Abstract
Objective
To assess the mediation of smoking-associated postoperative mortality by postoperative complications.
Design
Observational cohort study.
Setting
Using data from the Veterans Affairs (VA) Surgical Quality Improvement Programme, a quality assurance programme for major surgical procedures in the VA healthcare system, we assessed the association of current smoking at the time of the surgery with 6-month and 1-year mortality.
Primary and secondary outcome measures
Using mediation analyses, we calculated the relative contribution of each smoking-associated complication to smoking-associated postoperative mortality, both unadjusted and adjusted for age, race/ethnicity, work relative value unit of the operation, surgeon specialty, American Society of Anesthesiologists class and year of surgery. Smoking-associated complications included surgical site infection (SSI), cardiovascular complications (myocardial infarction, cardiac arrest and/or stroke) and pulmonary complications (pneumonia, failure to wean and/or reintubation).
Results
There were 186 632 never smokers and 135 741 current smokers. The association of smoking and mortality was mediated by smoking-related complications with varying effects. In unadjusted analyses, the proportions of mediation of smoking to 6-month mortality explained by the complications were as follows: SSIs 22%, cardiovascular complications 12% and pulmonary complications 89%. In adjusted analyses, the per cents mediated by each complication were as follows: SSIs 2%, cardiovascular complications 4% and pulmonary complications 22%. In adjusted analyses for 1-year mortality, respective per cents mediated were 2%, 3% and 16%.
Conclusions
Pulmonary complications, followed by cardiovascular complications and SSIs were mediators of smoking-associated 6-month and 1-year mortality. Interventions targeting smoking cessation and prevention and early treatment of pulmonary complications has the likelihood of reducing postoperative mortality after elective surgery.
Keywords: Epidemiology
Article summary.
Article focus
We aimed to examine whether smoking-associated postoperative mortality is mediated through smoking-associated postoperative complications in patients who were current smokers at the time of their surgery.
We hypothesised that specific smoking-associated complications (surgical site infections (SSIs), pulmonary and cardiovascular) in the postoperative period in current smokers, mediate smoking-related 6-month and 1-year mortality.
Key messages
Pulmonary complications, followed by cardiovascular complications and SSIs were mediators of smoking-associated 6-month and 1-year mortality after elective knee or hip replacement surgery.
Preoperative smoking counselling and implementation of smoking cessation programmes should be performed prior to an elective surgery such as knee/hip replacement.
Early treatment of complications that mediate postoperative 1-year mortality may help reduce risk of dying after an elective surgery.
Strengths and limitations of this study
Use of prospectively collected national data in the largest integrated healthcare system in the USA.
Outcomes and complications had been defined using standardised definitions and validated by nurse abstractors.
Findings may not be generalisable to women and non-veteran US population, since our sample included primarily men, representative of US veterans.
The current smoker variable is collected retrospectively from medical records, which could lead to misclassification bias and underestimation of the association.
Smoking status may change over time and the current study could not take that into account, since ongoing smoking status data are not available.
Mediation assumes no unmeasured variables and despite accounting for all the important variables to the best of our capability with the given data, residual confounding is possible.
Introduction
Smoking is the leading cause of preventable death in the USA.1 2 While the prevalence of smoking in the USA has decreased,3 smoking is still highly prevalent with a recent national survey showing between 10% and 26% prevalence in most of the US states.4 The prevalence of smoking in veterans using Veterans Affairs (VA) healthcare is even higher, at 30%.5 Smoking has detrimental effects on cardiovascular and lung health, and is linked to increased risk of surgical complications. Specifically, smokers undergoing surgery have a higher risk of several postoperative complications including wound infections, pneumonia and mortality.6 7 Smoking is a modifiable risk factor.8–10 Preoperative smoking cessation is associated with decreased postoperative wound complications and total complications.11
While smoking-related postoperative morbidity is important, smoking is also associated with increased postoperative mortality.12–14 There are several proposed mechanisms of increased mortality in the perioperative period for smokers including higher risk of cardiac13 14 and pulmonary complications.12 To our knowledge, no previous studies have assessed to what degree the increased smoking-associated postoperative mortality is mediated by specific complications associated with smoking. This has important consequences for designing interventions to improve outcomes. If the effect of smoking on mortality were direct (direct toxic effects on health, low likelihood), then the only effective method to improve smoking-related outcomes would be smoking cessation. Alternatively, to the extent that smoking is related to mortality through an increase in pulmonary complications among smokers, the effect of smoking is said to act through the mediating factor of pulmonary complications. Such a result would suggest that interventions to reduce pulmonary complications among smokers may be an additional strategy for improving the mortality outcome.
We have recently demonstrated that smoking was associated with both postoperative surgical site infections (SSIs) and pulmonary complications in a large cohort of veterans who underwent surgery in VA medical facilities and that mortality was also increased in this cohort.15 These data are collected prospectively and systematically as part of the National VA Surgical Quality Improvement Program (VASQIP).16 17
In this study, we aimed to examine whether smoking-associated postoperative mortality is mediated through smoking-associated postoperative complications in patients who are current smokers at the time of their surgery. Conceptually, ‘mediation’ occurs when a cause and its effects are linked through an intervening factor that is part of the causal chain of events.18 As an example, this study explored the link between smoking and postoperative morbidity and mortality. We hypothesised that specific smoking-associated complications (SSI, pulmonary and cardiovascular) in the postoperative period in current smokers, mediate smoking-related 6-month and 1-year mortality. This was performed in two steps: we first established a link between smoking and adverse outcomes, and we then investigated and quantified the proportion of the observed association appearing to act through a particular and plausible mediator, in this case, smoking-associated complications.
