Abstract
Introduction
Spinal epidural abscess is an uncommon entity, especially in the cervical region.
Case report
We report a patient with epidural abscess, vertebral osteomyelitis and discitis in the cervical spine that was caused by iatrogenic perforation of the pharynx during diagnostic oesophagoscopy, which has not been recorded previously in the literature.
Conclusion
Cervical spinal epidural abscess may be caused by iatrogenic perforation of pharyngeal wall during diagnostic oesophagoscopy. Early diagnosis with an MRI and surgical treatment with antimicrobial chemotherapy are keys to successful management of this rare and life-threatening complication.
Keywords: Spinal epidural abscess, Pharyngeal perforation, Oesophagoscopy
Introduction
Spinal epidural abscess (SEA) is an uncommon entity, especially in the cervical region. It may progress to severe neurologic deficit. When recognized early and treated promptly, the outcome is good [1–5]. This report concerns such a patient.
Case report
A 55-year-old female, with an unremarkable past medical, family, and social history, had undergone a routine upper gastrointestinal endoscopy due to swallowing problems. The procedure was conducted in a primary care clinic. During endoscopy, she experienced sharp pain in her throat that quickly subsided with analgesics. Next day, low-grade intermittent fever and chills with neck pain developed. She was evaluated by a family physician and ENT specialist, who found no apparent complications from the endoscopy procedure. Intravenous benzyl penicillin was administered. Over the next 2 weeks, her condition improved. Only slight neck stiffness remained. However, 1 week later she again complained of high-grade fever and neck pain. The patient was transferred to our institution. On admission, she was neurologically intact and denied any numbness or paresthesia. Painful swelling of the right posterior side of the neck was observed with limitation of movement in all directions. Her temperature was 39 °C. The laboratory examination revealed a white blood cell count of 18.7 × 109 L−1 and erythrocyte sedimentation rate was elevated at 78 mm/h. CT scan of the neck revealed an anterolaterally located epidural mass with slight rim enhancement and small amount of gas in paraspinal tissue and inside the spinal canal (Fig. 1). She was planned for MRI. Her oral intake was restricted. She was empirically placed on intravenous broad-spectrum antibiotics. Her condition was unchanged for the next 2 days. On the third day after admission, the patient experienced mild weakness of right arm and numbness of right shoulder. Neurologic examination revealed paresis of the right deltoid and biceps muscles, as well as hypesthesia and hypalgesia of the right C4–6 dermatomes.
Fig. 1.
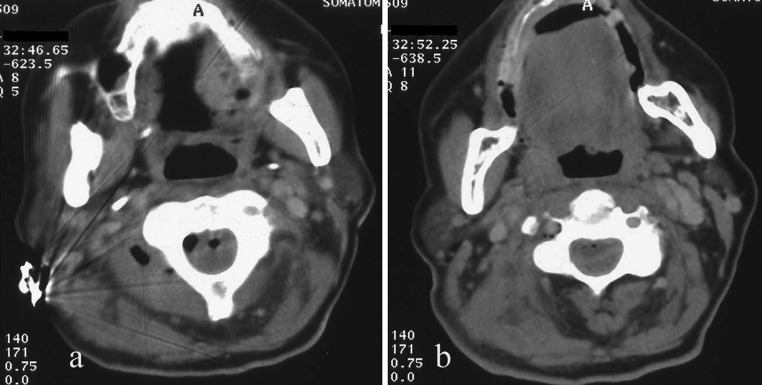
Post-contrast axial CT scans through C2 (a) and C3 (b) vertebrae. Epidural mass with slight rim enhancement is present. Small amount of gas in edematous right paraspinal tissue and inside the spinal canal is seen
The MRI scan of the cervical spine showed osteomyelitis in the C3 and C4 vertebral bodies with C3–4 disc space infection and an epidural collection, extending from the craniocervical junction to C5. The spinal cord showed signs of intraparenchymal edema and was displaced posteriorly and to the left. The fistulous channel at the C3–4 level, extending from the site of perforation on the posterior pharyngeal wall into the retropharyngeal space, was also visualized (Fig. 2).
Fig. 2.
