Abstract
Background
Non-adherence to statins limits the benefits of this common medication. Individual studies assessing predictors of non-adherence have produced inconsistent results.
Objective
The objective of this systematic review and meta-analysis was to identify reliable predictors of non-adherence to statins.
Methods
Multiple databases, including Medline, EMBASE and Psychinfo, were searched to identify studies that evaluated predictors of non-adherence to statins. Studies were selected using a priori defined criteria, and each study was reviewed by 2 authors who abstracted data on study characteristics and outcomes. Relative risks were then pooled using an inverse-variance weighted random-effects model.
Results
Twenty-two cohort studies met inclusion criteria. Age had a U-shaped association with adherence; the oldest (≥ 70 years) and youngest (< 50 years) had lower adherence than the middle-aged (50–69 years). Women and those with lower incomes were more likely to be non-adherent than men [odds of non-adherence 1.07 (95% CI 1.04 – 1.11)] and those with higher income [odds of non-adherence 1.18 (95% CI 1.10 – 1.28)], respectively. A history of cardiovascular disease predicted better adherence to statins [odds of non-adherence 0.68 (95% CI 0.66–0.78)]. Similarly, a diagnosis of hypertension or diabetes was associated with better adherence. Although there were too few studies for quantitative pooling, increased lipid testing and lower out-of-pocket costs appeared to be associated with better adherence. There was substantial (I2 range 68.7–96.3%) heterogeneity between studies across factors.
Conclusion
Several socio-demographic, medical, and healthcare utilization characteristics are associated with statin non-adherence. These factors may be useful guides for targeting statin adherence interventions.
Keywords: statins, meta-analysis, adherence, predictors
Introduction
Statins are highly effective medications for avoiding cardiovascular events.1, 2 Accordingly, their use has become widespread and continues to increase.3 Despite a favorable side-effect profile in a majority of patients4 and evidence that low adherence to statins is linked with worse outcomes5–7, numerous studies have documented high rates of non-adherence to statins.8, 9 Identifying patients with low adherence is a challenge. Using clinical judgment alone, physicians are poor at identifying which patients have problems with adherence.10, 11
Much of the research on statin adherence is derived from large insurance and pharmacy databases. These studies have generated a list of potential predictors of non-adherence. Previous reviews of these predictors have observed a wide variation in the types of predictors considered.12, 13 Moreover, these reviews have qualitatively concluded that there are no consistent socio-demographic or medical predictors of non-adherence.13
The variability in the identification of predictors of non-adherence may stem from the diversity of study designs, populations, measurement methodologies as well as secular trends in statin use. Previous reviews have elected to systematically evaluate adherence predictors, without performing a quantitative pooling of data.12, 13 Identification of consistent predictors of statin adherence across populations and studies may provide targets for the development of effective interventions to improve statin adherence. To expand our understanding of factors associated with non-adherence to statins, we performed a review of the literature and quantitative pooling of prior studies. We examined observational studies to assess the relationship between individual level characteristics and statin non-adherence.
Methods
Study Selection
Eligible study designs included prospective or retrospective observational cohorts in which adherence to statins was evaluated as an outcome measure. Articles were only considered if they were available in full text in English and if they included community dwelling, adult patients 18 years of age and older. Eligible studies measured adherence using either a validated self-report scale or objective measures of adherence including medication refill data, pill counts, or electronic medication monitoring. To be included, studies also had to have a description of the study design and the analysis had to report on at least two predictors of adherence to statins in a multivariable analysis with relative risks. As per pre-specified criteria, studies with fewer than 50 participants were excluded because accurate characterization of the predictive strength of multiple independent features would be weakened (i.e., potential for “over fitting” of the models).
Searching
This study was performed as part of a larger systematic review of predictors of adherence to oral cardiovascular and diabetic medications. All methods were informed by the meta-analysis of observational studies in epidemiology (MOOSE) criteria.14 Potentially relevant articles were identified by searching publicly available computerized databases with the assistance of a trained medical librarian (L.F.). The search included all articles published from inception to February 2009 from MEDLINE, Cochrane Central Register of Controlled Trials, Database of Abstracts of Reviews of Effects, National Health Service Economic and Evaluation Database, Health Technology Assessment Database, EMBASE, and PsycINFO. All relevant subject heading and free text terms used to represent cardiovascular disease or diabetes were combined with terms for adherence or compliance. For this substudy, terms for both the generic class of drug (statins) and the individual names, generic and proprietary, were included. Due to the very large volume of literature on this topic, a set of methodological terms (or filter) was applied to the search strategies of the larger databases (MEDLINE, EMBASE and PsycINFO) to capture relevant study designs.
Study selection and quality
Two investigators (D.M., I.K.), working independently, reviewed all of the abstracts and obtained the full text of potentially relevant articles. After applying the study selection criteria noted above, the two reviewers met to achieve consensus on candidate abstracts for full text, methodological review. In cases when limited information was available from the abstract, the full text of the article was always obtained. After obtaining full text of these studies, the same reviewers independently assessed eligibility using a predefined protocol.15
Several additional quality measures were incorporated at this stage. Studies were only included if they measured adherence using either a validated self-report scale or an objective measure of adherence (medication refill data, pill counts, or electronic medication monitoring). A number of sociodemographic characteristics, comorbid medical conditions, and regimen complexity qualities have been known to affect statin adherence.8 Accordingly, as a second quality filter, we only included studies that adjusted for at least one characteristic in their analysis of the association between candidate predictors and adherence to statins. Finally, as we were interested in deriving a quantitative estimate of the strength of candidate predictors of statin adherence, we excluded articles in which relative risks and a measure of its variance were not reported. The two authors met again after selecting articles based on these quality measures to discuss discrepancies and achieve consensus for final eligibility in this meta-analysis.
Data Extraction
Data from the identified studies were abstracted independently using a standardized form. Data abstractors (D.M., I.K.) collected information about the country of origin, study populations, sample size, method of adherence measurement, mean adherence, and predictors of adherence. When more than one adherence measurement technique was used, data on all measures used were extracted separately. For studies with incomplete quantitative information available on predictors, attempts were made to obtain data from study authors.
Data Synthesis
Studies were grouped together based on the type of adherence measure utilized (validated self-report scale, pharmacy or insurance claims refill data, pill counts, or electronic medication monitoring). Those relying on pharmacy or insurance claims refill data calculated adherence using two types of measures. The first type is usually referred to as the proportion of days covered (PDC) and is calculated as the sum of the days’ supply obtained between the first and the last pharmacy fill divided by the total number of days in this time period.16 This measure is dichotomized and individuals are categorized into adherent and non-adherent groups using a set threshold for PDC (usually 80%). The second adherence measure categorizes patients as adherent or non-adherent depending on whether individuals discontinued their medication over a set time period (usually 1 or 2 years).