Methods
Ethical approval, study funding and data sharing
The study was approved by the Institutional Review Boards at the VA Medical Centers (Birmingham, Alabama, Bedford, Massachusetts, Boston, Massachusetts and Seattle, Washington), the University of Colorado and by the Surgical Quality Data Use Group of VA Patient Care Services in VA Central Office, Washington DC (as needed for studies using data from this dataset). All analyses used SAS V.9.2 (SAS Institute Inc, Cary, North Carolina). This material is the result of work supported with VA Investigator-Initiated Research (IIR) IAB 06-038-2. Additionally, Dr Singh's time was protected by research grants from the National Institute of Aging, National Cancer Institute and Agency for Health Quality and Research Center for Education and Research on Therapeutics (CERTs). The study authors are committed to sharing the data with colleagues after an ethics committee approval and in accordance with VA data privacy and data security rules.
Study sample
We used data from the VASQIP, a system-wide initiative instituted in 1994 to improve the quality of surgical care through prospective collection and reporting of comparative risk-adjusted postoperative outcomes of major surgeries requiring general, spinal or epidural anesthesia.19 The abstracted data are >99% complete with >96% interobserver agreement.17 We requested all cases in major procedure groups defined by common procedural terminology codes within each of the eight surgical subspecialties (general, vascular, orthopaedic, thoracic, otolaryngology, urology, neurosurgery and plastic surgery) for the years 2002–2008. This produced a sample of roughly 60–70% of all non-cardiac operations in the VASQIP database for those years (n=507 545). We selected the first operation for each patient greater than or equal to 19 years of age, resulting in 412 511 unique patients. We excluded 17 202 patients coded as having emergency operations, since we wanted to focus on elective surgeries. We also excluded 1 515 patients who were coded as a current smoker but who had 0 pack-years (an inconsistency) or were missing the current smoker variable. Since our focus was current smoking, we excluded 71 421 prior smokers leaving a total of 322 373 patients for analysis.
Independent measure: current smoking
Smoking status was assessed using two variables. Patients are queried at the time of elective surgery if they have smoked cigarettes in the year prior to admission (yes/no) and regarding amount of smoking (pack-years=the number of packs smoked per day multiplied by the number of years the patient smoked), documented in patients' medical records. Never smokers were patients who had no smoking in the prior year and zero (or missing) pack-years. Current smokers were those who responded ‘yes’ to smoking in the year prior to admission and had pack-years not equal to zero.
Dependent measure: mortality
Mortality was assessed at 6 months and at 1 year. The VASQIP nurses have collected a 30-day postoperative vital status for all the patients assessed in the VASQIP program. Once every 6 months, the VASQIP database is passed through the VA administrative vitals file to obtain data on long-term postoperative mortality beyond 30 days after surgery.
Mediation variables: 30-day outcomes for complications
All complications of interest were assessed 30 days after elective surgery. Specifically, the outcomes included: (1) SSIs; (2) cardiovascular complications, defined as occurrence of myocardial infarction, cardiac arrest and/or stroke; (3) pulmonary complications, defined as occurrence of pneumonia, failure to wean and/or reintubation and (4) overall composite outcome, defined as the occurrence of SSI, cardiovascular and/or pulmonary complications. All outcomes have standard definitions in VASQIP and are extracted and validated for each patient by an independent nurse abstractor at each VA site for the 30-day period after the surgery.16 17
Covariates: patient, surgeon and procedural characteristics
Patient characteristics including age, race/ethnicity, American Society of Anesthesiologists (ASA) class, year of surgery, work relative value unit (RVU) for the operation and wound classification were extracted. ASA class is a validated measure of perioperative mortality and immediate postoperative morbidity, categorised into five classifications20 21 (class I, normal healthy patient; class II, patient with mild systemic disease (with no functional limitation); class III, patient with severe systemic disease (with some functional limitation); class IV, patient with severe systemic disease that is a constant threat to life; class V, moribund patient). Work RVU (a measure of procedure duration and complexity) and surgeon subspecialty were collected by chart review. These variables were chosen based on previous literature of association of these factors with mortality or because they represented the complexity of the surgery.
Statistical analyses
Summary statistics were calculated for clinical and demographic characteristics. Mediation analysis was performed with and without controlling for covariates that could potentially confound the relationship. Univariable and multivariable-adjusted logistic regression analyses were used to compute coefficients for association of smoking and mortality, smoking and major complications (SSI, pulmonary, cardiovascular or composite) and major complications and mortality, to assess mediation effect of complications on the relationship between smoking and mortality. In multivariable analyses, we adjusted for age, race/ethnicity, work RVU, surgeon specialty, ASA class and year at each step of the mediation analysis. Wound classification was additionally adjusted for in the model when assessing the mediation effect of SSI.
