Abstract
Background
Despite the development of multi-drug regimens for HIV, palliative care and quality-of-life issues in patients with advanced AIDS remain important areas of clinical investigation.
Objective
Authors assessed the impact of treatment for depression on desire for hastened death in patients with advanced AIDS.
Method
Patients with advanced AIDS (N=372) were interviewed shortly after admission to a palliative-care facility, and were reinterviewed monthly for the next 2 months. Patients diagnosed with a major depressive syndrome were provided with antidepressant treatment and reinterviewed weekly. Desire for hastened death was assessed with two questionnaire measures.
Results
Desire for death was highly associated with depression, and it decreased dramatically in patients who responded to antidepressant treatment. Little change in desire for hastened death was observed in patients whose depression did not improve. Although improved depression was not significantly associated with the use of antidepressant medication, those individuals prescribed antidepressant medication showed the largest decreases in desire for hastened death.
Discussion
Successful treatment for depression appears to substantially decrease desire for hastened death in patients with advanced AIDS. The authors discuss implications of these findings for palliative-care treatment and the physician-assisted suicide debate.
Despite the hope created by the development of multi-drug regimens, patients with AIDS are still dying in large numbers, and palliative care and quality-of-life issues in patients with advanced AIDS remain important areas of clinical investigation.1 Perhaps the most compelling and clinically relevant issue in palliative care today concerns desire for hastened death. Desire for hastened death is typically defined as a wish for death to occur more rapidly, whether by active (e.g., physician-assisted suicide [PAS] or conventional suicide) or passive means (e.g., terminating life-sustaining interventions such as dialysis, or stopping potential treatments so as to allow for disease progression). The United States Supreme Court decisions2,3 notwithstanding, issues such as whether or not to legalize PAS or how to manage requests to terminate life-sustaining interventions, will continue to be actively debated in many countries and state legislatures.
Cornerstones of this debate are questions as to the role and relevance of mental health evaluations, and, in particular, the extent to which requests for assisted suicide or other death-hastening interventions (e.g., cessation of dialysis, termination of potentially curative treatments) are fueled by depression.4 Although there is little dispute that mental health interventions are warranted for physically healthy individuals who have thoughts of suicide, psychiatric treatment of medically ill patients who desire hastened death is far more controversial. A critical component of this debate is the question of whether effective treatment for depression reduces the desire for hastened death in patients with advanced or life-threatening illness.
Virtually no empirical research to-date has examined whether palliative care interventions change a patient’s desire for hastened death. Meier and colleagues,5 in their survey of physicians who had received requests for PAS, found that 25% responded by prescribing antidepressant medications. However, they did not report whether patients actually received or benefited from antidepressant therapy, or whether any patients rescinded their request after this intervention. Given the central role played by depression in studies of desire for hastened death,6,7 we sought to address this critical question by studying the impact of depression treatment on desire for hastened death in a large sample of patients with advanced AIDS.
METHOD
Participants
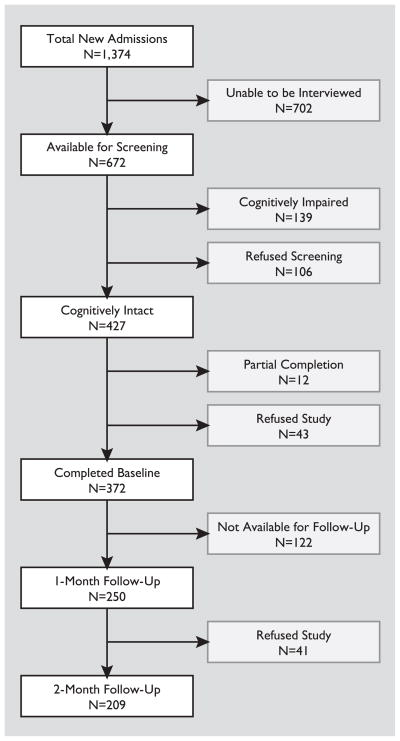
Patients with advanced AIDS were recruited from three palliative-care facilities in New York City between January of 1999 and December of 2002. All newly admitted patients were eligible for participation unless they did not speak English, were less than 18 years old, or revealed symptoms of psychosis. Also, all patients were administered the Mini-Mental State Exam8 in order to assess for cognitive impairment, and those who scored below 20 were excluded from study participation. During the 4-year study period, 1,374 new patients were admitted to the participating study facilities, 372 of whom ultimately completed the initial evaluation (Figure 1). We re-interviewed 250 (67.2%) of these participants 1 month later, and 209 (56.2%) completed a third interview 2 months after the initial assessment.