Data Analysis
Predictors were selected for quantitative pooling if 4 or more articles employing similar adherence measurement techniques were available. Several studies presented data only in subgroups and performed all analyses as distinct populations (e.g. by gender, age, history of CVD, etc.).17–19 As such, these data were treated as multiple studies within the same manuscript. Individual estimates of relative risk were pooled using random effects meta-analysis with inverse variance weighting20 in Stata, version 10 (College Station, TX). In cases when publications displayed results for distinct subgroups (e.g., men and women), the subgroups were included as separate terms in the meta-analysis. Pooled estimates were calculated separately for PDC and discontinuation, as well as for an overall estimate combining the two outcomes. The I2 statistic was used to estimate the percentage of variability across studies that is attributable to heterogeneity20, and tested for deviation from zero. Quantitative variables were typically reported in ordinal grouped format. If the raw data suggested a monotonic trend, we pooled relative risks comparing the highest to the lowest group (e.g., for income). Where there was no such monotonic relationship, and no clear parametric response relationship, we plotted individual studies rather than pooling (e.g., for age). To test for potential sources of heterogeneity between studies, subgroup analyses were performed on each of the final predictors by country of origin (North America vs. Other), and by the median sample size (N=20,000), year of study (2005) and duration of follow-up (5 years).
Results
Search Results
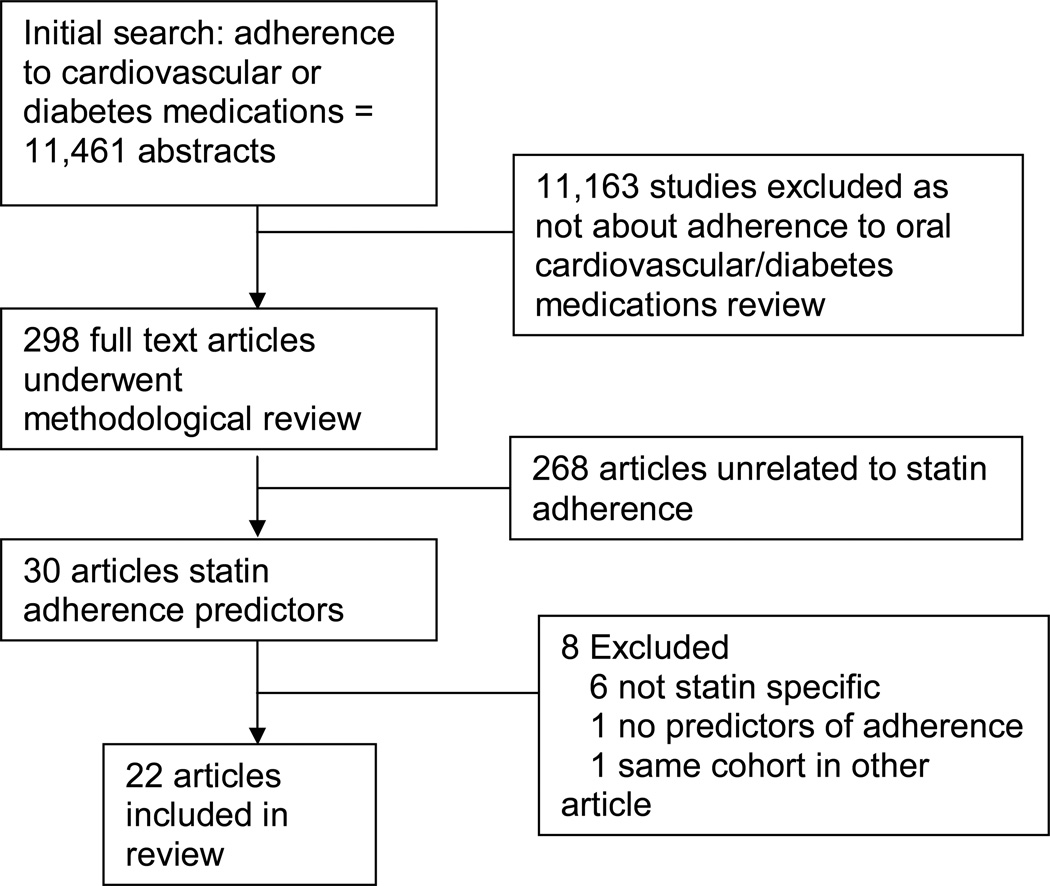
A comprehensive search was performed in March 2009 and yielded a total of 11,461 unique articles. Figure 1 shows the flow of literature into the systematic review. A total of 22 articles met the final inclusion criteria for the study of predictors of adherence to statins (See Table 1). Only 1 article reported statin adherence using a validated self-report scale21 and no articles reported statin adherence using either electronic medication monitoring or pill-counts. As a result, only studies using pharmacy and insurance database refill rates were included for meta-analysis. As depicted in Figures 2–6, the pooled estimates for the two outcomes (PDC and discontinuation) were similar, justifying use of an overall pooled estimate as an appropriate measure of association.
Fig 1.
Flowchart of the systematic literature review
Table 1.
Characteristics of Statin Non-Adherence Predictors Studies
| Source | Country | Sample Size |
Adherence Measure: PDC, Discontinuation, Both, Self Report |
Predictors | Maximum follow-up duration |
% Adherent |
|---|---|---|---|---|---|---|
| Ellis et al. (2004)30 | US | 4802 | Both | Age, Gender, Race, MI, Visits, Lipid Testing, Costs | 3 years |
a 3 years: 62.2% PP; a 3 years: 61.2% SP |
| Benner et al. (2004)22 | US | 19422 | PDC | Age, Gender, Income, Depression, MI, HTN, DM, Regimen Complexity, Visits. Lipid Testing | 2 years | 3 months: 51% 6 months: 36% 1 year: 30% 2 years: 27% 3 years: 25% |
| Donnelly et al. (2008)27 | UK | 6462 | PDC | Age, Gender, MI, HTN, DM | 13 years | 3 months: 94% 1 year: 66% 5 years: 75% 10 years: 68% |
| Howell et al. (2001)32 | UK | 1010 | PDC | Age, Gender, MI, HTN, DM, Lipid Testing | 12 years | 12 years: 75% |
