Abstract
Objectives/Hypothesis
To provide national level data on frequency of tracheotomy and complication rate and in-hospital mortality following tracheotomy.
Study Design
Retrospective cohort study.
Methods
Retrospective cohort study using a public national database, the Nationwide Inpatient Sample, 2006.
Results
There were 113,653 tracheotomies performed in patients 18 years or older in 2006. The overall complication rate was 3.2%, and the in-hospital mortality rate was 19.2%. The data suggest that in-hospital mortality is usually due to the underlying illness rather than the tracheotomy. Mortality was higher in patients older than 50 years, those with cardiac conditions, particularly congestive heart failure, those with public insurance, and patients in Northeast hospitals. Patients with neurologic conditions, trauma, and upper airway infection are more likely to survive to discharge. In-hospital mortality is slightly higher in nonteaching hospitals.
Conclusions
This database study determined baseline data for the rate of complications (3.2%) for patients undergoing tracheotomy; it showed that only 80% of adult patients who underwent tracheotomy in the United States survived to discharge. Patients located in the Northeast, patients more than 50 years old, and patients with cardiac conditions were at particularly high risk for mortality. This study provides normative data for these outcomes for patient counseling and planning future quality improvement initiatives in this patient population.
Keywords: Nationwide Inpatient Sample, database, mortality, disparity, long-term care facility
INTRODUCTION
Tracheotomy can be livesaving for patients with upper airway compromise. It is more frequently performed, however, for patients who have a need for extended mechanical ventilation secondary to respiratory failure from a variety of disease processes.
Complications from the procedure itself can range from mild (e.g., granulation tissue) to fatal (e.g., loss of airway, tracheoinnominate fistula, mucus plug). In addition, patients who need extended mechanical ventilation are often very ill, and there may be substantial mortality from their underlying illness. Information about complication rates and mortality following tracheotomy would, therefore, be valuable to otolaryngologists and perhaps all physicians in counseling patients and families about this procedure. This information would also be helpful for defining baseline metrics for the procedure for designing future quality improvement projects.
Any single-institution study of tracheotomy complications will have at least three limitations: 1) even a very busy institution will not accumulate enough complications to make strong, statistically significant conclusions; 2) no single-institution study can examine regional differences; and 3) single-institution studies are inherently vulnerable to publication bias, in which institutions with poorer outcomes are less likely to publish their results. Goldenberg et al. reported on tracheotomy complications in 1,130 patients treated at a single institution during a 10-year period.1 The authors were able to describe the major complications and deaths attributed to tracheotomy, but data analysis was limited to descriptive statistics rather than a more robust statistical analysis even in this large retrospective case series.
The objectives of the current study are to 1) determine tracheotomy complication and mortality rates at the national level; and 2) identify clinical or demographic variables that are most predictive of complications and in-hospital mortality. Knowledge of these two factors may allow targeted interventions focused on improving outcomes in patients who undergo a tracheotomy.
MATERIALS AND METHODS
Study Design and Setting
This is a retrospective cohort analysis of the Healthcare Cost and Utilization Project’s Nationwide Inpatient Sample (NIS) from the year 2006 developed by the Agency for Healthcare Research and Quality. Details of the NIS have been reported elsewhere2,3; in brief, it is the largest publicly available all-payer inpatient care database in the United States, containing up to 8 million admissions from 1,000 hospitals within 38 states.2 This study was approved by the institutional review board at Children’s National Medical Center with an informed consent waiver.
Study Population
Hospitalizations of patients aged 18 years and older who underwent tracheotomy during the hospitalization were included. Tracheotomy was identified from International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes of 31.1 (temporary tracheostomy) and 31.2 (permanent tracheostomy) within the primary or secondary procedure codes from each hospitalization. NIS contains up to 15 procedure codes per hospitalization.
Main Outcome Measures
In-hospital mortality and tracheotomy-related complications during the admission when tracheotomy occurred were the main outcome measures. Tracheotomy complications included tracheostomy site infection (ICD-9-CM code 519.01), mechanical complication including tracheal stenosis (code 519.02), and other complications including tracheostomy hemorrhage and tracheo-esophageal fistula (code 519.09).
Patient Characteristics
Demographic characteristics were age analyzed in categories by decade, race/ethnicity, and insurance use.
