risk of adult population in Kerman. In our study, we have reported the condom use in last sexual act. However, what’s required for prevention of HIV infection is the consistent and proper use of condom. We believe some parts of the high rate of broken condom we have seen in the results were due to the lack of knowledge and skill on how to use condom. This is considering higher than what we see in the literature (15, 16), and need to be added to the intervention package for FSW. It also need to involved adult men population as the target of these training programs to ensure proper use and safe use of condom (15).
Surprisingly, near to 80% of the FSW have a sort of link to place/home for sexual act or seeking for clients. This can be used as a great opportunity, as in such places the public health authority can have the focus for providing effective preventive measures and required services.
We have estimated the prevalence of HSV2 and syphilis as the level of 18% and 7%. In comparison to the general population (13), HSV2 is about six times more in the FSW which is a marker for high risk and unprotected sexual contacts. In the literature, HSV2 has been mentioned as a proxy indictor for much hidden stigmatized sexual high-risk behaviors in FSW and also other high-risk subpopulations (17).
For syphilis, we also have seen a very higher prevalence in FSW in compare to the general population (7, 10), where is almost less than 1% in Iran. In other countries, some reports have indicated extremely high syphilis prevalence in FSW, ranging from 10% to 38%. In China, during the last 5–7 years, the number of reported Syphilis case has been raising dramatically, while from 1999 to 2005, it was stables at a level of 5–7 cases per 100,000 in the general population. And syphilis becomes one of the top five communicable infections in many provinces and states (18). Based on the experiences in China regarding this epidemic and effective responses, it’s recommended to the Iran health authorities to develop and support a national control plan for syphilis while ensure the availability of rapid point-of-care tests in many public and private clinics in Iran helps promote routine screening and timely diagnosis of this epidemic-prone disease.
To add to what we have discussed about the prevalence of current STI infections in FSW, we should emphasis that the history of STI syndromes (even genital ulcer or vaginal discharge) in the recent year was three to four times more than the detected prevalence of HSV2 and syphilis. This put more stress on the necessity of having a comprehensive timely control programme for STIs in Iran. STI services should be included in the service package of all health facilities serving the female sex workers and also the family planning and antenatal clinic health centers where serving sexually active people.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
The authors would like to give special thanks to Dr. Halleh Tajadini and also all the staff of Rezvan Health Facility for providing assistance in implementing the survey. Also, we want to appreciate the HIV/AIDS National Office in CDC/Ministry of Health for the technical and financial support. The authors declare that there is no conflict of interest.
References
- 1.MOHME, Center for Disease Management. Statistics of HIV/AIDS in islamic republic of Iran: Quarterly, Oct 2011: Center for disease management. Ministry of Health and Medical Education; Islamic Republic of Iran: 2011. [Google Scholar]
- 2.Mumtaz G, Hilmi N, McFarland W, Kaplan RL, Akala FA, Semini I, Riedner G, Tawil O, Wilson D, Abu-Raddad LJ. Are HIV epidemics among men who have sex with men emerging in the Middle East and North Africa?: a systematic review and data synthesis. PLoS Med. 2010;8:e1000444. doi: 10.1371/journal.pmed.1000444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lattimore S, Yin Z, Logan L, Rice B, Thornton A, Molinar D, Leong G, Presanis A, De Angelis D, Gill N, Delpech V. Situation of HIV infections and STIs in the United Kingdom in 2007. Euro Surveill. 2008;13(49) article 3. [PubMed] [Google Scholar]
- 4.Kehinde AO, Lawoyin TO. STI/HIV co-infections in UCH, Ibadan, Nigeria. Afr J Reprod Health. 2005;9:42–8. [PubMed] [Google Scholar]
- 5.Gray RH, Wawer MJ. Probability of Heterosexual HIV-1 Transmission per Coital Act in Sub-Saharan Africa. J Infect Dis. 2012;205:351–2. doi: 10.1093/infdis/jir751. [DOI] [PubMed] [Google Scholar]
- 6.Gray RH, Wawer MJ, Brookmeyer R, Sewankambo NK, Serwadda D, Wabwire-Mangen F, Lutalo T, Li X, vanCott T, Quinn TC. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet. 2001;357:1149–53. doi: 10.1016/S0140-6736(00)04331-2. [DOI] [PubMed] [Google Scholar]
- 7.Ministry of Health and Medical Education, Center for disease Control,HIV/STI Office. Sep, 2008. Situation Analysis of Sexually Transmitted Infections In the Islamic Republic of Iran.