FIGURE 1.
Flowchart of Patient Accrual
The demographic and clinical characteristics of the sample have been described elsewhere9 and are only summarized briefly here (Table 1). Of the 372 participants, 280 were men (75.3%); the average age was 44.4 years (standard deviation [SD]: 9.4; range: 23–75), and average education level was 11.9 (2.9) years. The sample was predominantly minority, with 57.5% African American (N=214) and 22.3% Hispanic (N=83). The most common source of HIV infection was reported to be sexual contact (N=208; 56.7%). All participants were diagnosed with AIDS; median CD4 +cell count was 68, and median viral load was 16,850.
TABLE 1.
Sample Demographic Characteristics (at baseline assessment)
| Gender | Men N=280 (75.3%) |
Women N=92 (24.7%) |
||
| Age, years | ≤35 N=66 (17.8%) |
36–45 N=141 (38.0%) |
46–55 N=120 (32.3%) |
>55 N=44 (11.9%) |
| Race | White N=72 (19.4%) |
African American N=214 (57.5%) |
Hispanic N=83 (22.3%) |
Other N=3 (0.8%) |
| Education | <High school N=145 (39.1%) |
High school degree/equivalent N=95 (25.6%) |
Some college N=91 (24.5%) |
College graduate/advanced degree N=40 (10.8%) |
| HIV transmission risk factor | Sexual N=208 (56.7%) |
Intravenous drug use N=95 (25.9%) |
Transmission N=3 (0.8%) |
Multiple/unknown N=61 (16.6%) |
| Religion | Catholic N=138 (37.5%) |
Protestant/Baptist N=134 (36.4%) |
Other (Jewish, Muslim, etc.) N=77 (20.9%) |
Spiritual/non-religious N=19 (5.2%) |
Procedures
All participants who consented to participate were interviewed within 1 week after admission. Patients were administered several clinician-rated and self-report instruments, with the self-report instruments being read aloud to patients to minimize burden. Most assessments were completed in a single interview, although, occasionally, assessments were divided over two sessions (typically completed within 24 to 48 hours). Participants were re-interviewed 1 and 2 months later, except in cases of patients’ death (N=11), discharge from the facility (N=127), severe cognitive deterioration (on the basis of a readministration of the MMSE conducted before each evaluation; N=12), or if they refused to continue (N=8; reasons for attrition were missing for 10 participants). Roughly 10% of all assessments were rated by a second clinician to establish interrater reliability. The study was approved by the Institutional Review Boards of each participating institution.
To assess depression, we administered the Depression module of the Structured Clinical Interview for DSM–IV, HIV version (SCID),10 to establish a diagnosis of a major depressive syndrome, and the Hamilton Rating Scale for Depression (Ham-D)11 to quantify the current severity of depressive symptoms. In rating the presence and severity of somatic symptoms, we used a combination of the “inclusive” and “etiologic” approaches, wherein evaluators first attempted to determine whether the symptom was due to depression or illness, but when this determination could not be made, the symptom was included in the depression rating.12 Patients who were identified as having a major depressive syndrome were referred for antidepressant treatment. Barring contraindications or refusal, treatment consisted primarily of an SSRI (selective serotonin-reuptake inhibitor) antidepressant medication (sertraline or paroxetine), unless the patient was already prescribed another antidepressant, and titration to a therapeutic dose was deemed more appropriate. Patients also received standard psychosocial care provided by the facility (e.g., contact with social worker, pastoral care, palliative care), as well as weekly contact with study personnel and the facility’s psychiatric consultant to monitor improvement and side effects and ensure optimal dose titration. Services provided by the treatment setting were not monitored or controlled (i.e., patients received “usual care” in addition to study treatment).
