Abstract
Background
Validation for depression in preschool children has been established; however, to date no empirical investigations of interventions for the early onset disorder have been conducted. Based on this and the modest efficacy of available treatments for childhood depression, the need for novel early interventions has been emphasized. Large effect sizes for preschool psychotherapies for several Axis I disorders suggest that earlier intervention in depression may also be promising. Therefore, a novel form of treatment for preschool depression, Parent Child Interaction Therapy Emotion Development (PCIT-ED) was developed and tested.
Methods
A preliminary randomized controlled trial (RCT) was conducted comparing PCIT-ED to psycho-education in depressed 3-7 year olds and their caregivers. N=54 subjects met symptom criteria for DSM-IV MDD and were randomized, N=19 subjects completed the active treatment (N=8 drop-outs) and N=10 completed psycho-education (N=17 drop-outs).
Results
Both groups showed significant improvement in several domains, with PCIT-ED showing significance in a greater number of domains. An Intent-to-Treat analysis suggested that PCIT-ED was significantly more effective than psycho-education on executive functioning (p=0.011, ES=0.12) and emotion recognition skills (p=0.002, ES=0.83).
Conclusions
The RCT proved feasible and suggests an individual control condition should be used in future trials to minimize differential drop-out. These pilot data, although limited by power, suggest that PCIT-ED may be a promising early intervention for depression. Larger scale randomized controlled trials of PCIT-ED for depressed preschoolers are now warranted.
Keywords: preschool depression, parent child interaction therapy
Introduction
Over the past 2 decades, empirical studies have provided validation for a clinical depressive syndrome in children as young as age 3, preschool onset MDD (PO-MDD) (Egger & Angold, 2006; Luby et al., 2003; Luby et al., 2002; Luby, Mrakotsky, Heffelfinger, Brown, & Spitznagel, 2004). Preschool depression has also been detected in epidemiological samples in at least one European and several U.S. sites (Egger & Angold, 2006; Lavigne, LeBailly, Hopkins, Gouze, & Binns, 2009; Wichstrom, unpublished data). Homotypic continuity between PO-MDD and the well-known school age form of the disorder has also been reported, suggesting PO-MDD is an early manifestation of the childhood disorder (Luby, Si, Belden, Tandon, & Spitznagel, 2009). More recently, alterations in brain function and structure, similar to patterns observed in adult MDD, have been found in school age children who displayed PO-MDD even when depression had remitted (Gaffrey et al., 2010; Luby, Botteron, & Barch, unpublished data). These data suggest that PO-MDD has similar pathophysiology to the adult form of the disorder.
Since this earlier onset form of the disorder has only recently been recognized, no investigations of treatments have yet become available. The need for and challenges inherent in such investigations are underscored by the findings that the school age form of the disorder has proven to be difficult to effectively treat using currently available interventions. A meta-analysis of cognitive behavioral therapy in school age children, a treatment with known efficacy in adolescents and adults, demonstrated only small to moderate effect sizes (0.35 overall) when used in this age group (Weisz, McCarty, & Valeri, 2006). Interpersonal psychotherapy, a treatment also known to be effective in depressed adults and adolescents, has not yet been tested in school age children (Dietz et al., 2008; Mufson, Dorta, Moreau, & Weissman, 2004). While some efficacy of the serotonin reuptake inhibitor fluoxetine in affected school aged populations has been reported, dangers and side effects have also been of increased concern in this age group (Emslie et al., 1997; Wagner, 2005).
Based on these concerns, there has been increased interest in novel interventions with the potential for greater efficacy for the treatment of childhood depression. The findings of continuity of preschool depression into school age, as well as alterations in brain function and structure evident at school age related to a history of PO-MDD, support the need for early interventions that go beyond the important goal of relieving the suffering of affected preschoolers. These findings also suggest that early intervention in depression may have the potential to ameliorate the suffering and limit the impairment not only during the preschool period, but possibly across childhood.
The relatively slow progress of innovation, the modest effect sizes of many established mental health treatments, as well as the unfavorable risk-benefit ratios of some of the first-line pharmacological treatments have led to a call for new models for conceptualizing and investigating mental disorders using a neuro-developmental approach (Hyman, 2007; Insel et al., 2010). In this context, the relatively large effect sizes reported in early childhood interventions for several major mental disorders are of particular interest. Large effect sizes associated with positive treatment outcomes have been observed in very early behavioral interventions in several disorders, including Autistic Spectrum Disorders (Dawson, 2008) and disruptive disorders. Specifically, Parent Child Interaction Therapy (PCIT) vs. comparison groups’ effect sizes range from 0.61 to 5.67 (Thomas & Zimmer-Gembeck, 2007), and effect sizes for “The Incredible Years,” another early intervention for disruptive behaviors, range from 0.46 to 0.89 (Webster-Stratton & Hammond, 1997; Webster-Stratton, Reid, & Hammond, 2004). A number of factors, including the central and influential role of the parent-child relationship as well as greater neuroplasticity of the brain, may serve as unique moderators of the robust treatment effects evident in these very early childhood interventions. These promising findings could suggest that intervention earlier in life may provide a window of opportunity for more effective treatment in a wider variety of mental disorders, including depressive disorders, similar to the well-established greater efficacy of earlier interventions to remediate speech, language and motor delays.
Towards this end, we aimed to design and preliminarily test an early psychotherapeutic intervention for preschool depression. In searching for early interventions applicable for adaptation to the treatment of preschool onset MDD, PCIT (Brinkmeyer & Eyberg, 2003) stood out as an appropriate and promising treatment modality. While developmental adaptations of the leading psychotherapy for childhood MDD, Cognitive Behavioral Therapy, were considered, we chose instead to adapt a treatment with favorable age-appropriate methods and known efficacy in other preschool onset disorders. PCIT is a dyadic treatment that utilizes an in vivo teach and coach approach to enhance positive relationship development and firm and nurturing parenting. PCIT has been shown to be highly effective for the treatment of preschool disruptive disorders based on a large empirical database demonstrating impressive effect sizes, as noted above, and enduring efficacy into school age without booster sessions (Hood & Eyberg, 2003). Another appealing feature of PCIT was the goal of teaching the parent to serve as the “arm of the therapist,” a role that could have enhanced power in early childhood as well as high potential cost effectiveness. Therefore, we utilized the core techniques of PCIT in the design of an additional module to address emotion recognition and regulation, domains previously hypothesized to be central to early onset MDD (Luby & Belden, 2006), and areas that are not direct targets of standard PCIT. An open trial of this treatment with N=8 subjects revealed high favorability and treatment fidelity (Lenze, Pautsch, & Luby, 2011). Following this, a pilot RCT was conducted and findings related to feasibility and key outcomes are reported here.
