Abstract
Summary
A rib fracture history after age 45 was associated with a 5.4-fold increase in new rib fracture risk and a 2.4-fold increase in risk of any new clinical fracture in 155,031 postmenopausal women. A rib fracture history suggests osteoporosis and should be considered when evaluating patients for interventions to prevent fractures.
Introduction
Until recently, little attention was paid to rib fracture as an osteoporosis marker. Emerging evidence suggests rib fracture may be an osteoporotic fracture in men and women. We report the 5-year independent association between baseline rib fracture histories and self-reported future fractures by age (decade) in the NORA cohort (155,031 postmenopausal women, 50–99 years).
Methods
Participants reported fracture history and responded to follow-up surveys at years 1, 3, or 6. Women with a baseline rib fracture history without other fractures were compared with women with no fracture.
Results
At baseline, 4,758 (3.07%) women reported a rib fracture history without other fractures; 6,300 women reported 6,830 new clinical fractures, including wrist (2,271), rib (1,891), spine (1,136), hip (941), and forearm (591). Adjusted relative risk (ARR) values (95% confidence interval [CI]) for future fractures in women with rib fracture history versus women with no fracture history were 5.4 (4.8–6.1) at the rib, 2.1 (1.7–2.6) at the spine, and 1.4 (1.1–1.7) at the wrist, and not significant for forearm or hip fractures. Future fracture risk was at least doubled in women with a rib fracture history in all ages: ARR (95% CI) 3.4 (2.8–4.0) for ages 50–59, 2.5 (2.1–3.0) for ages 60–69, 2.0 (1.7–2.3) for ages 70–79, and 2.0 (1.6–2.6) for ages >80.
Conclusions
Rib fracture, the second most common clinical fracture in women (after wrist fracture), predicted future fractures of the rib, wrist, and spine at all ages. Women presenting with rib fractures should be evaluated for appropriate management to prevent future fractures.
Keywords: Aging, Fracture, Menopause, Osteoporosis, Population studies
Introduction
The clinical consequence of osteoporosis or low bone mass is fracture. A 50-year-old woman has a 40% chance of experiencing an osteoporosis-associated fracture in her lifetime [1]. It is well known that prior fractures greatly increase the risk of future fractures [2–8]. The consistent association between hip, spine, and wrist fracture history and increased future fracture risk led to the inclusion of prior fracture as a clinical risk factor in the revised Clinician’s Guide [9, 10] of the National Osteoporosis Foundation (NOF) (a U.S. consumer and community-focused health organization dedicated to prevention of osteoporosis and broken bones, promotion of strong bones, and reduction of human suffering through programs of public and clinician awareness, education, advocacy, and research).
In the European Prospective Osteoporosis Study (EPOS), a history of rib fracture approximately doubled the 3-year risk for any limb fracture in women ≥50 years [11]. In the 5-year prospective Osteoporotic Fractures in Men Study (MrOS) of ambulatory, community-dwelling men ≥65 years, a history of rib fracture was strongly associated with low bone mineral density (BMD) and future fractures [12].
The purpose of the present study was to examine the association between a history of rib fracture after age 45 and the 5-year risk of fracture (hip, spine, rib, wrist, or forearm) in the National Osteoporosis Risk Assessment (NORA) study of community-dwelling postmenopausal women aged 50–99 years, and the large size of the cohort (155,031 women) allowed us to study future fracture risk by decade of age.
Methods
The study cohort
The NORA study began in 1997 as a longitudinal observational analysis of osteoporosis among postmenopausal women in the United States. As previously reported [13, 14], postmenopausal women were eligible for enrollment in NORA if they were age ≥50 years and did not report an osteoporosis diagnosis, bone-specific medication use, or a bone density measurement within the preceding 12 months. Current estrogen therapy did not preclude participation.
The 200,160 women were recruited through the offices of 4,236 primary care physicians whose practices were located in 34 states and the District of Columbia and included large numbers of postmenopausal women [13]. Each office provided a randomly chosen list of up to 300 eligible women, who received letters of invitation from their physicians to participate in NORA. Between 40 and 100 women in each practice agreed to enroll and gave written informed consent.
Baseline BMD measurement at one of three skeletal sites (heel, forearm, or finger) was performed in each woman’s primary care physician’s office by NORA field personnel. Slightly more than half the women had a heel measurement by single energy X-ray absorptiometry (SXA), and approximately one-third had peripheral DEXA (pDEXA) of the forearm. The remaining women had heel ultrasound or finger pDEXA measurements. Participants completed a baseline questionnaire assessing demographics, personal and family history of fracture, estrogen therapy, and health behaviors (smoking, alcohol and caffeine consumption, and physical activity). All study protocols and consent documents were approved by a national institutional review board, The Essex IRB.
