Abstract
Prospective studies have suggested genetic variation in the neuregulin 1 (NRG1) and 𝒟-amino-acid oxidase activator (DAOA) genes may assist in differentiating high-risk individuals who will or will not transition to psychosis. In a prospective cohort (follow-up=2.4–14.9 years) of 225 individuals at ultra-high risk (UHR) for psychosis, we assessed haplotype-tagging single-nucleotide polymorphisms (htSNPs) spanning NRG1 and DAOA for their association with transition to psychosis, using Cox regression analysis. Two NRG1 htSNPs (rs12155594 and rs4281084) predicted transition to psychosis. Carriers of the rs12155594 T/T or T/C genotype had a 2.34 (95% confidence interval (CI)=1.37–4.00) times greater risk of transition compared with C/C carriers. For every rs4281084 A-allele the risk of transition increased by 1.55 (95% CI=1.05–2.27). For every additional rs4281084-A and/or rs12155594-T allele carried the risk increased ∼1.5-fold, with 71.4% of those carrying a combination of ⩾3 of these alleles transitioning to psychosis. None of the assessed DAOA htSNPs were associated with transition. Our findings suggest NRG1 genetic variation may improve our ability to identify UHR individuals at risk for transition to psychosis.
Keywords: gene, neuregulin 1, prediction, prodrome, risk, schizophrenia
Introduction
Identification of individuals at high risk for psychotic disorder has proven challenging. The development and validation of standardized clinical criteria to detect individuals at ultra-high risk (UHR) of psychosis has improved our ability to identify individuals at the greatest risk for transition from an at-risk state to frank-level psychotic symptoms.1, 2, 3, 4, 5, 6 Transition rates to psychotic disorder were found to be 18% 6 months after identification in a high-risk clinic, 22% after 1 year, 29% after 2 years and 36% after 3 years in a meta-analysis of 27 studies including 2 500 patients.7 Most (about 70%) of those who developed psychotic disorder had a diagnosis of schizophrenia-spectrum disorder.8 However, the majority of individuals meeting UHR criteria do not develop psychosis.9 Thus, use of secondary markers within the UHR group could further improve our ability to identify those most at risk.
Previous research has identified clinical features, such as severity of negative symptoms,2, 10, 11, 12 sub-threshold positive symptoms and poor life functioning,5, 13, 14 as well as neuroimaging markers, such as insula and pituitary volumes,15, 16 thickness of anterior cingulate cortex and corpus callosum,17, 18 and whole-brain neuroanatomical abnormalities19 as predictive markers of transition to psychosis in those at UHR. Neurocognitive markers have been less consistent, though recent meta-analyses20, 21, 22 suggest verbal fluency, memory functioning and olfactory identification as potential promising predictors. Interestingly, a recent review of predictive models for psychosis transition has concluded that measures of psychopathology, life functioning and brain imaging are the strongest predictors of psychosis transition, regardless of the predictive algorithm used.23 Although such markers are promising, they may represent ‘state' rather than ‘trait' markers, given the dynamic brain changes identified in these earliest stages of psychosis.24 Markers that are not influenced by such brain changes would include DNA sequence variation.
Recently, DNA sequence variation in two promising candidate genes for schizophrenia,25 neuregulin 1 (NRG1) and 𝒟-amino acid oxidase activator (DAOA), have been examined for their ability to differentiate high-risk individuals who will or will not transition to psychosis. Hall et al.26 and Keri et al.27 reported that the T/T genotype of the SNP8NRG243177 (rs6994992) located in the NRG1 HapICE schizophrenia-risk haplotype28 was associated with a 100% psychosis transition rate in two independent high-risk populations, the first a genetic high-risk (for example, family history of schizophrenia) sample and the second a clinical high-risk sample. Furthermore, Mossner et al.29 examined variation in the DAOA gene and found 100% of UHR individuals carrying the rs1341402 T/T genotype and 50% of those carrying the rs778294 A/A genotype transitioned to psychosis.
These seminal studies support the notion that genotypic-based tools could be used to identify UHR individuals who will or will not transition to psychosis. However, before these findings can become clinically useful, critical limitations related to the small number of individuals must be examined (N range: 67–82) as well as potential confounders (for example, duration of symptoms, cannabis use, medication, etc.) and biases (departures from Hardy–Weinberg equilibrium30) must be addressed.
In the present study, we sought to examine the effect of NRG1 and DAOA gene variants on transition to psychosis within the largest and longest running UHR cohort assembled to date. We hypothesized that if genetic variation in NRG1 and DAOA are independent markers for transition to psychosis, then they should be replicable and detectable after adjustment for possible confounders.
Materials and methods
Study population
Participants were recruited as part of a large follow-up study at the PACE (Personal Assessment and Crisis Evaluation) Clinic at Orygen Youth Health in Melbourne, Australia that aimed to locate and reassess all participants identified as UHR for psychosis between 1993 and 2006. At baseline, all participants met the PACE UHR criteria, rated on the CAARMS (Comprehensive Assessment of At-Risk Mental States).2 These criteria are (1) attenuated psychotic symptoms, (2) brief limited intermittent psychotic symptoms, and/or (3) trait vulnerability for psychotic illness (schizotypal personality disorder or a history of psychosis in a first-degree relative) and deterioration in functioning or chronic low functioning. The age range accepted to PACE was 15–30 years from 1993 to 2006 and changed in 2006 to 15–25 years owing to service system changes. Exclusion criteria at baseline were current or past psychotic disorder (treated or untreated), known organic cause for presentation and past neuroleptic exposure equivalent to a total continuous haloperidol dose of >50 mg (as this could modify the risk of transition). Participants underwent a face-to-face follow-up interview, including assessment of psychopathology and functioning 2.4–14.9 years after baseline.
