Abstract
Oesophageal atresia (OA) and tracheo-oesophageal fistula (TOF) are important human birth defects of unknown aetiology. The embryogenesis of OA/TOF remains poorly understood mirroring the lack of clarity of the mechanisms of normal tracheo-oesophageal development. The development of rat and mouse models of OA/TOF has allowed the parallel study of both normal and abnormal embryogenesis. Although controversies persist, the fundamental morphogenetic process appears to be a rearrangement of the proximal foregut into separate respiratory (ventral) and gastrointestinal (dorsal) tubes. This process depends on the precise temporal and spatial pattern of expression of a number of foregut patterning genes. Disturbance of this pattern disrupts foregut separation and underlies the development of tracheo-oesophageal malformations.
Introduction
Oesophageal atresia (OA) and tracheo-oesophageal fistula (TOF) are relatively common birth defects (approximately 1 in 3000 live births) and represent a challenge to the paediatric surgeon both in terms of surgical repair and the management of the long term morbidity. In about half the cases, there are malformations in other organ systems with the cardiovascular system being most commonly involved(1;2). Of several malformation associations involving OA/TOF, the best described is the VACTERL association which includes vertebral, anorectal, cardiac, tracheo-esophageal, renal and limb malformations(3).
The great majority of cases of OA/TOF occur as sporadic events and, together with the low recurrence risk (approximately 1%) and the low twin concordance rate (2.5%), this has previously been taken as evidence for a primarily non-genetic aetiology. There is, however, emerging evidence of an important role for genetic factors with the identification of disorders resulting from single gene mutations and chromosomal disorders, both featuring OA/TOF(4;5).
Our understanding of the embryology of OA/TOF has lagged considerably behind the dramatic improvement in the survival of affected neonates. This lag reflects continuing lack of clarity of the mechanisms of normal tracheo-oesophageal embryogenesis. In this review, we discuss the current understanding of both normal tracheo-oesophageal development and the disturbances in the molecular, cellular and morphogenetic mechanisms that underlie the embryogenesis of OA/TOF, primarily in teratogen-based and genetic models in rats and mice. These animal models of abnormal morphogenesis mainly relate to proximal OA with distal TOF, which is by far the commonest type, although the underlying mechanisms are likely to apply across the spectrum of malformations.
Normal embryogenesis
The allocation of the cells of the early embryo to the three principal germ layers (ectoderm, mesoderm and endoderm) is followed by a series of folding morphogenetic movements that convert the flat endodermal layer into the primitive gut tube. The respiratory system is derived from the foregut endoderm with the appearance of the laryngo-tracheal groove in the ventral floor of the foregut, just caudal to the level of the pharynx(6). Despite intense interest in the mechanisms of lung development(7), the events underlying the morphogenesis of the proximal respiratory structures have been the subject of continuing debate. In particular, the process by which the trachea is defined and becomes separate from the original foregut tube is not well understood.
Morphogenetic controversies
In broad terms, there have been two contrasting theories to explain how the respiratory foregut, cranial to the point of origin of the bronchopulmonary buds, separates from the gastrointestinal (oesophageal) foregut. One theory suggests that the respiratory system develops as a result of rapid outgrowth from the original foregut tube(8). This would be in keeping with the mode of development of other foregut derivatives, both midline and lateral. For example, the thyroid, thymus and parathyroid glands all bud off the foregut and rapidly grow away from it, eventually losing their original connection to it. The outgrowth theory is also consistent with the accepted pattern of rapid longitudinal growth at the distal tips of the developing bronchopulmonary structures. Applied to the trachea, this theory suggests that the tracheal primordium buds off the ventral foregut and remains as a separate structure from the foregut during the subsequent stages of development. This has been likened to the way a column of water forms after a tap is switched on (the so-called tap and water theory) (Fig. 1 a,b).