Participants were contacted by mail or telephone for three follow-up surveys over the next 6 years. Each survey collected information on new fractures, BMD measurements, current use of estrogen and osteoporosis-specific prescription medications, dietary supplements, falls, health behaviors, and health status. The first follow-up year 1 survey (Y1) was conducted approximately 12 months after enrollment (median=13.3 months) with an 81.9% response rate. Approximately 3 years after enrollment (median= 37.3 months), the year 3 survey (Y3) achieved an 80.6% response rate. The final year 6 survey (Y6) was conducted approximately 6 years after enrollment (median = 69.4 months) with a response rate of 78.8%.
Baseline risk factors
At enrollment, each participant completed mailed questionnaires that provided information on the presence or absence of risk factors for low BMD and fractures, including race/ethnicity, years of formal education, self-rated health (excellent to poor), body weight, height, personal and family history of fracture, medication use (corticosteroid, estrogen), lifestyle (cigarette smoking, alcohol use, regular exercise), and age at menopause. Body mass index (BMI) was calculated from self-reported height and weight. History of rib fracture was queried by asking, “Since the age of 45, have you broken any of the following bones: hip, rib, wrist, spine (backbone)?” Each fracture history question had a yes/no answer.
Study population
All women who reported their baseline history of fracture after age 45 (yes or no), and who responded to one or more (Y1 or Y3 or Y6) follow-up surveys were eligible for this analysis. Incident fractures were queried at each survey: “Since joining NORA/January 2000, have you broken or fractured: hip, spine/vertebra, rib, wrist, forearm, ankle, other bone?” Only ankle fractures were not assessed in Y1. The time to first fracture or the censoring time varied depending on whether women responded to one or more surveys.
Statistical analysis
The absolute risk of future fracture was calculated as new fracture rates per 1,000 women-years. In addition, the percentage of women experiencing a fracture during the follow-up period was calculated. Both percentage and rate of fracture are important in their own perspective to understand the issues of risk (suggesting etiology) and percent (with population-based health burden implications). χ2 and t-test statistics were used to compare characteristics between group with only rib fracture history and group with no fracture history at any site. The analysis of the association between rib fracture history and future fracture by fracture site was stratified by decade of age (50–59, 60–69, 70–79, 80+ years). Due to the large sample size, very small but statistically significant differences were observed; to avoid overinterpretation of statistically significant small associations, in this paper we report associations significant at the P<0.0001 level.
Multivariate analysis was performed to assess the association between baseline rib fracture history and future fractures stratified by decade of age group. The Cox model was developed for all future fractures combined. Relative risk (RR; 95% confidence interval [CI]) values adjusted for covariates were estimated from the Cox model using the time from baseline to the time of first new fracture. If no fractures occurred during follow-up, time (observed time) from baseline to the last survey response (Y1, Y3, or Y6 follow-up survey) was used as the censoring time. Fifteen potential covariates were considered (age, BMD T-score, ethnicity, education, self-rated health status, maternal or family history of fracture, estrogen use, body weight, current corticosteroid use, smoking status, menopause before age 40 years, thyroid medication use, BMI, exercise, and alcohol use). The final Cox model with stepwise selection criteria set at P<0.05 entry included all variables except thyroid medication use, BMI, and physical exercise. An interaction term between age group and rib fracture history was used to determine whether the association between rib fracture history and future fracture varied by age group. The osteoporotic fracture (any fracture) included hip, spine, wrist, rib, and forearm fractures.
Results
A total of 170,086 women had information at baseline and completed the Y1, Y3, or Y6 follow-up surveys. From these were derived a cohort of 4,758 women with a baseline history of rib fracture in the absence of other fractures, and a comparison group of 150,273 women with no baseline history of fracture at any site (Fig. 1).
Fig. 1.
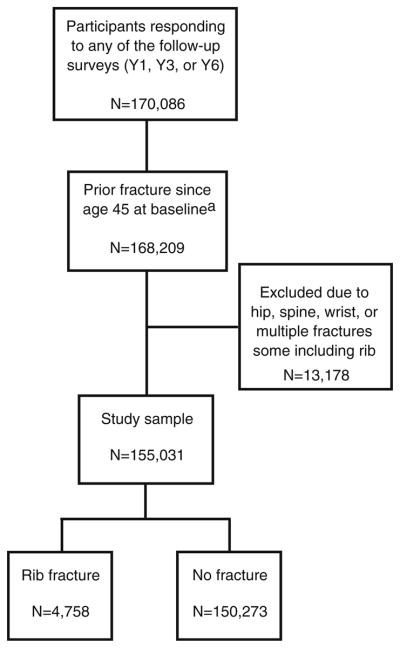
Flowchart showing the selection of study sample of women with either a history of rib fracture or history of no fracture since age 45. aRespondents were asked “Since age 45 have you broken any of the following bones: hip, rib, wrist, spine (backbone)?”