For the purposes of data analysis, patients were categorized as “depressed” at baseline if they met DSM–IV criteria for a Major Depressive syndrome on the basis of SCID interviews and obtained a score of ≥18 on the Hamilton Rating Scale for Depression (Ham-D). Patients who met neither of these criteria (i.e., no DSM–IV depression diagnosis and Ham-D score <18) were classified as “not depressed.” Patients who met one but not both of these criteria were classified as “mildly depressed,” although many of these individuals (as well as many patients classified as “not depressed”) nevertheless received anti-depressant treatment (Table 2).
TABLE 2.
Prevalence of Desire for Hastened Death and Antidepressant Treatment in Relation to Depression Severity
| Depression at Baseline Assessment | SAHD | DDRS | High Desire | % on Rx |
|---|---|---|---|---|
| Depressed (N=64) (SCID+/Ham-D ≥18) | 5.66 | 1.57 | 29.1% | 79% |
| Mildly depressed (N=59) (SCID+/Ham-D <18 or SCID ≥18) | 3.49 | 0.92 | 7.8% | 52% |
| Not depressed (N=249) (SCID−/Ham-D <18) | 1.68 | 0.31 | 0.9% | 24% |
SAHD: Schedule of Attitudes toward Hastened Death; DDRS: Desire for Death Rating Scale; SCID: Structured Clinical Interview for DSM–IV; Ham-D: Hamilton Rating Scale for Depression.
High desire: % with SAHD ≥10 or DDRS ≥3.
% Rx: Percent of sample receiving antidepressant medication, based on subset available at first follow-up assessment (N=42 for “Depressed,” 58 for “Mildly Depressed,” and 143 for “Not depressed.”)
Depressed patients were classified as “significantly improved” at follow-up if they had at least a 33% reduction in Ham-D score1 and the Ham-D fell below 18 (e.g., a patient with a baseline Ham-D of 21 would need a follow-up Ham-D of 14 or less); SCID interviews were not repeated at follow-up assessments. Patients were characterized as “still depressed” if their Ham-D score remained above 18 and they had less than a 33% reduction in symptoms. Some previously depressed patients met only one of these two criteria and were characterized as “partially improved.” Patients who were not depressed at baseline were classified as “significantly worse” if their Ham-D score increased by 50% or more and exceeded 18. These improvement categories were used to create four depression “trajectories” (described below) that distinguished different patterns of change in depressive symptoms.
Desire for hastened death was measured both by self-report (the Schedule of Attitudes toward Hastened Death [SAHD])13,14 and clinician-rated measures (the Desire for Death Rating Scale [DDRS]).15 Patients were identified as having a great desire for hastened death if they obtained an SAHD score of ≥10 or a DDRS score of ≥3. However, for multivariate analyses (HLM [hierarchical linear models]), we relied solely on the SAHD because of the greater variability in possible (and obtained) scores. A number of additional study measures were administered but are not described in this report.9
Statistical Analyses
We used descriptive analyses (chi-square tests of association and ANOVA), to assess associations between depression and improvement trajectories with desire for hastened death and treatment with antidepressant medications. In addition to descriptive analyses, we utilized HLM to more directly test the hypothesis that reduction in depressive symptoms would ameliorate desire for hastened death over time. The use of HLM models allows for an analysis of individual change trajectories and the variables that “explain” the differences in these trajectories. Thus, rather than grouping improvement trajectories (which is beneficial for understanding changes, but oversimplifies the data), HLM treats change (i.e., improvement trajectory) as a continuous dependent variable. Moreover, by using HLM (rather than, for example, repeated-measures ANOVA), missing data can be included in the analysis, maximizing the accuracy of data interpretation. The HLM model used in these analyses was based on the methods described in Bryk and Raudenbush16,17 and in Pinheiro and Bates.18 The HLM model was divided into two levels. In the upper-level model, patients’ desire for hastened death (SAHD scores) is a function of time. In the second level of HLM analysis, the influence of an antidepressant medication (ADP) and its effects on depression scores (Ham-D) are added in what Bryk and Raudenbush call the “intercept- and slope-as-outcomes” model.16 The intercept and slope in the upper-level model become outcome variables in the lower-level model. Thus, changes in SAHD scores over time consists of multiple components: average change in SAHD scores for the entire sample (the intercept), changes associated with depression (Ham-D), changes associated with the administration of an antidepressant (ADP), and changes attributed to the interaction of Ham-D and ADP (Ham-D:ADP). These calculations were carried out by use of R.
