Abstract
We report two detrimental neurologic complications after technically correct selected cervical nerve root blocks. Based on these cases and a thorough review of the literature, the indication for cervical nerve root blocks was reconsidered and limited. Similarly, we modified our technique to further reduce the likelihood for the occurrence of such severe complications.
Keywords: Cervical nerve root, Block, Injection, Safety, Technique, Corticosteroids, Complications
Introduction
The rationale for selective nerve root blocks is to tackle the inflammatory component of a nerve root compromise caused by a herniated disk or an osseous foraminal stenosis. Therefore, the goal is not to cure the patient by interfering with underlying pathogenetic factors, i.e., mechanical compression responsible for the radiculopathy but rather to provide temporary relief from peak pain during the time required for spontaneous resolution of radiculopathy [10, 11, 15].
There are only a few studies regarding selective cervical nerve root blocks [10, 11]. Strobel et al. [19] reported on 60 patients with cervical radiculopathy. The authors investigated whether magnetic resonance imaging findings can predict pain relief after CT-guided cervical root nerve block. The mean percentage of pain reduction (VAS) was 46 %. Patients with foraminal disk herniation, foraminal nerve root compromise, and no spinal canal stenosis appear to have the best pain relief after this procedure. Berger et al. [2] reported effective long-term pain relief in 11 of 18 patients with cervical radiculopathy (61 %) undergoing CT-guided foraminal injections. Slipman et al. [18] retrospectively investigated fluoroscopically guided cervical nerve root block in 20 patients with cervical spondylotic radicular pain. In 60 % of the patients, an overall good or excellent result was observed. Vallee et al. [21] treated 32 patients with chronic cervical radiculopathy unresponsive to medical treatment alone by periradicular corticosteroid injections. The mean evolutionary trends for radicular and neck pain relief were significant at 14 days (P < 0.001) and at 6 months (P < 0.001). The procedure did not produce any complications. In a large series of 802 procedures using an anterior oblique approach, Phobiel et al. [14] did not encounter any major complications.
Complications subsequent to cervical nerve root blocks remain very rare but may be more common than generally anticipated [17]. This particularly includes detrimental complications of the basilary arterial territory such as cerebellar and spinal cord infarction [16, 20]. Most often, such complications appear to be associated with the dissection or intra-arterial injection of crystalline steroids of the vertebral artery [17]. Such complications should be avoidable using image guidance correctly, both fluoroscopy and CT. However, there appears to be the possibility of infarction resulting from impaired perfusion of the major feeding anterior radicular artery of the spinal cord [4]. Such small vessels [8] may not be seen during image-guided injection, whatever imaging method is employed. This makes it practically impossible to avoid such complications.
The objective of this case report is to communicate detrimental complications after technically correct nerve root blocks in two patients resulting in incomplete transient tetraparesis as well as to discuss the procedural consequences implemented in our institution.
Case studies
Case 1
The first patient was a 71-year-old woman who developed a tetraplegia subsequent to a cervical nerve root block and was referred to our spinal cord injury unit. A radiologist with an experience of approximately 1,000 cervical nerve root injections had performed a C7/T1 foraminal injection on the left side, based on the presence of a foraminal stenosis. The needle was placed outside the intervertebral foramen to diminish the risk of an intravascular injection (Fig. 1a). A tentative injection of contrast media demonstrated extraforaminal contrast distribution. The report indicates that “diluted” Iotralan (Isovist®, Bayer-Schering Pharma, Berlin, Germany) was used. The following injection using triamcinolon (40 mg, 1 ml Kenacort 40®, Dermapharm, Huenenberg, Switzerland) and—according to the report—a “small” amount of local anesthetics (Bupivacain, Carbostesin®, AstraZeneca, Zug, Switzerland) led to immediate and excruciating pain and tetraplegia. An MR of the cervical spine performed on the day after injection demonstrated ischemic myelopathy at the C5–C7 levels (Fig. 1b). The patient initially had a complete tetraplegia below the C5 level, AIS A which recovered to AIS D [12] during the following 8 months of rehabilitation. In spite of the improvements during rehabilitation, the patient remained wheelchair-bound.
Fig. 1.