An analysis comparing baseline demographics and clinical characteristics of respondents with non-respondents showed that non-respondents to the Y6 survey were more likely to be older, Asian or Hispanic, and less likely to have received higher education. Non-respondents were also more likely to weigh less than 127 lb (58 kg), report worse self-rated health, be cigarette smokers, have rheumatoid arthritis, and have lower peripheral BMD (T-score ≤ −2.5 or between −1.0 and −2.49). The clinical characteristics of respondents versus non-respondents to the Y1 and Y3 surveys were similar to that of the Y6 survey and were reported in previous NORA publications [15].
Table 1 shows baseline demographics, medical history, lifestyle behaviors, and BMD T-score distribution of women with rib fracture history compared to women with no fracture history, by age group. Among women ages 50–79 years, those with a rib fracture history were slightly older, had a lower BMD T-score, and were more likely to have fair/poor health status, a family history of fracture, premature menopause (<40 years), and weigh <127 lbs (58 kg). Only in the oldest group (>80 years) did the mean (SD) T-score not differ between women with rib fractures and women with no fracture history [−1.9 (1.0) vs. −1.7 (1.1)]. We found no statistical association between rib fracture history and physical activity (Table 1).
Table 1.
Characteristics of women with and without a rib fracture history, by age group
| Characteristics | Age group (years)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 50–59 (N=59,227)
|
60–69 (N=54,175)
|
70–79 (N=34,585)
|
80+ (N=7,044)
|
|||||
| Rib fracture Hx | No fracture Hx | Rib fracture Hx | No fracture Hx | Rib fracture Hx | No fracture Hx | Rib fracture Hx | No fracture Hx | |
| N (%) | 1,092 (1.8) | 58,135 (98.2) | 1,588 (2.9) | 52,587 (97.1) | 1,589 (4.6) | 32,996 (95.4) | 489 (6.9) | 6,555 (93.1) |
| Follow-up time (months) | 47.2 | 47.6 | 44.0 | 46.6 | 41.0 | 43.2 | 34.8 | 36.3 |
| Age: mean (SD) (years) | 55.2a (2.6) | 54.7 (2.8) | 64.9a (2.9) | 64.4 (2.9) | 74.0a (2.8) | 73.7 (2.7) | 83.1 (2.8) | 83.0 (2.9) |
| T-score: mean (SD) | −0.7a (1.0) | −0.4 (1.0) | −1.1a (1.0) | −0.8 (1.1) | −1.6a (1.0) | −1.3 (1.0) | −1.9 (1.0) | −1.7 (1.1) |
| Race (%) | ||||||||
| Caucasian | 94.7 | 90.8 | 93.5 | 90.9 | 92.9 | 90.6 | 92.2 | 89.5 |
| Education (%) | ||||||||
| College or more | 48.6 | 51.4 | 39.7 | 38.8 | 38.1a | 34.5 | 38.9a | 34.4 |
| Health status (%) | ||||||||
| Excellent/very good | 30.1 | 50.8 | 38.7 | 36.4 | 33.7 | 39.2 | 37.2 | 39.2 |
| Good | 33.4 | 35.0 | 39.0 | 38.8 | 41.2 | 42.8 | 40.7 | 40.0 |
| Fair/poor | 25.6a | 13.5 | 21.4a | 14.0 | 23.9a | 16.7 | 20.5 | 19.3 |
| Estrogen use (%) | ||||||||
| Never | 22.3 | 24.2 | 30.7 | 31.7 | 39.8 | 42.5 | 49.9 | 52.6 |
| Former | 15.1 | 13.6 | 21.9a | 17.8 | 28.1a | 22.8 | 28.8 | 24.4 |
| Current | 61.5 | 60.8 | 45.2 | 48.5 | 29.5 | 31.5 | 17.6 | 18.5 |
| Cigarette smoking (%) | ||||||||
| Never | 38.8 | 49.8 | 45.8 | 52.1 | 54.7 | 58.3 | 65.6 | 65.1 |
| Former | 37.1 | 35.2 | 39.0 | 36.7 | 36.7a | 33.9 | 29.2 | 30.2 |
