Abstract
Background
Although dialysis modality education is associated with higher rates of peritoneal dialysis (PD) use, some patients start hemodialysis (HD) despite initially selecting PD as their modality of choice. This study seeks to identify predictors of this discrepancy.
Study Design
Retrospective cohort study.
Setting & Participants
217 patients who received dialysis modality education at the University of Rochester between January 2004 and September 2009 and subsequently started dialysis.
Predictors
Demographic (age, race, gender, timing of education), social (education, income, insurance, marital, employment and smoking status) and clinical data (estimated glomerular filtration rate, cause of ESRD, number of comorbidities and number of nephrology visits in the year proceeding dialysis start).
Outcome
Hemodialysis use at initiation and day 91 of dialysis in patients initially choosing PD.
Results
Of the 217 patients receiving education and starting dialysis, 124 chose PD, 52 were undecided and 41 chose hemodialysis. The initial modality split was 150 with HD and 67 with PD. Of the 124 patients initially choosing PD, 59 started with PD and 65 started with HD. On day 91, 60 patients were on PD and 55 were on HD (Nine patients had either died, been transplanted, or hadn’t yet reached 91 days of dialysis). On multivariable analysis, age greater than 75 and not being employed predicted starting with HD, while age greater than 75, non white race and a non glomerular cause of ESRD predicted HD use at day 91.
Limitations
Single center observational study.
Conclusions
This study demonstrates that many patients choosing PD after dialysis education do not start with this modality, and also identifies several predictors of this mismatch. Further investigation into predictors of this discrepancy and strategies to promote starting PD when this modality is selected are warranted.
Introduction
The prevalence of end stage renal disease (ESRD) in the United States is increasing, imparting a heavy burden not only on people suffering with the disease but also on society with costs of $30 billion annually 1. Ideally, patients are identified as having chronic kidney disease (CKD) early, referred to a nephrologist and, in the case of progressive disease, educated about hemodialysis (HD), peritoneal dialysis (PD) and transplant. This allows patients time to consider their options and prepare for dialysis (i.e. by placement of an arteriovenous [AV] access or a PD catheter) before it is acutely needed.
In the United States, the current modality split is approximately 93% HD and 7% PD 1. Pre-dialysis education significantly alters this distribution- when fully educated and given a free choice, patients choose a home based therapy (typically PD) between 31 and 50% of the time 2–5. We have noted that not everyone choosing PD after education starts with this modality. This is concerning, as patients who choose PD and start HD may not have time to obtain AV access, relegating them to an urgent, catheter based start. On a societal level, HD is more expensive than PD. Recent data suggesting that an increase in PD prevalence to 15% would save >$1 billion over 5 years 1, 6.
As most studies examining the effect of education on initial modality consider only the starting modality, data are scant regarding the relationship between intended and actual modality. One previous study reported that 9 out of 10 patients who started dialysis from an initial cohort, started with their intended modality 7, but which modality these patients chose is not clear. We sought to determine predictors of mismatch between chosen and actual dialysis modality after education.
Methods
Population
This was a retrospective study encompassing all patients receiving dialysis modality education at the University of Rochester between January 1, 2004 and October 29, 2009. Patients who underwent education and subsequently started dialysis as of October 5, 2010 were included.
Patients choosing PD who received education within two weeks of starting dialysis were excluded, as starting PD would not be feasible in such a short period of time. Patients with a known medical contraindication for PD were also excluded.
Dialysis Modality Education
Patients were referred for dialysis modality education at the discretion of their treating nephrologist. The education consisted of one visit with a certified nephrology nurse, well versed in all aspects of renal replacement therapy. During the study period, a single nurse provided all the education. Patients were shown a video describing all modalities, and there was ample opportunity to ask questions. Patients were offered a tour of both the HD and PD unit. At the end of the session, the patients were asked either to state their preferred modality, indicate whether they were undecided or had decided to forego dialysis. There was an attempt to contact the patients after three months time, and patients could contact the educator to follow up as needed.
Data Extraction
Demographic data were extracted from the patients’ medical record and from the ESRD Medical Evidence (2728) form if available. Information collected included gender, race, ethnicity and age. Age was recorded as age in years at the time of dialysis modality education, and was analyzed as both a continuous variable, as well as a dichotomous one with a cut off of 75 years. We chose this cutoff, because USRDS data shows that this patients over age 75 have a lower rate of PD use compared with any other adult age group 1 Social data included average income of zip code of residence, education level, marital and employment history and smoking and insurance status. For purposes of analysis, smoking was characterized as ever vs. never, education was divided into high school or less vs. more than high school. Work status was divided into employed (or in school) vs. not employed. Marital status was categorized as married or not. Insurance was categorized either as government insurance (i.e. Medicare or Medicaid primary) or not.