Clinical characteristics included the presence of health conditions that may influence patient outcomes following tracheotomy identified with ICD-9-CM codes used in prior studies and NIS Clinical Classification Software. Respiratory conditions included cystic fibrosis, chronic obstructive pulmonary disease, asthma, apnea, and pneumonia. Neurologic conditions were epilepsy, cerebrovascular accident, cerebral palsy, muscular dystrophy, dementia, and spinal cord and intracranial injury. Cardiac conditions were myocarditis, cardiomyopathy, myocardial infarction, and congestive heart failure (CHF).
Hospital Characteristics
We also analyzed the relationship between hospital setting (rural vs. urban), teaching status (determined by the American Hospital Association criteria), and geographic region (West, Midwest, South, Northeast) and outcomes following tracheotomy.
Statistical Analyses
For all analyses, the data were clustered within each individual hospital, stratified by hospital type, size, and regional location, and weighted to achieve national estimates of the total number of tracheotomy operations performed throughout the United States in 2006. The Rao-Scott χ2 was used to examine univariate relationships between dichotomous outcomes and patient and hospital characteristics. A Student t test was used to assess the relationship between outcomes and continuous variables (e.g., age).
In multivariate analysis, hierarchical logistic regression models were built using a backward elimination process with a P ≤ .05 covariate keeping threshold. Partition, classification, and regression tree (CART) modeling was used to determine which characteristic combinations were associated with the highest and lowest mortality following tracheotomy using CART binary split and postpruning, goodness of fit rules. Statistical significance was determined as P < .05. Statistical Analysis Software version 9.1.3 and JMP (SAS Institute, Inc., Cary, NC) were used for all analyses.
RESULTS
There were 113,653 tracheotomy operations performed in the United States among patients 18 years or older during 2006. Most tracheotomy operations were performed in urban hospitals (96.6%, n = 109,465), in teaching hospitals (66.5%, n = 75,722), and in hospitals in the South (40.3%, n = 45,792). The average age at admission when tracheotomy occurred was 60.8 years (standard deviation, 17.0). Results showed 48.9% (n = 55,685) of patients undergoing tracheotomy were non-Hispanic white, and 64.9% (n = 73,741) used public insurance. The most common diagnoses among patients undergoing tracheotomy were pneumonia (44.7%, n = 50,758), CHF (27.1%, n = 30,757), and chronic obstructive pulmonary disease (25.4%, n = 28,848).
Results showed that 19.2% (n = 21,801) of patients died during admission when tracheotomy was performed; 3.2% (n = 3,748) of patients experienced a tracheotomy-related complication; and 0.6% (n = 628) experienced both a tracheotomy-related complication and death. Mortality did not vary significantly with the presence or absence of a tracheotomy complication (16.7% vs. 19.3%, P = .09).
Complication Rates
The most common complications of the tracheotomy are listed in Table I. The prevalence of a tracheotomy complication did not vary significantly by age, race/ethnicity, or insurance type (P > .06). The complication rate was higher in nonteaching hospitals compared with teaching hospitals (3.7% vs. 3.1%, P = .03) and in western hospitals compared with southern hospitals (4.2% vs. 2.7%, P = 0.01). Higher complication rates were observed in patients with an upper airway infection (7.1% vs. 3.3%, P < .001), obesity (6.0% vs. 3.2%, P < .001), paralysis (5.1% vs. 3.2%, P < .001), and CHF (4.0% vs. 3.0%, P < .001). In multivariate analysis, significant variation in tracheotomy complications remained after controlling for these conditions, with the highest likelihood of complications observed in western hospitals (odds ratio [OR], 1.5; 95% confidence interval [CI], 1.2–1.9) compared with hospitals in other regions.
TABLE I.
Tracheotomy Complication Prevalence.
| Tracheotomy Complication | No. | All Discharges, % (N = 113,653) | Complications, % (N = 3,748) |
|---|---|---|---|
| Tracheoesophageal fistula or tracheal hemorrhage due to tracheostomy* | 2,223 | 2.0 | 59.3 |
| Tracheal stenosis | 962 | 0.8 | 25.8 |
| Infection of tracheostomy | 572 | 0.5 | 15.3 |
| Tracheotomy complication, unspecified | 77 | 0.1 | 2.0 |
The International Classification of Diseases, Ninth Revision, Clinical Modification code combines these two different complications together.