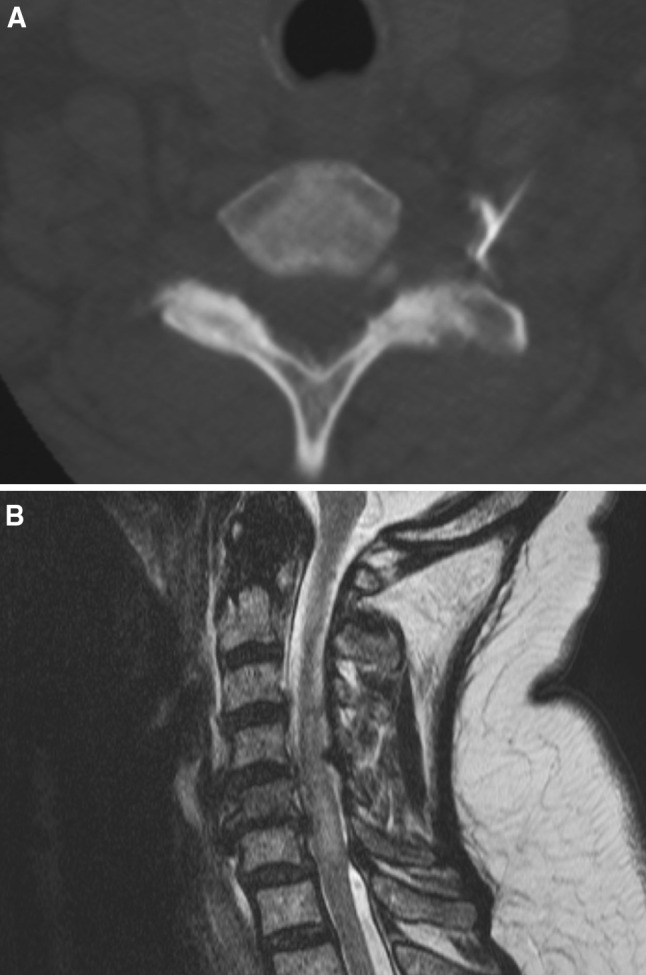
Imaging studies of a 71 year old female (Case 1). a C7/T1 foraminal injection on the left side. Needle position outside the intervertebral foramen. A tentative injection of contrast media demonstrated extraforaminal contrast distribution. b T2-weighted sagittal MR image obtained 1 day after injection demonstrating ischemic myelopathy at the C5–C7 levels
Case 2
The second patient was a 59-year-old man with chronic radicular C6 and C7 right-sided pain in the presence of cervical spine degeneration. Periradicular injection of both the C6 and C7 nerve root were requested by the referring physician. For both injections, 23 gauge (0.6 mm), 6-cm long needles were used according to the institution’s standard protocol. The needles were advanced step-by-step, while injecting small amounts of ropicvacain (Naropin®, 0.2 %, AstraZeneca, Zug, Switzerland). The C6 injection was performed first and was uneventful. For the C7 injection, the needle tip was placed at the entrance of the C6/7 foramen dorsally. 0.5 ml of contrast agent was injected after needle placement under fluoroscopic control (Iopamidol, Iopamiro 200®, Bracco, Milan, Italy). Contrast distribution was in the posterior part of the foramen (Fig. 2a). 20 mg (0.5 ml) of triamcinolon (Kenacort 40®, Dermapharm, Huenenberg, Switzerland) and 1 ml of Naropin® 0.2 % (Ropivacain, AstraZeneca, Zug, Switzerland) were then injected. Nearly immediately, the patient complained about visual color misperception and severe shoulder pain and became tetraplegic with incomplete sensory-motor deficits below the C4 level, AIS C [12] within minutes. MR images obtained 1 day after injection demonstrated spinal cord signal abnormalities consistent with ischemic myelopathy at the C4–C6 levels (Fig. 2b). The patient improved considerably and was dismissed after 4 months of rehabilitation with incomplete tetraplegia below C4 (AIS D). He was ambulatory without aids. However, paresis accentuated at the hands persisted, consistent with a mild central cord syndrome.
Fig. 2.