Phenotypic variables
Outcome
The main outcome of interest was transition to psychosis. This was defined as at least one fully positive psychotic symptom several times a week for over 1 week. From 1993 to 1995, this was assessed using a combination of the Brief Psychiatric Rating Scale (BPRS; to assess intensity of psychotic experience)31 and the Comprehensive Assessment of Symptoms and History (to assess conviction).32 Since 1996, psychosis status was determined by the Comprehensive Assessment of At Risk Mental States (CAARMS).2 This allows intensity, conviction, frequency, recency and duration to be assessed comprehensively using one instrument that has well-defined anchor points. The CAARMS has good to excellent reliability.2 If CAARMS data were not available (for example, because of not being able to locate the subject), the state public mental health records were consulted to determine whether the person had any contact with public psychiatric services since last contact with PACE and, if so, whether they had been diagnosed with a psychotic disorder.
Potential confounders
At baseline, negative symptoms were assessed using the Scale of Assessment for Negative Symptoms (SANS),33 and positive symptoms with the BPRS, psychotic subscale.31 Functioning and disability of participants was determined using the Quality of Life Scale34 and the Global Assessment of Functioning Scale (GAF).35 Lifetime alcohol, cannabis, opioid, sedative, stimulant, hallucinogen and inhalant use were determined using a substance use questionnaire. Any treatment (for example, medication) that participants received during their time at PACE was also recorded.
Psychopathological and clinical data were collected by trained research assistants. All procedures were conducted in accord with principles expressed in the Declaration of Helsinki and obtained approval from the Melbourne Health Human Research Ethics Committee.
Single-nucleotide polymorphism selection
For both the NRG1 and DAOA genes, 17 haplotype-tagging single-nucleotide polymorphisms (htSNPs) spanning each gene and ∼500 kbp of the 5′ flanking region were selected using the International Haplotype Map (HapMap) Project (release 27) and Tagger.36 The minimum pairwise linkage disequilibrium rate and minor allele frequency were set at 0.80 and 0.20, respectively. In addition, the three single-nucleotide polymorphisms (SNPs; NRG1: rs6994992, DAOA: rs1341402 and rs778294) previously associated with transition were included.26, 27, 29 Where applicable, the traditional M nomenclature37 for DAOA htSNPs was used. To determine the presence of population stratification, 60 unlinked ancestry informative markers (AIMs; Supplementary Table S1) representing three HapMap phase III populations (Northern/Western European, Han Chinese, and Yoruba in Nigeria) were also genotyped.38
DNA isolation and genotyping
DNA was isolated from Oragene DNA sample collection kits (DNA Genotek, Kanata, ON, Canada) using the Autopure LS nucleic-acid purification system and Qiagen Puregene salting out methodology (Qiagen, Valencia, CA, USA) at Genetic Repositories Australia. Extracted DNA was quantified fluorometrically using Quant-iT PicoGreen dsDNA reagent (Invitrogen, Mulgrave, Victoria, Australia) on an Eppendorf Mastercycler RealPlex (Eppendorf South Pacific, North Ryde, New South Wales, Australia) and stored in 1.0 × tris-EDTA buffer at −80 °C until required.
htSNPs were genotyped with the Sequenom MassARRAY MALDI-TOF genotyping system using Sequenom iPLEX Gold chemistries, according to manufacturer's instructions. The 60 AIMs and 37 htSNPs were multiplexed into four separate assays, using the Assay Design v3.1 software (Sequenom, San Diego, CA, USA). Two htSNPs (rs6994992 and rs1341402) were unable to be multiplexed using the assay design program; these assays were designed manually. PCR and extension primers for each genotyped SNP are listed in Supplementary Table S2. A random selection of 10% of samples was genotyped twice for all candidate htSNPs. Data analysis was performed in a semiautomated manner using the Typer 4.0 Analyser Software (Sequenom). All genotype calls not assessed as ‘conservative' by the analysis program were manually checked by the operator and discarded if a clear call could not be made. Genotyping accuracy was assessed by checking concordance among the 10% of samples genotyped twice.
Statistical analysis
The CubeX program39 was applied to detect departures from Hardy–Weinberg equilibrium, determine minor allele frequency, and estimate pairwise linkage disequilibrium measures r2 and D′. SNPs with Hardy–Weinberg equilibrium <0.01 or minor allele frequency <0.10 were excluded from the analysis. Utilizing the 60 AIMs, participants were assigned to the HapMap ancestral group (Northern/Western European, Han Chinese and Yoruba in Nigeria) for which they carried the greatest proportion of that population's AIMs. Cox proportional hazard regression (that is, time-to-event) analysis was used to estimate univariate hazard ratios for each htSNP on transition to psychosis. Where applicable, multivariate Cox regressions were also conducted, which adjusted for factors previously shown to predict transition to psychosis (that is, age, sex, GAF score, BPRS total and psychotic subscale scores, SANS attention subscale, lifetime cannabis use and duration of symptoms).5, 13 A Bonferroni correction was applied to adjust for multiple comparisons and guard against reporting false-positive findings. Raw P-values for the DAOA and NRG1 analyses were multiplied by the number of htSNPs examined to derive an adjusted P-value.