Methods
All study procedures were approved by the Washington University School of Medicine Institutional Review Board, and written informed consent from caregiver (and age-appropriate verbal assent from preschoolers) was obtained prior to participation in research procedures.
Participants
Children between the ages of 3.0 and 7.0 were recruited from community pediatricians’ offices between June 2008 and July 2010 using the Preschool Feelings Checklist (PFC), a parent-completed screening checklist with an established cut-off for identifying risk for MDD (Luby, Heffelfinger, Koenig-McNaught, Brown, & Spitznagel, 2004). The PFC was made available at primary care sites known to serve high risk populations and through advertisements for the treatment study on the child mental health clinic’s “on hold line” and parent resource websites. Those scoring above the cut-off were invited to complete a telephone screening interview for eligibility. Inclusion criteria were: between ages 3.0 and 7.0; meeting research diagnostic criteria for Major Depression [as assessed by the Preschool Age Psychiatric Assessment (PAPA; see Measures below)](Egger, Ascher, & Angold, 1999); and living with primary caregiver > 6 months. Exclusion criteria were: concurrently in active psychotherapy or on unstable doses of psychotropic medication; major medical or neurological disease; Pervasive Developmental Disorder; IQ <70; and adoption after 12 months of age (based on higher risk of attachment disorders and socio-emotional delays in this group that could impact treatment efficacy). Those meeting eligibility criteria were randomized (using a computer-generated randomization table) to one of the intervention conditions and scheduled to complete baseline assessments. No stratification or block techniques were used in randomization. After randomization, and prior to the start of treatment, a comprehensive baseline assessment (described in detail below) was conducted.
Interventions
A novel treatment for preschool depression, an adaptation of PCIT entitled PCIT-Emotion Development (PCIT-ED) was developed and manualized (Luby, 2009; Stalets, Pautsch, McGrath, & Luby, unpublished manual). PCIT-ED consists of 3 modules conducted over 14 sessions in 12 weeks. The core modules of PCIT, Child Directed Interaction (CDI) and Parent Directed Interaction (PDI), were utilized, but limited to 4 sessions each. These modules focus on key elements of PCIT including: strengthening the parent-child relationship by teaching and in vivo coaching of positive play techniques, giving effective commands, and methods for handling child noncompliance and disruptive behavior in a firm, non-punitive manner. The novel Emotion Development (ED) module was designed to help the parent serve as a more effective emotion guide and regulator for the child. This 6-session module was completed after the CDI and PDI based on the notion that with significant gains achieved in relationship quality and self-efficacy (from CDI) and effective limit-setting (from PDI), the dyad would be well poised to begin the challenging work of focusing on emotion development. The ED module reinforces skills learned during the CDI and PDI modules and continues to utilize core techniques of PCIT, in vivo teaching and coaching of skills, and between-session homework to facilitate emotional development. However, the novel ED module directly teaches emotional competence, including accurate recognition of one’s own emotions as well as those of others, and focuses on emotion regulation strategies.
Both parents were invited to participate, although the mother was the primary participant for most families. Five therapists (Master’s and Doctoral level clinicians) delivered the intervention as primary and co-therapist pairs. The co-therapist operated the recording equipment, assisted with in-session role plays, and monitored treatment fidelity and other in-session ratings. Co-therapists received the same training as primary therapists in all rating and adherence measures. Each session was rated in vivo by the co-therapist using the Treatment Integrity Checklist (Eyberg, 1999), customized for the content within each session to monitor adherence to the treatment manual. Therapists maintained a high degree of adherence (average 97%, range 87-100%). All treatment sessions were videotaped and viewed by all PCIT-ED research therapists and a senior child psychiatrist (JL) in weekly supervision sessions, in which fidelity to the treatment manual and therapeutic issues specific to each case were discussed.
A psycho-education control condition, “Developmental Education and Parenting Intervention (DEPI),” was developed for administration to parents in small group sessions. This didactic intervention was designed to control for time and expectancy and to educate parents about child development. It emphasized emotional and social development without individual coaching or practice with behavioral techniques as provided in PCIT-ED. Topics included growth, nutrition, safety, parenting practices, cognitive, language and brain development, and normative emotional and social development. DEPI was administered by an experienced Master’s level clinician, or licensed clinical psychologist, and a structured manual guided each session’s topic. Group size ranged between 2-6 attendees and sessions were 60 minutes long for a total of 12 weeks.
Measures
Trained interviewers blind to the treatment condition, and uninvolved in the treatment process, conducted the pre- and post-treatment assessments. Participants were randomized to treatment prior to administration of the full baseline assessment battery and the first treatment session took place within 7 days of the assessment. Attempts were made to conduct post-treatment assessments within 14 days of the final PCIT-ED or DEPI session (median 11 days). Parents were compensated $50 and the child was given a small toy for participating in each assessment.
Primary outcome
Caregivers were interviewed about their child’s symptoms of depression and other relevant Axis I co-morbid disorders using the PAPA, a reliable measure of Axis I disorders (and severity) in preschool children, pre- and post-treatment (Egger, et al., 1999; Egger et al., 2006). Depression severity was also measured pre- and post-treatment using parent ratings on the Preschool Feelings Checklist-Scale Version (PFC-S), a 20-item adaptation of the PFC (described above) with a likert rating scale (0=never, 4=most of time) designed to assess depression severity in preschool children with favorable psychometrics (Cronbach’s alpha= 0.92, test/re-test ICC=0.82). Examples of items on the scales include: “My child appears sad or says he/she feels sad” and “Blames him/her self”.