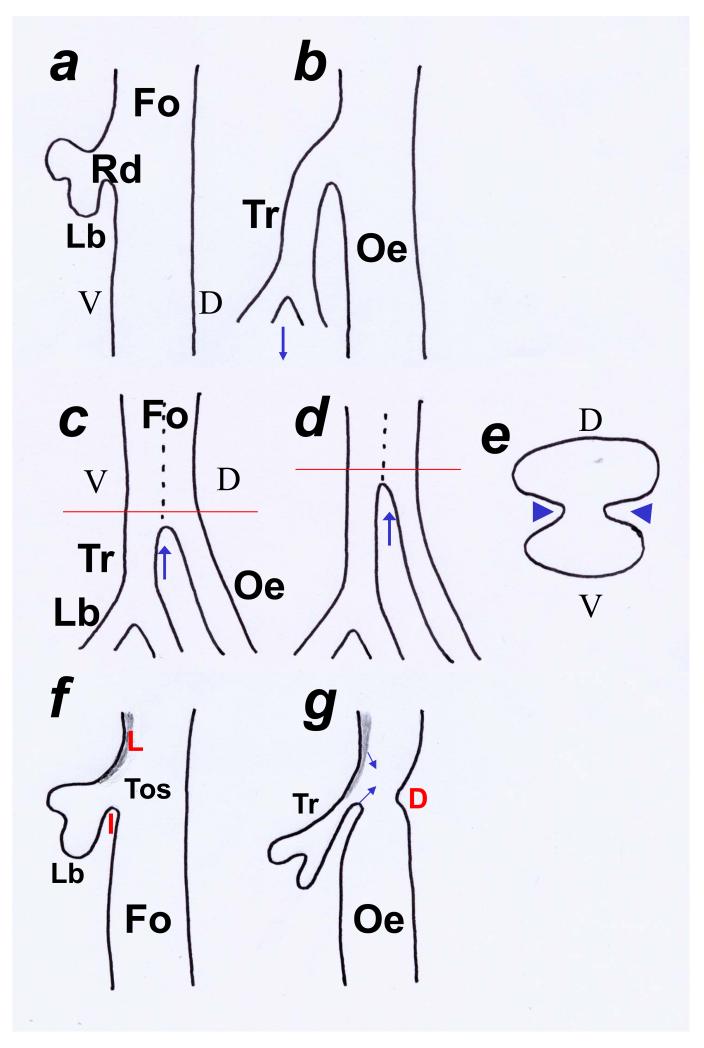
Fig. 1. Models of tracheo-oesophageal separation.
Schematic representation of the foregut illustrating theories of tracheo-oesophageal separation. Sagittal sections of the foregut (Fo) in a, b, c, d, f and g and transverse section in e at levels indicated in c and d. (a,b) One theory considers the respiratory diverticulum (Rd) to appear as a ventral evagination from the foregut with the two lung buds (Lb) at its caudal limit. It has been postulated that the trachea becomes separated from the oesophagus as a result of rapid downward growth (arrow in b) of the respiratory diverticulum. According to this theory, the trachea is never part of an undivided foregut and this model has been likened to a column of water emerging from a tap (tap and water theory). (c-e) An alternative theory suggests that the foregut initially elongates as an undivided structure having both ventral (V; tracheal) and dorsal (D; oesophageal) components (dotted line demarcates components in c and d). This theory suggests that the foregut then separates into the trachea (Tr) and oesophagus (Oe) as a result of the growth, in the coronal plane, of lateral mesenchymal ridges (arrowheads in e) which fuse to form a mesenchymal septum. Separation initially occurs at the level of the origin of the lung buds (Lb) and progresses in a rostral direction (arrows in c and d). A parallel theory supports the caudo-rostral progression of separation although it postulates that the lateral walls collapse and fuse, resulting in separation. This theory rejects the development of a septum. (f,g) In a third theory, paired laryngeal (L) and single inferior (I) folds define the tracheo-oesophageal space (Tos). Subsequent approximation (arrows) of these folds defines the separate trachea and oesophagus. The dorsal (D) fold marks the boundary between the pharynx and oesophagus.
An alternative theory suggests that there is active growth of a mesenchymal septum which develops in the coronal plane and, as a result, separates the foregut lumen into ventral (respiratory) and dorsal (gastrointestinal) structures (Fig. 1 c,d)(9;10). This theory postulates that the septum is formed by opposing epithelio-mesenchymal ridges that grow medially and meet in the midline, resulting in separation (Fig. 1 e). Furthermore, the septum has been described as ascending, with the separation first being established distally, at the level of the bronchopulmonary buds. Direct evidence of septum formation has, however, been lacking, casting doubt on this theory. Indeed, most studies of tracheo-oesophageal development have failed to identify such a structure(11-13). Other theories support the notion of fusion of the lateral foregut walls, resulting in separation of the trachea from the oesophagus. Separation progresses in a caudo-rostral direction but does not involve the development of a septum(14).