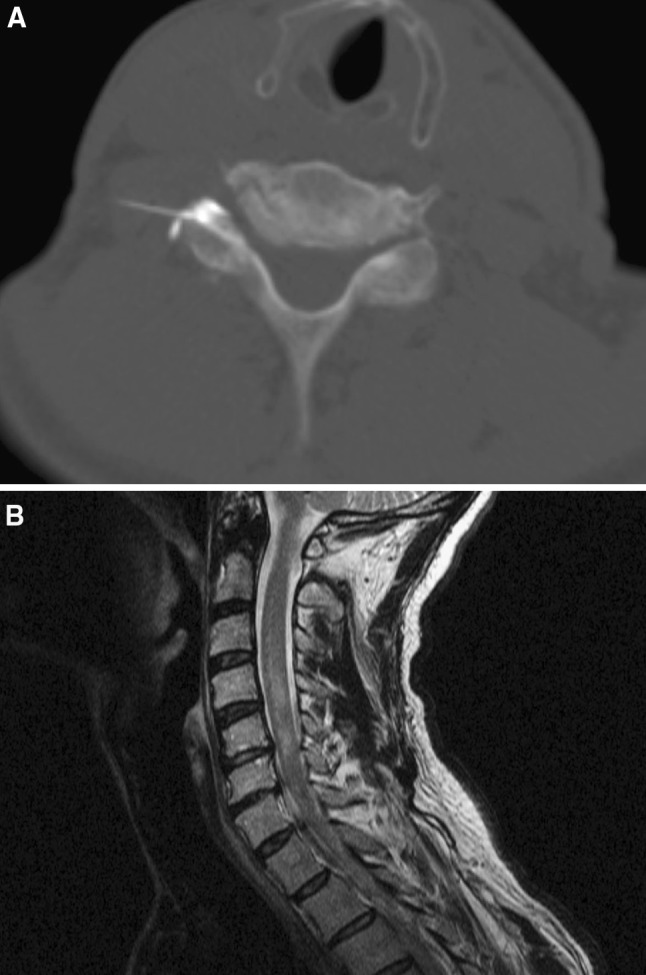
Imaging studies of a 59 year old male (Case 2). a Needle tip at the entrance of the right C6/7 foramen dorsally, after injection of 0.5 ml of contrast agent. b Sagittal T2-weighted MR image obtained 1 day after injection demonstrated spinal cord signal abnormalities consistent with ischemic myelopathy at the levels C4–C6
Discussion
In the light of the aforementioned detrimental and unexpected complications, a critical re-assessment of the indication for selective cervical nerve root blocks is prompted.
Approximately at the time of the second incident, an article was published by Scanlon et al. [17] highlighting complications of cervical nerve root injections. This cross-sectional survey described the occurence of 78 severe neurological side effects in the context of cervical transforaminal injections in the United States. An embolic mechanism was assumed for the majority of cases reported by Scanlon et al. [17] and is likely to have caused the spinal injury in our patients as well. An inadvertent intra-arterial injection of particulate corticosteroid was reported to cause a distal infarction [17]. The most common complication was infarction related to the vertebrobasilary territory (n = 16). Many complications, however, were not explained by injection into the vertebral artery but rather by injection of radicular arteries communicating with the anterior spinal artery and a network of medullary vessels [17]. There are few articles describing the relevant anatomy [8]. These radicular arteries are small, variable in number and location and may not be detected during image-guided contrast injections. Based on this description, there is no safe way to avoid these vessels by using a certain needle position or type [5]. To observe blood flowing back into the syringe before injection and then to reposition the needle may not be more useful because sensitivity of backflow of blood for intra-arterial needle position is only 45.9 % [6]. Imaging may detect inadvertent intravascular injections. CT precisely demonstrates the needle tip in relation to the vertebral artery [22], but may not detect very small vessels and vessels running out of the imaging plane [3]. CT has not been proved to be less safe than fluoroscopy guidance. In the article by Scanlon et al. [17], 59 of the 78 injections were performed by anesthesiologists, 13 by physiatrists, two by orthopedic surgeons, and one each by a radiologist, a neurologist and family medicine physician. It is fair to assume that most of these injections have been performed under fluoroscopic guidance and not with CT.
There are many different types of fluoroscopic units. Although contrast within small vessels may indeed be better demonstrated by fluoroscopy this requires optimal equipment, possibly with subtraction imaging [3]. A test injection of local anaesthetics has been recommended in order to prevent intravascular injection of steroids [9]. In case of intravascular injection, transient neurological symptoms may occur which prevent the injection of steroids. Based on the current literature [1, 13], the use of non-particulate steroids is advocated when injections are made around the spinal cord including the conus because of the decreased risk of a neurologic complication. According to a recent review, the study by Scanlon et al. shows the strongest association to date between particulate corticosteroids and brain/spinal cord infarctions [1].
In a pig model, injection of particulate steroids (methylprednisolone) into the vertebral artery lead do death in 4/4 animals while all non-particulate steroids (dexamethasone, prednisolone) survived and did not demonstrate gross abnormalities on MR images or histologically. There has been a debate regarding the use of blunt versus pointed needle tips but no obvious advantage of blunt needles has been shown [7, 8].