Results
Of the 416 individuals enrolled in the PACE UHR cohort, 247 (59.3%) underwent a face-to-face interview that included assessment of psychopathology and DNA collection at follow-up. We excluded 13 individuals that were of non-European ancestry based on the 60 unlinked AIMs, as well as nine individuals missing a majority of phenotypic data. This resulted in 225 individuals included in the analysis.
Over one-quarter (26.6%, n=60) of participants transitioned over the follow-up period. The mean number of days to transition was 572 (s.d.=710; median=281, range=4–3537) and the mean age of those who transitioned was 20.2 (s.d.=4.1; median=19.2, range=14–31). Table 1 provides characteristics of all participants at baseline and follow-up assessments.
Table 1. Participant characteristics at baseline and follow-up (n=225).
| Baseline | |
|---|---|
| PACE entry criteriaa, % (n) | |
| APS only | 61.0 (133) |
| BLIPS only | 5.0 (11) |
| Vulnerability only | 14.7 (32) |
| APS and BLIPS | 7.8 (17) |
| APS and vulnerability | 13.8 (30) |
| BLIPS and vulnerability | 3.2 (7) |
| All three criteria | 2.8 (6) |
| Age, mean (s.d.) years | 18.6 (3.3) |
| Gender, % (n) female | 58.2 (132) |
| Time from Sx onset to study enroll, mean (s.d.) days | 407 (488) |
| BPRS total, mean (s.d.) | 47.4 (10.0) |
| BPRS psychosis subscale, mean (s.d.) | 9.5 (3.0) |
| SANS total, mean (s.d.) | 19.7 (13.3) |
| GAF, mean (s.d.) | 58.7 (11.4) |
| QLS total score, mean (s.d.) | 76.1 (23.2) |
| Substance useb, % (n) ever used | |
| Alcohol | 88.2 (186) |
| Cannabis | 50.0 (107) |
| Opioids | 2.8 (6) |
| Sedatives | 10.3 (22) |
| Stimulants | 22.4 (48) |
| Hallucinogens | 13.6 (29) |
| Inhalants | 9.3 (20) |
| Follow-up | |
| Time from baseline to follow-up, mean (s.d.) days | 2698 (1189) |
| Age of censored/psychosis onset, mean (s.d.) years | 24.0 (5.2) |
| Time to psychosis transition, mean (s.d.) days | 552 (710) |
| Received trail treatment at PACE, % (n) yes | |
| Case management | 100 (225) |
| Risperdone | 11.1 (25) |
| Olanzapine | 0.4 (1) |
| Lithium | 5.8 (13) |
| Cognitive behavioral therapy | 94.2 (212) |
Abbreviations: APS, attenuated psychotic symptoms; BLIPS, brief limited intermittent psychotic symptoms; BPRS, Brief Psychiatric Rating Scale; GAF, Global Assessment of Functioning; QLS, Quality of Life Scale; SANS, Scale of Assessment for Negative Symptoms; Sx, symptoms.
PACE entry criteria was unavailable for five participants.
Substance use information was unavailable for six participants.
Characterization of the htSNPs in NRG1 and DAOA (Supplementary Tables S3 and S4) revealed all htSNPs in both genes were in Hardy–Weinberg equilibrium (P>0.01). One NRG1 htSNP (rs62497784) had a minor allele frequency <10% and was removed from further analyses. In addition, three pairs of htSNPs (rs7320588-rs1335075; rs2391191-rs3918341; rs3918342-rs1421292) in the DAOA gene were in strong LD (r2>0.80); arbitrarily we retained the htSNP closest to the 5′ end of the gene from each pair for further analysis. Thus, 16 DAOA and 17 NRG1 htSNPs were included in hypothesis testing. Genotyping accuracy based on re-genotyping a random 10% of the sample revealed 100% concordance for all NRG1 htSNPs, and 96–100% for DAOA htSNPs (Supplementary Table S5).