| Current | 22.8a | 14.1 | 14.0a | 10.1 | 7.7 | 6.2 | 2.5 | 2.4 |
| Family fracture history (%) | 32.0a | 22.2 | 31.4a | 23.7 | 28.3a | 20.3 | 21.5a | 16.3 |
| Thyroid medication Use (%) | 17.9a | 15.1 | 21.0a | 18.4 | 22.4 | 21.1 | 21.9 | 21.6 |
| Alcohol use, drinks/week (%) | ||||||||
| None | 70.3 | 69.8 | 73.2 | 72.1 | 74.0 | 74.6 | 76.3 | 76.4 |
| <7 drinks | 18.3 | 20.8 | 15.2 | 17.3 | 13.5 | 14.5 | 12.9 | 13.4 |
| 7+ drinks | 9.3a | 7.5 | 9.6 | 8.4 | 8.7 | 8.0 | 6.3 | 5.9 |
| Menopause age <40 years | 30.5a | 20.3 | 22.0a | 17.1 | 17.3a | 11.9 | 13.9a | 9.0 |
| Regular exercise 0–2 vs. 3+ times/week (%) | 54.3 | 54.3 | 47.5 | 47.4 | 45.4 | 43.6 | 44.6 | 44.7 |
| Weight <127 lb (%) | 15.4a | 12.5 | 15.7a | 12.5 | 19.7a | 17.6 | 29.2 | 29.4 |
| Low BMI (%) | 2.4a | 0.9 | 1.8 | 1.3 | 3.1a | 1.9 | 3.5 | 2.9 |
| Cortisone use | 3.5a | 1.7 | 3.1a | 2.0 | 2.8 | 2.5 | 3.5 | 3.0 |
Percentages are column percentages and may not add up to 100 due to missing/unknown data
P<0.0001 for rib fracture history versus no fracture history
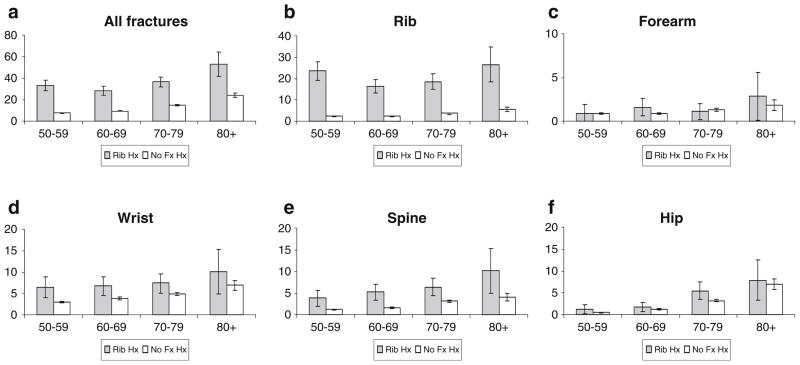
A total of 6,300 women reported 6,830 new fractures, including 2,271 wrist fractures, 1,891 rib fractures, 1,136 clinical spinal fractures, 941 hip fractures, and 591 forearm fractures. Rib fractures were second to wrist fractures as the most common clinical fracture for all age groups up to age 80 (Table 2). Figure 2 displays site-specific future fracture rates per 1,000 women-years by age category and by rib fracture history versus no fracture history. Future fracture rates were highest in oldest women (Fig. 2) but more than half of the women who reported new fractures were less than 70 years of age at baseline, reflecting the age distribution of the cohort (Table 2).
Table 2.
Number and the percent of women with future fracture by site, rib fracture history, and age group
| Future fracture site | Age group (years)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 50–59 (N=59,227)
|
60–69 (N=54,175)
|
70–79 (N=34,585)
|
80+ (N=7,044)
|
|||||
| Rib fracture Hx | No fracture Hx | Rib fracture Hx | No fracture Hx | Rib fracture Hx | No fracture Hx | Rib fracture Hx | No fracture Hx | |
| N (%) | 1,092 (1.8) | 58,135 (98.2) | 1,588 (2.9) | 52,587 (97.1) | 1,589 (4.6) | 32,996 (95.4) | 489 (6.9) | 6,555 (93.1) |
| Rib | 95 (8.7) | 555 (1.0) | 91 (5.7) | 483 (0.9) | 97 (6.1) | 428 (1.3) | 36 (7.4) | 106 (1.6) |
| Hip | 5 (0.5) | 117 (0.2) | 10 (0.6) | 260 (0.5) | 29 (1.8) | 373 (1.1) | 11 (2.3) | 136 (2.1) |
| Spine | 16 (1.5) | 270 (0.5) | 30 (1.9) | 327 (0.6) | 34 (2.1) | 365 (1.1) | 14 (2.9) | 80 (1.2) |
| Wrist | 27 (2.5) | 681 (1.2) | 38 (2.4) | 766 (1.5) | 39 (2.5) | 572 (1.7) | 14 (2.9) | 134 (2.0) |
| Forearm | 4 (0.4) | 202 (0.4) | 9 (0.6) | 183 (0.4) | 6 (0.4) | 148 (0.5) | 4 (0.8) | 35 (0.5) |
| Any fracturea | 132 (12.1) | 1,714 (3.0) | 154(9.7) | 1,863 (3.5) | 184 (11.6) | 1,731 (5.3) | 69 (14.1) | 453 (6.9) |
Any fracture patients with at least one or more osteoporotic fractures (rib, hip, spine, wrist, or forearm)
Fig. 2.