- 8.Abdolahian P, Shojai Tehrani H, Asghari S, Oodi M. Frequency of gonococcal endocervicitis in child bearing age women and its risk factors. Journal of Midical Faculty of Gilan University of Medical Sciences and Health Services. 2005;14:63–69. [Google Scholar]
- 9.Gooya MM, Nabaee S. Prevalence of some sexually transmitted infections in a family planning service. Journal of Iran University of Medical Sciences and Health Services. 2005;14:63–69. [Google Scholar]
- 10.Orang M, Asmar M. Seroreversion of serological tests for syphilis in the disabled community in Mazandaran province of Iran. Iranian Journal of Indectiouse Diseases and Tropical Medicine. 2002;19:22–26. [Google Scholar]
- 11.Chamani-Tabriz L, Tehrani MJ, Akhondi MM, Mosavi-Jarrahi A, Zeraati H, Ghasemi J, Asgari S, Kokab A, Eley AR. Chlamydia trachomatisprevalence in Iranian women attending obstetrics and gynaecology clinics. Pak J Biol Sci. 2007;10:4490–4. doi: 10.3923/pjbs.2007.4490.4494. [DOI] [PubMed] [Google Scholar]
- 12.Hashemi FB, Pourakbari B, Yazdi JZ. Frequency of Chlamydia trachomatis in women with cervicitis in Tehran, Iran. Infect Dis Obstet Gynecol. 2009;2009:67014. doi: 10.1155/2007/67014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arabzadeh AM, Fekri A, Shamseddini S, Zohoor A. Prevalence of HSV2 Ab among blood donors in Kermam in 2001. Journal of Kermam University of Medical Sciences. 2002;10:53–59. [Google Scholar]
- 14.Shokoohi M, Baneshi MR, Haghdoost AA. Size Estimation of Groups at High Risk of HIV/AIDS using Network Scale Up in Kerman, Iran. Int J Prev Med. 2012;3:471–476. [PMC free article] [PubMed] [Google Scholar]
- 15.Crosby RA, Yarber WL, Sanders SA, Graham CA, McBride K, Milhausen RR, Arno JN. Men with broken condoms: who and why? Sex Transm Infect. 2007;83:71–75. doi: 10.1136/sti.2006.021154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albert AE, Warner DL, Hatcher RA, Trussell J, Bennett C. Condom use among female commercial sex workers in Nevada's legal brothels. Am J Public Health. 1995;85:1514–1520. doi: 10.2105/ajph.85.11.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abu-Raddad LJ, Schiffer JT, Ashley R, Mumtaz G, Alsallaq RA, Akala FA, Semini I, Riedner G, Wilson D. HSV-2 serology can be predictive of HIV epidemic potential and hidden sexual risk behavior in the Middle East and North Africa. Epidemics. 2010;2:173–82. doi: 10.1016/j.epidem.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tucker JD, Yin YP, Wang B, Chen XS, Cohen MS. An expanding syphilis epidemic in China: epidemiology, behavioural risk and control strategies with a focus on low-tier female sex workers and men who have sex with men. Sex Transm Infect. 2011;87(Suppl 2):ii16–8. doi: 10.1136/sti.2010.048314. [DOI] [PMC free article] [PubMed] [Google Scholar]