The conceptual framework of ‘mediation’ indicates that mediation occurs when a cause and its effect are linked through an intervening factor that is part of the causal chain of events.18 The classic exposition of statistical mediation analysis was given by Baron and Kenny.18 The mediating relationship was conceived in causal terms, so while it was recognised that the statistical models cannot establish causality, the causal interpretation of the posited relationships must be plausible. The precondition was that the independent variable (smoking) is statistically significantly associated with the dependent variable (eg, 6-month mortality). The total effect of smoking on mortality was denoted by the path ‘c’ in figure 1 representing the association of smoking on mortality without adjustment for the potential mediator. Baron and Kenny outlined three steps for a formal mediation analysis using regression, which can be explained with reference to figure 1 in the context of the relationship between smoking and 6-month mortality with the putative mediating effect of pulmonary complications. The first step was to establish that there is a significant association between the independent variable (smoking) and the potential mediator (pulmonary complications) corresponding to the path coefficient ‘a’ in figure 1. The second step was to establish that the potential mediator (pulmonary complications) is associated with the dependent variable (6-month mortality), while controlling for the independent variable (smoking), corresponding to the path coefficient ‘b’. Last, when controlling for the mediator (pulmonary complications) the ‘direct effect’ of the independent variable (smoking) on the dependent variable (6-month mortality) corresponds to the coefficient ‘c′’. We interpret the ‘direct effect’ to be the ‘lifetime exposure’ of smoking. Less technically, if (1) smoking was related to both pulmonary complications and mortality, (2) pulmonary complications were related to mortality and (3) the magnitude of the relationship between smoking and mortality decreased by a statistically significant amount when controlling for pulmonary complications, then there was a significant amount of mediation by pulmonary complications.
Figure 1.
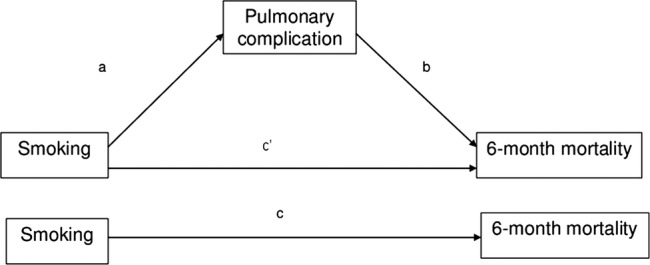
Path diagram of the relations among the three standardised variables and standardised coefficients of paths. a=regression coefficient for path from smoking to pulmonary complications; b=regression coefficient for path from pulmonary complications to 6-month mortality, controlling for smoking; c′=regression coefficient for path from smoking to 6-month mortality, controlling for pulmonary complications; c=regression coefficient for direct path from smoking to 6-month mortality. Smoking is the independent variable, pulmonary complications the mediator and 6-month mortality dependent variable. a, b, c and c′ are coefficients from logistic regression analyses.
Arithmetically, the indirect effect is equal to the product of coefficients a×b while the total effect (c) is equal to the indirect effect (a×b) plus the remaining direct effect (c′), thus: c=a×b+c′, so c′=c−a×b. Clearly, as the indirect effect through the mediator gets larger, the residual direct effect must decrease, implying that a larger part of the effect is via the mediator. The more the direct effect is diminished, the greater part of the effect is mediated.
The statistical significance of the mediated, or indirect, effect was determined by testing whether the product a×b is statistically different from zero. The standard approximate test was due to the work of Sobel, and presented by Baron and Kenny.18 Subsequent work, notably by Shrout and Bolger22 note that the Sobel test can be overly conservative for small samples but also that this ceases to be a concern when the sample size is greater than 1 000. The much larger sample size of this study suggested that the Sobel test was adequate in this context.
To evaluate the importance of the mediation it can be informative to calculate the proportion of the effect owing to mediation as the indirect effect divided by the total effect as a×b/c. In our work, the independent, dependent and mediator variable were all dichotomous. In this context where logistic regression is used a×b+c′ may only approximate c, so we followed the methods of MacKinnon and Dwyer23 and calculated the proportion of the effect owing to mediation using coefficients standardised to the same scale. We present only the unstandardised coefficients because they are more interpretable within the context of the individual regression models.
Results
There were 186 632 never smokers and 135 741 current smokers. The mean age was 63 years for never smokers and 58 years for current smokers. In total, 95% were men and 63% were Whites (race/ethnicity missing in 19%; table 1). Diabetes was less common among current smokers compared with never smokers, but chronic obstructive pulmonary disease (COPD), dyspnoea and alcohol consumption were more common. Other characteristics were similar between the two groups (table 1). Crude estimates of outcomes by smoking status are shown in table 2.
Table 1.
Patient characteristics by smoking status* (column per cents unless noted otherwise)
| Characteristic | Never smoked (n=186 632) | Current smoker (n=135 741) |
|---|---|---|
| Smoking pack-years, mean (SD) | N/A | 48.8 (32.6) |
| Demographics | ||
| Age, mean (SD) | 63.1 (13.7) | 57.6 (11.0) |
| Sex (%) | ||
| Female | 5.1 | 4.1 |
| Male | 94.9 | 95.9 |
| Race/ethnicity (%) | ||
| White | 62.3 | 63.1 |
| Black | 12.3 | 14.9 |
| Hispanic | 5.3 | 2.7 |
| Other/unknown | 20.2 | 19.3 |
| Comorbidities (%) | ||
| Diabetes | 20.2 | 14.6 |
| Congestive heart failure | 1.2 | 1.0 |
| History of severe COPD | 7.0 | 18.4 |
| Dyspnoea | 8.4 | 15.4 |
| Chronic corticosteroid use | 1.7 | 1.7 |
| Renal failure/dialysis | 0.7 | 0.5 |
| CVA/stroke | 5.9 | 6.6 |
| Transient ischaemic attacks | 2.9 | 3.6 |
| Functional health status (%) | ||
| Independent | 93.5 | 94.8 |
| Partially dependent | 5.2 | 4.6 |
| Totally dependent | 1.3 | 0.6 |
| >10% loss body weight in past 6 months | 1.8 | 3.4 |
| Disseminated cancer | 1.0 | 1.3 |
| Open wound/wound infection | 3.2 | 4.3 |
| DNR status | 0.9 | 0.6 |
| Alcohol >2 drinks/day | 4.3 | 14.6 |
| Operative characteristics | ||
| Anaesthesia technique (%) | ||
| General | 79.4 | 84.8 |
| Epidural/spinal | 15.6 | 10.9 |
| Local/monitored | 5.1 | 4.2 |
| ASA classification (%) | ||
| 1 | 4.4 | 1.6 |
| 2 | 35.8 | 33.4 |
| 3 | 53.8 | 58.2 |
| 4/5 | 6.1 | 6.8 |
| Admission status (%) | ||
| Outpatient | 51.0 | 47.1 |
| Inpatient | 49.0 | 52.9 |
| Specialty of surgeon (%) | ||
| General surgery | 39.3 | 35.3 |
| Neurosurgery | 5.4 | 7.9 |
| Orthopaedic surgery | 29.6 | 21.9 |
| Otolaryngology | 1.1 | 1.3 |
| Plastic surgery | 0.6 | 0.6 |
| Thoracic surgery | 1.7 | 5.6 |
| Urology | 15.6 | 13.1 |
| Cardiovascular surgery | 6.3 | 13.8 |
| Other | 0.4 | 0.4 |
| Wound classification (%) | ||
| Clean | 70.0 | 70.8 |
| Clean/contaminated | 27.3 | 26.2 |
| Contaminated | 1.6 | 1.6 |
| Infected | 1.2 | 1.4 |
| Work RVU (mean, SD) | 14.1 (7.1) | 14.8 (7.8) |
| Operation time, hours (mean, SD) | 1.9 (1.4) | 2.1 (1.6) |
*All p value are <0.001 with the exception of steroid use, for which was 0.581.
ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; DNR, Do not resuscitate; N/A, not applicable; RUV, relative value units.
Table 2.
Frequency of outcomes by smoking status
| Postoperative outcome | Never smoked (n=186632) | Current smoker (n=135741) |
|---|---|---|
| Surgical site infection | 2.4 | 3.4 |
| Vascular complications | 0.5 | 0.5 |
| Cerebral vascular accident/stroke | 0.2 | 0.3 |
| Myocardial infarction | 0.3 | 0.3 |
| Pulmonary complications | 2.0 | 3.1 |
| Reintubation for respiratory or cardiac failure | 0.9 | 1.6 |
| Pneumonia | 1.2 | 1.9 |
| Failure to wean >48 h | 0.8 | 1.4 |
| Composite outcome | 4.5 | 6.5 |
| Death within 6 months* | 3.5 | 3.9 |
| Death within 1 year* | 5.3 | 6.4 |
Results presented as column percentage.
*Never, N=186305; current, N=135561.
Mediation analyses for 6-month and 1-year mortality
Unstandardised coefficients were calculated without (unadjusted; table 3) and with (adjusted; table 4) potential confounders using regression analyses. Variances for computing standardised coefficients are footnoted. The unadjusted coefficients were highest between smoking and pulmonary complications (coefficient a=0.46), and between pulmonary complications and 6-month mortality, controlling for smoking was (coefficient b=2.90) among all complications (table 3); similar observations were made for pulmonary complications and 1-year mortality. In general, unadjusted coefficients were higher than adjusted coefficients.
Table 3.
Unadjusted coefficients* and their 95% CIs
| Outcome | Mediator | c | 95% CI | a | 95% CI | b | 95% CI | c′ | 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| 6 months mortality† | SSIs | 0.12 | 0.08 to 0.15 | 0.37 | 0.33 to 0.41 | 0.89 | 0.81 to 0.96 | 0.10 | 0.07 to 0.14 |
| Cardiovascular complications | 0.12 | 0.08 to 0.15 | 0.15 | 0.05 to 0.24 | 2.70 | 2.60 to 2.80 | 0.11 | 0.07 to 0.15 | |
| Pulmonary complications | 0.12 | 0.08 to 0.15 | 0.46 | 0.42 to 0.51 | 2.90 | 2.85 to 2.95 | 0.01 | −0.02 to 0.05 | |
| Composite outcome | 0.12 | 0.08 to 0.15 | 0.39 | 0.36 to 0.42 | 2.21 | 2.17 to 2.25 | 0.02 | −0.02 to 0.05 | |
| 1 year mortality‡ | SSIs | 0.20 | 0.17 to 0.23 | 0.37 | 0.33 to 0.41 | 0.83 | 0.76 to 0.89 | 0.19 | 0.16 to 0.22 |
| Cardiovascular complications | 0.20 | 0.17 to 0.23 | 0.15 | 0.05 to 0.24 | 2.42 | 2.32 to 2.52 | 0.20 | 0.17 to 0.23 | |
| Pulmonary complications | 0.20 | 0.17 to 0.23 | 0.46 | 0.42 to 0.51 | 2.60 | 2.57 to 2.64 | 0.13 | 0.10 to 0.17 | |
| Composite outcome | 0.20 | 0.17 to 0.23 | 0.39 | 0.36 to 0.42 | 1.91 | 1.88 to 1.95 | 0.13 | 0.10 to 0.16 |
c=direct path from smoking to mortality.
a=path from smoking to complications (SSI, cardiovascular, pulmonary or composite).
b=path from complications (SSI, etc) to mortality controlling for smoking.
c′=path from smoking to mortality controlling for complications (SSI, etc).
*All coefficients were unstandardised and rounded off to two digits after the decimal.