Clinical data collected from the patients’ medical records and the 2728 form included body mass index (BMI), cause of ESRD (divided into diabetes vs. other and glomerular disease vs. other), number of comorbidities (as defined on the 2728 form), whether and when the patient had been seen by a nephrologist as an outpatient, and the estimated glomerular filtration rate (eGFR) both at time of first nephrology encounter, and at dialysis modality education. Participants were considered to have seen a nephrologist if they had at least one outpatient appointment prior to starting dialysis. Estimated GFR was obtained by laboratory estimate using the 4 variable modification of diet in renal disease equation 8, and was chosen as the GFR closest in time to the visit of interest. Also recorded was the time between education and the start of dialysis, and whether or not the patient started dialysis urgently in the hospital.
Statistical Analysis
Statistical analysis was done using STATA version 10 (STATA corp, www.stata.com).
Continuous data are reported as mean +/− standard deviation if normal, and as median, interquartile range if not. They were analyzed with the unpaired t-test or the Kolmogorov-Smirnov test depending on normality. Categorical data are reported as proportions, and were analyzed via the chi-squared test. All factors were analyzed using univariate analysis. Those with a p value of < 0.1 along with factors that have been previously shown to affect initial modality were then entered as dependent variables in logistic regression models, with initial modality (PD or HD) as the independent variable. A Chi-squared joint test was used to test whether the glomerular and diabetes cause variables were both different from 0. A p value of < 0.05 was considered significant.
Results
Modality Choice Based on Initial Selection
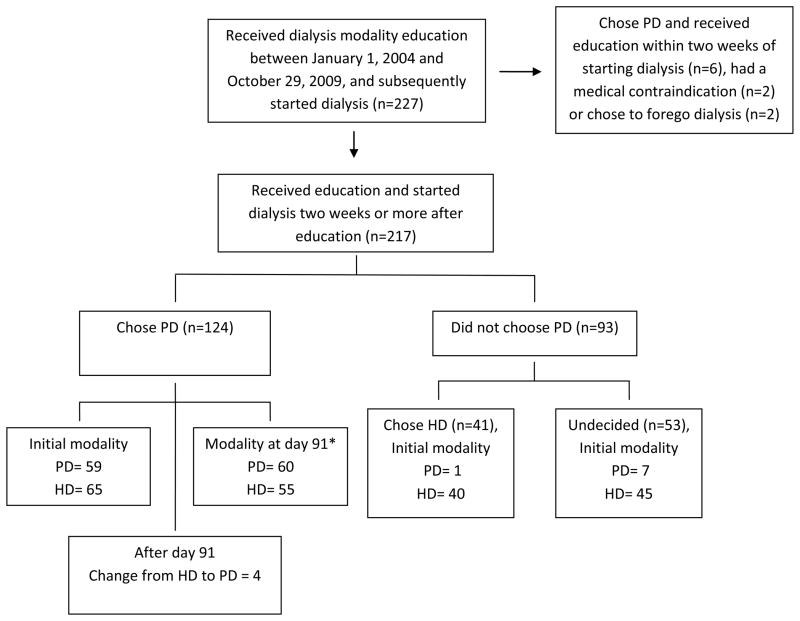
Of approximately 1800 incident dialysis patients over six years, 227 received education between January 1, 2004 and October 29, 2009. Of these, 8 patients choosing PD were excluded due to receiving education less than two week prior to starting dialysis (n=6) or having a medical contraindication to PD (n=2, one patient had surgery with involvement of the peritoneal cavity immediately before dialysis start, the other had a chronic indwelling drain of a blind intestinal loop, which was felt to confer too high of an infection risk). Two patients chose to forego dialysis. Of the remaining 217, 124 chose PD, 52 were undecided and 41 chose hemodialysis. Figure 1 shows the modality decision and ultimate disposition of these patients throughout the study. As a group, the PD patients were younger, less likely to be African American, and had education earlier than those not choosing HD (table 1A)
Figure 1.
Flow of patients through the study including provision of dialysis modality education, initial modality selection, initial starting modality and modality at day 91 and thereafter.
* 9 patients who started dialysis are not included in the day 91 modality due to death (n=5, transplant n=1, or not reaching 90 days of dialysis by study end (n=3).
Table 1.