Functional outcomes
The Health and Behavior Questionnaire (HBQ) (Armstrong, Goldstein, & the MacArthur Working Group on Outcome Assessment, 2003) parent-rated Internalizing and Externalizing domains were also used, providing dimensional ratings of mental health symptoms and adaptive functioning. Higher scores on the HBQ are indicative of more severe pathology. Psychosocial impairment was measured using the Preschool Early Childhood Functional Assessment Scale (PECFAS) (Hodges, 1994; Murphy, Ramirez, Anaya, Nowlin, & Jellinek, 1999), a semi-structured interview with established validity and reliability. Overall scores above 40 are indicative of serious impairment (Murphy, et al., 1999).
Emotion recognition and regulation
Emotion recognition was measured using the 40-item version of the Penn Emotion Differentiation Test (KIDSEDF) (Gur et al., 2001; Gur et al., 2010), a validated measure of emotion recognition that preschoolers completed via a standard computer program. This task involves selecting the more intense facial expression of emotion based on 40 pairs of faces shown one pair at a time. Scores indicate the total number of correct judgments, with higher scores indicative of better performance. Measures of emotion regulation included the Emotion Regulation Checklist (ERC)(Shields & Cicchetti, 1997), a parent-rated measure of the child’s typical pattern of emotion reactivity with established validity. Questions are rated on a likert scale (1=never, 4=almost always) and include items such as: “My child is a cheerful child” and “My child can recover quickly from episodes of upset or distress.”
Executive functioning
Parent-rated measures of the preschoolers’ executive functioning were obtained using the Behavior Rating Inventory of Executive Function-Preschool Version (BRIEF) (Gioia, Espy, & Isquith, 2003), a widely used 63-item measure with favorable psychometrics validated for use in children below age 6. Executive Function (EF) is generally defined as an overarching concept that captures the control, supervisory, or self-regulatory functions used to organize and direct cognitive activity and emotional and behavioral response (Isquith, Crawford, Espy, & Gioia, 2005). Core domains such as inhibition, shifting of attention, and working memory are considered to underlie many executive-related behaviors. Research has demonstrated that EF-related domains such as those noted above demonstrate a protracted developmental course that, when assessed with developmentally appropriate tasks, can be evaluated during the preschool years (Zelazo, Muller, Frye, & Marcovitch, 2003). Executive function in preschool children as measured by the BRIEF includes behavioral indicators of inhibitory self-control, emotional control, working memory, task shifting, and planning/organizational abilities. T-scores are calculated from a standardized program to allow normative comparisons.
Parent emotion and stress
Parents filled out the Beck Depression Inventory-II (BDI-II) (Beck, Steer, & Brown, 1996), a 21-item measure of parental depression symptom presence and severity. Clinical interpretations of BDI-II scores use the following guidelines: 0-13 minimal depression; 14-19 mild depression; 20-28 moderate depression; and 29-63 severe depression.
Parents also completed the Parenting Stress Index 3rd Edition (PSI) (Abidin, 1995), a widely used reliable and valid measure designed to assess child characteristics, parent characteristics, family context, and life stress as it relates to a parent-child system. Normative percentile scores fall between the 15th and 80th percentiles, with scores above the 85th percentile indicating clinical levels of stress or dysfunction.
Statistical Analyses
Categorical demographic variables at baseline were compared using Chi-square tests or Fisher’s Exact tests. Analyses of covariance, covarying for baseline values, were used to compare post-treatment assessment scores in PCIT-ED and DEPI groups. Pre- and post-treatment scores were compared within PCIT-ED and DEPI groups using paired t-tests. Both intent-to-treat (ITT) and completer analyses were conducted. For ITT analyses, subjects without a post-treatment assessment were considered to have no difference in pre- and post-treatment assessment scores. For completer analyses, only participants with both a pre- and post-treatment assessment completing at least 10 treatment sessions (to ensure that some ED sessions were completed) were included. The ITT analyses were considered the primary analyses, and completer analyses were considered secondary. Within group completer results are presented in eTable 1. Tests were considered significant at α=0.05 significance level. Analyses were performed using SPSS version 18 statistical software (SPSS, Inc., Chicago, IL).
Results
Demographic Data
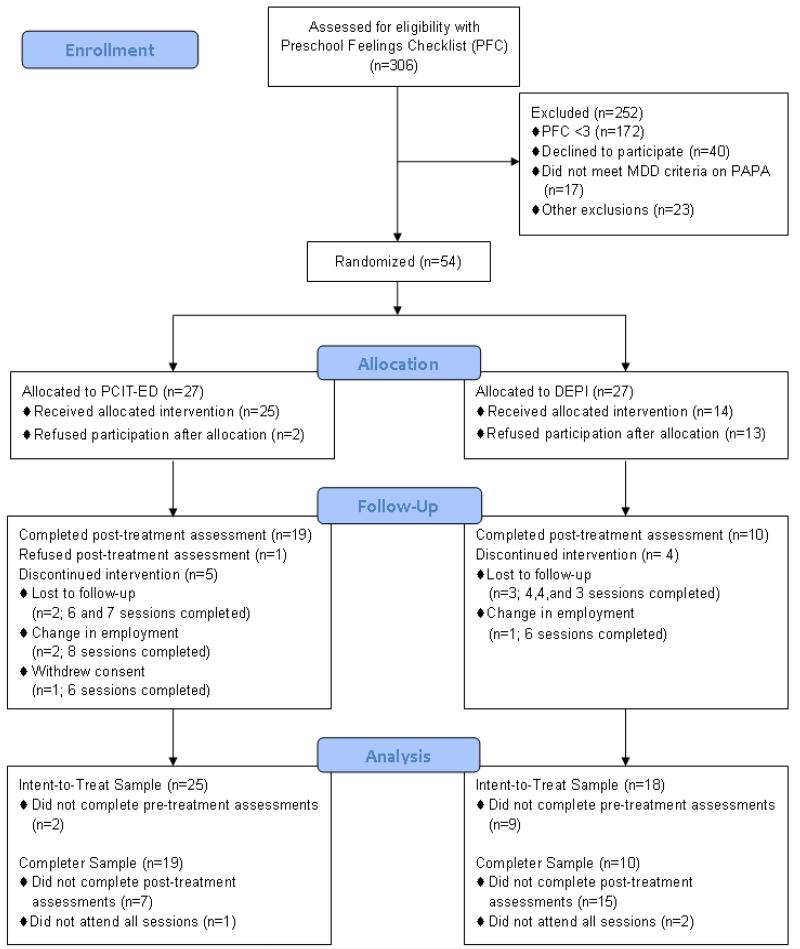
In response to the recruitment procedures described above, N=306 PFC checklists were submitted to the Early Emotional Development Program (EEDP) and N=134 had a score of ≥3 making them eligible for further screening (see Figure 1). Of these, N=40 met one or more exclusion criteria (including N=17 who failed to meet PAPA MDD symptom criteria) and N=40 refused further participation. The N=54 subjects who met all inclusion criteria and agreed to participate were randomized to the treatment study and completed full pre-treatment assessments. Several participants were taking stable doses of medication for disruptive behavior during the study protocol. Nineteen PCIT-ED subjects and 14 DEPI subjects were not taking psychotropic medications. After randomization, N=8 participants dropped out of the PCIT-ED intervention (N=2 dropped out prior to pre-treatment assessment) and 17 dropped out of the DEPI group (N=9 dropped out prior to pre-treatment assessment), leaving N=19 subjects completing PCIT-ED and N=10 completing DEPI (see Figure 1). The high drop-out rate for the control condition appeared to be related to the perceived need for more intensive treatment based on the following: 40.7% of DEPI families dropped out after group assignment and prior to any participation in DEPI sessions. The rates of completion in the PCIT-ED group (70.4%) and DEPI group (37.0%) were significantly different (Chi-square=6.03, df=1, p=0.014). There were no significant adverse events reported or observed from any study participants. Demographic characteristics of the sample of ITT subjects are presented in Table 1.