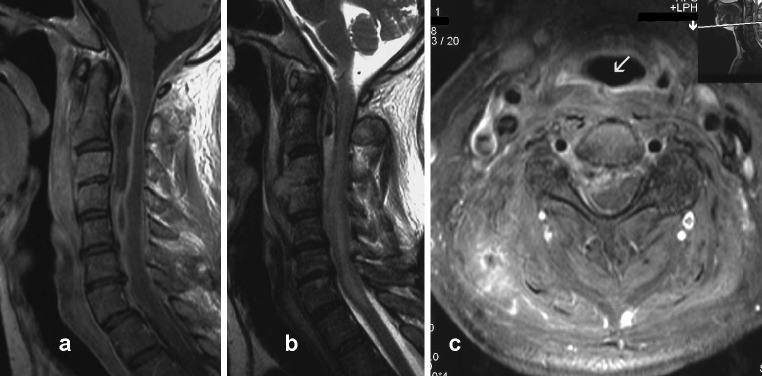
Post-contrast sagittal (a) and axial (c) T1-weighted, and sagittal T2-weighted (b) images of the cervical spine. Images illustrate a ventral-lateral right epidural collection that is hyperintense in T2 W and hypointense in T1 W sequences with an enhancing rim and small amount of gas in its rostral part. Cervical spinal cord is diffusely hyperintense in T2 W images. The C3–C4 disc space is obliterated and vertebral bodies of C3 and C4 are hyperintense in T2 W with well enhancement in T1 W sequences, reflecting discitis and osteomyelitis. Infection of retropharyngeal and paravertebral soft tissues is evident in all figures. Fistulous channel with good rim enhancement (arrow) at the C3–4 level is visualized in axial image
Five hours after the first signs of neurologic deterioration, her motor weakness dramatically progressed to a near-complete quadriparesis with minimal movement in left shoulder and no distal arm or leg movement. Sensory examination showed demarcated sensory loss at the C4 level.
The patient was then taken to the operating room emergently. After induction of general anesthesia, she was placed prone and laminectomies were performed from C2 to C4. The paraspinous muscles were markedly edematous. The capsule of the epidural abscess was incised along the right side of the cervical dura. Frank liquid pus was evacuated from the epidural space. The entire cervical epidural space was irrigated with saline solution delivered through an infant urinary catheter. The wound was closed in layers and drained for 2 days. The neck was immobilized in a rigid collar. The culture of the purulent material was negative. After surgery, she was treated with broad-spectrum intravenous antibiotics for 6 weeks. The patient’s condition improved, with progressive recovery of motor function. She was discharged and transferred to the rehabilitation hospital. Treatment with oral antibiotics was continued for the next 2 weeks. A follow-up MRI scan showed resolution of the epidural collection (Fig. 3). Two years post surgery, only slight paresis of the right deltoid muscle remained. A spontaneous fusion of vertebral bodies C2, C3 and C4 in kyphotic malalignment is seen, restricting the total range of motion of the cervical spine, on 2-year follow-up radiographs (Fig. 4). Oral intake was good.
Fig. 3.
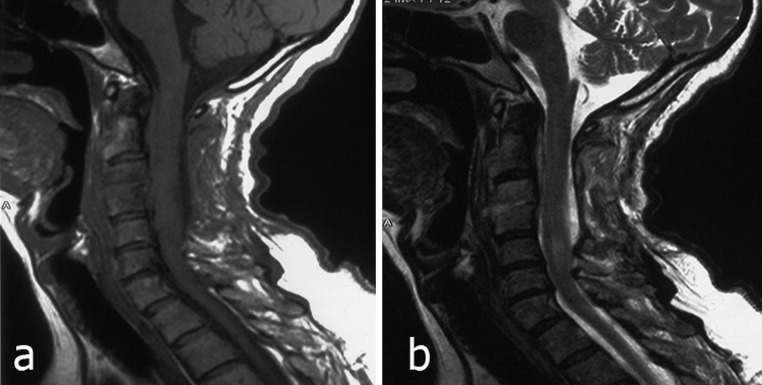
Postoperative (3 weeks after the surgery) sagittal T1-weighted (a), and T2-weighted (b) images of the cervical spine. Complete removal of epidural abscess is seen
Fig. 4.
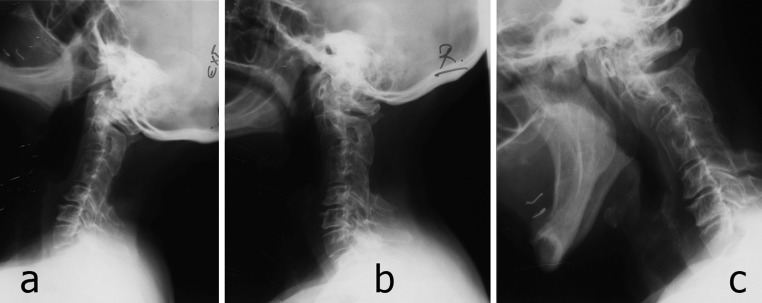
Lateral radiographs of cervical spine, extension (a), neutral (b), and flexion (c). Fusion of vertebral bodies C2, C3 and C4 in kyphotic malalignment restricting total range of motion of cervical spine is seen
Discussion
Spinal epidural abscess usually results from hematogenous dissemination from distant foci such as the skin, respiratory and urinary tracts [1–5]. Direct spread of the microorganisms from the gastrointestinal tract by spontaneous or accidental perforation is very rare [6–9]. To our knowledge, this is the first reported case of cervical SEA that was caused by iatrogenic perforation of the pharynx during diagnostic endoscopy. Inappropriate maneuver of the endoscope caused the initially unrecognized lesion of the pharyngeal wall. Perforation in this area, due to the septic content of the pharynx and its continual movements associated with swallowing and breathing caused the infection of the neighboring structures. Prevertebral cellulitis, vertebral osteomyelitis and discitis occurred. The infection was further complicated by cervical SEA formation, which caused severe neurologic deficit.