| Caspard et al. (2005)23 | US | 4776 | Both | Age, Gender | 5 years | 6 months: 80% 1 years: 74% 2 years:65% 3 years:61% |
| Benner et al. (2002)9 | US | 34501 | PDC | Age, Gender, Race, MI, HTN, DM, Regimen Complexity, Visits, Depression | 10 years | 3 months: 79% 6 months: 56% 1 year: 50% 10 years: 42% |
| Avorn et al. (1998)8 | US/Canada | 7287 | PDC | Age, Gender, MI, HTN, DM, Regimen Complexity, Visits, Statin naïve | 1 year | NA |
| Mann et al. (2007)21 | US | 71 | Self-reportc | Age, Race | 6 months | 6 months: 43% |
| Yu et al.33 | US | 19038 | Both | Age, Gender, MI, HTN, DM, Visits | 2.5 years | 6 months: 66% 1 year: 59.3% |
| Perrault et al. (2005)31 | Canada | 17958 | Discontinuation | Age, Gender, Income, HTN, DM, Regimen Complexity, Visits | 3 years |
b 6 months: 65%(PP) b 6 months: 71% (SP) b 3 years: 35% (PP) b 3 years: 45% (SP) |
| Larsen et al. (2002)24 | Denmark | 3623 | Discontinuation | Age, Gender | 5 years | Not reported |
| Chodick a et al. (2008)17 | Israel | 136052 | Discontinuation | Age, Gender, Income, HTN, DM, Visits | 10 years | 3 years: 37% |
| Chodick b et al. (2008)17 | Israel | 93866 | Discontinuation | Age, Gender, Income, HTN, DM, Visits | 10 years | 4 years: 23% |
| Yang et al. (2002)25 | UK | 22408 | Discontinuation | Age, Gender, Regimen Complexity, Visits | 8 years | 1 year: 70% |
| Abraha et al. (2003)26 | Italy | 39222 | Discontinuation | Gender, MI, HTN, DM | 4.5 years | 4.5 years: 13% |
| Hudson et al. (2007)18 | Canada | 34735 | Discontinuation | Age, HTN, DM, Regimen Complexity, Visits | 5 years | 2 years: 78% (M) 2 years: 80% (W) 5 years: 63% (M) 5 years: 68% (W) |
| Schneeweiss et al. (2007)29 | US | 31561 | PDC | Age, Gender, Income, MI, HTN, DM, Visits, Costs | 9 months | 9 months: 56% (Baseline) 51% (After cost increase) |
| Vinker et al. (2008)28 | Israel | 47680 | PDC | Age, Gender, Income | 8 years | 1 year: 39% 3 years: 18% 6 years: 10% |
| Jackevicius et al. (2002)34 | Canada | 22379 | Discontinuation | Age, Gender, MI, HTN, DM, Regimen Complexity, Visits | 2 years | 2 years: 40% ACS 36% CAD 25% PP |
| Rasmussen et al. (2007)19 | Denmark | 30078 | Discontinuation | Income | 6 years | NA |
| Rasmussen et al. (2007)5 | Canada | 17823 | PDC | Age, Gender, Income, HTN, DM, | 4 years | 1 year: 87.5% |
| Eagle et al. (2004)35 | 14 countries, 4 continents: NA, SA, Europe, Australia | 6320 | Discontinuation | HTN, DM | 1 year | 5 mo – 1 year: 13% discontinued statin |
| Hsu et al. (2006)36 | US | 199179 | PDC | Costs | 1 year | NA |
MI – Myocardial infarction or cardiovascular disease (CVD) equivalent
Comorbidities – comorbidities excluding hypertension (HTN), diabetes (DM) and CVD
ACS: acute coronary syndrome; CAD: chronic coronary artery disease; PP: primary prevention; SP: secondary prevention
These data reflect PDC only
These data reflect PDC only
Only included paper to not use pharmacy/claims refill data, used validated Morisky Scale
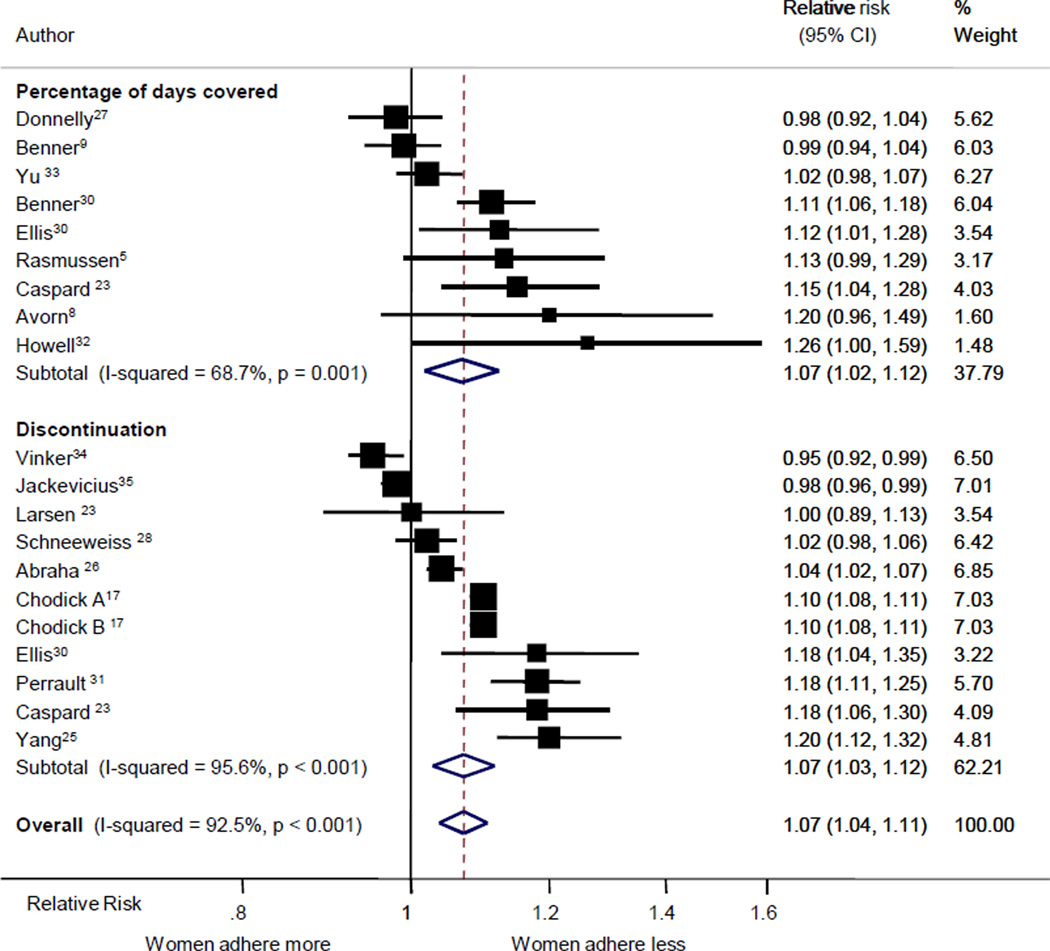
Fig 2.
Forest plot of relative risks for non- adherence comparing women to men. The center of each box is plotted at the relative risk for that study; the boxes are drawn in proportion to the amount of statistical information provided by that study; and the lines go out to the 95% confidence limits.
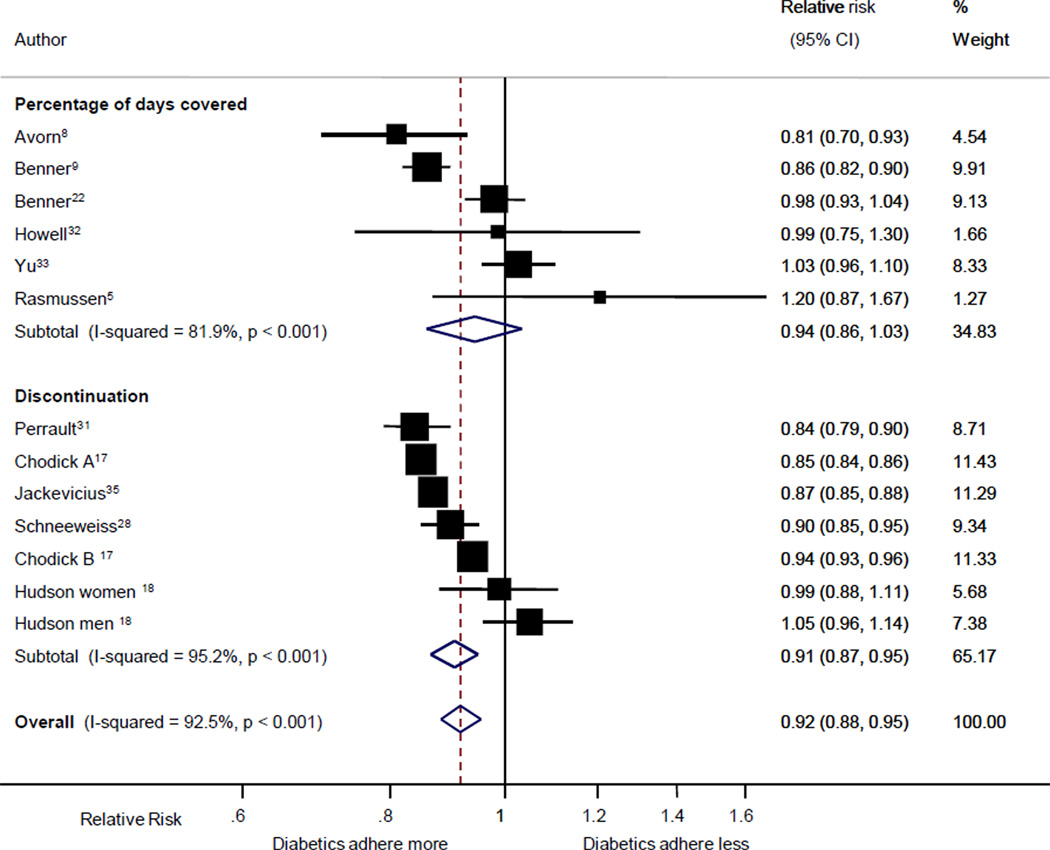
Fig 6.