A third theory combines elements of both main theories and uses scanning electron microscope images of chick embryos to suggest that tracheo-oesophageal separation is the result of the development of foregut folds(13;15). This theory describes three foregut folds: anterocranial or laryngeal, dorsal or pharyngo-oesophageal and inferior or tracheo-oesophageal (Fig. 1 f,g). The paired laryngeal and single tracheo-oesophageal folds appear first (day 2.5) defining between them the tracheo-oesophageal space. Subsequently, caudal movement of the laryngeal folds and cranial movement of the tracheo-oesophageal folds results in reduction of the tracheo-oesophageal space and the definition of a separate trachea and oesophagus. At the same time (day 3.5), the pharyngo-oesophageal fold appears dorsally and marks the boundary between pharynx and oesophagus. The approximation of the folds and tracheo-oesophageal separation are followed by rapid longitudinal growth of the trachea and oesophagus.
One study has attempted to resolve the controversy by measuring the foregut lengths between reproducible reference points (last pharyngeal pouch, respiratory primordium, tracheo-oesophageal separation and tracheal bifurcation) at various stages of foregut development(14). The authors concluded that both proliferation and lengthening, as well as active separation, contribute to the emergence of a separate trachea and oesophagus. Specifically, this study suggests that the formation of a tracheo-oesophageal groove and the fusion of the lateral epithelial walls of the foregut result in separation. Lengthening and proliferation play a role in the completion of separation at the level of the larynx.
Other studies that support the outgrowth (tap and water) theory have shown that the point of tracheo-oesophageal divergence remains constant relative to the pharynx and the level of the first cervical vertebra(8;12). This observation is not consistent with a theory of active tracheo-oesophageal separation that progresses in a caudal to cranial direction. This apparent conundrum has been addressed by another study that used digitised three-dimensional reconstructions of the foregut based on sequential transverse sections. The findings suggest that the trachea does separate from the undivided foregut in a caudocranial direction and that the distance between the separation point and the pharynx appears constant as a result of the ongoing lengthening of the cranial foregut(16).
More recently, data from mouse studies point to a process of active separation of the foregut into respiratory and gastrointestinal structures (Ioannides et al., 2008 submitted). There is an absolute reduction in the length of the undivided respiratory foregut proximal to the point of tracheo-oesophageal separation, while concurrently the length of divided foregut increases. Moreover, total increase in foregut length is independent of tracheo-oesophageal separation, arguing strongly against the outgrowth theory of foregut division.
In conclusion, there is mounting evidence to support the notion that physical separation of the original foregut tube plays a key role in tracheo-oesophageal organogenesis although confirmation of these events could only follow real-time imaging of foregut morphogenesis.
Molecular aspects of tracheo-oesophageal development
Respiratory field specification
The process that directs the positioning and establishment of the respiratory primordium in the ventral foregut is less well understood than the subsequent processes of branching morphogenesis and cytodifferentiation of the pulmonary epithelium. A number of studies have identified the homeodomain transcription factor Nkx2.1 as an early respiratory marker expressed in the ventral, prospective-respiratory epithelium of the foregut. The upstream events that control the timing, and the anteroposterior and dorso-ventral positioning, of the Nkx2.1- positive domain are not well understood. A recent study of lung bud formation in the chicken embryo has identified specific mesodermal factors that may play role in respiratory specification. Expression of Tbx4, a member of the T-box transcription factor gene family, correlates closely, both temporally and spatially, with the anteroposterior regionalisation of the respiratory primordium within the foregut(17). Gene expression studies demonstrate that the posterior boundaries of Tbx4 and Nkx2.1 are identical. Furthermore, ectopic expression of Tbx4 was shown to induce ectopic Nkx2.1 expression, albeit only in the ventral foregut endoderm. The action of Tbx4 could be mediated by Fgf10, as Tbx4 defines an Fgf10 mesodermal expression domain during early respiratory development. Interestingly, Fgf10 null mutants develop a trachea but lack any subsequent pulmonary branching morphogenesis(18). Other factors potentially involved in the specification of the lung primordium include the mesodermally expressed Gli family of transcription factors. Double homozygous Gli2−/−; Gli3 −/− embryos completely fail to develop respiratory structures and show a reduction in expression of the endodermal marker Hnf3β(19).