Characteristics of patient stratified by chosen modality (1A) and starting modality (1B)
| A | ||||||
|---|---|---|---|---|---|---|
| Total (n=217) | PD (n=124) | HD (n=41) | Undecided (n=52) | Not choosing PD (n=93) | p value* | |
| Age (years) | 61.6 ± 15.1 | 59.5 ± 14.4 | 65.5 ± 16.8 | 63.7 ± 14.8 | 64.5 ± 14.4 | 0.01 |
| Age > 75 years | 47 (22%) | 17 (14%) | 16 (39%) | 14 (27%) | 30(32%) | 0.0009 |
| Gender (#, % male) | 111 (51%) | 60 (48%) | 23 (56%) | 28 (54%) | 61 (55%) | 0.34 |
| Race (#, % Caucasian) | 145 (67%) | 92 (73%) | 22 (54%) | 31 (56%) | 53 (55%) | 0.007 |
| Time between education session and RRT (weeks) | 25.9, 10.9–53.9 | 31.8, 12.5–54.7 | 21.3, 2–56.6 | 23.9, 7.9–49.4 | 23.3, 5.4–51 | 0.015 |
| GFR** (ml/min) | 15.5 ± 5.9 | 15.5 ± 6.0 | 14.9 ± 5.8 | 16.1 ± 5.9 | 15.5 ± 5.9 | 0.96 |
| Diabetes as cause of ESRD (#, %) | 91 (42%) | 55 (44%) | 16 (39%) | 20 (38%) | 36 (39%) | 0.41 |
| Glomerular disease as cause of ESRD (#, %) | 35 (16%) | 25 (20%) | 5 (12%) | 5 (10%) | 10 (11%) | 0.06 |
| B | |||||
|---|---|---|---|---|---|
| PD (n=67) | HD total (n=150) | HD choosing PD (n=65) | HD not choosing PD (n=85) | p value † | |
| Age | 58.7 ±13.8 | 62.9 ± 15.5 | 60.6 ± 15.4 | 64.7 ± 15.5 | 0.06 |
| Age > 75 years | 7 (10%) | 40 (27%) | 13 (20%) | 27 (32%) | 0.007 |
| Gender (#, % male) | 34 (51%) | 77 (51%) | 31 (48%) | 46 (54%) | 0.94 |
| Race (#, % Caucasian) | 52 (78%) | 93 (60%) | 47 (71%) | 46 (56%) | 0.01 |
| Time between education session and RRT (weeks) | 23.9, 12.9–50 | 27.5, 8–54 | 38.9, 11.9–57.2 | 23.7, 4.3–51 | 0.08 |
| GFR** (ml/min) | 15.2 ± 4.8 | 15.7 ± 6.4 | 15.8 ± 6.9 | 15.6 ± 6.0 | 0.58 |
| Diabetes as cause of ESRD (#, %) | 31 (46%) | 60 (40%) | 27 (42%) | 33 (39%) | 0.39 |
| Glomerular disease as cause of ESRD (#, %) | 17 (25%) | 18 (12%) | 10 (14%) | 8 (10%) | 0.01 |
Percentage calculations are based on patients in whom the variable of interest was known.
Data are presented as mean ± standard deviation if normal, and as median, 25th percentile – 75th percentile if not.
PD vs. not choosing PD,
GFR at time of education using 4 variable MDRD equation,
PD vs. HD total
In terms of initial dialysis modality, many more patients started HD (n=150), compared with PD (n=67). Almost all patients (40/41) choosing HD started with this modality, as did the majority of undecided patients (45/52), and more than half of those choosing PD (65/124). Those starting with HD were more likely to be over 75 years old, non Caucasian, and more likely to have a non diabetic, non glomerular disease as the cause of ESRD (table 1B)
Predictors of Initial Modality in Those Initially Choosing PD
Of the 124 patients choosing PD, 59 (48%) started with this modality, and 65 (52%) with HD. On univariate analysis, patients starting PD were more likely to be employed. Although the difference in mean ages of the groups was not statistically significant, significantly more of those starting HD were over 75 years old (20%) compared with PD (7%). Duration between education and dialysis start was not significantly different between the two groups, nor was time between initial nephrology visit and dialysis start, or number of nephrology visits in the year preceding dialysis. None of the other demographic, social or clinical factors were significant predictors of starting one modality over another (table 2A). On multivariable analysis (table 2B) age greater than 75 (OR= 4.3) predicted starting with HD, whereas being employed predicted a PD start (OR= 0.18 for an HD start or 5.6 for a PD start). The joint test of glomerular disease and diabetes as ESRD cause yielded a p value of 0.13. Despite the individual p value of 0.05 glomerular disease, our data do not support that cause of ESRD is a significant predictor of initial dialysis modality.
Table 2.