Risk Factors for In-Hospital Mortality
Mortality varied significantly (P < .001) by hospital region, with patients in the Northeast experiencing the highest mortality (26.8%) and patients in the Midwest experiencing the lowest mortality (14.8%). Mortality was higher in nonteaching hospitals compared with teaching hospitals (21.0% vs. 18.2%, P < .001) (Table I).
Older patients had higher in-hospital mortality (Table II); mortality was also higher in patients utilizing public versus private insurance (22.0% vs. 14.3%, P < .001).
TABLE II.
Demographic and Hospital Characteristics of Adult Patients Undergoing Tracheotomy, National Inpatient Sample 2006.
| Characteristic | % (n) | In-Hospital Mortality, % | P Value |
|---|---|---|---|
| Demographic characteristics | |||
| Age, yr | <.001 | ||
| 18–29 | 6.2 (7,069) | 8.4 | |
| 30–39 | 6.0 (6,774) | 7.8 | |
| 40–49 | 11.9 (13,530) | 12.0 | |
| 50–59 | 19.2 (21,737) | 16.7 | |
| 60–69 | 22.1 (24,964) | 20.3 | |
| 70–79 | 21.5 (24,438) | 25.0 | |
| 80–89 | 12.0 (13,666) | 28.1 | |
| ≥90 | 1.2 (1,387) | 27.3 | |
| Race/ethnicity | <.001 | ||
| Non-Hispanic white | 48.9 (55,635) | 20.3 | |
| Black | 12.7 (14,388) | 21.2 | |
| Hispanic | 7.7 (8,685) | 20.6 | |
| Other | 4.4 (4,903) | 21.7 | |
| Missing | 26.2 (29,968) | 15.3 | |
| Primary insurance | <.001 | ||
| Public | 64.8 (73,711) | 22.0 | |
| Private | 30.7 (34,800) | 14.3 | |
| Other | 4.5 (5,033) | 11.4 | |
| Hospital characteristics | |||
| Teaching hospital | .001 | ||
| Yes | 65.7 (75,722) | 18.2 | |
| No | 34.3 (37,731) | 20.9 | |
| Urban hospital | .28 | ||
| Yes | 96.6 (109,465) | 19.2 | |
| No | 3.4 (3,988) | 17.4 | |
| Hospital region | <.001 | ||
| Northeast | 20.1 (24,504) | 26.8 | |
| West | 19.3 (20,978) | 18.3 | |
| South | 42.0 (45,792) | 17.8 | |
| Midwest | 18.6 (22,329) | 14.8 | |
In univariate analysis, cardiac conditions were associated with the highest mortality following tracheotomy. Mortality was higher in patients with myocardial infarction (27.1% vs. 18.3%, P < .001), CHF (27.1% vs. 16.2%, P < .001), and myocarditis/cardiomyopathy (26.4% vs. 18.7, P < .001) than in patients without these conditions. Trauma was associated with lower mortality following tracheotomy. Mortality was lower in patients with intracranial trauma, (9.0% vs. 20.3%, P < .001), spinal cord injury (11.5% vs. 19.3%, P < .001), and skull fracture (6.0% vs. 19.8%, P < .001) as compared to patients without these conditions. The lowest mortality was observed in patients undergoing tracheotomy with an upper airway infection (5.7% vs. 19.3%, P < .001) (Table III).
TABLE III.
Clinical Characteristics of Adult Patients Undergoing Tracheotomy, National Inpatient Sample 2006.