Molecular control of tracheo-oesophageal separation
Evidence from mouse studies suggests that boundaries between Shh expressing and non-expressing domains may play a role in respiratory system development. Shh expression is tightly regulated so that it shifts from the ventral, prospective-tracheal, epithelium (at E10.5) to the dorsal, oesophageal epithelium as tracheo-oesophageal separation proceeds in a caudal to cranial direction (at E11.5)(20). These changes in Shh expression are restricted to the foregut caudal to the pharynx and cranial to the lung buds. Strong ventral expression with a definite dorso-ventral boundary starts at the level of the laryngo-tracheal groove. At the caudal end of the tracheal epithelium, the strong Shh expression in the lung buds is not down-regulated even after tracheo-oesophageal separation is completed. These observations suggest that Shh is specifically upregulated in the ventral, prospective-tracheal epithelium and downregulated in the epithelium of the definitive trachea. Conversely, Shh expression appears to be downregulated in the dorsal, prospective-oesophageal epithelium and upregulated in the epithelium of the definitive oesophagus. This complete and specific ventral-to-dorsal switch in Shh expression, which immediately precedes tracheo-oesophageal separation, suggests that Shh may have a role in the separation process itself. Factors other than those involved in Shh signaling, but which are expressed in a dorso-ventral pattern in the anterior foregut, could also play a role in tracheo-oesophageal separation. The transcription factor Nkx2.1 is likely to be an important player, as demonstrated by the failure of separation in Nkx2.1 null mutant embryos(21). Evidence from a chick study shows that misexpression of the mesodermal factor Tbx4 induces ectopic Nkx2.1 expression and disrupts the process of tracheo-oesophageal separation(17). Conversely, factors such as Sox2 which is expressed in the dorsal, oesophageal-prospective, foregut could also play a role as evidenced by the failure of separation in embryos with reduced Sox2 function(22). Members of the Bmp (bone morphogenetic protein) pathway are also expressed in well defined dorso-ventral domains both in the endoderm and mesoderm and disruption of that pathway has resulted in failed tracheo-oesophageal separation(23;24).
The role of programmed cell death
A number of studies have focused on the role of programmed cell death (PCD) or apoptosis in the separation process. These studies have detected large numbers of dying cells in the approximating lateral epithelial ridges at the point of tracheo-oesophageal separation(25-28). They suggested that apoptosis plays a role in remodelling and reshaping the separating foregut. These studies have not described any PCD activity in the developing foregut at earlier stages of development, or at different levels within the developing foregut, suggesting a rather limited role for PCD in physically separating and reorganising the dividing foregut. These same studies have confirmed that following separation, PCD is rare within the foregut, suggesting that it plays a specific role in the process. These studies have however not addressed the question whether apoptosis is a consequence or a requirement of separation. In our recent studies, we confirmed the presence of PCD at the point of tracheo-oesophageal separation and also demonstrated a reproducible ventral-to-dorsal shift in PCD as the level of separation is approached. We went on to test the role of cell death experimentally using a whole embryo in vitro culture system and demonstrated that the use of an apoptosis inhibitor (z-VAD-fmk) disturbs tracheo-oesophageal separation proving that PCD is required for this morphogenetic process (Ioannides et. al., 2008 submitted).
Abnormal embryogenesis
One of the reasons that abnormal morphogenesis is not well understood is the lack of any significant number of human embryos with OA/TOF that are available for study at the appropriate stages of gestation (the separation process occurs in the human embryo between Carnegie stages 13 and 16 which is 28-37 days post-fertilisation). Furthermore, there are no satisfactory alternative techniques for the study of these defects, such as in vitro culture models or computer generated three dimensional reconstructions.
The use of animal models
In view of these shortcomings, the development of a reliable and reproducible animal model of these malformations had been a goal of paediatric surgical researchers for decades. A number of mechanical techniques (oesophageal ligation, embryo hyperflexion) were initially used to produce tracheo-oesophageal malformations(29-31). The major drawback of these approaches was that they assumed a mechanistic embryological basis for tracheo-oesophageal malformations, ignored any cellular and molecular aspects of the aetiology of these anomalies and did not attempt to understand OA/TOF in terms of an aberration of normal tracheo-oesophageal development. Depleting vitamin A or riboflavin from the diet of pregnant rats caused tracheo-oesophageal malformations including OA/TOF, but these were not consistent(32;33).
The study of the effect of teratogenic agents on embryo development appeared more promising. In 1978, Thompson et al, described a number of malformations, including OA/TOF, in rat and rabbit foetuses exposed in utero to the anticancer agent Adriamycin (doxorubicin hydrochloride)(34). This observation was followed up by Diez-Pardo et al (1996) who described in detail the first reproducible model of tracheo-oesophageal malformations based on exposure to this particular teratogenic agent. This model was subsequently adapted to the mouse in order to facilitate the study of the cellular and molecular events that underlie abnormal morphogenesis(35;36).