Univariate (2A) and multivariable analysis (2B) of factors associated with starting modality after an initial choice of PD
| A | |||
|---|---|---|---|
| Started PD (n=59) | Started HD (n=65) | p value | |
| Age (years) | 58.2 ± 13.5 | 60.6 ± 15.4 | 0.4 |
| Age > 75 years | 4 (7%) | 13 (20%) | 0.03 |
| Gender (% male) | 29 (49%) | 31 (48%) | 0.9 |
| Race (#, % Caucasian) | 45 (76%) | 47 (71%) | 0.5 |
| Ethnicity (#, % Hispanic) | 6 (10%) | 3 (5%) | 0.3 |
| Time* (weeks) | 24.9, 12.9–50 | 38.9, 11.9–57.3 | 0.4 |
| GFR** (ml/min) | 15.2 ± 4.9 | 15.8 ± 6.9 | 0.6 |
| Income | $41687± $16200 | $44027 ± $17545 | 0.4 |
| BMI | 29.7 ± 6.1 | 29.8 ± 7.3 | 1 |
| Diabetes as cause of ESRD (#, %) | 28 (47%) | 27 (42%) | 0.5 |
| Glomerular disease as cause of ESRD (#, %) | 15 (24%) | 10 (14%) | 0.2 |
| Comorbidities | 2, 1–3 | 2, 2–4 | 0.3 |
| Education (#, % more than high school) | 26 (49%) | 18 (45%) | 0.7 |
| Smoking (#, % ever) | 32 (54%) | 35 (55%) | 1 |
| Insurance (#, % government) | 31 (53%) | 38 (68%) | 0.1 |
| Employment Status (#, % working) | 14 (24%) | 3 (5%) | 0.004 |
| Marital Status (#, % married) | 37 (63%) | 33 (59%) | 0.68 |
| Time 2 † (weeks) | 126, 55.9–303.3 | 102.7, 10.3–230.4 | 0.8 |
| Number of visits in year preceding RRT | 5.8 ± 2.9 | 4.8 ± 3.0 | 0.07 |
| GFR2 †† (ml/min) | 24, 19–34 | 23.5, 16–31 | 0.95 |
| B | |||
|---|---|---|---|
| OR | p value | 95% CI | |
| Age > 75 years | 4.0 | 0.05 | 1.03–15.8 |
| Employed | 0.16 | 0.01 | 0.04–0.64 |
| Gender | 1.0 | 0.92 | 0.46–2.4 |
| Race | 1.7 | 0.26 | 0.67–4.3 |
| # of visits | 0.87 | 0.06 | 0.74–1.01 |
| Glomerular cause of ESRD ^ | 0.31 | 0.05 | 0.95 – 1.0 |
| Diabetes as cause of ESRD ^ | 0.57 | 0.24 | 0.23 – 1.4 |
Percentage calculations are based on patients in whom the variable of interest was known.
The joint test of glomerular disease and diabetes as cause of ESRD relative to other causes as a predictor of initial modality yielded a p = 0.13
Data are presented as mean ± standard deviation if normal, and as median, 25th percentile – 75th percentile if not.
Time between education session and RRT start,
GFR at time of education using 4 variable MDRD equation,
Time between first nephrologist visit and RRT start,
GFR at first nephrologist visit using 4 variable MDRD equation.
Modality day 91 and later time points
Of the 124 patients who chose PD and started HD, 115 were on dialysis at 91 days- 60 on PD, 55 on HD. Five patients died, one was transplanted and 3 had not yet reached 91 days of dialysis. Only 8 of the 65 HD patients initially choosing PD had transferred to PD by day 91. By univariate analysis, patients on HD at 90 days were more likely to be over 75 and have a longer duration between education and dialysis start (table 3A). Those on PD at 90 days were more likely to have a glomerular cause of ESRD. Age over 75 (OR= 7.8) and non white race (OR =2.7) predicts HD use at day 91 in the multivariable model (table 3B). In this case, the joint test of glomerular disease and diabetes does suggest that cause of ESRD predicts day 91 modality p=0.01). Given the larger effect of a glomerular cause of ESRD in predicting PD use (OR= 0.25 for an HD start or 3.9 for a PD start), it is likely that glomerular disease is in fact responsible for the findings of the joint test.
Table 3.