Conclusions
Cervical nerve root blocks may more commonly cause complications than anticipated by many physicians ordering or performing nerve root blocks. The location of the injection close to delicate central nervous structures and their ample vascular supply entails the possibility of severe neurological complications, one of the most likely being infarctions of the cervical cord and ischemia within the territory of the vertebrobasilary system. Careful needle positioning and documentation is required. Probatory injection of local anesthetics is recommended prior to the injection of the therapeutic compound. Application of non-particulate steroids is recommended.
Procedural modifications made in our center
Based on the aforementioned conclusions, we have discontinued the use of pure diagnostic subaxial and therapeutic atlanto-axial nerve root blocks because of the immanent risks. However, we continue with the application of therapeutic subaxial selective cervical nerve root blocks if:
patients gave an informed consent after being informed that there is a small (estimated 1:3,500) but unavoidable risk of severe complications associated with cervical nerve root blocks including permanent neurological damage
indication is unequivocal, i.e., radicular pain concordant with imaging findings and severe symptoms non-responsive to usual conservative treatment
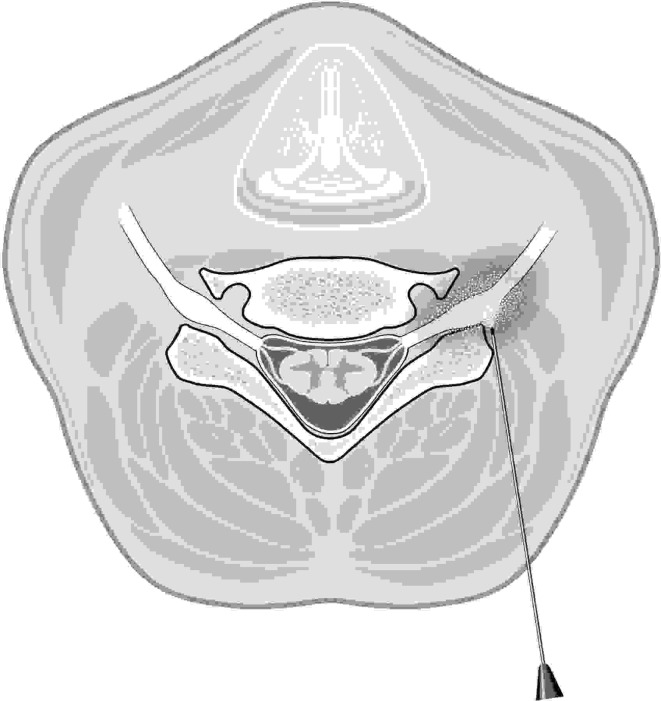
a strictly posterior approach can be done with the patient in the supine position. The needle tip is placed at the antero-lateral aspect of the facet joint. The needle is not further advanced into the course of the nerve root in order to avoid any chance of injecting a radicular artery (Fig. 3)
probatory injection is possible with local anaesthetics. The patient is asked about any new symptoms before steroids injection after a waiting period of at least 2 min
non-particular (e.g., dexamethasone) steroids are injected slowly.
Fig. 3.
The patient is positioned supine and the needle is advance to the lateral and anterior aspect of the facet joint
Conflict of interest
None.
Contributor Information
Juerg Hodler, Email: juerg.hodler@usz.ch.
Norbert Boos, Email: norbert.boos@prodorso.ch.
Martin Schubert, Email: martin.schubert@balgrist.ch.
