Abstract
Introduction
Intraspinal teratomas associated with congenital scoliosis are extremely rare, especially in an elderly adult.
Materials and methods
We report the seventh case of intraspinal extramedullary teratoma coexisting with congenital scoliosis in a patient older than 50 years, possibly the oldest patient documented in literature. A 56-year-old male suffered from low back pain that increased with calf numbness and foot weakness. Conventional radiography showed a congenital scoliosis due to incomplete segmentation of the L2 and L4 vertebras, and magnetic resonance images revealed a heterogeneous intraspinal extramedullary mass located at L4-S1.
Results
The tumor was totally removed, and was confirmed as a mature teratoma on biopsy. The patient remains asymptomatic at 34-month follow-up.
Conclusions
Rare intraspinal teratoma should be included in the differential diagnosis of intraspinal mass, especially in patient with congenital scoliosis. Patient with mature teratoma may survive with out any symptoms in the long term. Progressing neurological deficit is a main indication for surgery. Excellent clinical outcomes could be achieved by surgical resection and dural sac decompression.
Keywords: Teratoma, Congenital scoliosis , Surgery
Introduction
Spinal teratomas associated with congenital scoliosis are very uncommon [1], which have been previously reported with the majority occurring in the pediatric population [2–7]. Intraspinal teratoma coexisting with congenital scoliosis in the adult is considered to be an extremely rare entity. We present an unusual case of lumbar teratoma in a 56-year-old patient with congenital scoliosis, possibly the oldest patient recorded in the literature.
Case report
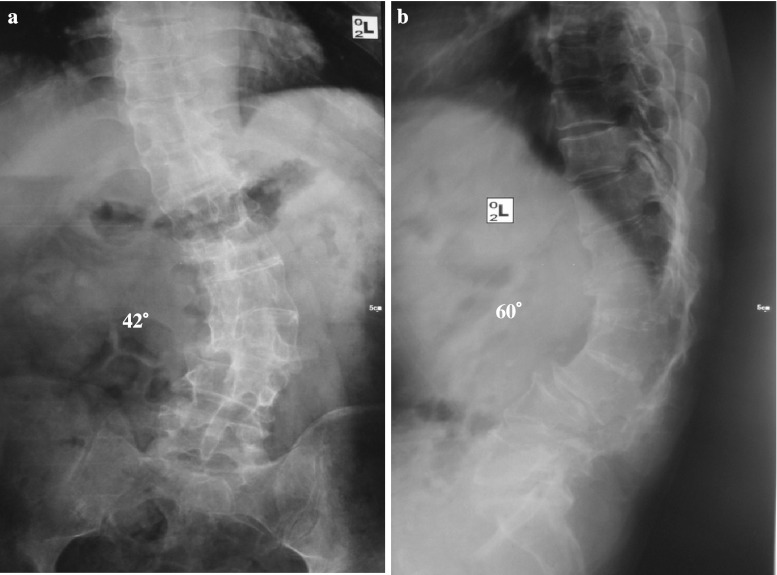
A 56-year-old man was admitted to our hospital with a 1-year history of low back pain and radiating pain in both posterior calves. In the last 2 months, his symptoms progressed gradually to calf numbness and foot weakness. He had neither history of trauma nor any other spinal procedures. Neurological examination revealed weakness of the both extensor hallucis longus. Straight leg raise was positive at 40° bilaterally. A sensory deficit involved left anterior tibial and dorsalis pedis. No abnormal hairy patch or dimple was found in the skin over the lumbosacral region. The X-ray of the lumbar spine demonstrated a left curve of 42° (Fig. 1a), and a kyphosis of 60° (Fig. 1b). Incomplete segmentation of the L2 and L4 vertebras was noted on plain radiographs. Magnetic resonance (MR) images indicated a heterogeneous intraspinal extramedullary mass located at L4-S1 levels. The intraspinal lesion showed inhomogeneous high and low signal intensity on T1WI and T2WI (Fig. 2a, b). MR images of the whole spine displayed no cord tether, syrinx or other dysraphic abnormality.