Univariate (3A) and multivariable analysis (3B) of factors associated with day 91 modality after an initial choice of PD
| A | |||
|---|---|---|---|
| PD (n=60) | HD (n=55) | p value | |
| Age (years) | 56.7 ± 12.8 | 61.1 ± 16.1 | 0.1 |
| Age > 75 years | 3 (5%) | 13 (24%) | 0.004 |
| Gender (#, % male) | 28 (47%) | 27 (49%) | 0.8 |
| Race (#, % Caucasian) | 44 (73%) | 40 (73%) | 0.94 |
| Ethnicity (#, % Hispanic) | 3 (5%) | 3 (6%) | 0.86 |
| Time*(weeks) | 22.4, 12–50.5 | 41.4, 12.7–63.1 | 0.05 |
| GFR**(ml/min) | 14.8 ± 5.2 | 16.4 ± 7.1 | 0.2 |
| Income | $41822 ± $16829 | $42642 ± $16125 | 0.79 |
| BMI | 29.1 ± 6.0 | 30.3 ± 7.1 | 0.35 |
| Diabetes as cause of ESRD (#, %) | 25 (42%) | 24 (44%) | 0.83 |
| Glomerular disease as cause of ESRD (#, %) | 16 (27%) | 6 (11%) | 0.03 |
| Comorbidities | 2, 1–3 | 2, 2–4 | 0.17 |
| Education (#, % more than high school) | 27 (52%) | 14 (39%) | 0.23 |
| Smoking (#, % ever) | 32 (54%) | 31 (56%) | 0.82 |
| Insurance (#, % government) | 31 (54%) | 32 (65%) | 0.26 |
| Employment Status (#, % working) | 12 (21%) | 5 (10%) | 0.13 |
| Marital Status (#, % married) | 39 (65%) | 27 (58%) | 0.42 |
| Time 2 † (weeks) | 122.3, 46.5–255.4 | 112.9, 51.7–261.1 | 0.81 |
| Number of visits in year preceding RRT | 5.2 ± 2.8 | 5.2 ± 3.2 | 0.97 |
| GFR 2 †† (ml/min) | 23, 16.5–33 | 25, 17.5–32 | 0.95 |
| B | |||
|---|---|---|---|
| OR | P value | 95% CI | |
| Age > 75 | 7.8 | 0.001 | 2.4–25.2 |
| Time* | 1.0 | 0.77 | 0.99–1.01 |
| Non white race | 2.7 | 0.006 | 1.3 – 5.5 |
| gender | 1.1 | 0.93 | 0.54–2.0 |
| Glomerular cause of ESRD^ | 0.25 | 0.004 | 0.10–0.64 |
| Diabetes as cause of ESRD ^ | 0.92 | 0.22 | 0.45 – 1.9 |
Percentage calculations are based on patients in whom the variable of interest was known.
The joint test of glomerular disease and diabetes as cause of ESRD relative to other causes as a predictor of day 91 modality yielded a p = 0.01.
Data are presented as mean ± standard deviation if normal, and as median, 25th percentile – 75th percentile if not.
Time between education session and RRT start,
GFR at time of education using 4 variable MDRD equation,
Time between first nephrologist visit and RRT start,
GFR at first nephrologist visit using 4 variable MDRD equation.
After 91 days, only four additional patients transferred to HD from PD, with a mean follow time of approximately two years.
Effect of modality mismatch on mortality
Thirteen (6%) out of the initial cohort of 217 died within 90 days, and 30 (14%) were dead at one year. Initial choice of modality did not predict mortality at either time point. For the cohort as a whole, 90 day and one year mortality were associated an HD start, older age and starting dialysis urgently. When considering only those who chose PD, starting HD, older age and an urgent dialysis start were associated with a higher risk of death at 90 days and at one year. White patients were more likely to die over one year compared with non white patients. No other variable predicted mortality at either 90 days or one year. The only significant variable on multivariable analysis is the initial mode related to 90 day mortality(data not shown).
Factors Occurring Between Education and Initiation
In patients initially choosing PD, there were 40 urgent, hospital based starts. Urgent starts were much were in HD patients (n=38), comparing with PD (n=2, p<0.0001). In addition, 13 patients choosing PD but starting HD had a permanent access in place.
Discussion
This study shows that many patients start hemodialysis despite choosing PD as their modality of choice, and only a minority of patients transition to PD. We found few predictors of this mismatch- age over 75 years, employment status and, to a degree, etiology of ESRD and, to a degree, non white race. Our study is unique in that it considers the initial dialysis modality choice by patient, not only the actual dialysis modality used.
Age over 75 years predicted an HD start in our cohort, even in those selecting PD. This finding correlates with USRDS data for Medicare Part D enrollees which show the incidence of PD start in those over 75 to be less than half that of younger patients 1 and with a study by Stack where patients starting PD were likely to be younger than those starting HD 9. There are many potential reasons for this mismatch in elderly patients. Some physicians believe that elderly patients do not do as well on PD compared with HD10. While this is supported by some (but not all) registry studies 11, the only prospective study examining modality and outcome in elderly patients demonstrated no differences in mortality and quality of life 12, 13. Medical and/or social contraindications are also important, and these will be discussed more fully below.
Employment status as a predictor of PD use has been previously reported. Stack found PD patients were more likely to be working full time compared with HD patients 9. Being employed was also associated with PD use in a British 14 and a Taiwanese cohort 15. In a qualitative study, 45% of new start PD patients cited the flexibility of treatment and the ability to continue working as a major factor in their modality decision, whereas none of the HD patients did so 16.
The complex of the decision making process may explain why we did not find many predictors of the observed mismatch. Patient related, physician related and disease related factors may all contribute.