Loss of function mutations in foregut patterning genes have been generated in mice in order to study the role of these genes in development. The developmental defects caused by these mutations include tracheo-oesophageal malformations. Although the tracheo-oesophageal phenotype may differ from that described in the Adriamycin-treated rat, these models represent a unique opportunity to gain an insight into the genetic and molecular mechanisms that underlie the development of tracheo-oesophageal malformations in contrast to the Adriamycin model, whose molecular basis is unknown and could involve a multitude of molecular effects. The mouse genes whose mutation yields foregut defects are summarised in Table 1.
Table 1.
Mouse genes, mutations in which cause tracheo-oesophageal malformations
| Gene | Function | Foregut phenotype | Reference |
|---|---|---|---|
| Shh | Secreted glycoprotein with multiple patterning roles |
OA/TOF and fused/ hypoplastic lungs |
(54) |
| Nog | Secreted BMP antagonist |
OA/TOF and defects in lung branching |
(23) |
| Sox2 | Transcription factor | OA/TOF | (22) |
| Nkx2.1 | Homeodomain transcription factor |
Undivided oesophagotrachea and hypoplastic lungs |
(21) |
| Gli2/Gli3 | Zinc-finger transcription factors |
Undivided oesophagotrachea and hypoplastic lungs |
(19) |
| Foxf1 | Forkhead transcription factor |
OA/TOF and hypoplastic lungs | (57) |
| Hoxc4 | Homeobox transcription factor |
Partial or complete blockage of oesphageal lumen |
(60) |
| RAR α/β2 | Retinoic acid receptors |
Undivided oesophagotrachea | (61) |
Theories of disturbed tracheo-oesophageal morphogenesis
Analysis of the rat model has contributed significantly to our understanding of the embryogenesis of tracheo-oesophageal malformations. A number of theories have been put forward which themselves reflect the theories of normal development. One such proposal assumes that normal tracheal development and tracheo-oesophageal separation is the result of rapid longitudinal growth of the tracheal primordium away from the foregut. According to this theory, tracheo-oesophageal malformations are fundamentally caused by a failure of tracheal growth, the result of which is a compensatory overgrowth of the undivided foregut with the bronchopulmonary buds originating directly from the foregut (Fig. 2a,b)(8;37;38).
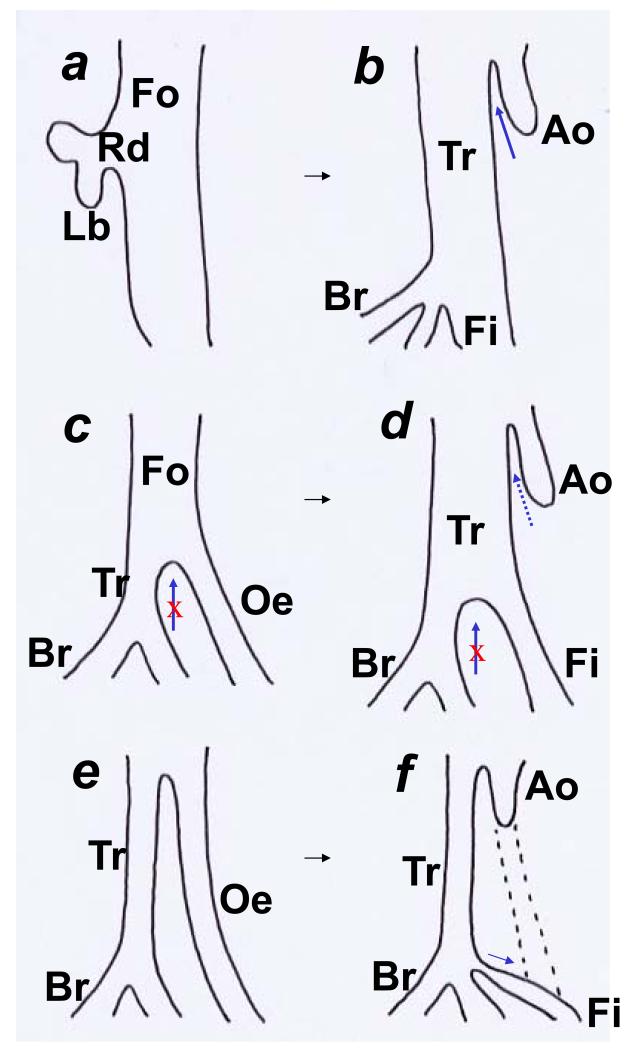
Fig. 2. Theories on the development of oesophageal atresia and tracheo-oesophageal fistula.