Finally, interrater reliability was established with an intraclass correlation coefficient (ICC)19 for continuous variables (Ham-D and DDRS) and kappa coefficients20 for categorical ratings (SCID diagnoses). For each of these analyses, reliability was very high; k=0.93; N=29; p<0.0001 for the diagnosis of a major depressive syndrome (Ham-D ICC=0.94; N=42; p<0.0001, and DDRS ICC=0.92; N=42; p<0.0001.
RESULTS
Prevalence of Depression and Desire for Hastened Death
Of the 372 patients initially assessed, 100 (26.9%) were diagnosed with a Major Depressive syndrome (MDS) on the basis of the SCID, and 87 (23.4%) had Ham-D scores of at least 18. A total of 64 patients (17.2%) met both criteria for classification as “depressed” (SCID diagnosis and Ham-D ≥18) for the purposes of this study. An additional 249 patients (66.9%) were categorized as “not depressed” (i.e., no diagnosis of MDS on the SCID and Ham-D <18). There were an additional 59 patients (9%) who met one but not both of our criteria for depression and were classified as “mildly depressed.” Not surprisingly, these three groups differed with regard to desire for hastened death (Table 2): χ2=74.05; p<0.0001, with desire for hastened death being highest in the “depressed” group and lowest in the “not depressed” group.
Response to Treatment for Depression
We examined response to treatment for depression among the 42 depressed patients (of 64, 65.6%) who were reevaluated 1 month later. Of these 42 patients, 21 (50%) were classified as “significantly improved” (i.e., Ham-D <18 and ≥33% reduction in Ham-D scores), and 2 patients (4.8%) showed partial improvement. However, 19 patients (45.2%) were “still depressed” at the 1-month follow-up evaluation. Surprisingly, there was no association between improvement in depression and whether patients were prescribed antidepressant medications: χ2=1.58; p=0.45. Of the 21 significantly improved patients, 17 (81%) had been prescribed anti-depressant medications. However, 14 of the 19 patients (79%) who remained depressed also received antidepressant medications, as did both of the patients who showed partial improvement.
Of the original 64 depressed subjects, 38 were available for assessment after 2 months. Twenty-three of these patients (60.5%) were “significantly improved” after 2 months, and one patient (2.6%) showed “partial improvement;” 14 (36.8%) were “still depressed.” Again, there was no association between improvement and antidepressant medications: χ2=2.31; p=0.31. Of the 23 “significantly improved” patients, 17 (74%) were prescribed an antidepressant, as were 13 of 14 patients who were “still depressed” (93%).
In order to better understand the relationships between change in depression and desire for hastened death, we categorized patients into four groups, based on the trajectory of their depression over time; individuals lost to follow-up at the second assessment were classified as unchanged from the previous assessment (i.e., a “last response carried forward” approach to classification). Depressed patients who were significantly improved (as defined above) at the 1-month follow-up and who maintained that improvement were classified as “Successfully Treated” (N=20). Participants who were still depressed or only partially improved at the 1-month follow-up assessment but were significantly improved after 2-months were classified as “Improved Late” (N=8). Patients who remained depressed throughout the 2-month study period (N=15) were classified as “Remained Depressed.” Finally, there were seven participants who were not depressed at baseline but “Became Depressed” during the course of the study (as described above).