Forest plot of relative risks for non- adherence comparing those with a history of diabetes to those without a history of diabetes. Conventions as on Figure 3.
Predictors
Reviewed articles considered a broad range of possible predictors including demographics (race, gender, income, ethnicity), psychiatric illness (depression), cognitive impairment (dementia), physician factors (communication skills, racial concordance), health beliefs of patients, complexity of medication regimen (number of medications, dosing frequency), severity of disease, medication side effects, and systemic barriers (cost, transitions in care from outpatient to inpatient, restricted formularies). For each risk factor, the percentage of variability due to between-study heterogeneity was large, and, except in the case of income, significantly different from zero (p<0.05).
Age
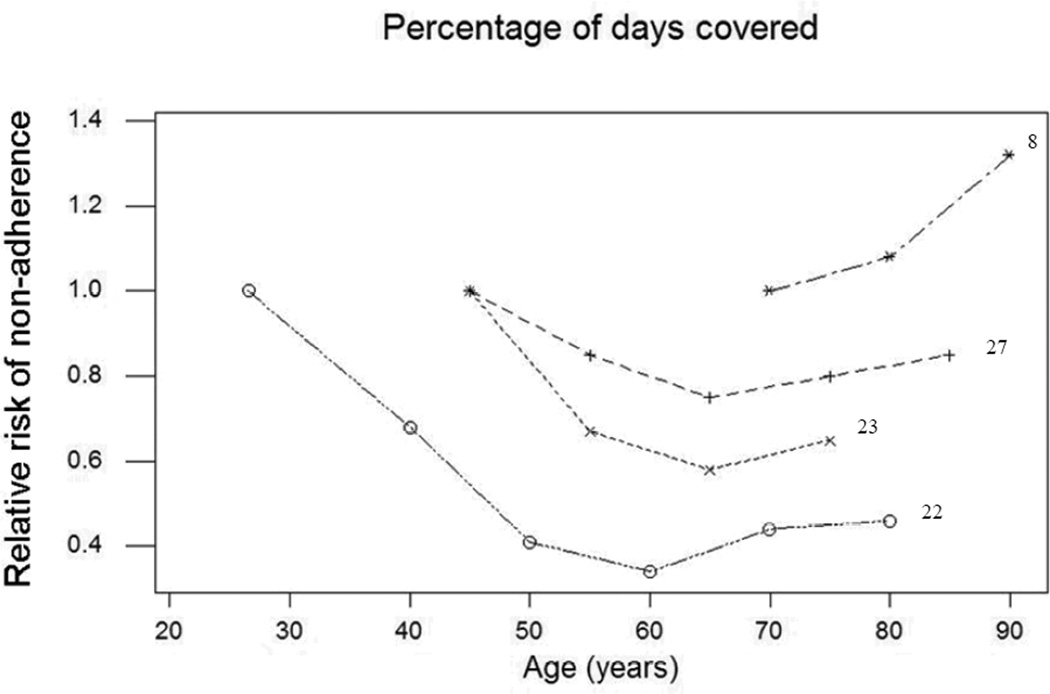
Age was a statistically significant predictor of adherence in all studies. However, the relationship was not monotonic. The youngest participants (usually age < 50 years) were significantly more likely to have lower adherenc (PDC<80%) or to have discontinued their statin compared to “middle aged” adults (usually ages 50–65 years). However, older adults (usually ≥ 70 years old) also displayed lower adherence and increased discontinuation compared to middle aged adults. For example, in the study by Benner et al.22 using adults aged 18–34 as the reference, a U shaped relationship is observed with an odds for non-adherence of 0.68 (0.56–0.85) among 35–44 year olds, 0.41 (0.34–0.50) among 45–54 year olds, 0.34 (0.28–0.41) among 55–64 year olds, 0.44 (0.36–0.53) among 65–74 year olds and 0.46 (0.38–0.57) among those ≥ 75 years old. Figure 7 demonstrates the U-shaped relationship among four studies that examined age as a predictor and used PDC as the adherence measure (the other seven used discontinuation). In total, 10 of the 11 studies that examined age as a multi-level predictor of statin adherence8, 18, 22–28 were consistent with the aforementioned U shaped relationship while 3 studies29 showed a more monotonic improvement of adherence with older age; however these did not include younger populations.
Fig 7.
Plot of relative risks for non-adherence according to increasing age limited to studies using PDC as the measure of adherence.
Gender
Eighteen studies examined gender as a predictor of adherence and the majority of these showed that women were less likely to be adherent (see Figure 2).5, 8, 17, 22, 23, 25, 26, 30–33 The relative risk for low adherence, comparing women to men, via PDC, discontinuation, and overall were 1.07 (95% CI 1.02 – 1.12), 1.07 (95% CI 1.03 – 1.12) and 1.07 (95% CI 1.04 – 1.11), respectively.