Figure 1. Participant Flow.
Table 1. Demographics and Sample Characteristics.
| Intent-to-Treat, N (%) |
|||||
|---|---|---|---|---|---|
| PCIT-ED (N=25) |
DEPI (N=18) |
p | |||
| Age, y | |||||
| 3 | 2 | (8.0) | 7 | (38.9) | 0.108a |
| 4 | 10 | (40.0) | 5 | (27.8) | |
| 5 | 10 | (40.0) | 4 | (22.2) | |
| 6 | 3 | (12.0) | 2 | (11.1) | |
| Sex | |||||
| Male | 14 | (53.8) | 13 | (72.2) | 0.278b |
| Female | 11 | (42.3) | 5 | (27.8) | |
| Ethnicity | |||||
| White | 23 | (88.5) | 14 | (77.8) | 0.414a |
| Black | 1 | (3.8) | 3 | (16.7) | |
| Other | 1 | (3.8) | 1 | (5.6) | |
| Parental education | |||||
| High school diploma | 4 | (16.0) | 3 | (16.7) | 0.524a |
| Some college | 5 | (20.0) | 7 | (38.9) | |
| 4-year college degree | 8 | (32.0) | 3 | (16.7) | |
| ≥Graduate education | 8 | (32.0) | 5 | (27.8) | |
| Parent marital status | |||||
| Married | 18 | (69.2) | 11 | (61.1) | 0.549a |
| Widowed | 1 | (3.8) | 0 | (0.0) | |
| Separated | 0 | (0.0) | 2 | (11.1) | |
| Divorced | 2 | (7.7) | 2 | (11.1) | |
| Never married | 4 | (15.4) | 3 | (16.7) | |
| Total family income, $ | |||||
| ≤20,000 | 3 | (12.0) | 2 | (12.5) | 0.923a |
| 20,001 - 40,000 | 3 | (12.0) | 3 | (18.8) | |
| 40,001 - 60,000 | 4 | (16.0) | 3 | (18.8) | |
| >60,000 | 15 | (60.0) | 8 | (50.0) | |
Fisher’s exact test;
χ2 test
Depression Diagnosis and Severity
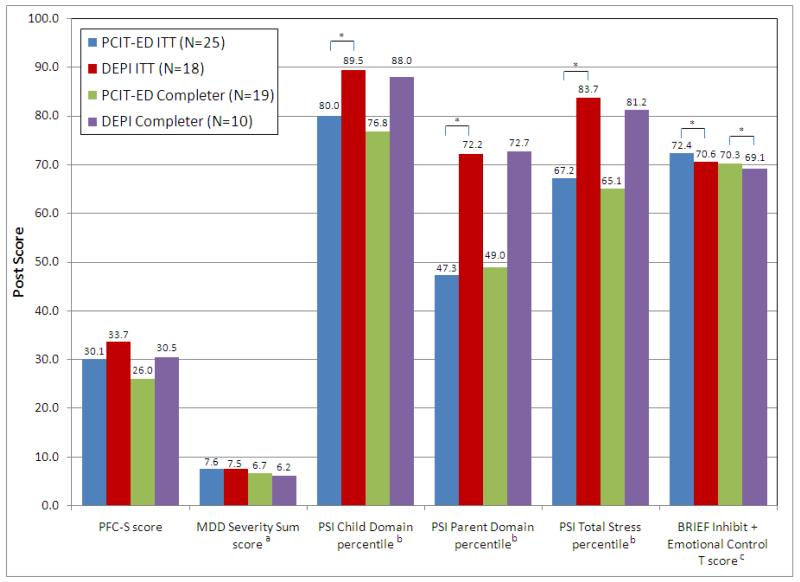
When depression severity was measured according to the PFC-S, preschoolers in both the PCIT-ED and DEPI groups showed significant declines in depression severity (see Table 2). Depression severity measured using the PAPA MDD severity sum score decreased significantly only in the PCIT-ED group (see Table 2), but no differences in post-treatment PAPA MDD severity sum scores between groups were found (see Figure 2).