†Variances used to compute standardised coefficients22: var (smoking)=0.975, var (mortality)=0.036, var (predicted mortality|smoking′)=3.30, var (SSI)=0.028, var (predicted SSI|smoking’)=3.42, var (predicted mortality|smoking and SSI″)=3.32, var (cardiovascular)=0.005, var (predicted cardiovascular|smoking′)=3.31, var (predicted mortality|smoking and cardiovascular″)=3.34, var (pulmonary)=0.024, var (predicted pulmonary|smoking′)=3.50, var (predicted mortality|smoking and pulmonary″)=3.49, var (composite)=0.051, var (predicted composite|smoking′)=3.44, var (predicted mortality|smoking and composite″)=3.54.
‡Variances used to compute standardised coefficients22: var (smoking)=0.975, var (mortality)=0.054, var (predicted mortality|smoking′)=3.33, var (SSI)=0.028, var (predicted SSI|smoking′)=3.42, var (predicted mortality|smoking and SSI″)=3.34, var (cardiovascular)=0.005, var (predicted cardiovascular|smoking′)=3.31, var (predicted mortality|smoking and cardiovascular″)=3.36, var (pulmonary)=0.024, var (predicted pulmonary|smoking′)=3.50, var (predicted mortality|smoking and pulmonary″)=3.47, var (composite)=0.051, var (predicted composite|smoking′)=3.44, var (predicted mortality|smoking and composite″)=3.49.
SSIs, surgical site infections; var, variance.
Table 4.
Adjusted coefficients* and their 95% CIs controlling for confounding
| Outcome | Mediator | c | 95% CI | a | 95% CI | b | 95% CI | c′ | 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| 6 months mortality† | SSIs | 0.39 | 0.35 to 0.44 | 0.19 | 0.14 to 0.24 | 0.45 | 0.37 to 0.53 | 0.39 | 0.35 to 0.43 |
| Cardiovascular complications | 0.38 | 0.34 to 0.42 | 0.19 | 0.08 to 0.30 | 2.00 | 1.89 to 2.12 | 0.38 | 0.34 to 0.42 | |
| Pulmonary complications | 0.38 | 0.34 to 0.42 | 0.48 | 0.43 to 0.54 | 2.17 | 2.11 to 2.23 | 0.32 | 0.27 to 0.36 | |
| Composite outcome | 0.38 | 0.34 to 0.42 | 0.29 | 0.25 to 0.32 | 1.71 | 1.66 to 1.76 | 0.33 | 0.28 to 0.37 | |
| 1 year mortality‡ | SSIs | 0.45 | 0.42 to 0.49 | 0.19 | 0.14 to 0.24 | 0.44 | 0.37 to 0.51 | 0.45 | 0.41 to 0.48 |
| Cardiovascular complications | 0.44 | 0.40 to 0.47 | 0.19 | 0.08 to 0.30 | 1.77 | 1.66 to 1.88 | 0.44 | 0.40 to 0.47 | |
| Pulmonary complications | 0.44 | 0.40 to 0.47 | 0.48 | 0.43 to 0.54 | 1.90 | 1.85 to 1.96 | 0.39 | 0.36 to 0.43 | |
| Composite outcome | 0.44 | 0.40 to 0.47 | 0.29 | 0.25 to 0.32 | 1.44 | 1.40 to 1.48 | 0.40 | 0.36 to 0.44 |
c=direct path from smoking to mortality controlling for age, race/ethnicity, work RVU, surgeon specialty, ASA class and year.
a=path from smoking to complications (SSI, cardiovascular, pulmonary or composite) controlling for age, race/ethnicity, work RVU, surgeon specialty, ASA class and year.
b=path from complications (SSI, etc) to mortality controlling for smoking, age, race/ethnicity, work RVU, surgeon specialty, ASA class and year.
c′=path from smoking to mortality controlling for complications (SSI, etc), age, race/ethnicity, work RVU, surgeon specialty, ASA class and year.
*All coefficients were unstandardised and were rounded off to two digits after the decimal.
†Variances used to compute standardised coefficients22: var (smoking)=0.975, var (mortality)=0.036, var (predicted mortality|smoking [SSI)′)=3.44, var (predicted mortality|smoking (cardiovascular, pulmonary and composite)′)=3.43, var (SSI)=0.028, var (predicted SSI|smoking′)=3.32, var (predicted mortality|smoking and SSI″)=3.44, var (cardiovascular)=0.005, var (predicted cardiovascular|smoking′)=3.33, var (predicted mortality|smoking and cardiovascular″)=3.45, var (pulmonary)=0.024, var (predicted pulmonary|smoking′)=3.52, var (predicted mortality|smoking and pulmonary″)=3.49, var (composite)=0.051, var (predicted composite|smoking′)=3.37, var (predicted mortality|smoking and composite″)=3.53.
‡Variances used to compute standardised coefficients22: var (smoking)=0.975, var (mortality)=0.054, var (predicted mortality|smoking (SSI)′)=3.49, var (predicted mortality|smoking (Cardiovascular, pulmonary and Composite)′)=3.48, var (SSI)=0.028, var (predicted SSI|smoking′)=3.32, var (predicted mortality|smoking and SSI″)=3.49, var (cardiovascular)=0.005, var (predicted cardiovascular|smoking′)=3.33, var (predicted mortality|smoking and cardiovascular″)=3.49, var (pulmonary)=0.024, var (predicted pulmonary|smoking′)=3.52, var (predicted mortality|smoking and pulmonary″)=3.52, var (composite)=0.051, var (predicted composite|smoking′)=3.37, var (predicted mortality|smoking and composite″)=3.54.
ASA, American Society of Anesthesiologists; RVU, relative value unit; SSIs, surgical site infections; var, variance.