Schematic representations (sagittal sections) of the foregut illustrating the theories to explain the faulty organogenesis in oesophageal atresia (OA) and tracheo-oesophageal fistula (TOF). (a,b) In the first theory, the respiratory diverticulum (Rd) fails to elongate resulting in failure of the trachea to grow (tracheal agenesis) in contrast to the lung buds that develop normally. The overall growth and elongation of the foregut continues with the bronchial structures originating directly from the foregut. At a later stage, the foregut rostral to the bronchi assume tracheal (Tr) histological characteristics whereas the foregut distal to the bronchial origin connects to the stomach and is described as the fistula (Fi). The upper atretic oesophagus (Ao) results from rearrangement of the anterior foregut (arrow in b). (c,d) In the second theory, the process of tracheo-oesophageal separation becomes arrested (arrows in c and d). If the failure is only partial, a small length of oesophagus (Oe) does separate from the trachea, whereas total failure of separation yields an almost completely undivided tracheo-oesophagus. Following the arrest of separation, the undivided foregut assumes the histological characteristics of trachea whereas the initially separated oesophagus becomes the fistula that connects the trachea to the stomach. The upper atretic oesophagus forms, as in the first theory, by late rearrangement of the anterior foregut (dotted arrow in d). (e,f) In contrast to the first two theories, the third postulates that normal tracheo-oesophageal separation does take place. An insult to the embryo (possibly ischaemic) results in loss of part of the oesophagus (dotted lines in f) resulting in an atretic upper oesophageal pouch. The development of the fistula from the trachea (arrow in f) compensates for the oesophageal loss by reconnecting to the stomach. This theory suggests that the fistula is a structure of respiratory origin.
According to a second theory, normal development depends on an active separation process that divides the foregut into a ventral trachea and a dorsal oesophagus and it is this process that fails (Fig. 2c,d)(14;16). Interestingly, both of these theories share one important point: atresia of the proximal oesophagus is not part of the initial malformation. Both theories suggest that the atretic oesophagus is a result of late rearrangement of the cranial foregut resulting in a blind-ending structure in the dorsal mesenchyme. According to both theories, the tracheo-oesophageal fistula represents the primitive foregut distal to the origin of the bronchopulmonary buds, which connects the undivided foregut to the stomach. The near-term arrangement is completed by trachealisation of the undivided foregut.
A third theory is in sharp contrast with the two described above. It proposes that the oesophagus does develop initially as a separate structure which then becomes atretic secondary to an, as yet undetermined, event. According to this theory, the tracheo-oesophageal fistula grows from the trachea at the level of the lung buds and reconnects with the stomach in order to re-establish the continuity of the gastrointestinal tract (Fig. 2e,f)(39;40).
Finally, proponents of the foregut fold theory have suggested that OA/TOF is caused by abnormal movement of the pharyngo-oesophageal fold which comes to lie too far ventrally, leading to failure of division of the tracheo-oesophageal space and subsequent trachealisation of the undivided structure(13). This theory is based on observations of normal chick development rather than study of a model of tracheo-oesophageal malformations.
Molecular mechanisms in the Adriamycin models
Studies of the rat and mouse Adriamycin models have suggested possible molecular mechanisms in the embryogenesis of tracheo-oesophageal malformations. One group studied the expression of the respiratory marker Nkx2.1 and found it to be expressed in the tracheo-oesophageal fistula throughout gestation, leading to the conclusion that it is a respiratory structure(41). In this particular study, the trachea was found to trifurcate into three Nkx2.1-positive structures (two bronchi and a fistula). The conclusion was that an imbalance between respiratory and gastrointestinal fates underlies the development of OA/TOF. The same group addressed the question of the difference in the branching characteristics between the three Nkx2.1-positive branches of the trachea. Although Nkx2.1-positive, the fistula did not develop branches but connected the trachea to the stomach. They found a difference in the activity of the FGF signalling pathway in the epithelium and mesenchyme of the fistula compared to the epithelium and mesenchyme of the bronchi and attributed to this the failure of the fistula to develop branches. Specifically, reduced levels of FGF1 and FGF7 mRNA were detected in the fistula mesenchyme and there was absence of transcripts of the FGF7 and FGF10 receptor FGF2R-IIIb in the fistula epithelium(40;42;43). However, study of the Adriamycin mouse model has contradicted the respiratory origin of the fistula by demonstrating that it is essentially an Nkx2.1-negative structure originating from the dorsal, gastrointestinal part of the undivided foregut(35).