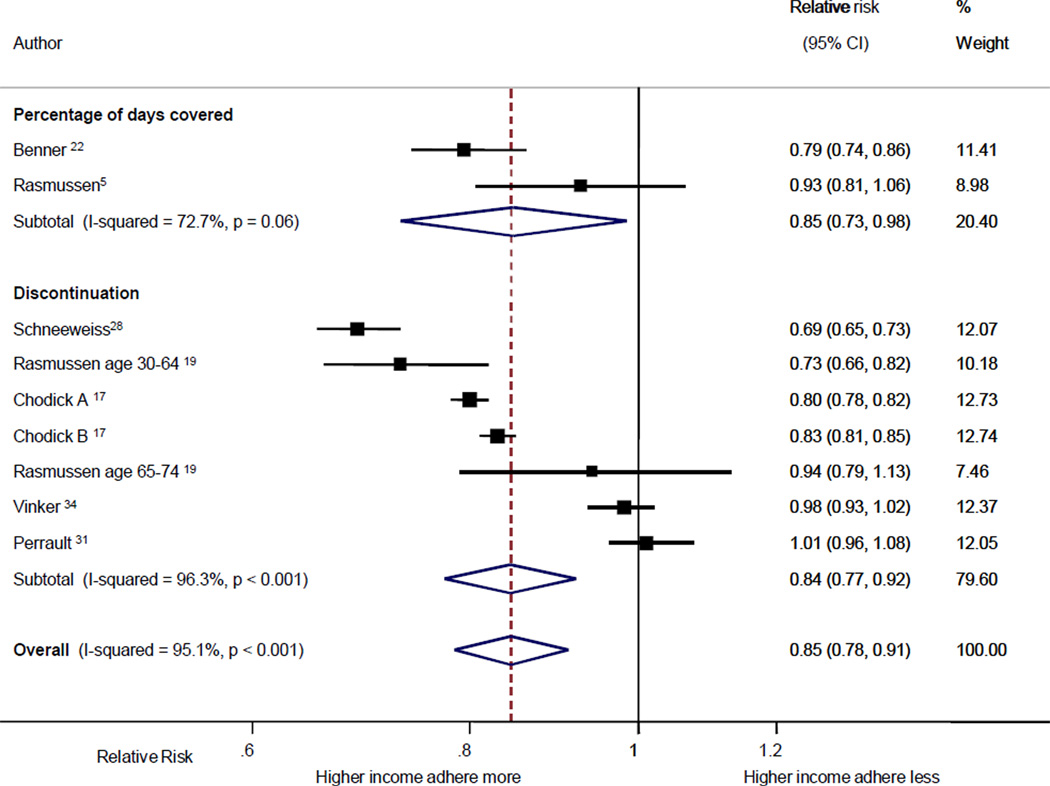
Income
Higher income was significantly associated with adherence assessed by PDC and discontinuation in 5 studies17, 19, 22, 29 with equivocal results in 4 studies (Figure 3).5, 28, 31 Overall, patients with higher income were more likely to be adherent [odds of non-adherence 0.85 (95% CI 0.78 – 0.91)].
Fig 3.
Forest plot of relative risks for non- adherence comparing those with relatively high income to those with relatively low income. Conventions as on Figure 3.
Co-morbidities
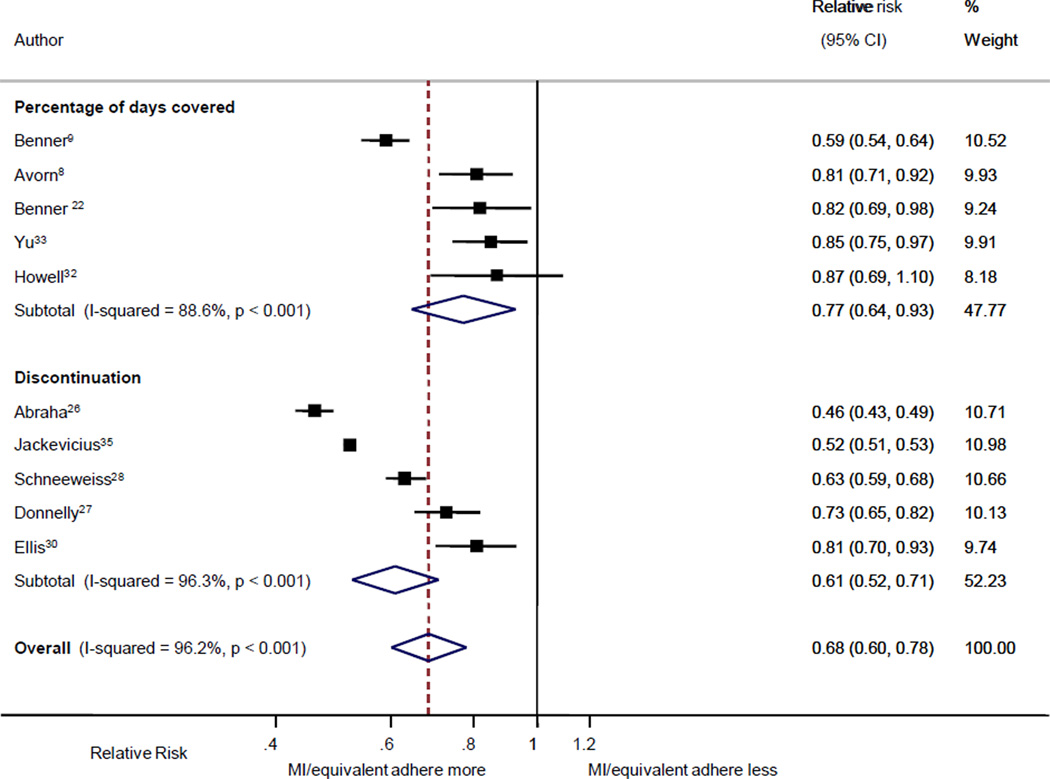
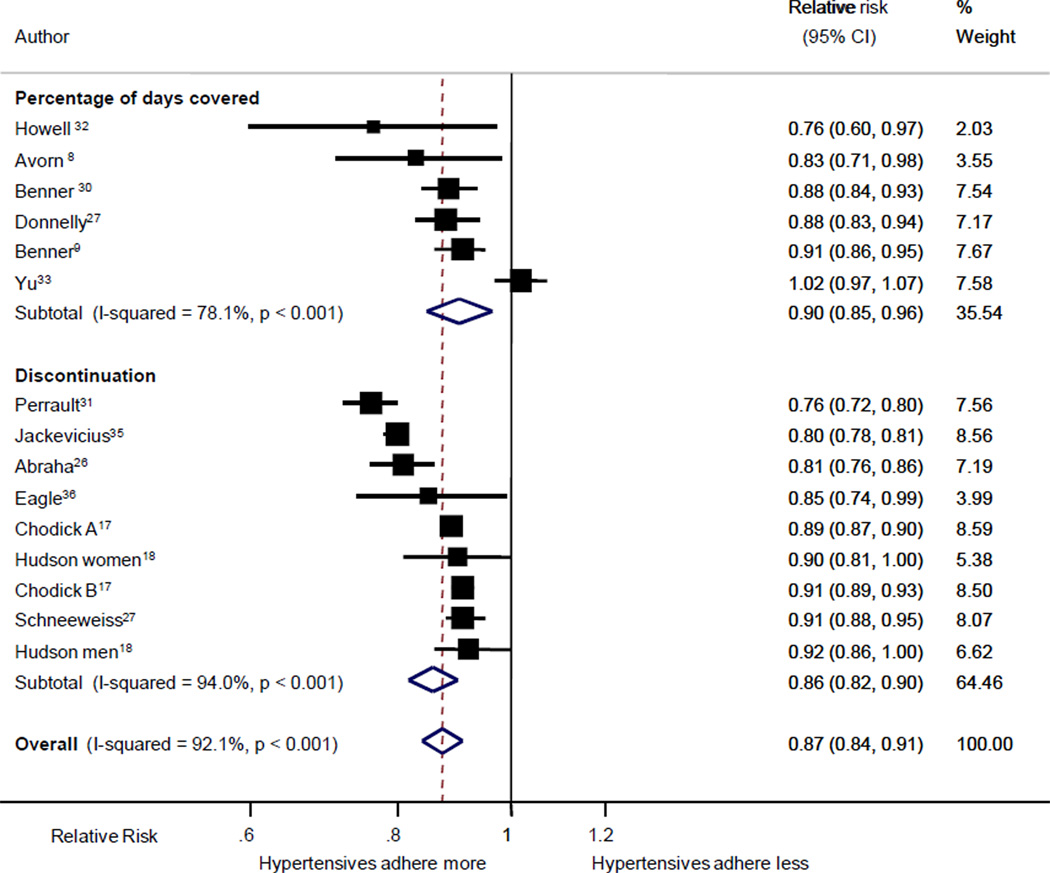
A history of an MI or cardiovascular disease (CVD) equivalent (MI or stroke) was associated with higher adherence in 9 studies (Figure 4).8, 9, 22, 26, 27, 29, 30, 33, 34 Overall, patients with a prior history of CVD were more likely to be adherent [odds of non-adherence 0.68 (95% CI 0.68 – 0.71)]. Similarly, those with a history of hypertension were more likely to be adherent in 12 studies8, 9, 17, 22, 26, 27, 29, 31, 32, 34, 35 with a trend towards better adherence in the remaining studies (Figure 5).18, 33 People with diabetes were also more likely to be adherent in 7 out of 13 studies.8, 9, 17, 29, 31, 34 Diabetes was associated with a trend towards worse adherence in just one study5 and had equivocal results in the remaining 5 studies (Figure 6).18, 32, 33
Fig 4.