Table 4 provides coefficients for the mediation analyses controlling for confounding from age, race/ethnicity, work RVU, surgeon specialty, ASA class and year for 6-month and 1-year mortality. Mediation analysis for SSI additionally controlled for wound classification. The coefficients for the path from smoking to 6-month and 12-month mortality while considering the mediation factor of SSI were 0.39 and 0.45 (coefficient c). Again, as an example, the coefficient between smoking and pulmonary complications was 0.48 (coefficient a), between pulmonary complications and 6-month mortality controlling for smoking was 2.17 (coefficient b), and that between smoking and 6-month mortality controlling for pulmonary complications was 0.32 (coefficient c′). The association between smoking and 6-month mortality was significantly mediated by pulmonary complications (22%; table 5). For 6-month mortality, adjusted coefficients between smoking and complications were highest for pulmonary complications (0.48), followed by composite outcome (0.29), SSI (0.19) and cardiovascular complications (0.19; coefficient a). Adjusted coefficients were highest for pulmonary followed by cardiovascular, composite and SSI complications for association with 6-month mortality, controlling for smoking (coefficient b). The proportion of mediation of smoking to 6-month mortality explained by the complications in adjusted analyses was 16% for the composite outcome, while the proportions were lower for SSI (2%) and cardiovascular complications (4%; table 5).
Table 5.
Proportion of mediation of smoking to mortality association explained by each complication in unadjusted and adjusted models
| Outcome | Mediator | Proportion mediation unadjusted for covariates (%) | Proportion mediation adjusted for covariates (%) |
|---|---|---|---|
| 6 months mortality | Surgical site infection | 22.2 | 2.0 |
| Cardiovascular complications | 12.2 | 3.8 | |
| Pulmonary complications | 88.9 | 21.6 | |
| Composite outcome | 86.4 | 15.7 | |
| 1 year mortality | Surgical site infection | 12.6 | 1.7 |
| Cardiovascular complications | 6.5 | 3.0 | |
| Pulmonary complications | 42.7 | 16.2 | |
| Composite outcome | 40.8 | 11.3 |
Because the proportion mediated is ratio statistic, its estimated value is sensitive to variation in point estimates of the regression coefficients from which it is derived; it should therefore be interpreted with caution. Coefficient values (magnitude and significance) should be the main proponent in assessing mediation.
Similar patterns were noted for mediation of smoking and 1-year mortality for adjusted coefficients (table 4). In the adjusted models, the proportion of mediation of smoking to 1-year mortality explained by the complications in adjusted analyses was 16% for pulmonary complications, 11% for composite complications, 3% for cardiovascular complications and 2% for SSI (table 5).
Discussion
In this analysis of prospectively collected data in a national sample of non-cardiac elective surgeries at VA facilities, we found that increased 6-month and 1-year smoking-associated mortalities were mediated by pulmonary complications and to a lesser extent cardiovascular complications and SSIs. Not unexpectedly, estimates of the proportion of smoking-related mortality mediated by each perioperative complications were all numerically larger for 6-month mortality compared with that for 1-year mortality, although this was not tested statistically. The proportion mediated by complications also attenuated significantly between adjusted and unadjusted analyses, as expected. These observations are novel and have important implications for targeting interventions for patients undergoing elective surgery.
That smoking is associated with increased mortality after elective surgical procedures is well known.12 13 Preoperative period has been proposed a ‘window of opportunity’ and a ‘teachable moment’ to help patients quit smoking.24 25 This study examined a critical question, that is, is this increased mortality mediated by the postoperative complications seen more commonly in smokers than in non-smokers? The evidence presented here confirmed that these postoperative complications mediated significant proportion of increased mortality risk, and that this varied by the type of complication. Pulmonary complications explained the most variation in this increased risk, as compared with cardiovascular complications or SSIs. Our findings suggest pulmonary complications are far more important contributors to the smoking–mortality association than the cardiovascular complications. There has been significant emphasis placed on preoperative cardiac risk assessment for non-cardiac surgery.26 Consensus statements on cardiac risk stratification including who should undergo screening and revascularisation and management of patients with implanted cardiac stents have been developed and widely disseminated.27–29 Perhaps this focus and attention on identifying and intervening on cardiac risk has mitigated the associations of smoking-related cardiovascular events with mortality, in both smokers and never smokers. Similar attention has not been given to preoperative risk stratification for postoperative pulmonary events. These events occur more frequently than cardiovascular events and lead to substantial postoperative mortality.30–35
Perioperative complications associated with smoking mediated a high proportion of the association of smoking and mortality before adjustment. But the proportion mediation was greatly attenuated after adjustment. This suggests that a major part of the mediation effect was contained in variables we adjusted for including ASA class. In addition, some of the association of smoking and subsequent mortality is related to lifetime exposure to smoking (direct effect), and not the association of smoking on perioperative complications (indirect effect through pulmonary complications). This may be related to occurrence of major lifetime complications from smoking, for example, COPD, coronary artery disease, various cancers and stroke, which can all contribute to postoperative mortality.
We did find that even after adjustment, smoking-related pulmonary complications mediated over 15% of the association of smoking and postoperative mortality. Thus, part of the association of smoking on mortality is because of a lifetime exposure, as shown previously,36 and part owing to immediate complications, such as pulmonary complications. The first goal should always be to get smokers to quit prior to surgery. But acknowledging that not all smokers will quit prior to their surgery, the surgical staff should be especially vigilant of pulmonary complications, as our data clearly demonstrates them to mediate mortality. Careful monitoring of adherence to pneumonia prevention guidelines in postoperative period as well as early diagnosis and management may lead to reduction in mortality. Far more importantly, preventive preoperative evaluation and optimisation of pulmonary health in addition to implementation of preoperative smoking cessation programmes in patients undergoing elective surgery have the likelihood of reducing the increased mortality risk. Consensus statements on pulmonary risk assessment and patients who should be referred for intervention are strongly needed.