Future fracture rates per 1,000 women-years for each fracture site during follow-up, by age group and fracture history (rib fracture vs. no fracture) (a all fractures, b rib, c forearm, d wrist, e spine, f hip). Error bars represent 95% confidence intervals
Table 3 presents age group-specific unadjusted and adjusted hazard ratios for future fractures among women with a rib fracture history compared to those with no fracture history. The unadjusted relative risk estimates were higher than adjusted estimates. The adjusted relative risk of future rib fracture within 5 years among women with a rib fracture history (vs. no-fracture history) was high across all age groups (RR, 4.3 for ages 70–79 years to 7.2 for ages 50–59 years). Overall, women with a rib fracture history were 4 to 7 times more likely to have another rib fracture within the next 5 years.
Table 3.
Unadjusted and adjusteda relative risk estimates with their 95% confidence interval (CI) for future fracture by site in women with rib fracture history 0compared to no fracture history
| Future fx site | Relative risk (95% CI) for future fracture by specific future fracture site
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rib
|
Hip
|
Spine
|
Wrist
|
Forearm
|
Any fracture
|
|||||||
| Age group (years) | Unadj | Adj | Unadj | Adj | Unadj | Adj | Unadj | Adj | Unadj | Adj | Unadj | Adj |
| 50–59 (N=59,227) | 9.7 (7.8–12.1) | 7.2 (5.8–9.0) | 2.3 (0.9–5.6) | 1.6 (0.7–4.0) | 3.2 (1.9–5.3) | 2.3 (1.4–3.9) | 2.1 (1.5–3.2) | 1.7 (1.1–2.4) | 1.1 (0.4–2.9) | 0.9 (0.3–2.4) | 4.4 (3.7–5.3) | 3.4 (2.8–4.0) |
| 60–69 (N=54,175) | 6.9 (5.5–8.7) | 5.5 (4.4–6.9) | 1.4 (0.7–2.6) | 1.0 (0.6–1.9) | 3.3 (2.3–4.8) | 2.6 (1.8–3.8) | 1.8 (1.3–2.4) | 1.4 (1.03–2.0) | 1.7 (0.9–3.4) | 1.5 (0.8–2.9) | 3.1 (2.6–3.6) | 2.5 (2.1–3.0) |
| 70–79 (N=34,585) | 5.1 (4.1–6.4) | 4.3 (3.4–5.3) | 1.7 (1.2–2.5) | 1.4 (0.9–2.0) | 2.1 (1.5–3.0) | 1.7 (1.2–2.4) | 1.5 (1.1–2.1) | 1.2 (0.9–1.7) | 0.9 (0.4–2.0) | 0.8 (0.3–1.7) | 2.4 (2.1–2.8) | 2.0 (1.7–2.3) |
| 80+ (N=7,044) | 5.0 (3.4–7.2) | 4.5 (3.1–6.6) | 1.1 (0.6–2.1) | 1.0 (0.6–1.9) | 2.5 (1.4–4.4) | 2.2 (1.3–3.9) | 1.5 (0.9–2.6) | 1.3 (0.7–2.3) | 1.6 (0.6–4.5) | 1.5 (0.5–4.1) | 2.2 (1.7–2.9) | 2.0 (1.6–2.6) |
| Overallb | 7.2 (6.4–8.1) | 5.4 (4.8–6.1) | 2.1 (1.6–2.8) | 1.2 (0.9–1.6) | 3.1 (2.5–3.9) | 2.1 (1.7–2.6) | 1.9 (1.6–2.3) | 1.4 (1.1–1.7) | 1.4 (0.9–1.7) | 1.1 (0.7–1.8) | 3.4 (3.1–3.7) | 2.4 (2.2–2.6) |
Adjusted for BMD T-score, ethnicity, education, self-rated health status, maternal or family history of fracture, estrogen use, body weight, current corticosteroid use, smoking status, menopause before age 40 years, and alcohol use
Adjusted variables included age plus the covariates listed above
The adjusted relative risk of future clinical spine fracture within 5 years among women with a rib fracture history (vs. no-fracture history) was at least 2-fold (RR, 1.7 for ages 70–79 years to 2.6 for ages 60–69 years). The adjusted relative risk for future wrist fracture after a baseline rib fracture was significantly higher among women 50–59 years (RR, 1.7; 95% CI, 1.1–2.4) and 60–69 years (RR, 1.4; 95% CI, 1.03–2.0). A history of rib fracture was not independently associated with future forearm fracture or hip fracture in any age group.