Forest plot of relative risks for non- adherence comparing those with a history of MI or equivalent to those without a history of CVD or equivalent. Conventions as on Figure 3.
Fig 5.
Forest plot of relative risks for non- adherence comparing those with a history of hypertension to those without a history of hypertension. Conventions as on Figure 3.
Regimen complexity
Regimen complexity was examined in 8 studies as a possible predictor of adherence to statins.8, 9, 18, 22, 25, 31, 34 Overall there was no clear pattern of association between the total number of medications people were prescribed and their adherence to statins. There was a relatively strong relationship between increasing number of non-cardiovascular medications and low statin adherence. In contrast, increasing cardiovascular medications was associated with higher statin adherence in one study.25
Other Predictors
There was no clear relationship between the number of healthcare provider visits and adherence. Increasing number of visits was associated with better adherence in 3 out of 12 studies examining this relationship17, 25 and a trend towards better adherence in one other study29. However, it was associated with worse adherence in 2 studies30, 31, a trend towards worse adherence in 1 study8, and an equivocal relationship in 5 studies.9, 18, 33, 34
Several other variables were recorded in too few studies for quantitative pooling but suggested trends in their relationships with non-adherence. For example, only 3 eligible articles examined race/ethnicity as a predictor of statin adherence and demonstrated that minorities were less likely to be adherent than Caucasians.9, 21, 30 Similarly, 1 out of 2 articles found that people with depression were less likely to be adherent.9, 22 In one article, first time statin users were less likely to be adherent as compared to experienced statin users.8 In three studies, people with lipid testing had better adherence.22, 30, 32 In 3 out of 3 studies, higher out of pocket costs was associated with lower statin adherence.29, 30, 36
Subgroup Analysis
Grouping articles according to country of participants, years patients were studied, and duration of follow-up did not substantially alter the heterogeneity between studies. The only significant reduction in heterogeneity occurred for the history of an MI or CVD equivalent predictor in studies with <20,000 participants (p<0.0001, I2 0%).
Discussion
These data demonstrate that several socio-demographic, medical history, and health care utilization variables are reliably associated with adherence to statins. Female gender was significantly associated with increased non-adherence and qualitative review suggested that minorities were also more likely to be non-adherent. Age appeared to have a U-shape relationship with adherence with the relatively young adults (< 50 years) and those ≥ 70 years of age demonstrating higher rates of non-adherence compared to middle aged adults. A history of co-morbid diabetes, hypertension, or cardiovascular disease was associated with better adherence as was higher income and increased testing of lipid levels. Other commonly studied variables including the frequency of medical visits and increased complexity of non-cardiovascular drug regimens demonstrated no clear relationship to statin adherence.
There are many possible explanations for the observed relationships. Women are known to access medical care more frequently and to be more attentive to their health.37 Their more careful approach to health may lead to increased doubts regarding the need for statins or more concerns about their potential side effects.21, 38 On the other hand, minorities are known to have less access to care which could lead to lower oversight of their care, and in turn, lower adherence.39 The trend towards an association between more frequent lipids testing with better adherence suggests that access to care could explain the association between race and statin adherence.
Higher rates of adherence among adults with higher income and the trend toward lower adherence with increasing out-of-pocket costs has been observed across many drug classes and appears to have a clear dose-response relationship.13 The relationship is robust regardless of the type of cost (e.g., copay, coinsurance). Accordingly, the low out-of-pocket cost of medications for Veterans may partially explain the higher rates of adherence to statins observed in Veterans Administration populations.40 The importance of financial resources as a barrier to achieving high rates of adherence was recently highlighted in the development of a new rapid adherence screener that identified financial barriers as one of three critical barriers to chronic disease medication adherence.41
Psychological theories, such as the health belief model, suggest that perceived risk of a disease affects behaviors.42 Hence, the observed U-shaped relationship for age in which younger adults are less adherent may be explained by the fact that younger individuals are less likely to perceive themselves as being at risk for heart disease. The relationship between lower perceived heart disease risk and lower statin adherence has been noted in other settings.21 The observed association between a history of myocardial infarction or CVD equivalent, diabetes and hypertension with higher adherence further supports the connection between perceived risk of heart disease and statin adherence. The higher rate of adherence among people taking more cardiovascular medications observed in one study also supports this relationship between perceived risk and adherence. Although older adults should perceive a higher CVD risk, low statin adherence in this group is likely a product of complex regimens, sensitivity to medication costs and increasing prevalence of impaired cognition and health literacy.12, 43 Similarly, lower adherence among those taking more non-cardiovascular medications may be a result of increased complexity of medication regimens.
In contrast to the large number of articles that considered predictors of medication adherence using medication refill databases, there was a paucity of articles meeting our inclusion criteria that considered predictors of medication adherence using validated self-report scales. This has limited the conclusions that can be made regarding how more detailed patient-level predictors such as health beliefs influence medication adherence.43 Future studies need to more carefully explore how individual health beliefs and expectations shape adherence to statins and other CVD medications.
Prior reviews of adherence predictors have observed inconsistent results.12, 13, 44 In the comprehensive review of predictors of adherence to any medication, DiMatteo examined the effects of patient demographics on adherence among 569 studies ranging from HIV to cancer studies.44 It was found that demographic variables had small effects on adherence, in part due to the disparate sample characteristics and measurement variables. This diversity in adherence studies led Vik and colleagues to limit their work to a systematic review of medication adherence correlates among older adults.12 They reported polypharmacy and poor patient-clinician relationships as possible predictors of poor medication adherence and concluded that socio-demographics had negligible impact and there was “little consensus regarding other determinants of non-adherence”. We chose to focus our meta-analysis on statin adherence studies using standardized adherence measures (refill rates from pharmacy and insurance claims databases) to alleviate the issues of excessive heterogeneity found in the prior reviews. This approach allowed us to reduce the variability and quantify the relationship between the candidate predictors and statin adherence. We suspect this is a critical reason for our ability to observe the reported predictive relationships.