In terms of patient related factors, Finkelstein et al. reported that 35% of all CKD patients have very limited or no knowledge of their kidney disease 17, and NHANES data showed that less than half of patients with advanced CKD are aware of it 18. There are cognitive deficits associated with CKD 19–21, and patients have commented they did not “catch on to” all of the options presented as they were “so sick at the time” 22. As patients in our study waited over 40 weeks between the education and starting dialysis, it likely the some of the imparted information was not retained.
Patients initially choosing PD may simply change their mind over time. This study did not track whether patients initially choosing PD consciously decided against it prior to starting dialysis. This was likely for the 13 patients who started HD with an AV access already in place, and possible some of the remaining patients, as catheter start would be inevitable if patients changed their minds late in their disease course.
Family members may influence a patient’s modality decision 23. A patient selecting PD may reverse this decision if they do not feel supported by family. Focus group data reveal that ESRD patients are concerned about the effects of dialysis on their family, and affirm the importance of family involvement in, and acceptance of, their modality choice 24. In one study family members opinion was an important determination in modality selection for one half of incident PD patients 16. We did not track whether patients had someone with them during the educational session. Having family present during the education session may serve two purposes. A “second pair of ears” may lead to better understanding and retention of the information presented, and family members present at the session may be able to vocalize their objections to a particular modality choice immediately, such that a patient who may have chosen PD if alone, will no longer do so with their family member(s) present.
Peer influence may also explain some of the discrepancy, as patients are influenced by other patients 22. Hearing about a particularly good or bad experience with a particular dialysis modality after DME may cause patients to change their initial decision. Our data did not capture whether patients knew and/or sought input from current dialysis patients.
Provider opinion, especially that of the nephrologist, may influence patient choice of modality. Wuerth et al. found that almost 90% of patients felt their physician influenced their modality selection 16. A patient initially enthusiastic about PD may be dissuaded if this decision is not supported by his or her nephrologist. Our patient population was referred for DME by 13 different nephrologists each with his or her own perspective on modality selection which undoubtedly influenced individual patients.
Physician opinion of a patient’s suitability for PD may lead to mismatch between chose and actual modality. Mendlesson et al. found 13% of all CKD patients were deemed medically ineligible for PD, by their provider 25. This may be an overestimation of true ineligibility however, as several of the cited contraindications, including older age, multiple abdominal surgeries, and obesity are not university accepted as such 26–29. Nonetheless, perceived, rather than absolute medical contraindications are important, as these perceptions may lead some physicians to discourage PD for a patient who is able use this modality.
Social barriers to PD use are somewhat more common than medical contraindications, with 17% of CKD patients being deemed socially ineligible for PD 25. Again, this may be an overestimation as some of the barriers cited may not be true barriers at all (such as age), or may be overcome with intense family support or assisted PD (such as the inability to due PD by oneself, compliance issues and cognitive issues) 30. However, as above, the existence of one of these factors may be enough for a nephrologist to abandon PD as a viable option despite a patient’s selection of this modality.
With the exception of the two patients excluded at the outset, our study did not examine the role of medical and social barriers (perceived or real) to the use of PD, especially those developing between time of education and dialysis start. Certainly this may have contributed to the observed mismatch between chosen and actual modality, particularly in the elderly in whom these contraindications are more prevalent.
Disease related factors are another potential contributor to modality mismatch. In our study 57% of the patients choosing PD but starting HD started in the hospital, the vast majority with central venous catheters The large number of unplanned, urgent dialysis starts in our population is concerning, and although not necessarily so, it is likely that many of these patients had either a rapid progression of CKD or a superimposed acute event requiring an urgent, hospital based start. Separating out which of these patients truly had an unforeseeable event requiring emergent RRT start from those who “fell through the cracks” is important, as the latter may be amenable to specific interventions designed to enhance follow up whereas the former would not.
Finally, factors specific to the educational session itself may have some bearing on initial dialysis modality. There is no consensus on the best way to educate CKD patients, and it is conceivable that the method used in our institution is not optimal. There was an attempt to contact patients after three months to follow up, but it is not clear how often this contact was successful. The vast majority of patients did not have return visits for education, and although they were encouraged to call with questions, only approximately 10% did so. All education done for this cohort was completed prior to the institution of the Medicare Improvement for Patients and Providers Act, which funds up to six educational sessions of CKD. It is possible that with multiple educational sessions many of the potential issues discussed above could have been identified and modality selection modified, if appropriate.
Our study has several strengths. Tracking patients from modality selection to start of dialysis provides a starting point for future interventional strategies, and provides baseline data against which we may gauge their success. Also, our follow up was complete, in that all of the patients started dialysis in our catchment area.
There are several limitations of this study. Our cohort was small in size and is a single centered such that our findings may not be applicable to other institutions or practices due to differences in patient demographics, provider opinion on optimal dialysis modality and structure of the pre-ESRD education program.