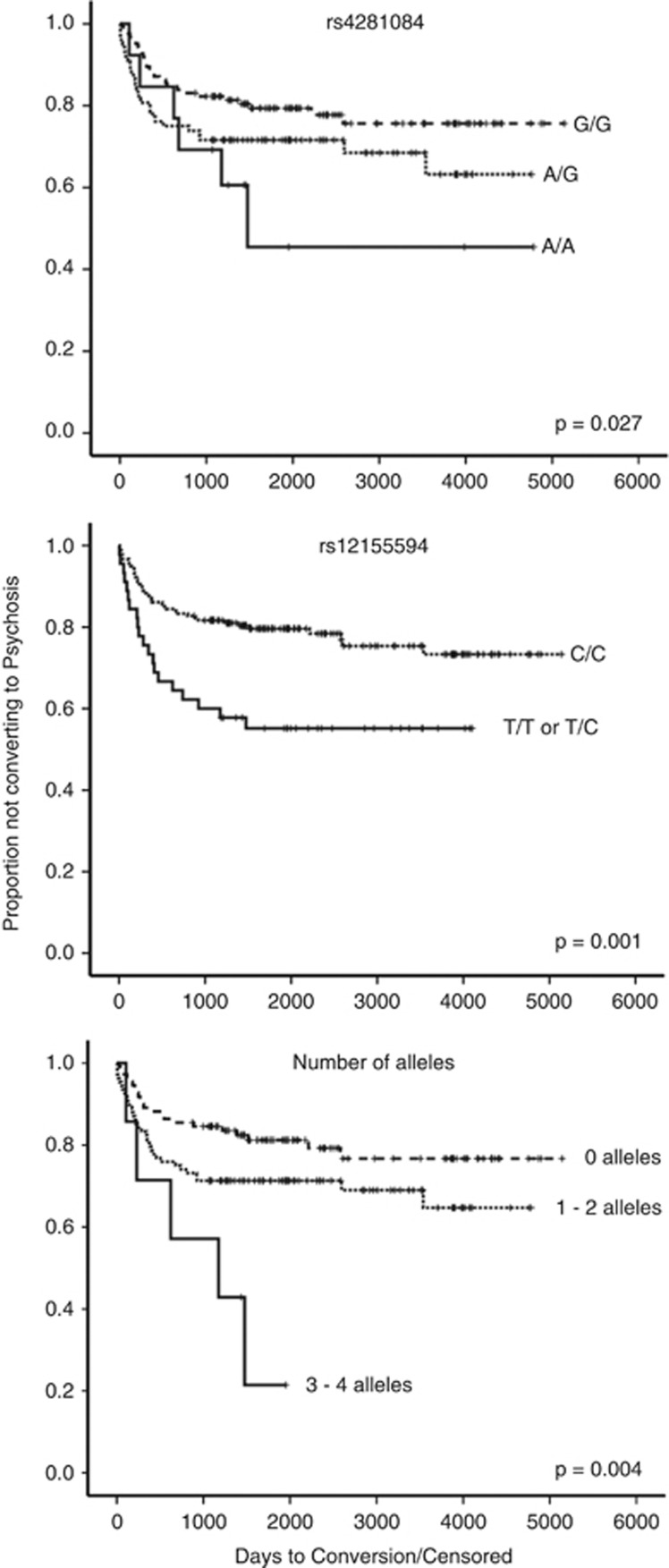
None of the examined DAOA htSNPs reached statistical significance (Supplementary Table S6). However, two (rs12155594 and rs4281084) NRG1 htSNPs were shown to predict transition to psychosis (Supplementary Table S7). Carriers of the rs12155594 T/T or T/C genotype had a 2.34 (95% confidence interval (CI)=1.37–4.00, raw P=0.001) greater risk of transition compared with C/C carriers. Similarly, for every rs4281084 A-allele the risk for transition increased by a factor of 1.55 (95% CI=1.05–2.27, raw P=0.027). For every additional rs4281084 A-allele and/or rs12155594 T-allele carried, the risk for transition increased 1.56 times (95% CI=1.20–2.04, raw P=0.004) (Figure 1). However, only rs12155594 remained significant after adjustment for multiple comparisons (Bonferroni P=0.033; Supplementary Table S7) and adjustment for factors previously shown to predict transition to psychosis5, 13 (Table 2). Examination of baseline and follow-up clinical characteristics by rs12155594 genotype (Supplementary Table S8) showed no significant differences, with the exception of T-allele (T/T or T/C) carriers meeting PACE entry criteria for attenuated psychotic symptoms and trait vulnerability for psychosis in greater proportion compared with C/C carriers (29.5% versus 9.8% χ2=11.5, df=1, P=0.001).
Figure 1.
Kaplan–Meier estimates of the rate of psychosis transition in ultra-high risk (UHR) individuals by NRG1 rs4281084 (top), rs12155594 (middle), rs4281084 A-alleles and rs1255594 T-alleles (bottom). The Cox proportional hazards model was used.
Table 2. Univariate and multivariate Cox regression models for progression to psychosis (N=225).
| Variables |
Model 1 |
Model 2 |
Model 3 |
|||
|---|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | |
| Univariate models | ||||||
| rs4281084 (NRG1) | 1.55 (1.05–2.27) | 0.027 | ||||
| rs12155594 (NRG1) | 2.29 (1.39–3.78) | 0.001 | ||||
| Number of risk allelesa | 1.56 (1.20–2.04) | 0.001 | ||||
| Multivariate models | ||||||
| rs4281084 | 1.48 (0.97–2.25) | 0.071 | ||||
| rs12155594 | 2.06 (1.21–3.49) | 0.008 | ||||
| Number of risk allelesa | 1.47 (1.11–1.95) | 0.007 | ||||
| Age | 0.97 (0.89–1.05) | 0.428 | 0.97 (0.89–1.05) | 0.410 | 0.97 (0.88–1.05) | 0.415 |
| Sex | 1.00 (0.57–1.76) | 0.999 | 1.04 (0.59–1.82) | 0.907 | 1.00 (0.57–1.76) | 0.999 |
| Duration of symptomsb | 1.00 (1.00–1.01) | 0.105 | 1.00 (1.00–1.01) | 0.076 | 1.00 (1.00–1.01) | 0.112 |
| GAF score | 0.95 (0.92–0.98) | 0.002 | 0.95 (0.92–0.98) | 0.003 | 0.95 (0.92–0.98) | 0.002 |
| BPRS total score | 0.95 (0.90–0.99) | 0.042 | 0.95 (0.91–1.01) | 0.078 | 0.95 (0.90–0.99) | 0.048 |
| BPRS psychotic subscale | 1.07 (0.93–1.24) | 0.340 | 1.08 (0.92–1.24) | 0.340 | 1.08 (0.93–1.25) | 0.319 |
| SANS attention subscale | 1.10 (0.95–1.28) | 0.195 | 1.09 (0.94–1.27) | 0.239 | 1.10 (0.94–1.27) | 0.237 |
| Cannabis use (yes) | 0.34 (0.10–1.31) | 0.078 | 0.31 (0.09–1.03) | 0.060 | 0.31 (0.09–1.07) | 0.064 |
Abbreviations: BPRS, Brief Psychiatric Rating Scale; CI, confidence interval; GAF, Global Assessment of Functioning; HR, hazard ratio; SANS, Scale for the Assessment of Negative Symptoms.
rs4281084 A-alleles+rs1255594 T-alleles.