Table 2. Within Group Pre- and Post-Treatment Assessment Score Comparisonsa.
| Intent-to-Treat Analyses |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PCIT-ED (N=25) |
DEPI (N=18) |
|||||||||
| Pre Mean (SD) | Post Mean (SD) | ES | Pre Mean (SD) | Post Mean (SD) | ES | |||||
| PFC-S score | 42.8 | (5.8) | 30.1 | (11.3) | 2 17** * | 39.8 | (10.3) | 33.7 | (10.6) | 0.58** |
| MDD severity sum scoreb | 11.3 | (4.2) | 7.6 | (4.0) | 0.86*** | 9.0 | (4.7) | 7.5 | (4.7) | 0.31 |
| HBQ-P internalizing symptomsc | 0.76 | (0.29) | 0.65 | (0.34) | 0.37* | 0.74 | (0.26) | 0.63 | (0.28) | 0.40* |
| HBQ-P externalizing/ADHDd | 0.91 | (0.37) | 0.82 | (0.41) | 0.25* | 0.84 | (0.41) | 0.79 | (0.40) | 0.10 |
| HBQ-P functional impairment-selfe | 0.86 | (0.31) | 0.64 | (0.43) | 0.72** | 0.79 | (0.39) | 0.61 | (0.47) | 0.46* |
| HBQ-P functional impairment-familyd | 1.26 | (0.53) | 0.93 | (0.56) | 0.60*** | 1.20 | (0.68) | 1.08 | (0.71) | 0.17 |
| PECFAS total scoreb | 63.2 | (21.7) | 50.0 | (25.5) | 0.60** | 61.2 | (23.9) | 55.3 | (29.0) | 0.24 |
| ERC negativity/lability scoref | 41.5 | (6.0) | 37.8 | (7.2) | 0.60** | 38.9 | (7.8) | 38.5 | (8.9) | 0.05 |
| ERC emotion regulation scoref | 21.6 | (3.1) | 23.3 | (3.5) | 0.53** | 22.8 | (3.6) | 24.0 | (3.2) | 0.32 |
| Penn Emotion Differentiation scoreg | 19.9 | (8.2) | 23.6 | (9.1) | 0.44** | 20.3 | (5.3) | 17.1 | (7.6) | 0.59 |
| BRIEF inhibit + emotional control T scoreh | 77.7 | (13.9) | 72.4 | (13.5) | 0.37*** | 69.5 | (12.4) | 70.6 | (14.5) | 0.09 |
| BRIEF shift + emotional control T scoreh | 76.7 | (11.4) | 70.9 | (12.4) | 0.50*** | 69.3 | (10.6) | 67.3 | (11.2) | 0.18 |
| BRIEF working memory + plan/organize T scoreh | 70.6 | (14.9) | 65.6 | (13.4) | 0.33** | 65.2 | (12.5) | 63.1 | (14.2) | 0.16 |
| BDI-II total score | 10.7 | (8.3) | 8.0 | (8.8) | 0.31** | 14.5 | (8.4) | 13.1 | (9.7) | 0.17 |
| PSI child domain percentilei | 94.6 | (9.3) | 80.1 | (25.8) | 1.53** | 89.8 | (18.9) | 89.5 | (18.2) | 0.02 |
| PSI parent domain percentilei | 47.3 | (31.9) | 46.6 | (32.0) | 0.02 | 63.1 | (28.8) | 72.2 | (24.8) | 0.31 |
| PSI total stress percentilei | 79.6 | (22.9) | 67.0 | (32.3) | 0.54** | 82.9 | (20.0) | 83.7 | (23.2) | 0.04 |
| PSI life stress percentilei | 63.0 | (30.4) | 43.0 | (35.7) | 0.65** | 69.2 | (25.8) | 61.6 | (33.9) | 0.29 |
PFC-S = Preschool Feelings Checklist - Scale Version, HBQ-P = Health and Behavior Questionnaire - Parent Version, PECFAS = Preschool Early Childhood Functional Assessment Scale, ERC = Emotion Regulation Checklist, BRIEF = Behavior Rating Inventory of Executive Function -Preschool Version, BDI-II = Beck Depression Inventory-II, PSI = Parenting Stress Index
comparisons were made using paired t-tests;
N=17 DEPI;
N=24 PCIT-ED, N=16 DEPI;
N=24 PCIT-ED, N=17 DEPI;
N=24 PCIT-ED, N=17 DEPI;
N=16 DEPI;
N=19 PCIT-ED, N=16 DEPI;
N=23 PCIT-ED, N=16 DEPI;
N=23 PCIT-ED, N=18 DEPI;
p<0.05;
p<0.01;
p<0.001
Figure 2. Between Group Comparisons of Post Scores.
ITT = intent-to-treat, PFC-S = Preschool Feelings Checklist - Scale Version, PSI = Parenting Stress Index, BRIEF = Behavior Rating Inventory of Executive Function - Preschool Version
aN=17 DEPI ITT; bN=24 PCIT-ED ITT, N=18 PCIT-ED completer, N=9 DEPI completer; cN=23 PCIT-ED ITT, N=16 DEPI ITT, N=16 PCIT-ED completer, N=9 DEPI completer; * p<0.05
Symptom Scales and Impairment
There were no significant differences between the PCIT-ED and DEPI groups on any post-treatment HBQ subscale scores. Both the PCIT-ED and DEPI ITT groups showed significant improvement in the internalizing (see Table 2), depression (PCIT-ED: 0.74±0.28 to 0.60±0.29, p=0.021, ES=0.49; DEPI: 0.67±0.30 to 0.51±0.24, p=0.029, ES=0.52), and functional impairment-self domains (see Table 2). The PCIT-ED group also showed significant improvement in the overanxious (0.80±0.42 to 0.69±0.40, p=0.027, ES=0.26), externalizing/ADHD symptoms (see Table 2), conduct problems (0.57±0.41 to 0.49±0.40, p=0.041, ES=0.21), overt hostility (0.93±0.60 to 0.74±0.50, p=0.019, ES=0.31), ADHD symptoms (1.19±0.41 to 1.09±0.50, p=0.033, ES=0.24), inattention (1.18±0.43 to 1.01±0.50, p=0.008, ES=0.38), and functional impairment-family domains (see Table 2), and the DEPI group showed significant improvement in the separation anxiety domain (0.83±0.37 to 0.70±0.42, p=0.017, ES=0.34). Total PECFAS scores decreased significantly in the PCIT-ED group, but not in the DEPI group (see Table 2). Post-treatment total impairment measured by the PECFAS did not significantly differ between groups.