Discussion
In this prospective study of 155,031 postmenopausal women from the NORA cohort, a history of rib fracture after age 45 was associated with 5.4-fold increase in risk of a new rib fracture and a 2.1-fold increased risk for a future clinical fracture of the spine. Rib fracture predicted an increased risk of wrist fracture in women aged 50–70 years but not older and was not predictive of future fracture at the hip or forearm in any age group. The absence of an association between rib fracture and subsequent hip fracture in NORA may reflect the low incidence of hip fracture in younger women (0.8 per 1,000 person-years for hip in NORA women 50–64 years [16]) or that women were more likely to be lost to follow-up after a hip fracture.
These results for NORA are similar to those of an analysis of limb fractures in 5,995 women ≥50 years in EPOS [11]. In EPOS, women with a self-reported history of low-trauma rib fracture had an increased risk of sustaining any limb fracture (relative hazard [RH] 2.0). The results of these two cohort studies differ in that in EPOS, but not in NORA, a history of rib fracture increased the risk of future fracture of the hip (RH 5.5). Also, in NORA but not in EPOS, the risk of future fracture of the wrist (Colles’ fracture) after rib fracture was significantly increased in postmenopausal women younger than 70. The analysis of EPOS did not report future fractures of the rib, which in NORA were the most frequent incident fractures in women with a history of rib fracture.
Rib fracture was the most common incident fracture in women without a history of rib fracture in NORA (Table 2), but this was not the case in other studies of postmenopausal women [17]. It is possible that the differences in incidence rank order, and differences between NORA and EPOS in the associations between prior rib fracture and subsequent fractures of the hip and wrist, reflect methodological differences in the ascertainment of fractures.
Some limitations of the NORA study are that fractures were based on self-report, and the authors were unable to confirm that each fracture was due to osteoporosis; neither a history of rib fracture nor report of incident fractures was validated by radiography or medical record review. Thus there is potential for bias, but it is difficult to know the direction or the extent of the bias without knowing the numbers of false-positive self-reports or under-reporting. Nevertheless, based on the epidemiology of osteoporotic fractures [23], it is likely that the vast majority of fractures in this cohort of postmenopausal women were associated with low BMD, even if they occurred as a result of major trauma. A potential systematic recall bias, in which patients who reported rib fractures at baseline also reported them at follow up [11], could have exaggerated the strength of the association between prior and future rib fractures.
Studies of the validity of elderly women’s self-reported fractures indicate that this method is relatively accurate for fractures of the wrist, hip, and humerus, but less accurate for fractures of the rib [18–20]. In the (AGES)-Reykjavik study, rib fractures in elderly women had the lowest concurrence between self-report and record in a fracture registry—kappa value 0.25 for rib fracture, versus 0.82 for fracture of the forearm, and 0.78 for fractures of the hip, femoral shaft, or pelvis [21]. Nevitt et al. [18] reported that 23% of rib fractures identified through self-report were false positives. It seems equally plausible that rib fractures are underestimated because they usually heal spontaneously without medical attention. Under-reporting of other fractures (false negatives) may be less common, with the EPOS study showing that only 7% and 3% did not recall a hip or distal forearm fracture, respectively [19].
Nevertheless, NORA results are very similar to MrOS results in men, although only the latter validated new rib (and all other) fractures by radiology reports [12]; in MrOS men a validated rib fracture was the most common incident clinical fracture, and a history of rib/chest fracture was an independent risk factor for incident fractures of the rib (HR 2.71), wrist (HR 2.06), and hip (HR 2.05).
Variation in response rates by age may also have affected the observed rates of fractures. The duration of follow up (average 45.7 months) was similar for all age groups except for women who were more than 80 years of age at baseline (who had an average follow-up of 36 months). The shorter follow up likely reflects frailty or mortality. This truncation of those at highest fracture risk would be expected to lead to underestimation of the true fracture incidence in the elderly.