SEA is a well-characterized clinical entity. The triad of fever, pain overlying the site of compression, and progressive neurologic deficits, which has often been described as typical for SEA in the literature [1–5], was also observed in our patient. Insidious and subtle initial clinical presentation was probably caused by small perforation of pharyngeal wall and early application of antibiotics. The patient was neurologically intact, with neck pain and fever as the only symptoms, during the period of 3 weeks after the endoscopic accident. Neurologic deterioration occurred in the later course of disease, and it was very acute and severe.
Prognosis of SEA was found to be inversely proportional to the duration and severity of neurologic deficit. Thus, early recognition and treatment of this unusual complication are of the critical importance for favorable outcome. Prompt surgical spinal cord decompression, drainage of the SEA, and long-term antibiotic therapy has been the treatment of choice for SEA. This has been confirmed in numerous series to date [1–5]. Drainage of the purulent collection allows immediate decompression of neural elements and accesses the most voluminous sample from which to culture an organism. In our case, the initiation of antibiotic therapy before obtaining culture resulted in failure to isolate a specific bacterial agent.
An MRI is the study of choice for detecting SEA [1–8]. Furthermore, it permits detection of associated infections of the intervertebral discs, the vertebrae, and the paraspinal space. In our patient, MRI also provided accurate identification of fistulous channel on the posterior pharyngeal wall through which bacterial contamination occurred.
Conclusion
Cervical SEA may be caused by iatrogenic perforation of pharyngeal wall during diagnostic oesophagoscopy. Early diagnosis with MRI, surgical decompression and abscess drainage, long-term intravenous antibiotics, and physical therapy are keys to successful management with a good functional outcome of this unfortunate complication.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000;232:175–204. doi: 10.1007/PL00011954. [DOI] [PubMed] [Google Scholar]
- 2.Lam KS, Pande KC, Mehdian H. Surgical decompression: a life-saving procedure for an extensive spinal epidural abscess. Eur Spine J. 1997;6:332–335. doi: 10.1007/BF01142681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sampath P, Rigamonti D. Spinal epidural abscess: a review of epidemiology, diagnosis, and treatment. J Spinal Disord. 1999;12:89–93. doi: 10.1097/00002517-199904000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Rigamonti D, Liem L, Sampath P, Knoller N, Namaguchi Y, Schreibman DL, Sloan MA, Wolf A, Zeidman S. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999;52:189–196. doi: 10.1016/S0090-3019(99)00055-5. [DOI] [PubMed] [Google Scholar]
- 5.Lu CH, Chang WN, Lui CC, Lui CC, Lee PY, Chang HW. Adult spinal epidural abscess: clinical features and prognostic factors. Clin Neurol Neurosurg. 2002;104:306–310. doi: 10.1016/S0303-8467(02)00020-3. [DOI] [PubMed] [Google Scholar]
- 6.Chen Y, Kim BJ, Lee SH, Hu SS. High thoracic spinal infection following upper gastrointestinal work-up. J Clin Neurosci. 2007;14(11):1132–1135. doi: 10.1016/j.jocn.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 7.Ekbom DC, D-Elia J, Isaacson B, Lamarca F, Chepeha DB, Bradford CR. Spinal epidural abscess after cervical pharyngoesophageal dilation. Head Neck. 2005;27(6):543–548. doi: 10.1002/hed.20183. [DOI] [PubMed] [Google Scholar]
- 8.Metcalfe S, Morgan-Hough C. Cervical epidural abscess and vertebral osteomyelitis following non-traumatic oesophageal rupture: a case report and discussion. Eur Spine J. 2009;18(Suppl 2):224–227. doi: 10.1007/s00586-009-0889-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barr RJ, Hannon DG, Adair IV, McCoy GF. Cervical osteomyelitis after rigid oesophagoscopy: brief report. J Bone Joint Surg Br. 1988;70(1):147–148. doi: 10.1302/0301-620X.70B1.3339050. [DOI] [PubMed] [Google Scholar]