Time between onset of symptoms and first contact with PACE Clinic.
Discussion
Our findings suggest that NRG1 genetic variation may improve our ability to identify UHR individuals at risk for transition to frank psychosis. We found in the largest and longest running cohort of UHR individuals reported to date, that nearly half (46.2%) of the NRG1 rs4281084 AA genotype carriers and 44% of those carrying a rs12155594 T-allele transitioned to psychosis, a 1.55 and 2.29 increase in risk compared with those carrying the G-allele and CC genotype, respectively. For every additional rs4281084-A and/or rs12155594-T allele carried, the risk increased ∼1.5-fold, with 71.4% of those carrying a combination of ⩾3 of these alleles transitioning to psychosis. Notably, the rs4281084 association did not survive correction for multiple comparisons and did not remain significant after adjusting for factors previously shown to predict transition to psychosis,5, 13 suggesting a potential false-positive finding.
Our findings are in contrast with the two previous studies that examined the association between NRG1 variation and transition to psychosis,26, 27 in which a significant risk-conferring effect for the T/T genotype of the rs6994992 (SNP8NRG243177) located in the HapICE schizophrenia-risk haplotype28 was observed. The risk-conferring rs4281084 SNP in the current study is positioned 207 base pairs upstream from rs6994992 and was in moderate linkage disequilibrium (D'=1.0, r2=0.23), whereas the rs12155594 SNP is located in intron 1 between two HapICE microsatellite repeats (478B14–848 and 420M9–1395). Thus, our findings point to a potentially generalized HapICE haplotype region effect for transition to psychosis, in which any number of polymorphisms in this region may confer risk for transition. This interpretation is supported by the absence of any significant main effects in the current study for NRG1 htSNPs located outside the boundaries of the HapICE risk haplotype region, albeit htSNP coverage outside this region may not have been dense enough to detect such an effect. Our results also align with the notion that discrepancies among identified risk-conferring SNPs between studies are the expectation rather than the exception. In fact, meta-analyses40, 41, 42, 43 suggest that specific NRG1 risk alleles are likely to vary between populations, and more recently Weickert et al.44 suggested that the risk conveyed by sequence variation within NRG1 is likely not to be driven by one SNP, but a diverse accumulation of nucleotide changes.
The mechanism by which the NRG1 genotypic variation observed might confer risk for transition to psychosis is not clear. However, Law et al.45 have suggested NRG1 genotypic variation, particularly in the HapICE region of the gene, in post-mortem brain is associated with NRG1 type IV isoform expression. More recently, an Australian post-mortem brain study44 has shown that the risk-conferring 5-SNP HapICE haplotype28 is associated with increased NRG1 type III (that is, sensory and motor neuron-derived factor) isoform expression and an additional cluster of SNPs in intron 1, including the 478B14-848 microsatellite, was associated with increased type II (that is, glial growth factor) isoform expression. Increased NRG1 type III isoform expression was also associated with earlier age of onset. Interestingly, in the human brain, NRG1 type III and II isoforms are the most abundant (73% and 21%, respectively).46 Type III isoform expression has been associated with lateral ventricle enlargement, axonal myelination, and reduced prefrontal cortex and hippocampus function in animal models,47, 48 whereas type II NRG1 has been linked to Schwann cell development, myelination and ensheathment of primary nerves49, 50 as well as protection of dopaminergic neurons.51 Given that the two risk-conferring SNPs (rs42810894 and rs12155594) in the current study are located within this region, it would seem possible that these htSNPs are also associated with expression and age of onset or are successfully ‘tagging' for the polymorphisms that have been previously implicated in schizophrenia. Additional research is needed to determine the biological and clinical effects of increased NRG1 gene expression, particularly during the transition period. An example is a recent study52 of 97 UHR individuals and 50 controls, which reported a decrease in peripheral blood expression of combined NRG1 type I and II among those who transitioned to psychosis compared with those who did not transition and controls. Unfortunately, NRG1 genetic variation of these individuals was not reported, and the concordance between blood and brain NRG1 expression is not yet clear. Further work examining the effects of NRG1 genetic variation on peripheral expression of NRG1 is needed to determine whether peripheral blood may serve as an appropriate surrogate for the NRG1 genotype expression relationship in the brain.