Our study should be interpreted in the context of several limitations. We narrowed our study question to statin adherence studies with validated measurements of adherence. This was done in an attempt to identify a homogenous group of studies to evaluate. However, this did not eliminate significant heterogeneity between the studies and studies of mixed quality and sizes were combined. Our subgroup analyses did not find differences to help account for some of the observed heterogeneity. This heterogeneity may be explained by the high level of precision of the relative risks reported by individual studies. The high precision is reflective of the large data sets typical of the majority of the studies pooled together in the meta-analysis. The comparison of high and low values for several predictors also contributes heterogeneity due to the different thresholds set in the individual studies. We also pooled results from studies drawn from over 10 years of research (no relevant articles were found from prior to 1998). Trends in medication taking related behaviors may have changed significantly over this period and this may contribute to variability in our estimates. Each study used various levels of adjustment for confounders which also contributes to the heterogeneity. Although our use of a random effects model accounts for heterogeneity between studies, our estimates of the odds of non-adherence for predictors are likely conservative and may still be affected by uncontrolled confounders.
In summary, our systematic review identified socio-demographic, medical, and health care utilization characteristics that are associated with statin adherence. Several of the identified predictors are likely not unique to statins13 and may represent a core set of easily obtainable variables that should be used to identify individuals and populations at risk for poor adherence to other cardiovascular (anti-hypertensives, aspirin, anti-diabetics) and potentially non-cardiovascular (osteoporosis) medications. Additional predictors likely exist, and additional high quality research of adherence predictors using gold-standard adherence measurement techniques and considering patient-level characteristics is needed.
The current predictors of adherence should be used to identify high-risk populations for targeted counseling and to design adherence interventions aimed at these high risk groups. Particular attention should be paid to younger individuals and those who are taking statins as part of primary prevention as these groups had the highest rates of non-adherence. Clinicians may consider emphasizing non-pharmacologic approaches in addition to statins for reducing cholesterol in these lower CVD risk patient populations. Future research should attempt to clarify the underlying mechanisms for differences in adherence identified by these characteristics.
Acknowledgements
Funding/Support: This research was supported by grant 1K23DK081665, a Patient-Oriented Mentored Scientist Award through the National Institute of Diabetes, Digestive, and Kidney Diseases (Dr Mann). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Appendix 1
Search Strategy Medication Adherence -- Statins
Ovid Medline 1950 to February 2009
exp Cardiovascular Diseases/
exp Hydroxymethylglutaryl-CoA Reductase Inhibitors/
(cholesterol adj lowering).tw.
statin$.tw.
Atorvastatin.af.
Cerivastatin.af.
Fluvastatin.af.
Lovastatin.af.
Mevastatin.af.
Pitavastatin.af.
Pravastatin.af.
Rosuvastatin.af.
Simvastatin.af.
or/2–13
1 and 14
exp Patient Compliance/
(complian$ or noncomplian$ or (non adj complian$) or comply or complies or discontinu$ or adher$ or persist$).tw.
or/16–17
exp Risk Factors/
risk$.tw.
predict$.tw.
determinant$.tw.
associat$.tw.
correlate$.tw.
or/19–24
randomized controlled trial.pt.
exp Randomized Controlled Trials/
controlled clinical trial.pt.
Controlled Clinical Trials/
exp Cohort Studies/
random$.tw.
control$.tw.
cohort$.tw.
prospective$.tw.
observational.tw.
retrospective.tw.
volunteer$.tw.
group$.tw.
or/26–38
and/15,18,25,39
Footnotes
Disclosures: There are no conflicts to report.
Contributor Information
Devin M. Mann, Division of General Internal Medicine, Mount Sinai School of Medicine, 1 Gustave Levy Place, Box 1087, New York, NY, USA, P: 212-824-7559, F: 212-831-8116, devin.mann@mssm.edu.
Mark Woodard, George Institute, University of Sydney, Sydney, Australia.
Paul Muntner, Department of Epidemiology, University of Alabama at Birmingham, Birmingham, AL, USA.
Louise Falzon, Center for Behavioral Cardiovascular Health, Department of Medicine, Columbia University Medical Center, NY, NY, USA.
Ian Kronish, Division of General Internal Medicine, Mount Sinai School of Medicine, New York, NY.
References
- 1.Thavendiranathan P, Bagai A, Brookhart MA, Choudhry NK. Primary prevention of cardiovascular diseases with statin therapy: A meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166(21):2307–2313. doi: 10.1001/archinte.166.21.2307. [DOI] [PubMed] [Google Scholar]
- 2.Cheung BMY, Lauder IJ, Lau C-P, Kumana CR. Meta-analysis of large randomized controlled trials to evaluate the impact of statins on cardiovascular outcomes. Br J Clin Pharmacol. 2004;57(5):640–651. doi: 10.1111/j.1365-2125.2003.02060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42(9):1208–1215. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 4.Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ. 2003;326(7404):1423–1430. doi: 10.1136/bmj.326.7404.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rasmussen JN, Chong A, Alter DA. Relationship Between Adherence to Evidence-Based Pharmacotherapy and Long-term Mortality After Acute Myocardial Infarction. JAMA. 2007;297(2):177–186. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- 6.Bouchard MH, Dragomir A, Blais L, Berard A, Pilon D, Perreault S. Impact of adherence to statins on coronary artery disease in primary prevention. Br J Clin Pharmacol. 2007;3:3. doi: 10.1111/j.1365-2125.2006.02828.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho PM, Spertus JA, Masoudi FA, et al. Impact of Medication Therapy Discontinuation on Mortality After Myocardial Infarction. Arch Intern Med. 2006;166(17):1842–1847. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- 8.Avorn J, Monette J, Lacour A, et al. Persistence of Use of Lipid-Lowering Medications: A Cross-National Study. JAMA. 1998;279(18):1458–1462. doi: 10.1001/jama.279.18.1458. [DOI] [PubMed] [Google Scholar]
- 9.Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. Jama. 2002;288(4):455–461. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- 10.Zeller A, Taegtmeyer A, Martina B, Battegay E, Tschudi P. Physicians' ability to predict patients' adherence to antihypertensive medication in primary care. Hypertens Res. 2008;31(9):1765–1771. doi: 10.1291/hypres.31.1765. [DOI] [PubMed] [Google Scholar]
- 11.Mushlin AI, Appel FA. Diagnosing potential noncompliance. Physicians' ability in a behavioral dimension of medical care. Arch Intern Med. 1977;137(3):318–321. doi: 10.1001/archinte.137.3.318. [DOI] [PubMed] [Google Scholar]
- 12.Vik SA, Maxwell CJ, Hogan DB. Measurement, Correlates, and Health Outcomes of Medication Adherence Among Seniors. Ann Pharmacother. 2004;38(2):303–312. doi: 10.1345/aph.1D252. [DOI] [PubMed] [Google Scholar]