We found that the attributable risk of SSI to smoking-related mortality was lower than that for pulmonary and cardiovascular complications. SSIs constitute the most common infection, accounting for 38% of all infections.6 In addition, SSIs are associated with significant increases in hospital stay,6 making them one of the most costly postoperative complications.6 37 SSIs are the third most common nosocomial infection overall, representing 14% of all hospital-acquired infections. Thus even though their contribution to mortality is lower, their common prevalence and the ability to institute measures to prevent them make them suitable targets for interventions.
The proportion mediated by each of the three complications was attenuated by adjustment for age, race/ethnicity, work RVU, surgeon specialty and ASA class, indicating that these factors may have contributed to mortality outcome. In addition, other factors that we did not measure in this study such as other smoking-related diseases such as cancer, COPD, etc may have contributed. Additionally, as is common in observational studies such as this, smoking status may be a marker for unmeasured variables that may be causal. Thus, smoking status should alert clinicians to other factors, which may need to be addressed preoperatively.
Our study has several limitations. It is possible that findings may not be generalisable to women, since our sample included primarily men, representative of US veterans. These findings may not be generalisable to non-veterans; however, it is unlikely that the pathway of smoking-associated mortality risk differs by the veteran status. The current smoker variable in VASQIP is collected retrospectively from medical records, which could lead to misclassification bias and underestimation of the association. Thus, these results are conservative estimates of these associations. Another limitation is that smoking status may change over time and the current study design and analyses did not take that into account. Mediation assumes no unmeasured variables; this is of course not true as we can never account for all omitted factors. We accounted for all the important variables to the best of our capability with the given data. Another limitation of the mediation analysis is that the proportion mediated is influenced by sample size, coefficient estimates and distribution of the outcomes/predictors and since our variables were dichotomous and we have small standardised coefficient estimates. Cause of death was not available to us, so these details could not be provided for smokers and never smokers.
In conclusion, this study found that a high proportion of association between smoking and postoperative 6-month and 1-year mortality is mediated by postoperative complications, especially pulmonary complications. Future efforts at reducing postoperative mortality should be aimed at preoperative risk identification and intervention. Efforts directed at pulmonary risk stratification, surveillance and prevention for pulmonary and other complications in smokers undergoing elective surgery may likely impact mortality in current smokers undergoing elective surgical procedures.
Supplementary Material
Acknowledgments
The authors acknowledge The VA Surgical Quality Data Use Group (SQDUG) for its role as scientific advisors and for the critical review of data use and analysis presented in this manuscript.
Footnotes
Contributors: JAS, MH, WGH and TKH contributed to the conception of the study. EJC and WGH were responsible for analysis. JAS, MH, WGH, TKH and EJC were responsible for review of analyses. JAS prepared the manuscript. JAS, MH, WGH, TKH and EJC critically revised the manuscript and given final approval. JAS submitted the approved manuscript.
Funding: Veterans Affairs Research Grant —VA IIR IAB 06-038-2.
Grant support, this material is the result of work supported with VA IIR IAB 06-038-2 and the use and resources of facilities at the Department of Veterans Affairs Medical Centers at Bedford, Massachusetts; Birmingham, Alabama; and Denver, Colorado. JAS is supported by research grants from the National Institute of Aging, National Cancer Institute and Agency for Health Quality and Research Center for Education and Research on Therapeutics (CERTs).
Competing interests: There are no financial conflicts related to this work. JAS has received investigator-initiated research grants from Allergan, Takeda and Savient; consultant fees from URL pharmaceuticals, Takeda, Savient, Ardea, Allergan and Novartis; and is a member of the executive of OMERACT, an organisation that develops outcome measures in rheumatology and receives arms-length funding from 36 companies. JAS is also a member of the American College of Rheumatology's Guidelines Subcommittee of the Quality of Care Committee and Veterans Affairs Rheumatology Field Advisory Committee. Other authors declare no conflict of interest.