Fig. 1.
A 56-year-old male with a 42° left lumbar scoliosis and a 60° kyphosis due to unilateral unsegmented bar
Fig. 2.
MR images revealing a T1-hyperintense (a) and T2-hypointense (b) intraspinal mass at L4-S1 levels
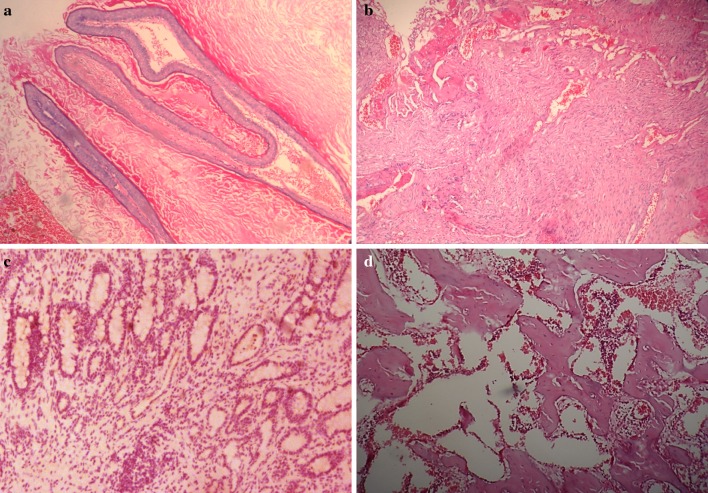
As the patient denied the surgical correction of scoliosis, the surgeons proceeded to remove the tumor without treating spinal deformity. During surgery, a L4-L5 total laminectomy and S1 partial laminectomy were performed. After the dura was opened, the cystic mass could be visualized without any firm attachment posteriorly to the dura. Consequently the tumor was totally removed, which contained brown hair and cartilaginous tissue (Fig. 3). Histological examination demonstrated a mature tridermal teratoma with fully differentiated components including stratified squamous epithelium, neural tissue, enteric glandular cells and cartilage (Fig. 4). The patient had complete resolution of their neurological symptoms within 3 months postoperatively. There was no obvious progression of the kyphoscoliosis at 34-month follow-up.
Fig. 3.

Postoperative photographs demonstrating the tumor with hair shaft, cartilage, fibrous tissue and adipose tissue
Fig. 4.
Photomicrographs of the tumor specimen showing tissues derived from all three germ layers: a stratified squamous epithelium, b neural tissue, c enteric glandular cells, d cartilage, hematoxylin and eosin, original magnification (×100)
Discussion
The incidence of intraspinal teratomas is low, and these tumors account for approximately 0.5–2.2 % of all intraspinal tumors [1, 8]. Intraspinal teratomas have been commonly reported in relation to abnormal neural tube including diastematomyelia, myelomeningocele and tethered cord syndrome [9, 10]. The occurrence of intraspinal teratomas associated with congenital scoliosis is rare, and is more common among infants and adolescents than among adults [8]. Only six studies on spinal teratomas coexisting with congenital scoliosis have been previously reported [2–7] (Table 1). To our knowledge, we present the seventh case of a mature intraspinal teratoma associated with congenital scoliosis in a 56-year-old male who may be the oldest patient documented in the literature.
Table 1.