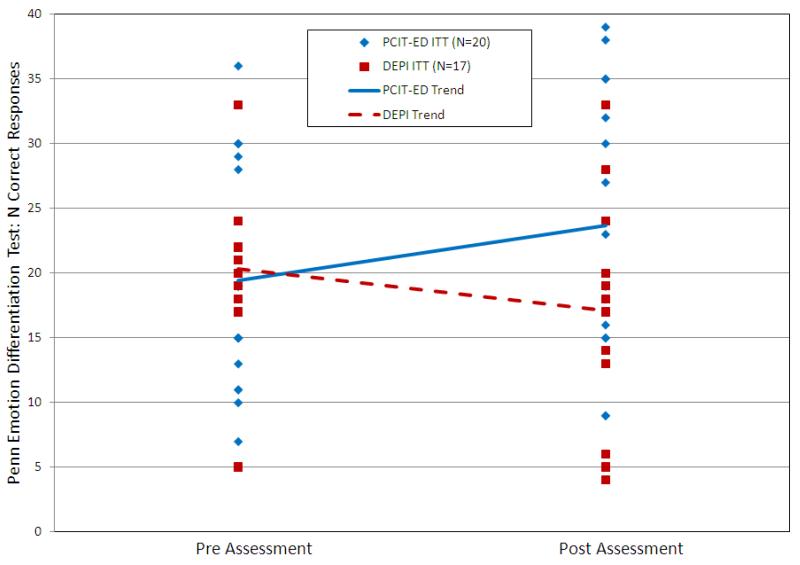
Emotion Development
Total number of correct responses on the KIDSEDF increased significantly in the PCIT-ED group and did not change significantly in the DEPI group (see Table 2), and there was a significant difference between the PCIT-ED and DEPI groups in both ITT (see Figure 3; F=11.86, df=1,34, p=0.002, ES=0.83) and completer analyses (F=9.82, df=1,21, p=0.005, ES=1.09). Both ERC subscale scores (lability/negativity and emotion regulation) improved significantly in the PCIT-ED group but not in the DEPI group (see Table 2). However, no significant differences in post scores between the PCIT-ED and DEPI groups were found.
Figure 3. Number of Correct Responses on the Penn Emotion Differentiation Test Post-Treatment in PCIT-ED and DEPI Intent-to-Treat Subjects.
Post-treatment number of correct responses on the Penn Emotion Differentiation Test was significantly different in the PCIT-ED and DEPI groups, controlling for number of correct responses at the pretreatment assessment (F=11.86, df=1,34, p=0.002, ES=0.83).
Executive Functioning
T scores on the BRIEF improved significantly in the PCIT-ED group only (see Table 2). Significant differences between the PCIT-ED and DEPI groups were found in post-treatment BRIEF inhibit + emotional control T scores in both ITT and completer analyses (see Figure 2).
Maternal Depression
Mothers’ BDI-II scores did not significantly change from pre- to post-treatment in the DEPI group but did improve significantly in the PCIT-ED group (see Table 2). No between group differences were found on post-treatment BDI-II score.
Parenting Stress
On average, both the PCIT-ED group and the DEPI group scored in the above normal range (>80th percentile) on the Child Domain scale at pre-treatment, indicating parental perception of child characteristics as contributing to overall parenting stress (see Table 2). Within group analyses indicate the PCIT-ED group demonstrated significant reductions in Total Stress, Child Domain, and Life Stress from pre- to post-treatment. The DEPI group did not show significant changes on any domain pre- to post-treatment, with scores on the Child Domain and Total Stress domain continuing to fall in the above normal range (see Table 2). Post-treatment PSI Total Stress, Child Domain, Parent Domain, and Life Stress percentiles were compared between the PCIT-ED and DEPI groups, with Child Domain, Parent Domain, and Total Stress percentiles differing significantly between the groups in the ITT analyses only (see Figure 2).
Discussion
To our knowledge, this pilot feasibility study is the first RCT of any form of treatment for depressed preschoolers. The absence of established effective treatments for depression in later childhood, and the increasing rates of antidepressant medications being prescribed to young children with unknown efficacy and safety, underscores the need to design and empirically test early psychotherapeutic interventions for depression. These data overall suggest that an RCT of early intervention in depression is feasible and that PCIT-ED is acceptable to families. This pilot study was preliminary and was not sufficiently powered to detect differences between treatment groups or to determine accurate effect sizes. However, it was promising that significant effects of PCIT-ED compared to the control condition were detected in specific areas of emotion recognition, child executive functioning and parenting stress. Additionally, significant improvements were found in several depressive and other symptom domains only in the PCIT-ED group. While these findings are intriguing, they must be viewed as preliminary and interpreted with caution, given the multiple limitations of this pilot study (Kraemer, Mintz, Noda, Tinklenberg, & Yesavage, 2006; Leon, Davis, & Kraemer, 2011). However, these findings in the context of the public health need for innovative early interventions for depression do suggest that further testing of this novel early intervention is now indicated using more optimal and adequately powered designs.
PCIT-ED families showed a much higher completion rate compared to the education control condition. This was notable because the sample was not seeking treatment for depression (as most depressed preschoolers are not referred) and was ascertained predominantly from community sites. Although drop-out rates in DEPI were high, after a design change in which DEPI parents were offered the PCIT-ED upon completion of DEPI, these rates decreased and were comparable to other active control conditions. DEPI was designed to account for contact with a mental health professional, duration of sessions, non-specific support, and education that overlapped with the content in PCIT-ED. Parents in DEPI also reported significant improvements in child outcomes although not as broadly as those who participated in PCIT-ED. The high drop-out rate in DEPI suggests that an individual control condition should be employed in future studies.
The between group differences found on measures of emotion recognition and executive functioning, if enduring in more adequately powered testing, suggests the possibility of unique and specific effects of PCIT-ED treatment in these domains of child functioning. Evidence for improvements in emotion recognition and regulation is of interest as this domain is a direct target of the ED module based on an emotion development model of early onset depression previously proposed (Luby & Belden, 2006). These positive changes post-treatment, in conjunction with amelioration of symptoms of depression arising from this very preliminary test, suggest that this developmental line may be worthy of further consideration and investigation as a target for interventions in depression.