In NORA, women with a rib fracture history had a lower baseline BMD T-score (Table 1). This finding is consistent with the thesis that a rib fracture is a marker for low bone mass in postmenopausal women, and therefore likely to predict future fractures [11, 22]. Current NOF guidelines identify a prior fracture of the hip or spine as a sufficiently important clinical risk factor for future fractures that pharmacologic therapy is recommended irrespective of the patient’s BMD T-score [10]. These data from NORA and from EPOS [11] point to a history of rib fracture as a marker of bone fragility in postmenopausal women and suggest that this history should also be considered when evaluating patients for an intervention to prevent future fractures. In conclusion, in this analysis of 155,031 postmenopausal women, a self-reported history of rib fracture after age 45 was independently associated with 5.4-fold increase in risk of a new rib fracture and a 2.4-fold increase in risk of any new clinical fracture. Overall associations were observed in all age groups. A history of rib fractures is suggestive of osteoporosis and should be considered when evaluating patients for interventions to prevent fracture.
Acknowledgments
We thank Julia Vishnevetsky, in collaboration with SCRIBCO, for providing editorial/medical writing assistance.
Dr. Barrett-Connor has received grant support from NIH (National Institutes of Health/National Institute on Aging grants AG07181 and AG028507 and the National Institute of Diabetes and Digestive and Kidney Diseases, grant DK31801) and from The Osteoporotic Fractures in Men (MrOS) Study, supported by National Institutes of Health funding [National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140]. In addition, she has received research support from the following: Merck & Co., Arena Pharmaceuticals, Roche, and Pfizer. She served as a paid member of the steering committee and as the lead epidemiologist for NORA.
Paul D. Miller has received grant support from Roche Pharmaceuticals, Eli Lilly, Merck & Co., Novartis Pharmaceuticals, and Amgen. He has served as a consultant and on advisory and speaker boards for Amgen, Novartis Pharmaceuticals, and Genetech. He served as a member of the steering committee for NORA.
Ethel Siris has been a consultant for Amgen, Eli Lilly, Merck, Novartis, and Pfizer, and on the Speaker’s Bureau for Amgen and Eli Lilly. She served as a member of the steering committee for NORA.
Footnotes
Conflicts of interest Drs. McHorney, Sen, and Sajjan are employees of Merck & Co., Inc.
Contributor Information
S. G. Sajjan, Email: shiva_sajjan@merck.com, Merck & Co., Inc., West Point, PA, USA
E. Barrett-Connor, Email: ebarrettconnor@ucsd.edu, University of California San Diego, La Jolla, CA, USA. Department of Family and Preventive Medicine, University of California San Diego, 9500 Gilman Drive, La Jolla, CA 92093-0607, USA
C. A. McHorney, Email: colleen_mchorney@merck.com, Merck & Co., Inc., North Wales, PA, USA
P. D. Miller, Email: millerccbr@aol.com, Colorado Center for Bone Research, Lakewood, CO, USA
S. S. Sen, Email: shuvayu_sen@merck.com, Merck & Co. Inc., Whitehouse Station, NJ, USA
E. Siris, Email: es27@columbia.edu, Columbia University College of Physicians and Surgeons, New York, NY, USA
References
- 1.Melton LJ, 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective. How many women have osteoporosis? J Bone Miner Res. 1992;7:1005–1010. doi: 10.1002/jbmr.5650070902. [DOI] [PubMed] [Google Scholar]
- 2.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 3.Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–382. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 4.Porthouse J, Birks YF, Torgerson DJ, Cockayne S, Puffer S, Watt I. Risk factors for fracture in a UK population: a prospective cohort study. Q J Med. 2004;97:569–574. doi: 10.1093/qjmed/hch097. [DOI] [PubMed] [Google Scholar]
- 5.Mallmin H, Ljunghall S, Persson I, Naessen T, Krusemo UB, Bergstrom R. Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int. 1993;52:269–272. doi: 10.1007/BF00296650. [DOI] [PubMed] [Google Scholar]
- 6.Cuddihy MT, Gabriel SE, Crowson CS, O’Fallon WM, Melton LJ., 3rd Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int. 1999;9:469–475. doi: 10.1007/s001980050172. [DOI] [PubMed] [Google Scholar]