References
- 1.Benedetti EM, Siriwetchdarek R, Stanec J, Rosenquist R. Epidural steroids injections: complications and management. Tech Reg Anesth. 2009;13:236–250. [Google Scholar]
- 2.Berger O, Dousset V, Delmer O, Pointillart V, Vital JM, Caille JM. Evaluation of the efficacy of foraminal infusions of corticosteroids guided by computed tomography in the treatment of radicular pain by foraminal injection. J Radiol. 1999;80:917–925. [PubMed] [Google Scholar]
- 3.Bogduk N, Dreyfuss P, Baker R, Yin W, Landers M, Hammer M, Aprill C. Complications of spinal diagnostic and treatment procedures. Pain Med. 2008;9:S11–S34. doi: 10.1111/j.1526-4637.2008.00437.x. [DOI] [Google Scholar]
- 4.Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91:397–399. doi: 10.1016/S0304-3959(00)00437-1. [DOI] [PubMed] [Google Scholar]
- 5.Candido KD, Ghaly RF, Mackerley S, Knezevic NN. A Whitacre-type spinal needle does not prevent intravascular injection during cervical nerve root injections. South Med J. 2010;103:679–682. doi: 10.1097/SMJ.0b013e3181e1e3d6. [DOI] [PubMed] [Google Scholar]
- 6.Furman MB, Giovanniello MT, O’Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976) 2003;28:21–25. doi: 10.1097/00007632-200301010-00007. [DOI] [PubMed] [Google Scholar]
- 7.Heavner JE, Racz GB, Jenigiri B, Lehman T, Day MR. Sharp versus blunt needle: a comparative study of penetration of internal structures and bleeding in dogs. Pain Pract. 2003;3:226–231. doi: 10.1046/j.1533-2500.2003.03027.x. [DOI] [PubMed] [Google Scholar]
- 8.Huntoon MA. Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005;117:104–111. doi: 10.1016/j.pain.2005.05.030. [DOI] [PubMed] [Google Scholar]
- 9.Karasek M, Bogduk N. Temporary neurologic deficit after cervical transforaminal injection of local anaesthetic. Pain Med. 2004;5:202–205. doi: 10.1111/j.1526-4637.2004.04028.x. [DOI] [PubMed] [Google Scholar]
- 10.Leonardi M, Pfirrmann CW. Spinal injections. In: Aebi M, Boos N, editors. Spinal disorders. Fundamentals of diagnosis and treatment. Heidelberg: Springer; 2008. pp. 261–290. [Google Scholar]
- 11.Leonardi M, Pfirrmann CW, Boos N. Injection studies in spinal disorders. Clin Orthop Relat Res. 2006;443:168–182. doi: 10.1097/01.blo.0000200254.42500.58. [DOI] [PubMed] [Google Scholar]
- 12.Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, Haak M, Hudson LM, Priebe MM. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26(Suppl 1):S50–S56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- 13.Okubadejo GO, Talcott MR, Schmidt RE, Sharma A, Patel AA, Mackey RB, Guarino AH, Moran CJ, Riew KD. Perils of intravascular methylprednisolone injection into the vertebral artery. An animal study. J Bone Jt Surg Am. 2008;90:1932–1938. doi: 10.2106/JBJS.G.01182. [DOI] [PubMed] [Google Scholar]
- 14.Pobiel RS, Schellhas KP, Eklund JA, Golden MJ, Johnson BA, Chopra S, Broadbent P, Myers ME, Shrack K. Selective cervical nerve root blockade: prospective study of immediate and longer term complications. AJNR Am J Neuroradiol. 2009;30:507–511. doi: 10.3174/ajnr.A1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004;100:1595–1600. doi: 10.1097/00000542-200406000-00035. [DOI] [PubMed] [Google Scholar]
- 16.Rozin L, Rozin R, Koehler SA, Shakir A, Ladham S, Barmada M, Dominick J, Wecht CH. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol. 2003;24:351–355. doi: 10.1097/01.paf.0000097790.45455.45. [DOI] [PubMed] [Google Scholar]
- 17.Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine (Phila Pa 1976) 2007;32:1249–1256. doi: 10.1097/BRS.0b013e318053ec50. [DOI] [PubMed] [Google Scholar]
- 18.Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000;81:741–746. doi: 10.1016/s0003-9993(00)90104-7. [DOI] [PubMed] [Google Scholar]
- 19.Strobel K, Pfirrmann CW, Schmid M, Hodler J, Boos N, Zanetti M. Cervical nerve root blocks: indications and role of MR imaging. Radiology. 2004;233:87–92. doi: 10.1148/radiol.2331030423. [DOI] [PubMed] [Google Scholar]
- 20.Suresh S, Berman J, Connell DA. Cerebellar and brainstem infarction as a complication of CT-guided transforaminal cervical nerve root block. Skelet Radiol. 2007;36:449–452. doi: 10.1007/s00256-006-0215-0. [DOI] [PubMed] [Google Scholar]
- 21.Vallee JN, Feydy A, Carlier RY, Mutschler C, Mompoint D, Vallee CA. Chronic cervical radiculopathy: lateral-approach periradicular corticosteroid injection. Radiology. 2001;218:886–892. doi: 10.1148/radiology.218.3.r01mr17886. [DOI] [PubMed] [Google Scholar]
- 22.Wolter T, Mohadjer M, Berlis A, Knoeller S. Cervical CT-guided, selective nerve root blocks: improved safety by dorsal approach. AJNR Am J Neuroradiol. 2009;30:336–337. doi: 10.3174/ajnr.A1222. [DOI] [PMC free article] [PubMed] [Google Scholar]