The preliminary finding suggesting that maternal depressive symptoms were reduced in the PCIT-ED group is intriguing. If confirmed by further testing, this finding could represent evidence for a virtuous cycle (interventions targeting the child associated with maternal improvements) between child and mother as a result of early intervention for child depression. The reciprocal relationship between maternal depression and child maladjustment is well known (Goodman & Gotlib, 1999). Just as maternal depression is associated with increased child emotional and behavioral problems, a virtuous cycle, where improvements in child behavior are associated with improvements in maternal mood and parenting ability, may also be operational. Evidence for a virtuous cycle in which mothers’ recovery from depression was related to improved outcomes for child depression has been reported (Gunlicks & Weissman, 2008; Wickramaratne et al., 2011). These preliminary results suggest that there could be a potential benefit to maternal mood and parenting stress from the PCIT-ED intervention. Confirmation of this finding and investigations of the mechanism of effect is an important area for future study.
Small sample size is a limitation of the current study designed as a pilot feasibility study. Related to this, for the purposes of the pilot study, which was exploratory, we did not adjust alpha to account for multiple comparisons, which may contribute to Type I error. Differential attrition, common in RCTs involving education control conditions (Weisz, et al., 2006), was also a limitation. The attrition rate in the DEPI condition was reduced after dyads were offered PCIT-ED upon completion. The high drop-out rate in the group control condition suggests that an individual control condition should be employed in future testing to minimize drop out and to provide a better test of time and expectancy. The drop-out rate in the PCIT-ED group compares favorably to those found in clinical trials of standard PCIT (range 30-50%) (Fernandez, Butler, & Eyberg, 2011). The current report is based on parent report, which is also a common limitation in studies targeting young child psychopathology. However, observational data were obtained to measure emotional functioning in several domains, and will be presented once coded and analyzed.
Further investigations to determine whether earlier intervention in depression may provide a window of opportunity for more powerful treatment effects is of great interest. If the improvements suggested by this pilot study are confirmed in more rigorous testing, another question key to determining the value of this treatment more generally would be whether early treatment effects are enduring over time. Possible sources of the treatment effects suggested by these preliminary data, if confirmed by more adequately powered studies, could include the young age of the child and the use of the parent as the “arm of the therapist.” Future larger scale investigations of PCIT-ED are now needed to more definitely test efficacy, to generate more accurate effect sizes, and to inform moderators and mediators of treatment response. Such investigations, if fruitful, could be very important for efforts to enhance the efficacy of interventions for MDD in childhood and potentially across the lifespan.
Supplementary Material
Key points.
There has been little investigation of early interventions for childhood depression.
Early interventions for mental disorders during the preschool period appear very promising and some large effect sizes have been reported in some diagnostic domains.
Investigations of early interventions for depression during the preschool period are now warranted based on an emerging body of data validating depression onset as early as age 3 years.
An adaptation of a well validated treatment for preschool disruptive disorders, Parent Child Interaction Therapy (PCIT) entitled PCIT-Emotion Development appears feasible for further testing and may be promising for the early treatment of preschool depression.
Acknowledgments
Grant support is from the National Institute of Mental Health, grants 5R34MH080163-02 (Dr. Luby) and K23MH090245 (Dr. Lenze). Dr. Luby reports receiving royalties from Guilford Press for a book on Preschool Mental Health (2006).
Footnotes
Conflict of interest:
Dr. Lenze and Ms. Tillman have no interests to disclose.
Clinical trial registration information: Early Intervention in Depression Dyadic Emotion Development Therapy for Preschool Children, NCT00595283.
References
- Abidin R. The Parenting Stress Index professional manual. 3rd edn. Psychological Assessment Resources; Odessa, FL: 1995. [Google Scholar]
- Armstrong J, Goldstein L, the MacArthur Working Group on Outcome Assessment . Manual for the MacArthur Health and Behavior Questionnaire (HBQ 1.0). MacArthur Foundation Research Network on Psychopathology and Development (David J. Kupfer, Chair) University of Pittsburgh; Pittsburgh, PA: 2003. [Google Scholar]
- Beck A, Steer R, Brown G. Manual for Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Brinkmeyer M, Eyberg S. Parent-child interaction therapy for oppositional children. In: Kazdin AE, Weisz J, editors. Evidence-based psychotherapies for children and adolescents. Guilford Press; New York: 2003. pp. 204–223. [Google Scholar]
- Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology. 2008;20:775–803. doi: 10.1017/S0954579408000370. [DOI] [PubMed] [Google Scholar]
- Dietz LJ, Birmaher B, Williamson DE, Silk JS, Dahl RE, Axelson DA, Ehmann M, Ryan ND. Mother-child interactions in depressed children and children at high risk and low risk for future depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:574–582. doi: 10.1097/CHI.0b013e3181676595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger H, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Egger H, Ascher B, Angold A. Preschool Age Psychiatric Assessment (PAPA): Version 1.1. Center for Developmental Epidemiology, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center; Durham, NC: 1999. [Google Scholar]
- Egger H, Erkanli A, Keeler G, Potts E, Walter B, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Hughes CW, Carmody T, Rintelmann J. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Archives of General Psychiatry. 1997;54:1031–1037. doi: 10.1001/archpsyc.1997.01830230069010. [DOI] [PubMed] [Google Scholar]
- Eyberg SM. Parent-child interaction therapy: Treatment integrity checklists. Psychological Assessment Resources; Odessa, FL: 1999. [Google Scholar]
- Fernandez MA, Butler AM, Eyberg SM. Treatment outcome for low socioeconomic status African American families in parent-child interaction therapy: A pilot study. Child & Family Behavior Therapy. 2011;33:32–48. [Google Scholar]