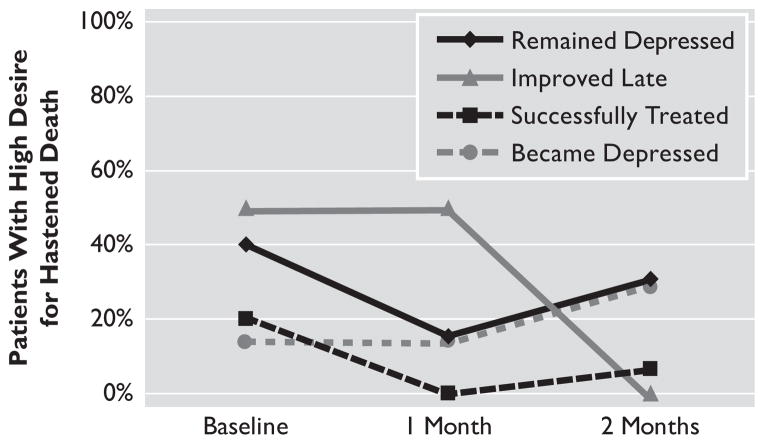
At the baseline assessment, the frequency of patients with a high desire for hastened death was comparable across the four trajectory groups: χ2[3]=4.01; p=0.26 (Figure 2). Although there were modest differences in desire for death at baseline across these four groups (ranging from 14% to 50%), these differences were not significant because of the small samples for several of the groups. However, at the first follow-up assessment, the proportion of patients high in desire for hastened death differed significantly: χ2=13.36; p=0.004. None of the 20 patients whose depression resolved at the first follow-up assessment still had a high desire for hastened death, whereas desire for hastened death remained essentially unchanged among the three groups whose depression had not improved.
FIGURE 2.
Changes in Desire for Hastened Death, Based on Trajectory of Depression Improvement
However, at the second follow-up period, desire for hastened death no longer differed significantly across the four groups: χ2=5.88; p=0.12. This finding reflects two changes: of the eight patients whose depression improved between the first and second follow-up assessments (the “Improved Late” group), none still had an elevated desire for hastened death; but one of the patients who had been successfully treated for depression nevertheless developed a high desire for hastened death at the final assessment, despite no worsening of depression. Desire for hastened death also emerged in a second patient who was classified as “Became Depressed.” Thus, the proportion of patients with elevated desire for death was roughly comparable across the four groups.
Fluctuations in desire for hastened death were quite rare among patients who were never depressed (205 of whom were available for follow-up assessments). Four nondepressed individuals (2%) exhibited a high desire for hastened death at some point during the study period; two had high desire for death (despite no indication of depression) at the baseline assessment, and two more developed a high desire for hastened death at a subsequent assessment. However, none of these individuals had a high desire for hastened death at more than one of the three time-points, suggesting that their desire was relatively transient.
Impact of Change in Depression on Desire for Hastened Death
Although the descriptive analyses above suggest a strong relationship between improvement in depression and reduced desire for death that is independent of anti-depressant medications, these group-level data do not allow for an analysis of individual changes in desire for death, nor do they provide a rigorous test of the importance of antidepressant treatment. Thus, we analyzed the relationship between changes in desire for hastened death (based on SAHD scores) and changes in depression by utilizing a series of three HLM models. The first model, analyzing whether desire for hastened death changed over time, yielded nonsignificant coefficients (t=1.35, p=0.18 and t=1.74, p=0.09 for the contrast between baseline and the first and second follow-up assessments, respectively). Thus, across the sample as a whole, there was no “time” effect, which indicates that desire for hastened death was relatively stable.