Ethics approval: Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. JAMA 2004;291:1238–45 [DOI] [PubMed] [Google Scholar]
- 2.Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001;135:847–57 [DOI] [PubMed] [Google Scholar]
- 3.Land T, Warner D, Paskowsky M, et al. Medicaid coverage for tobacco dependence treatments in Massachusetts and associated decreases in smoking prevalence. PLoS ONE 2010;5:e9770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC State-specific prevalence of cigarette smoking and smokeless tobacco use among adults—United States, 2009. MMWR Morb Mortal Wkly Rep 2010;59:1400–6 [PubMed] [Google Scholar]
- 5.Office of Quality and Performance VHA Health behaviors of veterans in the VHA: tobacco use—1999 large health survey of VHA enrollees. Washington, DC: Veterans Health Administration, 2001 [Google Scholar]
- 6.Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999;20:250–78 [DOI] [PubMed] [Google Scholar]
- 7.Brooks-Brunn JA. Predictors of postoperative pulmonary complications following abdominal surgery. Chest 1997;111:564–71 [DOI] [PubMed] [Google Scholar]
- 8.Alberg AJ, Margalit R Stashefsky, Burke A, et al. The influence of offering free transdermal nicotine patches on quit rates in a local health department's smoking cessation program. Addict Behav 2004;29:1763–78 [DOI] [PubMed] [Google Scholar]
- 9.Koffman DM, Lee JW, Hopp JW, et al. The impact of including incentives and competition in a workplace smoking cessation program on quit rates. Am J Health Promot 1998;13:105–11 [DOI] [PubMed] [Google Scholar]
- 10.Lenert L, Munoz RF, Perez JE, et al. Automated e-mail messaging as a tool for improving quit rates in an internet smoking cessation intervention. J Am Med Inform Assoc 2004;11:235–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mills E, Eyawo O, Lockhart I, et al. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med 2011;124:144–54 e148 [DOI] [PubMed] [Google Scholar]
- 12.Ashraf MN, Mortasawi A, Grayson AD, et al. Effect of smoking status on mortality and morbidity following coronary artery bypass surgery. Thorac Cardiovasc Surg 2004;52:268–73 [DOI] [PubMed] [Google Scholar]
- 13.Jones R, Nyawo B, Jamieson S, et al. Current smoking predicts increased operative mortality and morbidity after cardiac surgery in the elderly. Interact Cardiovasc Thorac Surg 2011;12:449–53 [DOI] [PubMed] [Google Scholar]
- 14.Sakuma LM, Machado FS, Mde A Martins. Independent association of smoking with postoperative cardiac events and thirty-day mortality. Arq Bras Cardiol 2010;94:625–32 [DOI] [PubMed] [Google Scholar]
- 15.Hawn MT, Houston TK, Campagna EJ, et al. The attributable risk of smoking on surgical complications. Ann Surg 2011;254:914–20 [DOI] [PubMed] [Google Scholar]
- 16.Khuri SF, Daley J, Henderson W, et al. The National Veterans Administration Surgical Risk Study: risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg 1995;180:519–31 [PubMed] [Google Scholar]
- 17.Davis CL, Pierce JR, Henderson W, et al. Assessment of the reliability of data collected for the Department of Veterans Affairs national surgical quality improvement program. J Am Coll Surg 2007;204:550–60 [DOI] [PubMed] [Google Scholar]
- 18.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82 [DOI] [PubMed] [Google Scholar]
- 19.Daley J, Khuri SF, Henderson W, et al. Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg 1997;185:328–40 [PubMed] [Google Scholar]
- 20.Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA 1961;178:261–6 [DOI] [PubMed] [Google Scholar]
- 21.Weaver F, Hynes D, Hopkinson W, et al. Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty 2003;18:693–708 [DOI] [PubMed] [Google Scholar]
- 22.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods 2002;7:422–45 [PubMed] [Google Scholar]
- 23.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev 1993;17:144–58 [Google Scholar]
- 24.Shi Y, Warner DO. Surgery as a teachable moment for smoking cessation. Anesthesiology 2010;112:102–7 [DOI] [PubMed] [Google Scholar]
- 25.Warner DO. Helping surgical patients quit smoking: why, when, and how. Anesth Analg 2005;101:481–7, table of contents [DOI] [PubMed] [Google Scholar]
- 26.Karnath BM. Preoperative cardiac risk assessment. Am Fam Physician 2002;66:1889–96 [PubMed] [Google Scholar]
- 27.Almanaseer Y, Mukherjee D, Kline-Rogers EM, et al. Implementation of the ACC/AHA guidelines for preoperative cardiac risk assessment in a general medicine preoperative clinic: improving efficiency and preserving outcomes. Cardiology 2005;103:24–9 [DOI] [PubMed] [Google Scholar]
- 28.Hoeks SE, Poldermans D. European Society of Cardiology 2009 guidelines for preoperative cardiac risk assessment and perioperative cardiac management in noncardiac surgery: key messages for clinical practice. Pol Arch Med Wewn 2010;120:294–9 [PubMed] [Google Scholar]
- 29.Poldermans D, Bax JJ, Boersma E, et al. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery: the task force for preoperative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery of the European Society of Cardiology (ESC) and endorsed by the European Society of Anaesthesiology (ESA). Eur J Anaesthesiol 2010;27:92–137 [DOI] [PubMed] [Google Scholar]
- 30.Sogame LC, Vidotto MC, Jardim JR, et al. Incidence and risk factors for postoperative pulmonary complications in elective intracranial surgery. J Neurosurg 2008;109:222–7 [DOI] [PubMed] [Google Scholar]
- 31.Kanat F, Golcuk A, Teke T, et al. Risk factors for postoperative pulmonary complications in upper abdominal surgery. ANZ J Surg 2007;77:135–41 [DOI] [PubMed] [Google Scholar]
- 32.Salahuddin N, Fatimi S, Salahuddin N, et al. Predicting postoperative cardio-pulmonary complications by a test of stair climbing. J Coll Physicians Surg Pak 2005;15:761–4 [PubMed] [Google Scholar]
- 33.Hulzebos EH, Van Meeteren NL, De Bie RA, et al. Prediction of postoperative pulmonary complications on the basis of preoperative risk factors in patients who had undergone coronary artery bypass graft surgery. Phys Ther 2003;83:8–16 [PubMed] [Google Scholar]
- 34.Trayner E, Jr, Celli BR. Postoperative pulmonary complications. Med Clin North Am 2001;85:1129–39 [DOI] [PubMed] [Google Scholar]
- 35.Mitchell CK, Smoger SH, Pfeifer MP, et al. Multivariate analysis of factors associated with postoperative pulmonary complications following general elective surgery. Arch Surg 1998;133:194–8 [DOI] [PubMed] [Google Scholar]
- 36.Bueno de Mesquita HB, Maisonneuve P, Moerman CJ, et al. Life-time history of smoking and exocrine carcinoma of the pancreas: a population-based case-control study in The Netherlands. Int J Cancer 1991;49:816–22 [DOI] [PubMed] [Google Scholar]
- 37.Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004;199:531–7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