Our analysis was limited to those variables which could be extracted from our dataset, namely quantitative metrics. For a complex decision such as dialysis modality selection, there are factors involved which are not accessible via a quantitative approach. Previous studies using focus groups and patient interviews have identified qualitative considerations, including flexibility of schedule, privacy considerations, the ability to continue working, and effects of the modality on the family 16, 23, 24. These were not explored in this study.
In conclusion, over half the patients who choose PD start dialysis with HD, many of them urgently. We found that age over 75, and employment status predicts starting with HD when PD is chosen, and age over 75 and a non glomerular etiology of ESRD predict HD use day 91. These findings help define a group who should be carefully monitored to ensure they start PD, if this remains their modality choice. Closer examination of the events occurring between education and dialysis start is needed to determine the root cause of HD starts in those choosing PD, paying particular attention to the development of medical/social contraindications, superimposed acute kidney injury or rapid progression of CKD and losses to follow up in patients with established nephrology care. Qualitative analysis of this decision making process looking at factors such as family support and conscious change of modality choice is also warranted.
Acknowledgments
Part of this work was presented in abstract form at the annual meeting of the American Society of Nephrology, November 16 to 21, 2010, Denver, CO. This work was supported by the Buswell Fellowship award (University of Rochester School of Medicine) to S.L.
The University of Rochester Buswell fellowship award provided funding for this project.
References
- 1.Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; 2009. [Google Scholar]
- 2.Goovaerts T, Jadoul M, Goffin E. Influence of a Pre-Dialysis Education Programme (PDEP) on the mode of renal replacement therapy. Nephrol Dial Transplant. 2005;20(9):1842–1847. doi: 10.1093/ndt/gfh905. [DOI] [PubMed] [Google Scholar]
- 3.Jager KJ, Korevaar JC, Dekker FW, Krediet RT, Boeschoten EW. The effect of contraindications and patient preference on dialysis modality selection in ESRD patients in The Netherlands. American Journal of Kidney Diseases. 2004;43(5):891–899. doi: 10.1053/j.ajkd.2003.12.051. [DOI] [PubMed] [Google Scholar]
- 4.Little J, Irwin A, Marshall T, Rayner H, Smith S. Predicting a patient’s choice of dialysis modality: Experience in a United Kingdom renal department. American Journal of Kidney Diseases. 2001;37(5):981–986. doi: 10.1016/s0272-6386(05)80014-9. [DOI] [PubMed] [Google Scholar]
- 5.Prichard S. Treatment modality selection in 150 consecutive patients starting ESRD therapy. Perit Dial Int. 1996;16(1):69–72. [PubMed] [Google Scholar]
- 6.Neil N, Guest S, Wong L, et al. The financial implications for medicare of greater use of peritoneal dialysis. Clinical therapeutics. 2009;31(4):880–888. doi: 10.1016/j.clinthera.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Manns BJ, Taub K, VanderStraeten C, et al. The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: A randomized trial. Kidney Int. 2005;68(4):1777–1783. doi: 10.1111/j.1523-1755.2005.00594.x. [DOI] [PubMed] [Google Scholar]
- 8.Levey A, Greene T, Kusek J, Beck G. A simplified equation to predict glomerular filtration rate from serum creatinine [Abstract] J Am Soc Nephrol. 2000;11(155A) [Google Scholar]
- 9.Stack AG. Determinants of Modality Selection among Incident US Dialysis Patients: Results from a National Study. J Am Soc Nephrol. 2002;13(5):1279–1287. doi: 10.1681/ASN.V1351279. [DOI] [PubMed] [Google Scholar]
- 10.Teitelbaum I. Peritoneal dialysis is appropriate for elderly patients. Contrib Nephrol. 2006;150:240–246. doi: 10.1159/000093600. [DOI] [PubMed] [Google Scholar]
- 11.Lo W-K. Peritoneal dialysis utilization and outcome: what are we facing? Perit Dial Int. 2007;27(Supplement 2):S42–47. [PubMed] [Google Scholar]
- 12.Harris S, Lamping D, Brown E, Constantinovici N North Thames Dialysis Study Group. Clinical outcomes and quality of life in elderly patients on peritoneal dialysis versus hemodialysis. Perit Dial Int. 2002;22(4):463–470. [PubMed] [Google Scholar]