The second model added Ham-D scores into the analysis of changes in SAHD scores. Model 2 demonstrated a significant effect for depression on changes in SAHD scores over time (t=17.50; p<0.0001), with no main effect for either time contrast (t=0.89; p=0.38 and t=0.66; NS for baseline to first follow-up and between the first and second follow-up assessments, respectively). Thus, whereas desire for hastened death remained relatively stable for most individuals, changes in depression severity (based on Ham-D scores) were associated with changes in desire for death (i.e., decreased depression resulted in decreases in desire for hastened death).
Finally, the effects of antidepressant medication and the interaction between antidepressant medication and depression symptoms were entered in the final model. This model showed that antidepressant medications provided a significant contribution to explaining changes in SAHD scores over time, beyond the effects of improved depression. Specifically, for every unit decrease in the Ham-D score, the corresponding decrease in the SAHD score was estimated to be 0.26 (t=10.45; p<0.0001; Table 3). However, this 0.26 decrease in SAHD score was bolstered by −0.07 if the patient was administered an antidepressant (t=1.89; p=0.06). This interaction was strongest (and was only statistically significant) at the first follow-up assessment (t=2.15; p=0.03; the Ham-D:ADP:Time 1 parameter in Table 3). Other parameters in the HLM model were not statistically significant.
TABLE 3.
Parameter Estimates of the Hierarchical Linear Models (HLM) Testing the Efficacy of Antidepressants in Reducing Patients’ Desire for Hastened Death (based on Model 3)
| Value | Standard Error | t | p | |
|---|---|---|---|---|
| Intercept | −0.16 | 0.36 | −0.45 | NS |
| Depression (Ham-D) | 0.26 | 0.02 | 10.45 | 0.0001 |
| Time 1 | 0.51 | 0.56 | 0.92 | NS |
| Time 2 | 0.27 | 0.59 | 0.45 | NS |
| Antidepressant Rx (ADP) | 0.57 | 0.55 | 1.03 | NS |
| Ham-D*Time 1 | −0.07 | 0.05 | −1.36 | NS |
| Ham-D*Time 2 | −0.06 | 0.05 | −1.10 | NS |
| Ham-D*ADP | −0.07 | 0.04 | −1.89 | 0.06 |
| ADP*Time 1 | −0.79 | 0.82 | −0.97 | NS |
| ADP*Time 2 | 0.19 | 0.87 | 0.22 | NS |
| Ham-D*ADP*Time 1 | 0.14 | 0.06 | 2.15 | 0.03 |
| Ham-D*ADP*Time 2 | 0.07 | 0.07 | 1.03 | NS |
Ham-D: Hamilton Rating Scale for Depression; ADP: antidepressant medication.
DISCUSSION
This study represents the first longitudinal analysis of the impact of depression and its treatment on desire for hastened death. Virtually all depressed patients with advanced AIDS who experienced significant improvement in depressive symptoms also showed a significant reduction in desire for hastened death. Conversely, those individuals who remained depressed rarely showed significant improvement in desire for hastened death. Moreover, desire for hastened death emerged in some patients as they became more depressed over time. Thus, these data suggest that successful treatment for depression, whether success is due to antidepressant medications, other palliative care, psychosocial interventions, or the natural course of mood disorders, is likely to reduce desire for hastened death, even in patients with an advanced and/or life-threatening illness. These findings show a much stronger impact of depression improvement than had been previously reported by Ganzini et al., who found that successful treatment of depression had only modest effects on patient preferences for life-sustaining interventions.21
However, our data also reveal that not all desire for hastened death can be attributed to unresolved depression. A small number of patients had high desire for death even in the absence of depression. Furthermore, nearly half of our sample who received antidepressant treatment (medication and/or supportive psychotherapy or counseling), showed little or no improvement in depressive symptoms. Hence, it is clearly inaccurate to assert that treatment for depression will invariably reduce desire for hastened death, but, rather, that there is a substantial likelihood of reduced desire for death for those patients in whom depression is successfully treated.