- 7.Schousboe JT, Fink HA, Taylor BC, et al. Association between self-reported prior wrist fractures and risk of subsequent hip and radiographic vertebral fractures in older women: a prospective study. J Bone Miner Res. 2005;20:100–106. doi: 10.1359/JBMR.041025. [DOI] [PubMed] [Google Scholar]
- 8.Barrett-Connor E, Sajjan SG, Siris ES, Miller PD, Chen YT, Markson LE. Wrist fracture as a predictor of future fractures in younger versus older postmenopausal women: results from the National Osteoporosis Risk Assessment (NORA) Osteoporos Int. 2008;19:607–613. doi: 10.1007/s00198-007-0508-8. [DOI] [PubMed] [Google Scholar]
- 9.Dawson-Hughes B, Tosteson AN, Melton LJ, 3rd, et al. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int. 2008;19:449–458. doi: 10.1007/s00198-008-0559-5. [DOI] [PubMed] [Google Scholar]
- 10.National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. Washington DC: 2008. [Google Scholar]
- 11.Ismail AA, Silman AJ, Reeve J, Kaptoge S, O’Neill TW. Rib fractures predict incident limb fractures: results from the European prospective osteoporosis study. Osteoporos Int. 2006;17:41–45. doi: 10.1007/s00198-005-1887-3. [DOI] [PubMed] [Google Scholar]
- 12.Barrett-Connor E, Nielson CM, Orwoll E, Bauer DC, Cauley JA. Epidemiology of rib fractures in older men: Osteoporotic Fractures in Men (MrOS) prospective cohort study. BMJ. 2010;340:c1069. doi: 10.1136/bmj.c1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siris E, Miller P, Barrett-Connor E, Abbott T, Sherwood L, Berger M. Design of NORA, the National Osteoporosis Risk Assessment Program: a longitudinal US registry of postmenopausal women. Osteoporos Int. 1998;8(Suppl 1):S62–S69. [PubMed] [Google Scholar]
- 14.Siris ES, Miller PD, Barrett-Connor E, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001;286:2815–2822. doi: 10.1001/jama.286.22.2815. [DOI] [PubMed] [Google Scholar]
- 15.Barrett-Connor E, Weiss T, McHorney C, Miller P, Siris E. Predictors of falls among postmenopausal women: results from the National Osteoporosis Risk Assessment (NORA) Osteoporos Int. 2009;20:715–722. doi: 10.1007/s00198-008-0748-2. [DOI] [PubMed] [Google Scholar]
- 16.Siris ES, Brenneman SK, Miller PD, et al. Predictive value of low BMD for 1-year fracture outcomes is similar for postmenopausal women ages 50–64 and 65 and older: results from the National Osteoporosis Risk Assessment (NORA) J Bone Miner Res. 2004;19:1215–1220. doi: 10.1359/JBMR.040508. [DOI] [PubMed] [Google Scholar]
- 17.Bensen R, Adachi JD, Papaioannou A, et al. Evaluation of easily measured risk factors in the prediction of osteoporotic fractures. BMC Musculoskelet Disord. 2005;6:47. doi: 10.1186/1471-2474-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nevitt MC, Cummings SR, Browner WS, et al. The accuracy of self-report of fractures in elderly women: evidence from a prospective study. Am J Epidemiol. 1992;135:490–499. doi: 10.1093/oxfordjournals.aje.a116315. [DOI] [PubMed] [Google Scholar]
- 19.Ismail AA, O’Neill TW, Cockerill W, et al. Validity of self-report of fractures: results from a prospective study in men and women across Europe. EPOS Study Group. European Prospective Osteoporosis Study Group. Osteoporos Int. 2000;11:248–254. doi: 10.1007/s001980050288. [DOI] [PubMed] [Google Scholar]
- 20.Chen Z, Kooperberg C, Pettinger MB, et al. Validity of self-report for fractures among a multiethnic cohort of postmenopausal women: results from the Women’s Health Initiative observational study and clinical trials. Menopause. 2004;11:264–274. doi: 10.1097/01.gme.0000094210.15096.fd. [DOI] [PubMed] [Google Scholar]
- 21.Siggeirsdottir K, Aspelund T, Sigurdsson G, et al. Inaccuracy in self-report of fractures may underestimate association with health outcomes when compared with medical record based fracture registry. Eur J Epidemiol. 2007;22:631–639. doi: 10.1007/s10654-007-9163-9. [DOI] [PubMed] [Google Scholar]
- 22.Honkanen R, Kroger H, Tuppurainen M, Alhava E, Saarikoski S. Fractures and low axial bone density in perimenopausal women. J Clin Epidemiol. 1995;48:881–888. doi: 10.1016/0895-4356(94)00220-k. [DOI] [PubMed] [Google Scholar]
- 23.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]