| Characteristic | Total Study Population, % (N = 113,653) | In-Hospital Mortality, %* | P Value |
|---|---|---|---|
| Cardiac conditions | |||
| Congestive heart failure | 27.1 | 27.1 vs. 16.2 | <.001 |
| Myocardial infarction | 10.1 | 27.1 vs. 18.3 | <.001 |
| Myocarditis/cardiomyopathy | 5.6 | 26.4 vs. 18.7 | <.001 |
| Pulmonary conditions | |||
| Pneumonia | 44.6 | 21.1 vs. 17.6 | <.001 |
| Chronic obstructive pulmonary disease | 25.4 | 21.7 vs. 18.3 | <.001 |
| Asthma | 4.5 | 16.7 vs. 19.3 | .06 |
| Neurologic conditions | |||
| Cerebrovascular accident | 12.1 | 18.9 vs. 19.2 | .8 |
| Epilepsy | 9.3 | 18.1 vs. 19.3 | .2 |
| Paralysis | 4.6 | 11.6 vs. 19.5 | <.001 |
| Dementia | 1.3 | 17.3 vs. 19.2 | .4 |
| Muscular dystrophy | 0.6 | 9.8 vs. 19.2 | <.001 |
| Cerebral Palsy | 0.3 | 2.8 vs. 19.2 | <.001 |
| Trauma | |||
| Intracranial trauma | 10.3 | 8.9 vs. 20.3 | <.001 |
| Skull fracture | 4.3 | 6.0 vs. 19.8 | <.001 |
| Spinal cord injury | 1.8 | 11.5 vs. 19.3 | <.001 |
| Other | |||
| Obesity | 4.2 | 11.8 vs. 19.5 | <.001 |
| Upper airway infection | 1.0 | 5.7 vs. 19.3 | <.001 |
Shown is the percentage of in-hospital mortality in the presence and absence of each condition.
In multivariate analysis (Fig. 1), patients undergoing tracheotomy in the Northeast had the highest likelihood of mortality during the hospitalization compared with patients in the Midwest (OR, 2.00; 95% CI, 1.68–2.38) after controlling for other significant characteristics including age, insurance, and comorbid health conditions. Cardiac conditions remained associated with higher mortality. Neurologic conditions and trauma remained associated with lower mortality. Patients undergoing tracheotomy in the setting of an upper airway infection had the lowest likelihood of mortality (OR, 0.27; 95% CI, 0.16–0.45).
Fig. 1.
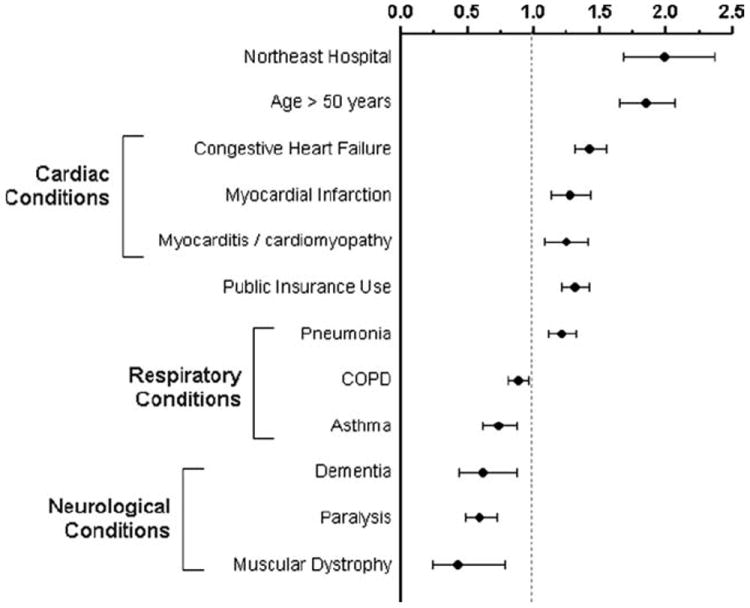
Multivariate analysis of mortality during the hospitalization when tracheotomy was performed, National Inpatient Sample 2006. COPD = chronic obstructive pulmonary disease.
Admission source remained significantly associated with in-hospital mortality in multivariate analysis, with patients transferred from another hospital (OR, 1.2; 95% CI, 1.1–1.4) and patients admitted from the emergency department (OR, 1.2; 95% CI, 1.1–1.3) experiencing a higher likelihood of mortality than patients experiencing a routine admission. Furthermore, those admitted from a long-term care facility had higher complication rates than the other admission sources.
In the CART analysis, age was the characteristic most significantly associated with in-hospital mortality. Mortality in patients aged 50 years and older was 22.6% vs. 13.0% for patients aged less than 50 years, P < .001. Among patients age 50 years and more, using a hospital within the Northeast was the characteristic most significantly associated with mortality. Mortality among patients aged 50 years who underwent tracheotomy in a Northeast hospital was 32.4% compared with 21.1% for patients using hospitals in other regions, P < .001. The highest mortality was observed among patients age 50 years or more with CHF who underwent tracheotomy in the Northeast (38.4%). The lowest mortality was observed among patients aged less than 30 years who did not have CHF (7.4%) (Fig. 2).