Understanding the role of antidepressant medications is complicated by the divergent findings from these analyses. Although there was no difference in reduction of depression depending on whether antidepressant medications were prescribed (i.e., improvement in depression was not more likely when antidepressants were prescribed), antidepressant medication appeared to enhance the effects of depression improvement in reducing desire for hastened death (on the basis of the HLM models). Thus, although reduced depression was not simply a function of antidepressant medications, when these medications were prescribed and depression improved, desire for hastened death was reduced to a greater degree than when medications were not utilized. Because we did not recommend antidepressant treatment for individuals who were not depressed, we cannot assess the impact of medications alone on desire for hastened death in the absence of depression.
These results, however, should not be interpreted as an indication of the efficacy of antidepressant medications in the treatment of depressed patients with advanced AIDS. Because treatment for depression was not standardized (that is, patients often received multiple interventions), this study should not be considered a controlled clinical trial of antidepressant therapy. Moreover, because our goal was not to systematically analyze the effectiveness of depression treatment in palliative-care settings, we did not attempt to control for, or even monitor, ancillary interventions (e.g., psychotherapy, symptom-management). Rates of improvement in depression may be quite different in a randomized, controlled trial. Hence, the finding that improved depression was unrelated to prescribed antidepressant medications should not be taken as evidence that antidepressants are not useful in palliative-care settings. Rather, these results highlight the need for rigorous, controlled research in order to determine optimal treatment approaches for individuals with severe medical illness.
Another limitation in any study involving palliative-care patients is the problem of attrition. This study is no exception, and it demonstrates the difficulties in conducting longitudinal research in a population with advanced illness. Without access to patients who were lost to follow-up, it is not possible to determine whether any systematic bias might have existed (e.g., with more refractory patients being less likely to remain in the study). In an effort to deal with the problem of attrition, we applied sophisticated statistical procedures (i.e., HLM) that permit inclusion of even those individuals who are lost to follow-up. However, even these methods have limitations, and thus attrition may nevertheless have an unknown impact on study findings.
Notwithstanding our reliance on sophisticated statistical models, the modest sample size of individuals in our depression trajectory groups warrants note. This problem is, of course, inherent in any research focused on palliative-care patients, as problems with recruitment and attrition are inevitable and lead to sample sizes that are smaller than ideal. Despite the large sample size recruited for the baseline assessment, the division of those depressed patients available at follow-up (N=42) into even smaller categories based on response to treatment resulted in several small groups (e.g., the “Improved Late” group had only eight patients, and the “Became Depressed” group had only seven). Thus, the failure to observe significant differences in the proportion of patients with a high desire for hastened death may well reflect the limited power of these analyses. Further research regarding the impact of depression and its treatment is clearly necessary before firm conclusions can be drawn about these complex relationships.
The possibility that many patients who express a desire for hastened death are actually suffering from a treatable depression is a significant source of concern for palliative-care specialists, mental health clinicians, and healthcare policymakers. Although our findings do not suggest that desire for hastened death is always due to depression, it does demonstrate the importance of careful assessment for depression and, when present, aggressive treatment, particularly when patients articulate a desire for hastened death. Also, our finding that desire for hastened death may persist, in a small proportion of individuals, even in the absence of depression, highlights the importance of investigating other sources of despair that may also benefit from mental health intervention.
Acknowledgments
The authors express their gratitude to the several hundred patients with advanced AIDS who participated in this research study. We also thank Drs. Glenn Heller and Mithat Gonen from the Department of Epidemiology and Biostatistics, MSKCC; Louise Phillips, M.D., Medical Director of Rivington House; and the medical and nursing staffs of the Terrence Cardinal Cooke Health Care Center, Rivington House, and Coler-Gold-water Memorial Hospital.
This research was supported by a grant from the NIMH (MH R01-57629, W. Breitbart, P.I.).