- 13.Osterberg L, Blaschke T. Adherence to Medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 14.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of Observational Studies in Epidemiology: A Proposal for Reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 15.Berlin JA. Does blinding of readers affect the results of meta-analyses? University of Pennsylvania Meta-analysis Blinding Study Group. Lancet. 1997;350(9072):185–186. doi: 10.1016/s0140-6736(05)62352-5. [DOI] [PubMed] [Google Scholar]
- 16.Hess LM, Raebel MA, Conner DA, Malone DC. Measurement of Adherence in Pharmacy Administrative Databases: A Proposal for Standard Definitions and Preferred Measures. Ann Pharm Ther. 2006;40(7):1280–1288. doi: 10.1345/aph.1H018. [DOI] [PubMed] [Google Scholar]
- 17.Chodick G, Shalev V, Gerber Y, et al. Long-term persistence with statin treatment in a not-for-profit health maintenance organization: A population-based retrospective cohort study in Israel. Clin Ther. 2008;30(11):2167–2179. doi: 10.1016/j.clinthera.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Hudson M, Richard H, Pilote L. Parabolas of medication use and discontinuation after myocardial infarction--are we closing the treatment gap? Pharmacoepidemiol Drug Saf. 2007;16(7):773–785. doi: 10.1002/pds.1414. [DOI] [PubMed] [Google Scholar]
- 19.Rasmussen JN, Gislason GH, Rasmussen S, et al. Use of statins and beta-blockers after acute myocardial infarction according to income and education. J Epidemiol Community Health. 2007;61(12):1091–1097. doi: 10.1136/jech.2006.055525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woodward M. Epidemiology: Study Design and Data Analysis. Second Edition. Boca Raton: CRC Press; 2005. [Google Scholar]
- 21.Mann DM, Allegrante JP, Natarajan S, Halm EA, Charlson M. Predictors of adherence to statins for primary prevention. Cardiovasc Drugs Ther. 2007;21(4):311–316. doi: 10.1007/s10557-007-6040-4. [DOI] [PubMed] [Google Scholar]
- 22.Benner JS, Tierce JC, Ballantyne CM, et al. Follow-up lipid tests and physician visits are associated with improved adherence to statin therapy. Pharmacoeconomics. 2004;22(Suppl 3):13–23. doi: 10.2165/00019053-200422003-00003. [DOI] [PubMed] [Google Scholar]
- 23.Caspard H, Chan AK, Walker AM. Compliance with a statin treatment in a usual-care setting:Retrospective database analysis over 3 years after treatment initiation in health maintenance organization enrollees with dyslipidemia. Clinical Therapeutics. 2005;27(10):1639–1646. doi: 10.1016/j.clinthera.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 24.Larsen J, Andersen M, Kragstrup J, Gram LF. High persistence of statin use in a Danish population: Compliance study 1993–1998. Br J Clin Pharmacol. 2002;53(4):375–378. doi: 10.1046/j.1365-2125.2002.01563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang CC, Jick SS, Testa MA. Discontinuation and switching of therapy after initiation of lipid-lowering drugs: the effects of comorbidities and patient characteristics. Br J Clin Pharmacol. 2003;56(1):84–91. doi: 10.1046/j.1365-2125.2003.01818.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abraha I, Montedori A, Stracci F, Rossi M, Romagnoli C. Statin compliance in the Umbrian population. Eur J Clin Pharmacol. 2003;59(8–9):659–661. doi: 10.1007/s00228-003-0675-2. [DOI] [PubMed] [Google Scholar]
- 27.Donnelly LA, Doney AS, Morris AD, Palmer CN, Donnan PT. Long-term adherence to statin treatment in diabetes. Diabet Med. 2008;25(7):850–855. doi: 10.1111/j.1464-5491.2008.02476.x. [DOI] [PubMed] [Google Scholar]
- 28.Vinker S, Shani M, Baevsky T, Elhayany A. Adherence with statins over 8 years in a usual care setting. Am J Manag Care. 2008;14(6):388–392. [PubMed] [Google Scholar]
- 29.Schneeweiss S, Patrick AR, Maclure M, Dormuth CR, Glynn RJ. Adherence to Statin Therapy Under Drug Cost Sharing in Patients With and Without Acute Myocardial Infarction: A Population-Based Natural Experiment. Circulation. 2007;115(16):2128–2135. doi: 10.1161/CIRCULATIONAHA.106.665992. [DOI] [PubMed] [Google Scholar]
- 30.Ellis JJ, Erickson SR, Stevenson JG, Bernstein SJ, Stiles RA, Fendrick AM. Suboptimal Statin Adherence and Discontinuation in Primary and Secondary Prevention Populations. Should We Target Patients with the Most to Gain? Journal of General Internal Medicine. 2004;19(6):638–645. doi: 10.1111/j.1525-1497.2004.30516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perreault S, Blais L, Lamarre D, et al. Persistence and determinants of statin therapy among middle-aged patients for primary and secondary prevention. British Journal of Clinical Pharmacology. 2005;59(5):564–573. doi: 10.1111/j.1365-2125.2005.02355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Howell N, Trotter R, DR M, Rowe P. Compliance with statins in primary care. The Pharmaceutical Journal. 2004;272(3):23–32. [Google Scholar]
- 33.Yu AP, Yu YF, Nichol MB, Gwadry-Sridhar F. Delay in filling the initial prescription for a statin: a potential early indicator of medication nonpersistence. Clin Ther. 2008;30(4):761–774. doi: 10.1016/j.clinthera.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 34.Jackevicius CA, Mamdani M, Tu JV. Adherence With Statin Therapy in Elderly Patients With and Without Acute Coronary Syndromes. JAMA. 2002;288(4):462–467. doi: 10.1001/jama.288.4.462. [DOI] [PubMed] [Google Scholar]
- 35.Eagle KA, Kline-Rogers E, Goodman SG, et al. Adherence to evidence-based therapies after discharge for acute coronary syndromes: an ongoing prospective, observational study. Am J Med. 2004;117(2):73–81. doi: 10.1016/j.amjmed.2003.12.041. [DOI] [PubMed] [Google Scholar]
- 36.Hsu J, Price M, Huang J, et al. Unintended consequences of caps on Medicare drug benefits. N Engl J Med. 2006;354(22):2349–2359. doi: 10.1056/NEJMsa054436. [DOI] [PubMed] [Google Scholar]
- 37.Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49(2):147–152. [PubMed] [Google Scholar]
- 38.Tolmie EP, Lindsay GM, Kerr SM, Brown MR, Ford I, Gaw A. Patients' perspectives on statin therapy for treatment of hypercholesterolaemia: a qualitative study. Eur J Cardiovasc Nurs. 2003;2(2):141–149. doi: 10.1016/S1474-5151(03)00028-8. [DOI] [PubMed] [Google Scholar]
- 39.Steinbrook R. Disparities in Health Care -- From Politics to Policy. N Engl J Med. 2004;350(15):1486–1488. doi: 10.1056/NEJMp048060. [DOI] [PubMed] [Google Scholar]
- 40.Kopjar B, Sales AEB, Pineros SL, Sun H, Li Y-F, Hedeen AN. Adherence with statin therapy in secondary prevention of coronary heart disease in veterans administration male population. The American Journal of Cardiology. 2003;92(9):1106–1108. doi: 10.1016/j.amjcard.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 41.McHorney CA. The Adherence Estimator: a brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr Med Res Opin. 2009;25(1):215–238. doi: 10.1185/03007990802619425. [DOI] [PubMed] [Google Scholar]
- 42.Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education. 4 ed. San Francisco: Jossey-Bass; 2008. [Google Scholar]
- 43.Mann D. Resistant disease or resistant patient: problems with adherence to cardiovascular medications in the elderly? Geriatrics. 2009;4(9):10–15. [PubMed] [Google Scholar]
- 44.DiMatteo MR. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]