Although the DAOA locus has been associated with schizophrenia in two meta-analyses53, 54 and has been shown to be upregulated in the dorsolateral prefrontal cortex of those with schizophrenia,55 we did not observe significant effects for any of the examined DAOA htSNPs or previously reported risk-conferring SNPs in our sample of newly transitioned individuals. This finding diverges from the only other study to examine the ability of DAOA genetic variation to predict transition to psychosis. In that study Mossner et al.29 reported 100% and 50% of UHR individuals carrying the rs1341402-CC and rs778294-AA transitioned to psychosis, respectively. In contrast, we observed a non-significant 37.5% of rs1341402-CC and 29.4% of rs778294-AA carriers transitioned to psychosis, despite a study sample size that was more than two times that used by Mossner et al.29 The conflicting results suggest the initial finding may have been a false-positive, the current finding is a false-negative, or sample heterogeneity between the two studies resulted in findings that are not comparable. Further examination of the link between DAOA genetic variation and psychosis transition among UHR individuals is required as the collective number of individuals examined to date (n=307) is not large enough for firm conclusions to be made.
In summary, our findings provide evidence supporting NRG1 genetic variation as a promising factor for differentiating UHR individuals who will or will not transition to psychosis. Current tools used for early identification of individuals at risk for transition, although standardized, are dependent on subjective measures (for example, clinical rating scales) that relative to genotyping are more susceptible to measurement errors and consequently reduced prediction accuracy. Our findings in combination with previous studies provide support for the addition of measures that are not dependent on state-related changes that have the potential to further improve upon current levels of risk prediction.9 However, we caution against the temptation to include NRG1 genetic variation in psychosis risk prediction until replication has been undertaken in much larger samples, and the true effect size of any replicated association can be more accurately determined.56, 57 Additional investigation may then determine which genetic markers, in what contexts, and at what costs will provide the most clinically useful genetically informed risk prediction among at-risk populations.
Acknowledgments
We thank HP Yuen for his assistance with data management. We also thank the young people who participated. DNA was provided by Genetic Repositories Australia, an Enabling Facility supported by NHMRC Grant number 401184, and samples were collected by Orygen Youth Health Research Centre, Centre for Youth Mental Health. This work was supported by Colonial Foundation (Australia) (PDM; ARY; DLF); National Health and Medical Research Council of Australia Project Grants and Program Grant (ARY, CP, PDM); John McKenzie Post-Doctoral Fellowship (CAB); NHMRC Senior Research Fellowship (ARY); NHMRC Senior Principal Research Fellowship (CP); Ronald Phillip Griffith Fellowship and NHMRC Career Development Fellowship (BN).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Translational Psychiatry website (http://www.nature.com/tp)
Supplementary Material
References
- Yung AR, Nelson B, Stanford C, Simmons MB, Cosgrave EM, Killackey E, et al. Validation of ‘prodromal' criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophr Res. 2008;105:10–17. doi: 10.1016/j.schres.2008.07.012. [DOI] [PubMed] [Google Scholar]
- Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39:964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, et al. Psychosis prediction: 12-month follow up of a high-risk (‘prodromal') group. Schizophr Res. 2003;60:21–32. doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res. 2004;67:131–142. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69:220–229. doi: 10.1001/archgenpsychiatry.2011.1472. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Bechdolf A, Taylor MJ, Bonoldi I, Carpenter WT, Yung AR, et al. At risk for schizophrenic or affective psychoses? a meta-analysis of DSM/ICD Diagnostic outcomes in individuals at high clinical risk Schizophrenia bulletin 2013(e-pub ahead of print). [DOI] [PMC free article] [PubMed]
- Cannon TD.Prediction of Psychosis Through the Prodromal SyndromeIn: Gattaz WF, Busatto G (eds).Advances in Schizophrenia Research Springer: New York; 2010. p251–266. [Google Scholar]
- Piskulic D, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry Res. 2012;196:220–224. doi: 10.1016/j.psychres.2012.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason O, Startup M, Halpin S, Schall U, Conrad A, Carr V. Risk factors for transition to first episode psychosis among individuals with ‘at-risk mental states'. Schizophr Res. 2004;71:227–237. doi: 10.1016/j.schres.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Velthorst E, Nieman DH, Becker HE, van de Fliert R, Dingemans PM, Klaassen R, et al. Baseline differences in clinical symptomatology between ultra high risk subjects with and without a transition to psychosis. Schizophr Res. 2009;109:60–65. doi: 10.1016/j.schres.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2010;67:241–251. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- Garner B, Pariante CM, Wood SJ, Velakoulis D, Phillips L, Soulsby B, et al. Pituitary volume predicts future transition to psychosis in individuals at ultra-high risk of developing psychosis. Biol Psychiatry. 2005;58:417–423. doi: 10.1016/j.biopsych.2005.04.018. [DOI] [PubMed] [Google Scholar]