More recently, Sonic hedgehog has been implicated in the development of Adriamycin-induced malformations. In one study, reduced levels of Shh protein have been found in the foregut of Adriamycin-treated embryos developing OA/TOF(44). In another, reduced levels of mRNA for Gli-2 (a key member of the Shh signalling cascade) have been found in the mesenchyme of the fistula(45). A further study reported a disturbance in the spatial pattern of Shh expression in the foregut of Adriamycin-treated embryos, showing failure of downregulation of Shh at the site of tracheo-oesophageal separation(28). In human neonates with OA/TOF, Shh protein is absent from the epithelium of the fistula but present in the epithelium of the atretic oesophagus(46). Our analysis of the Adriamycin mouse model of OA/TOF has shown that failure of tracheo-oesophageal separation is associated with disturbance of the Shh dorso-ventral boundary of foregut expression and loss of the precise ventral-to-dorsal switch in expression(20).
Another important aspect of abnormal morphogenesis in the Adriamycin models of OA/TOF are defects of the notochord(47-49). These range from notochord duplications to abnormally shaped and ectopic notochords. A frequent observation is that the abnormal notochord remains attached to the foregut tube, whereas normally the two structures would become separated. These notochordal defects could be implicated in the embryogenesis of OA/TOF in different ways. A persistent attachment to the foregut could interfere with foregut lengthening during periods of rapid growth and provide a mechanical explanation for the development of the malformations(50;51). Furthermore, the notochord acts as an important source of diffusible signals that have been shown to play a key role in both neural tube patterning and hepatic/ pancreatic specification in the more distal foregut(52). One of these diffusible signals is Shh and it would be plausible to speculate that an abnormally positioned source of the Shh signal could lead to disturbance of the dorso-ventral patterning of the foregut and interfere with tracheo-oesophageal separation. The Adriamycin models have also demonstrated a disturbance of programmed cell death (PCD) within the developing foregut and specifically reduction of apoptotic cells on the lateral walls of the foregut at the site of epithelial folding in embryos with disturbed tracheo-oesophageal separation(26-28;53). However, these studies did not reveal whether this is simply a consequence of the failure of separation or has a role in its causation.
Molecular mechanisms in the mouse and human genetic models
Study of the mouse genetic models of OA/TOF allows more precisely focused analysis of the molecular events that underlie disturbed morphogenesis. Sonic hedgehog (Shh) null mutant embryos have disturbed tracheo-oesophageal development with the trachea and oesophagus having separate lumens but being very closely juxtaposed(54;55). The description of the caudal foregut in Shh−/− embryos includes a communication between the lungs and the stomach, and an atresia of the oesophagus, although these phenotypic arrangements were not illustrated in detail(54). The lungs themselves are abnormal, consisting of dilated sacs with reduced branching(54). The foregut phenotype of the double mutant Gli2−/−Gli3+/− is better defined. There is an undivided foregut ending in a trifurcation of two lung buds and a fistula to the stomach, while the lungs are fused with significantly reduced epithelial branching(19). Both the Shh−/− and Gli2−/−Gli3+/− embryos have malformations in other organ-systems. A number of these conform to the VACTERL association supporting the involvement of the Shh pathway in its embryogenesis(56). Haploinsufficiency of Foxf1 (also known as FREAC1 or HFH8), a transcriptional target of Shh also causes tracheo-oesophageal malformations including oesophageal atresia and tracheo-oesophageal fistula as well as lung hypoplasia and fusion of the lung lobes(57). An almost identical foregut phenotype to the Gli2−/−Gli3+/− mutants is produced by a loss of function mutation of the transcription factor and respiratory marker Nkx2.1, which is not a member of the Shh pathway(21;58). In these embryos, there is failure of tracheo-oesophageal separation and an undivided oesophagotrachea connects the pharynx to the stomach. The bronchi originate from this undivided tube and the lungs are markedly hypoplastic.
Recent studies have implicated the Bmp signalling pathway in the embryogenesis of OA/TOF. Mice homozygous null for Noggin (Nog), a Bmp antagonist exhibit failed tracheo-oesophageal separation(23;24). In normal development Nog is expressed in the dorsal half of the pre-separation foregut, in a pattern that is complementary to the expression of its antagonist Bmp4 in the ventral mesoderm surrounding the ventral half of the foregut. This finely regulated dorso-ventral expression balance is disturbed in Nog mutants with resulting failure of separation. Interestingly, disturbance of expression of another dorsal marker Sox2 also leads to failed separation in mutant embryos(22).