Cases of intraspinal teratomas associated with congenital scoliosis
| Case author | Year | Age | Gender | Location of teratoma | Spinal anomalies | Treatment of teratoma | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1 | Cameron [2] | 1957 | NB | M | Extramedullary, lumbar | Congenital kyphoscoliosis | None | Died |
| 2 | McMaster [3] | 1984 | 4 y | F | Intradural, thoracolumbar | Scoliosis, left lower limb hypoplasia, thoracolumbar cutaneous lipoma | Surgery (extent not specified) |
Improved at 8 y |
| 3 | Koen et al. [4] | 1998 | 14 m | M | Intradural, thoracic | T5–6 Hemivertebra, absent 6th rib, scoliosis | Gross total resection | NS |
| 4 | Hader et al. [5] | 1999 | 16 y | F | Intramedullary, thoracic | T7–9 Hemivertebra, scoliosis | Subtotal resection | Symptom free at 2 m |
| 5 | Jarmundowicz et al. [6] | 2004 | 13 y | F | Intraspinal, lumbar | Split cord malformation, scoliosis | Subtotal resection | NS |
| 6 | Suri et al. [7] | 2006 | 8 y | M | Intraspinal, thoracic | Hole in T4 vertebral body, butterfly vertebra, scoliosis | Gross total resection | Symptom free at 1 y |
| 7 | Present case | 2008 | 56 y | M | Intraspinal, lumbar | L3–4 Incomplete segmentation, scoliosis | Gross total resection | Symptom free at 3 m |
NB newborn, NS not specified, m months, y years
The etiology of spinal teratoma has not been fully understood. Several hypotheses have been proposed, including the dysembryogenic theory and misplaced germ cell theory [11]. Our case is considered to support misplaced germ cell theories because, it is an instance of adult teratoma without dysraphism. Additionally, several authors reported that intraspinal teratoma can occur in adults after trauma or surgical interventions [12, 13]. However, the patient in the present study had neither history of trauma nor any other spinal procedures.
Preoperative diagnosis of spinal teratoma is not easy. The role of plain radiography is limited to detect the vertebral abnormalities including hemi vertebrae, butterfly vertebrae and block vertebrae [14]. In the current case, X-ray images revealed incomplete segmentation of the L2 and L4 vertebras leading to lumbar kyphoscoliosis. Furthermore, MR scans may provide more information about intraspinal lesions. Heterogeneous signal intensity on MR images indicated a solid and cystic composition of the tumor, which would be helpful for diagnosis of teratomas in the early stage [11, 13]. Correspondingly, teratomas in histopathology are composed of the heterogeneous remnants of all three germ cell layers, and are classified as mature, immature or malignant type [10]. Mature teratomas, represented by our case, contained fully differentiated tissue elements such as cartilage, squamous epithelial cells, glands, mucosal tissue and neural elements.
As posterior correction and fusion were currently widely used for the treatment of congenital scoliosis [15], two-stage surgical treatment was recommended in our preoperative procedures including tumor resection and scoliosis correction. However, the patient in this case denied the scoliosis correction, because of socio-economic restriction. Fortunately, his neurological symptoms had been completely resolved within 3 months after tumor removal. Nonetheless, we strongly recommend that surgical procedures for intraspinal teratoma coexisting with congenital scoliosis be performed in two stages, and the intraspinal anomalies be treated surgically before management of scoliosis.
Conclusion
Intraspinal extramedullary teratoma associated with congenital scoliosis is extremely uncommon, especially in patients over 50 years. Heterogeneous signal intensity on MR images indicated a solid or cystic composition of the tumor, which would be helpful for diagnosis of teratoma in early stage. The good outcome could be achieved by surgical resection, because the clinical symptoms may be mainly attributed to dural sac compression by intraspinal teratoma.
Acknowledgments
The authors are grateful to the pathological data of the patient provided by the department of pathology of our hospital.
Conflict of interest
None.