- Takahashi T, Wood SJ, Yung AR, Phillips LJ, Soulsby B, McGorry PD, et al. Insular cortex gray matter changes in individuals at ultra-high-risk of developing psychosis. Schizophr Res. 2009;111:94–102. doi: 10.1016/j.schres.2009.03.024. [DOI] [PubMed] [Google Scholar]
- Fornito A, Yung AR, Wood SJ, Phillips LJ, Nelson B, Cotton S, et al. Anatomic abnormalities of the anterior cingulate cortex before psychosis onset: an MRI study of ultra-high-risk individuals. Biol Psychiatry. 2008;64:758–765. doi: 10.1016/j.biopsych.2008.05.032. [DOI] [PubMed] [Google Scholar]
- Walterfang M, Yung A, Wood AG, Reutens DC, Phillips L, Wood SJ, et al. Corpus callosum shape alterations in individuals prior to the onset of psychosis. Schizophr Res. 2008;103:1–10. doi: 10.1016/j.schres.2008.04.042. [DOI] [PubMed] [Google Scholar]
- Koutsouleris N, Meisenzahl EM, Davatzikos C, Bottlender R, Frodl T, Scheuerecker J, et al. Use of neuroanatomical pattern classification to identify subjects in at-risk mental states of psychosis and predict disease transition. Arch Gen Psychiatry. 2009;66:700–712. doi: 10.1001/archgenpsychiatry.2009.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer WJ, Wood SJ, McGorry PD, Francey SM, Phillips LJ, Yung AR, et al. Impairment of olfactory identification ability in individuals at ultra-high risk for psychosis who later develop schizophrenia. Am J Psychiatry. 2003;160:1790–1794. doi: 10.1176/appi.ajp.160.10.1790. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Deste G, Smieskova R, Barlati S, Yung AR, Howes O, et al. Cognitive functioning in prodromal psychosis: a meta-analysiscognitive functioning in prodromal psychosis. Arch Gen Psychiatry. 2012;69:562–571. doi: 10.1001/archgenpsychiatry.2011.1592. [DOI] [PubMed] [Google Scholar]
- Giuliano AJ, Li H, Mesholam-Gately RI, Sorenson SM, Woodberry KA, Seidman LJ. Neurocognition in the psychosis risk syndrome: a quantitative and qualitative review. Curr Pharm Des. 2012;18:399–415. doi: 10.2174/138161212799316019. [DOI] [PubMed] [Google Scholar]
- Strobl EV, Eack SM, Swaminathan V, Visweswaran S. Predicting the risk of psychosis onset: advances and prospects. Early Interv Psychia. 2012;6:368–379. doi: 10.1111/j.1751-7893.2012.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantelis C, Yucel M, Bora E, Fornito A, Testa R, Brewer WJ, et al. Neurobiological markers of illness onset in psychosis and schizophrenia: the search for a moving target. Neuropsychol Rev. 2009;19:385–398. doi: 10.1007/s11065-009-9114-1. [DOI] [PubMed] [Google Scholar]
- Allen NC, Bagade S, McQueen MB, Ioannidis JP, Kavvoura FK, Khoury MJ, et al. Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat Genet. 2008;40:827–834. doi: 10.1038/ng.171. [DOI] [PubMed] [Google Scholar]
- Hall J, Whalley HC, Job DE, Baig BJ, McIntosh AM, Evans KL, et al. A neuregulin 1 variant associated with abnormal cortical function and psychotic symptoms. Nat Neurosci. 2006;9:1477–1478. doi: 10.1038/nn1795. [DOI] [PubMed] [Google Scholar]
- Keri S, Kiss I, Kelemen O. Effects of a neuregulin 1 variant on conversion to schizophrenia and schizophreniform disorder in people at high risk for psychosis. Mol Psychiatry. 2009;14:118–119. doi: 10.1038/mp.2008.1. [DOI] [PubMed] [Google Scholar]
- Stefansson H, Sigurdsson E, Steinthorsdottir V, Bjornsdottir S, Sigmundsson T, Ghosh S, et al. Neuregulin 1 and susceptibility to schizophrenia. Am J Hum Genet. 2002;71:877–892. doi: 10.1086/342734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossner R, Schuhmacher A, Wagner M, Quednow BB, Frommann I, Kuhn KU, et al. DAOA/G72 predicts the progression of prodromal syndromes to first episode psychosis. Eur Arch Psychiatry Clin Neurosci. 2010;260:209–215. doi: 10.1007/s00406-009-0044-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zintzaras E. Impact of Hardy-Weinberg equilibrium deviation on allele-based risk effect of genetic association studies and meta-analysis. Eur J Epidemiol. 2010;25:553–560. doi: 10.1007/s10654-010-9467-z. [DOI] [PubMed] [Google Scholar]
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- Andreasen NC, Flaum M, Arndt S. The Comprehensive Assessment of Symptoms and History (CASH). An instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry. 1992;49:615–623. doi: 10.1001/archpsyc.1992.01820080023004. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39:789–794. doi: 10.1001/archpsyc.1982.04290070025006. [DOI] [PubMed] [Google Scholar]
- Heinrichs DW, Hanlon TE, Carpenter WT., Jr The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10:388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association Diagnostic criteria from DSM-IV Washington, D.C.: The Association 1994. p358
- de Bakker PI, Yelensky R, Pe'er I, Gabriel SB, Daly MJ, Altshuler D. Efficiency and power in genetic association studies. Nat Genet. 2005;37:1217–1223. doi: 10.1038/ng1669. [DOI] [PubMed] [Google Scholar]