- Gaffrey MS, Luby JL, Repovs G, Belden AC, Botteron KN, Luking KR, Barch DM. Subgenual cingulate connectivity in children with a history of preschool-depression. Neuroreport. 2010;21:1182–1188. doi: 10.1097/WNR.0b013e32834127eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia G, Espy K, Isquith P. Behavior Rating Inventory of Executive Function-Preschool Version (BRIEF-P) Psychological Assessment Resources; Lutz, FL: 2003. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gunlicks ML, Weissman MM. Change in child psychopathology with improvement in parental depression: A systematic review. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:379–389. doi: 10.1097/CHI.0b013e3181640805. [DOI] [PubMed] [Google Scholar]
- Gur RC, Ragland JD, Moberg PJ, Turner TH, Bilker WB, Kohler C, Siegel SJ, Gur RE. Computerized neurocognitive scanning: I. Methodology and validation in healthy people. Neuropsychopharmacology. 2001;25:766–776. doi: 10.1016/S0893-133X(01)00278-0. [DOI] [PubMed] [Google Scholar]
- Gur RC, Richard J, Hughett P, Calkins ME, Macy L, Bilker WB, Brensinger C, Gur RE. A cognitive neuroscience-based computerized battery for efficient measurement of individual differences: Standardization and initial construct validation. Journal of Neuroscience Methods. 2010;187:254–262. doi: 10.1016/j.jneumeth.2009.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges K. The Preschool and Early Childhood Functional Assessment Scale (PECFAS) Eastern Michigan University; Ypsilanti, MI: 1994. [Google Scholar]
- Hood KK, Eyberg SM. Outcomes of parent-child interaction therapy: Mothers’ reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology. 2003;32:419–429. doi: 10.1207/S15374424JCCP3203_10. [DOI] [PubMed] [Google Scholar]
- Hyman SE. Can neuroscience be integrated into the DSM-V? Nature Reviews Neuroscience. 2007;8:725–732. doi: 10.1038/nrn2218. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Isquith PK, Crawford JS, Espy KA, Gioia GA. Assessment of executive function in preschool-aged children. Mental Retardation and Developmental Disabilities Research Reviews. 2005;11:209–215. doi: 10.1002/mrdd.20075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child and Adolescent Psychology. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- Lenze S, Pautsch J, Luby J. Parent-child interaction therapy emotion development: A novel treatment for depression in preschool children. Depression and Anxiety. 2011;28:153–159. doi: 10.1002/da.20770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon A, Davis L, Kraemer H. The role and interpretation of pilot studies in clinical research. Journal of Psychiatric Research. 2011;45:626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby J. Early childhood depression. American Journal of Psychiatry. 2009;166:974–979. doi: 10.1176/appi.ajp.2009.08111709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby J, Belden AC. Mood disorders and an emotional reactivity model of depression. In: Luby J, editor. Handbook of Preschool Mental Health: Development, disorders, and treatment. Guilford Press; New York: 2006. pp. 209–230. [Google Scholar]
- Luby J, Botteron K, Barch D. Longitudinal assessment of brain change in depressed preschoolers. unpublished data. [Google Scholar]
- Luby J, Heffelfinger A, Koenig-McNaught AL, Brown K, Spitznagel E. ThePreschool Feelings Checklist: A brief and sensitive screening measure for depression in young children. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:708–717. doi: 10.1097/01.chi.0000121066.29744.08. [DOI] [PubMed] [Google Scholar]
- Luby J, Heffelfinger A, Mrakotsky C, Brown K, Hessler M, Wallis J, Spitznagel E. The clinical picture of depression in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:340–348. doi: 10.1097/00004583-200303000-00015. [DOI] [PubMed] [Google Scholar]
- Luby J, Heffelfinger A, Mrakrotsky C, Hessler M, Brown K, Hildebrand T. Preschool major depressive disorder: Preliminary validation for developmentally modified DSM-IV criteria. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:928–937. doi: 10.1097/00004583-200208000-00011. [DOI] [PubMed] [Google Scholar]
- Luby J, Mrakotsky C, Heffelfinger A, Brown K, Spitznagel E. Characteristics of depressed preschoolers with and without anhedonia: Evidence for a melancholic depressive subtype in young children. American Journal of Psychiatry. 2004;161:1998–2004. doi: 10.1176/appi.ajp.161.11.1998. [DOI] [PubMed] [Google Scholar]
- Luby J, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: Homotypic continuity and course over 24 months. Archives of General Psychiatry. 2009;66:897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mufson L, Dorta KP, Moreau D, Weissman MM. Interpersonal psychotherapy for depressed adolescents. 2nd edn. Guilford; New York: 2004. [Google Scholar]
- Murphy MJ, Ramirez A, Anaya Y, Nowlin C, Jellinek MS. Validation of the preschool and early childhood functional assessment. Journal of Child and Family Studies. 1999;8:343–356. doi: 10.1023/A:1022071430660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields A, Cicchetti D. Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology. 1997;33:906–916. doi: 10.1037//0012-1649.33.6.906. [DOI] [PubMed] [Google Scholar]
- Stalets MM, Pautsch J, McGrath M, Luby J. Parent-child interaction therapy-emotion development. Washington University School of Medicine; unpublished manual. [Google Scholar]
- Thomas R, Zimmer-Gembeck MJ. Behavioral outcomes of Parent-Child Interaction Therapy and Triple P-Positive Parenting Program: a review and meta-analysis. Journal of Abnormal Child Psychology. 2007;35:475–495. doi: 10.1007/s10802-007-9104-9. [DOI] [PubMed] [Google Scholar]
- Wagner KD. Pharmacotherapy for major depression in children and adolescents. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2005;29:819–826. doi: 10.1016/j.pnpbp.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology. 1997;65:93–109. doi: 10.1037//0022-006x.65.1.93. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ, Hammond M. Treating children with early-onset conduct problems: Intervention outcomes for parent, child, and teacher training. Journal of Clinical Child and Adolescent Psychology. 2004;33:105–124. doi: 10.1207/S15374424JCCP3301_11. [DOI] [PubMed] [Google Scholar]
- Weisz J, McCarty C, Valeri S. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichstrom L. The Trondheim Early Secure Study (TESS): Prevalance of MDD among 4-year olds in Norway. unpublished data. [Google Scholar]
- Wickramaratne P, Gameroff MJ, Pilowsky DJ, Hughes CW, Garber J, Malloy E, King C, Cerda G, Sood AB, Alpert JE, Trivedi MH, Fava M, Rush AJ, Wisniewski S, Weissman MM. Children of depressed mothers 1 year after remission of maternal depression: Findings from the STAR*D-Child Study. The American Journal of Psychiatry. 2011;168:1–10. doi: 10.1176/appi.ajp.2010.10010032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelazo PD, Muller U, Frye D, Marcovitch S. The development of executive functioning in early childhood. Monographs of the Society for Research in Child Development. 2003;68:vii–137. doi: 10.1111/j.0037-976x.2003.00260.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.