Fig. 2.
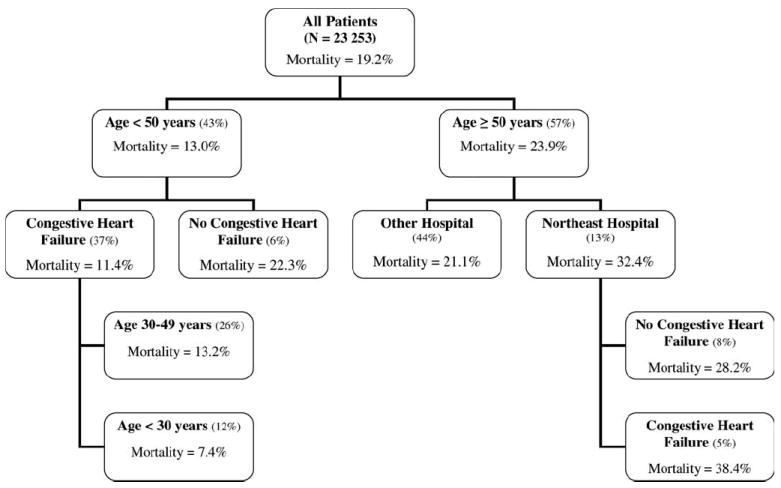
Partition classification and regression tree analysis of patient characteristic combinations associated with in-hospital mortality, National Inpatient Sample 2006.
DISCUSSION
This study comprehensively evaluated a large population of patients who underwent tracheotomy to examine factors that make in-hospital mortality following this procedure more likely. Perhaps the most striking finding is that, on a national basis, almost 20% of all adult patients who undergo tracheotomy will not survive to discharge. The ability to identify those patients at particularly high risk of in-hospital mortality would be helpful to clinicians counseling those patients and their families; furthermore, deeper examination of why they are more likely to die may provide opportunities for targeted interventions.4-6
It is impossible to determine from this sample whether mortality is due to tracheotomy complications. However, the fact that mortality following tracheotomy is higher in cardiac conditions and lower conditions such as muscular dystrophy and upper airway infection strongly suggests that the tracheotomy itself is rarely the cause of death.5,6 This is certainly in accord with the authors’ personal experiences, in that most patients who die with a tracheotomy in place die of an underlying disease rather than a tracheotomy complication.7,8
The greatest patient risk factors for in-hospital mortality were age >50 years, any cardiac condition, public insurance, and pneumonia. Chronic obstructive pulmonary disease, asthma, neurologic conditions, trauma, and upper airway infections were conditions that were associated with lowered in-hospital mortality. Public insurance use may possibly be a marker for increased age, as most Medicare beneficiaries are >65 years. In theory, multivariate analysis should account for the two variables separately. In practice, because almost all American patients who are >65 years are on public insurance, multivariate analysis might be unable to tease out the influence of age as distinct from payer.
Although the differences in mortality after tracheotomy based on ethnicity were statistically significant, they were clinically insignificant (minimum 20.3%, maximum 21.7%). Likewise, mortality after tracheotomy in teaching hospitals was statistically different from that in nonteaching hospitals, but the size of the difference was very modest (18.2% vs. 20.9%).
An extraordinary and previously unreported finding is the significant regional variation in in-hospital mortality after tracheotomy, ranging from 14.8% in the Midwest to 26.8% in the Northeast. Because both these data and clinical experience suggest strongly that mortality after tracheotomy is determined primarily by other underlying illnesses, the most parsimonious hypothesis to explain this variability is that Northeastern hospitals are more likely to perform tracheotomies on patients who have more severe underlying illnesses, particularly CHF. This finding may be due to differences in medical practice in the Northeast or conceivably to cultural differences in patient preferences for aggressive care for chronic conditions.9 Of course, it is beyond the scope of an administrative data set to test this hypothesis. However, the NIS perhaps suggests this association, which may be answered by a properly conducted research study.