- Chumakov I, Blumenfeld M, Guerassimenko O, Cavarec L, Palicio M, Abderrahim H, et al. Genetic and physiological data implicating the new human gene G72 and the gene for D-amino acid oxidase in schizophrenia. Proc Natl Acad Sci USA. 2002;99:13675–13680. doi: 10.1073/pnas.182412499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enoch MA, Shen PH, Xu K, Hodgkinson C, Goldman D. Using ancestry-informative markers to define populations and detect population stratification. J Psychopharmacol. 2006;20:19–26. doi: 10.1177/1359786806066041. [DOI] [PubMed] [Google Scholar]
- Gaunt TR, Rodriguez S, Day IN. Cubic exact solutions for the estimation of pairwise haplotype frequencies: implications for linkage disequilibrium analyses and a web tool 'CubeX'. BMC Bioinform. 2007;8:428. doi: 10.1186/1471-2105-8-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong YG, Wu CN, Xing QH, Zhao XZ, Zhu J, He L. A two-method meta-analysis of Neuregulin 1(NRG1) association and heterogeneity in schizophrenia. Schizophr Res. 2009;111:109–114. doi: 10.1016/j.schres.2009.03.017. [DOI] [PubMed] [Google Scholar]
- Li D, Collier DA, He L. Meta-analysis shows strong positive association of the neuregulin 1 (NRG1) gene with schizophrenia. Hum Mol Genet. 2006;15:1995–2002. doi: 10.1093/hmg/ddl122. [DOI] [PubMed] [Google Scholar]
- Munafo MR, Attwood AS, Flint J. Neuregulin 1 genotype and schizophrenia. Schizophr Bull. 2008;34:9–12. doi: 10.1093/schbul/sbm129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafo MR, Thiselton DL, Clark TG, Flint J. Association of the NRG1 gene and schizophrenia: a meta-analysis. Mol Psychiatry. 2006;11:539–546. doi: 10.1038/sj.mp.4001817. [DOI] [PubMed] [Google Scholar]
- Weickert CS, Tiwari Y, Schofield PR, Mowry BJ, Fullerton JM. Schizophrenia-associated HapICE haplotype is associated with increased NRG1 type III expression and high nucleotide diversity. Transl Psychiatry. 2012;2:e104. doi: 10.1038/tp.2012.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law AJ, Lipska BK, Weickert CS, Hyde TM, Straub RE, Hashimoto R, et al. Neuregulin 1 transcripts are differentially expressed in schizophrenia and regulated by 5′ SNPs associated with the disease. Proc Nl Acad SciUSA. 2006;103:6747–6752. doi: 10.1073/pnas.0602002103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Bates R, Yin DM, Shen C, Wang F, Su N, et al. Specific regulation of NRG1 isoform expression by neuronal activity. J Neurosc. 2011;31:8491–8501. doi: 10.1523/JNEUROSCI.5317-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy K, Murtie JC, El-Khodor BF, Edgar N, Sardi SP, Hooks BM, et al. Loss of erbB signaling in oligodendrocytes alters myelin and dopaminergic function, a potential mechanism for neuropsychiatric disorders. Proc Natl Acad Sci USA. 2007;104:8131–8136. doi: 10.1073/pnas.0702157104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YJ, Johnson MA, Lieberman MD, Goodchild RE, Schobel S, Lewandowski N, et al. Type III neuregulin-1 is required for normal sensorimotor gating, memory-related behaviors, and corticostriatal circuit components. J Neurosci. 2008;28:6872–6883. doi: 10.1523/JNEUROSCI.1815-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchionni MA, Goodearl AD, Chen MS, Bermingham-McDonogh O, Kirk C, Hendricks M, et al. Glial growth factors are alternatively spliced erbB2 ligands expressed in the nervous system. Nature. 1993;362:312–318. doi: 10.1038/362312a0. [DOI] [PubMed] [Google Scholar]
- Trachtenberg JT, Thompson WJ. Schwann cell apoptosis at developing neuromuscular junctions is regulated by glial growth factor. Nature. 1996;379:174–177. doi: 10.1038/379174a0. [DOI] [PubMed] [Google Scholar]
- Zhang L, Fletcher-Turner A, Marchionni MA, Apparsundaram S, Lundgren KH, Yurek DM, et al. Neurotrophic and neuroprotective effects of the neuregulin glial growth factor-2 on dopaminergic neurons in rat primary midbrain cultures. J Neurochem. 2004;91:1358–1368. doi: 10.1111/j.1471-4159.2004.02817.x. [DOI] [PubMed] [Google Scholar]
- Kiss I, Kelemen O, Keri S. Decreased peripheral expression of neuregulin 1 in high-risk individuals who later converted to psychosis. Schizophr Res. 2012;135:198–199. doi: 10.1016/j.schres.2011.12.012. [DOI] [PubMed] [Google Scholar]
- Detera-Wadleigh SD, McMahon FJ. G72/G30 in schizophrenia and bipolar disorder: review and meta-analysis. Biol Psychiatry. 2006;60:106–114. doi: 10.1016/j.biopsych.2006.01.019. [DOI] [PubMed] [Google Scholar]
- Shi J, Badner JA, Gershon ES, Liu C. Allelic association of G72/G30 with schizophrenia and bipolar disorder: a comprehensive meta-analysis. Schizophr Res. 2008;98:89–97. doi: 10.1016/j.schres.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korostishevsky M, Kaganovich M, Cholostoy A, Ashkenazi M, Ratner Y, Dahary D, et al. Is the G72/G30 locus associated with schizophrenia? single nucleotide polymorphisms, haplotypes, and gene expression analysis. Biol Psychiatry. 2004;56:169–176. doi: 10.1016/j.biopsych.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Ioannidis JP, Ntzani EE, Trikalinos TA, Contopoulos-Ioannidis DG. Replication validity of genetic association studies. Nat Genet. 2001;29:306–309. doi: 10.1038/ng749. [DOI] [PubMed] [Google Scholar]
- Ioannidis JP, Trikalinos TA, Ntzani EE, Contopoulos-Ioannidis DG. Genetic associations in large versus small studies: an empirical assessment. Lancet. 2003;361:567–571. doi: 10.1016/S0140-6736(03)12516-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.