- 13.Lamping DL, Constantinovici N, Roderick P, et al. Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: a prospective cohort study. The Lancet. 2000;356(9241):1543–1550. doi: 10.1016/S0140-6736(00)03123-8. [DOI] [PubMed] [Google Scholar]
- 14.Little J, Irwin A, Marshall T, Rayner H, Smith S. Predicting a patient’s choice of dialysis modality: Experience in a United Kingdom renal department. American Journal of Kidney Diseases. 2001;37(5):981–986. doi: 10.1016/s0272-6386(05)80014-9. [DOI] [PubMed] [Google Scholar]
- 15.Huang HC, Wang JY, Chang CC, Chiu PF, Chiang M-C, Yang Y. Nonclinical Factors Associated With Treatment With Peritoneal Dialysis In ESRD Patients In Taiwan. Perit Dial Int. 2010;30(6):638–43. doi: 10.3747/pdi.2009.00112. [DOI] [PubMed] [Google Scholar]
- 16.Wuerth D, Finkelstein S, Schwetz O, Carey H, Kliger A, Finkelstein F. Patients’ descriptions of specific factors leading to modality selection of chronic peritoneal dialysis or hemodialysis. Perit Dial Int. 2002;22(2):184–190. [PubMed] [Google Scholar]
- 17.Finkelstein FO, Story K, Firanek C, et al. Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int. 2008;74(9):1178–1184. doi: 10.1038/ki.2008.376. [DOI] [PubMed] [Google Scholar]
- 18.Nickolas TL, Frisch GD, Opotowsky AR, Arons R, Radhakrishnan J. Awareness of kidney disease in the US population: Findings from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2000. American Journal of Kidney Diseases. 2004;44(2):185–197. doi: 10.1053/j.ajkd.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 19.Hailpern SM, Melamed ML, Cohen HW, Hostetter TH. Moderate Chronic Kidney Disease and Cognitive Function in Adults 20 to 59 Years of Age: Third National Health and Nutrition Examination Survey (NHANES III) J Am Soc Nephrol. 2007;18(7):2205–2213. doi: 10.1681/ASN.2006101165. [DOI] [PubMed] [Google Scholar]
- 20.Khatri M, Nickolas T, Moon YP, et al. CKD Associates with Cognitive Decline. J Am Soc Nephrol. 2009;20(11):2427–2432. doi: 10.1681/ASN.2008101090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yaffe K, Ackerson L, Tamura MK, et al. Chronic Kidney Disease and Cognitive Function in Older Adults: Findings from the Chronic Renal Insufficiency Cohort Cognitive Study. Journal of the American Geriatrics Society. 2010;58(2):338–345. doi: 10.1111/j.1532-5415.2009.02670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morton RL, Tong A, Howard K, Snelling P, Webster AC. The views of patients and carers in treatment decision making for chronic kidney disease: systematic review and thematic synthesis of qualitative studies. BMJ J. 2010;340:c112–c122. doi: 10.1136/bmj.c112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray MA, Brunier G, Chung JO, et al. A systematic review of factors influencing decision-making in adults living with chronic kidney disease. Patient education and counseling. 2009;76(2):149–158. doi: 10.1016/j.pec.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 24.Lee A, Gudex C, Povlsen JV, Bonnevie B, Nielsen CP. Patients’ views regarding choice of dialysis modality. Nephrol Dial Transplant. 2008;23(12):3953–3959. doi: 10.1093/ndt/gfn365. [DOI] [PubMed] [Google Scholar]
- 25.Mendelssohn DC, Mujais SK, Soroka SD, et al. A prospective evaluation of renal replacement therapy modality eligibility. Nephrol Dial Transplant. 2009;24(2):555–561. doi: 10.1093/ndt/gfn484. [DOI] [PubMed] [Google Scholar]
- 26.Brown EA. Peritoneal dialysis for older people: Overcoming the barriers. Kidney Int. 2008;73(S108):S68–S71. doi: 10.1038/sj.ki.5002604. [DOI] [PubMed] [Google Scholar]
- 27.Castrale C, Evans D, Verger C, et al. Peritoneal dialysis in elderly patients: report from the French Peritoneal Dialysis Registry (RDPLF) Nephrol Dial Transplant J. 2010;25(1):255–262. doi: 10.1093/ndt/gfp375. [DOI] [PubMed] [Google Scholar]
- 28.Chen S-Y, Chen T-W, Lin S-H, Chen C-J, Yu J-C, Lin C-H. Does previous abdominal surgery increase postoperative complication rates in continuous ambulatory peritoneal dialysis? Perit Dial Int. 2007;27(5):557–559. [PubMed] [Google Scholar]
- 29.Snyder JJ, Foley RN, Gilbertson DT, Vonesh EF, Collins AJ. Body size and outcomes on peritoneal dialysis in the United States. Kidney Int. 2003;64(5):1838–1844. doi: 10.1046/j.1523-1755.2003.00287.x. [DOI] [PubMed] [Google Scholar]
- 30.Oliver MJ, Garg AX, Blake PG, et al. Impact of contraindications, barriers to self-care and support on incident peritoneal dialysis utilization. Nephrol Dial Transplant. 2010;25(8):2737–2744. doi: 10.1093/ndt/gfq085. [DOI] [PubMed] [Google Scholar]