References
- 1.Selwyn PA, Rivard M. Palliative care for AIDS: challenges and opportunities in the era of highly active antiretroviral therapy. J Palliat Med. 2003;6:475–487. doi: 10.1089/109662103322144853. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez v. Oregon, S. Ct. 04-623, 2006
- 3.Schiavo, ex. Rel. Schindler v. Schiavo, 2005, 544: U.S. 957
- 4.Rosenfeld B. Physician-assisted suicide and the right to die: the interface of social science, public policy, and medical ethics. Washington, D.C: American Psychological Association Press; 2004. [Google Scholar]
- 5.Meier DE, Emmons C, Wallenstein S, et al. A national survey of physician-assisted suicide and euthanasia in the United States. N Engl J Med. 1998;338:1193–1201. doi: 10.1056/NEJM199804233381706. [DOI] [PubMed] [Google Scholar]
- 6.Hudson PL, Kristjanson LJ, Ashby M, et al. Desire for hastened death in patients with advanced disease and the evidence base of clinical guidelines: a systematic review. Palliat Med. 2006;20:693–701. doi: 10.1177/0269216306071799. [DOI] [PubMed] [Google Scholar]
- 7.Breitbart W, Rosenfeld B, Pessin H, et al. Depression, hopelessness, and desire for death in terminally ill cancer patients. JAMA. 2000;284:2907–2911. doi: 10.1001/jama.284.22.2907. [DOI] [PubMed] [Google Scholar]
- 8.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State:” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 9.Rosenfeld B, Breitbart W, Gibson C, et al. Desire for hastened death among patients with advanced AIDS. Psychosomatics. 2006;47:504–512. doi: 10.1176/appi.psy.47.6.504. [DOI] [PubMed] [Google Scholar]
- 10.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV–TR Axis I Disorders. New York: Biometrics Research, NY State Psychiatric Institute; 2001. [Google Scholar]
- 11.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen-Cole SA, Stoudemire A. Major depression and physical illness: special considerations in diagnosis and biologic treatment. Psychiatr Clin North Am. 1987;10:1–17. [PubMed] [Google Scholar]
- 13.Rosenfeld B, Breitbart W, Stein K, et al. Measuring desire for death among patients with HIV/AIDS. Am J Psychiatry. 1999;156:94–100. doi: 10.1176/ajp.156.1.94. [DOI] [PubMed] [Google Scholar]
- 14.Rosenfeld B, Breitbart W, Galiatta M, et al. The Schedule of Attitudes Toward Hastened Death: measuring desire for death in terminally ill cancer patients. Cancer. 2000;88:2868–2875. doi: 10.1002/1097-0142(20000615)88:12<2868::aid-cncr30>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 15.Chochinov HMC, Wilson KG, Enns M, et al. Desire for death in the terminally ill. Am J Psychiatry. 1995;152:1185–1191. doi: 10.1176/ajp.152.8.1185. [DOI] [PubMed] [Google Scholar]
- 16.Bryk AS, Raudenbush SW. Hierarchical Linear Models in Social and Behavioral Research: Applications and Data Analysis Methods. Newbury Park, CA: Sage; 1992. [Google Scholar]
- 17.Raudenbush SW, Burk AS. Hierarchical Linear Models. 2. Newbury Park, CA: Sage; 2002. [Google Scholar]
- 18.Pinheiro JC, Bates DM. Statistics and Computing. New York: Springer; 2000. Mixed-Effects Models in S and S–PLUS. [Google Scholar]
- 19.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 20.Cohen J. Coefficient of agreement for nominal scales. Ed Psychol Meas. 1960;20:37–46. [Google Scholar]
- 21.Ganzini L, Lee MA, Heintz RT, et al. The effect of depression treatment on elderly patients’ preferences for life-sustaining medical therapy. Am J Psychiatry. 1994;151:1631–166. doi: 10.1176/ajp.151.11.1631. [DOI] [PubMed] [Google Scholar]