References
- 1.Nonomura Y, Miyamoto K, Wada E, Hosoe H, Nishimoto H, Ogura H, Shimizu K. Intramedullary teratoma of the spine: report of two adult cases. Spinal Cord. 2002;40:40–43. doi: 10.1038/sj.sc.3101247. [DOI] [PubMed] [Google Scholar]
- 2.Cameron AH. Malformations of the neuro-spinal axis, urogenital tract and foregut in spina bifida attributable to disturbances of the blastopore. J Pathol Bacteriol. 1957;73:213–221. doi: 10.1002/path.1700730125. [DOI] [Google Scholar]
- 3.McMaster MJ. Occult intraspinal anomalies and congenital scoliosis. J Bone Joint Surg Am. 1984;66:588–601. [PubMed] [Google Scholar]
- 4.Koen JL, McLendon RE, George TM. Intradural spinal teratoma: evidence for a dysembryogenic origin report of four cases. J Neurosurg. 1998;89:844–851. doi: 10.3171/jns.1998.89.5.0844. [DOI] [PubMed] [Google Scholar]
- 5.Hader WJ, Steinbok P, Poskitt K, Hendson G. Intramedullary spinal teratoma and diastematomyelia: case report and review of the literature. Pediatr Neurosurg. 1999;30:140–145. doi: 10.1159/000028782. [DOI] [PubMed] [Google Scholar]
- 6.Jarmundowicz W, Tabakow P, Markowska-Woyciechowska A. Composite split cord malformation coexisting with spinal cord teratoma—case report and review of the literature. Folia Neuropathol. 2004;42:55–57. [PubMed] [Google Scholar]
- 7.Suri A, Ahmad FU, Mahapatra AK, Mehta VS, Sharma MC, Gupta V. Mediastinal extension of an intradural teratoma in a patient with split cord malformation: case report and review of literature. Childs Nerv Syst. 2006;22:444–449. doi: 10.1007/s00381-005-1240-3. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez-Cornejo VJ, Martinez-Perez M, Polo-Garcia LA, Martinez-Lage JF, Poza M. Cystic mature teratoma of the filum terminale in an adult: case report and review of the literature. Neurocirugia (Astur) 2004;15:290–293. doi: 10.1016/s1130-1473(04)70486-8. [DOI] [PubMed] [Google Scholar]
- 9.Makary R, Wolfson D, Dasilva V, Mohammadi A, Shuja S. Intramedullary mature teratoma of the cervical spinal cord at C1–2 associated with occult spinal dysraphism in an adult: case report and review of the literature. J Neurosurg Spine. 2007;6:579–584. doi: 10.3171/spi.2007.6.6.12. [DOI] [PubMed] [Google Scholar]
- 10.Ak H, Ulu MO, Sar M, Albayram S, Aydin S, Uzan M. Adult intramedullary mature teratoma of the spinal cord: review of the literature illustrated with an unusual example. Acta Neurochir (Wien) 2006;148:663–669. doi: 10.1007/s00701-006-0755-z. [DOI] [PubMed] [Google Scholar]
- 11.Park SC, Kim KJ, Wang KC, Choe G, Kim HJ. Spinal epidural teratoma: review of spinal teratoma with consideration on the pathogenesis: case report. Neurosurgery. 2010;67:E1818–E1825. doi: 10.1227/NEU.0b013e3181f846ca. [DOI] [PubMed] [Google Scholar]
- 12.Per H, Kumandas S, Gumus H, Yikilmaz A, Kurtsoy A. Iatrogenic epidermoid tumor: late complication of lumbar puncture. J Child Neurol. 2007;22:332–336. doi: 10.1177/0883073807300531. [DOI] [PubMed] [Google Scholar]
- 13.Ziv ET, Gordon McComb J, Krieger MD, Skaggs DL. Iatrogenic intraspinal epidermoid tumor: two cases and a review of the literature. Spine (Phila Pa 1976) 2004;29:E15–E18. doi: 10.1097/01.BRS.0000104118.07839.44. [DOI] [PubMed] [Google Scholar]
- 14.Ugarte N, Gonzalez-Crussi F, Sotelo-Avila C. Diastematomyelia associated with teratomas report of two cases. J Neurosurg. 1980;53:720–725. doi: 10.3171/jns.1980.53.5.0720. [DOI] [PubMed] [Google Scholar]
- 15.Arlet V, Odent T, Aebi M. Congenital scoliosis. Eur Spine J. 2003;12:456–463. doi: 10.1007/s00586-003-0555-6. [DOI] [PMC free article] [PubMed] [Google Scholar]