CART is a statistical model that determines the best questions to ask, and in which order, to identify the groups of patients with highest and lowest mortality. In our CART model, in-hospital mortality ranged from 7.4% (in patients with CHF who were <30 years old) to 38% (in patients aged >50 years, in the Northeast, with CHF). It is particularly interesting that CHF increases the in-hospital mortality for patients >50 years, and decreases it for patients <50 years. Presumably young patients with CHF have congenital lesions that are palliated and/or acute cardiac conditions (e.g., myocarditis) that may resolve. Older patients with CHF are more likely to have multisystem vascular disease and irreversibly failing hearts.
Although it is impossible to determine in advance that a tracheotomy in a particular patient is futile, it is likely that many patients and families who have tracheotomies and do not survive to discharge would ultimately consider the tracheotomy (in retrospect) ‘‘futile.’’ There are several other benefits of tracheotomy, however, including improved pulmonary hygiene, comfort of being extubated from an orotracheal tube, and facilitating weaning from the ventilator, which are difficult to measure. Providers have an obligation to ensure that patients and families understand the chances of benefit from a tracheotomy. These data may help physicians wishing to counsel adult patients about their likelihood of survival to discharge following tracheotomy.
There are several inherent limitations in our study methodology that warrant discussion. The primary limitation of our study is the use of ICD-9-CM codes as inclusion criteria. It may be that due to coding irregularities, certain patients or types of patients may have been overlooked. However with the large sample size, we estimate that the impact of such would be mitigated. Specifically, a limit of using ICD-9-CM codes is that areas of intense study with regard to tracheotomy technique (for example between open versus percutaneous technique) are not able to be evaluated. Further, the NIS does not include all states, and as such its general-izability may be limited. However, states not included in the data acquisition may still be able to use the national estimates for benchmarking.
CONCLUSION
A publicly available, national data set was used to determine the number of patients who undergo tracheotomy annually and to determine the rate of complications (3.2%) and in-hospital mortality (19.2%). Specific variables, most notably patient age, cardiac conditions, and geographic location, increase the likelihood of in-hospital mortality. The overall survival to discharge after adult tracheotomy in the United States is only about 80%, and it is substantially less for some patient groups. We recommend that patients and families be counseled about the likelihood of survival to discharge as part of the informed consent process for tracheotomy.
Acknowledgments
Dr. Berry was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development career development award (K23 HD058092).
Footnotes
Presented in part at the Annual Meeting of the American Bronchoesophagological Association, Chicago, Illinois, U.S.A., May 1, 2011.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
BIBLIOGRAPHY
- 1.Goldenberg D, Ari EG, Danino J, Netzer A, Joachims HZ. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg. 2000;123:495–500. doi: 10.1067/mhn.2000.105714. [DOI] [PubMed] [Google Scholar]
- 2.NIS introduction. [June 8, 2009]; Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/2006NIS_INTRODUCTION.pdf.
- 3. [June 8, 2009];Data use agreement. Available at: http://www.hcup-us.ahrq.gov/team/NIS%20DUA_%20062508.pdf.
- 4.Berry JG, Graham RJ, Roberson DW, et al. Patient characteristics associated with in-hospital mortality in children following tracheotomy. Arch Dis Child. 2010;95:703–710. doi: 10.1136/adc.2009.180836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berry JG, Graham DA, Graham RJ, et al. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009;124:563–572. doi: 10.1542/peds.2008-3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darrat I, Yaremchuk K. Early mortality rate of morbidly obese patients after tracheotomy. Laryngoscope. 2008;118:2125–2128. doi: 10.1097/MLG.0b013e3181847a78. [DOI] [PubMed] [Google Scholar]
- 7.Souza FM, Lai P. Tracheotomy in Canadian urban centre. J Otolaryngol. 2005;34:341–345. doi: 10.2310/7070.2005.34508. [DOI] [PubMed] [Google Scholar]
- 8.Straetmans J, Schlondorff G, Herzhoff G, Windfuhr JP, Kremer B. Complications of midline-open tracheotomy in adults. Laryngoscope. 2010;120:84–92. doi: 10.1002/lary.20703. [DOI] [PubMed] [Google Scholar]
- 9.Lewis CW, Carron JD, Perkins JA, Sie KC, Feudtner C. Tracheotomy in pediatric patients: a national perspective. Arch Otolaryngol Head Neck Surg. 2003;129:523–529. doi: 10.1001/archotol.129.5.523. [DOI] [PubMed] [Google Scholar]