The characterisation of human genetic conditions that feature OA/TOF supports the role of particular molecular factors in the embryogenesis of the malformations. The various single gene and chromosomal conditions with OA/TOF are summarised in Table 2. Interestingly, the human homologue of Nog is found on 17q and OA/TOF has been described as part of the 17q22 deletion phenotype. The identification of SOX2 as the gene responsible for the AEG (anophthalmia, esophageal atresia, genital) syndrome assumes an even more important role with the description of the Sox2 mouse model. Similarly, mutations in GLI3 (a member of the SHH signalling pathway) also cause tracheo-oesophageal malformations as part of Pallister-Hall syndrome(59). It seems likely that the enormous advances in our understanding of the human genome will allow us to make best use in future of the information generated from the study of mouse genetics.
Table 2.
Human single gene and chromosomal disorders associated with tracheo-oesophageal malformations
| Name | Gene | Locus | Foregut malformations | References |
|---|---|---|---|---|
| CHARGE | CHD7 | 8q12 | OA/TOF | (62) |
| Feingold | MYCN | 2p24.1 | OA/TOF | (63) |
| Fanconi | FANCC | 9p22.3 | OA/TOF | (64) |
| Anophthalmia- Esophageal-Genital (AEG) |
SOX2 | 3q26.3- q27 |
OA/TOF | (65) |
| Pallister-Hall | GLI3 | 7p13 | Laryngo-tracheo-oeosphageal cleft |
(59) |
| Opitz | MID1 | Xp22 | Laryngo-tracheo-oeosphageal cleft |
(66) |
| Full trisomies (13,18 & 21) |
OA/TOF | (67) | ||
| 3p25pter duplication |
OA/TOF | (68) | ||
| 5p15pter deletion | OA/TOF | (69) | ||
| 13q34qter deletion | OA/TOF | (70) | ||
| 17q22q23.3 deletion | OA/TOF | (71) | ||
| 22q11.2 deletion | OA/TOF | (72) |
Conclusion
The parallel development of both teratogenic and genetic models of OA/TOF has demonstrated that the fundamental developmental aberration appears to be the disturbance of the process of separating the foregut into a respiratory (ventral) and a gastrointestinal (dorsal) component. The study of the genetic models shows that factors which are expressed in a well defined dorso-ventral pattern within the anterior foregut at the time of separation are fundamental to this process and that loss of the dorso-ventral boundary of expression domains disrupts the physical separation of the foregut. This has been demonstrated for both respiratory and gastrointestinal markers (Nkx2.1 and Sox2) as well as for factors with more dynamic expression patterns (Shh and Nog). That exposure to a teratogenic agent disturbs this precisely regulated dorso-ventral expression (as in Shh expression by Adriamycin) leading to failed separation provides a unique insight into how a non-genetic factor can disrupt a specific developmental process. While the precise aetiology of the majority of human OA/TOF cases remains elusive, our understanding of the interplay between molecular and morphogenetic events may provide targets for modulation leading to possible prevention of these important birth defects, perhaps similar to the prevention of neural tube defects by the administration of folic acid.
Reference List
- (1).Chittmittrapap S, Spitz L, Kiely EM, Brereton RJ. Oesophageal atresia and associated anomalies. Arch Dis Child. 1989 Mar;64(3):364–8. doi: 10.1136/adc.64.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Spitz L. Esophageal atresia: past, present, and future. J Pediatr Surg. 1996 Jan;31(1):19–25. doi: 10.1016/s0022-3468(96)90313-9. [DOI] [PubMed] [Google Scholar]
- (3).Brown AK, Roddam AW, Spitz L, Ward SJ. Oesophageal atresia, related malformations, and medical problems: a family study. Am J Med Genet. 1999 Jul 2;85(1):31–7. doi: 10.1002/(sici)1096-8628(19990702)85:1<31::aid-ajmg7>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- (4).Shaw-Smith C. Oesophageal atresia, tracheo-oesophageal fistula, and the VACTERL association: review of genetics and epidemiology. J Med Genet. 2006 Jul;43(7):545–54. doi: 10.1136/jmg.2005.038158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Felix JF, Tibboel D, de KA. Chromosomal anomalies in the aetiology of oesophageal atresia and tracheo-oesophageal fistula. Eur J Med Genet. 2007 May;50(3):163–75. doi: 10.1016/j.ejmg.2006.12.004. [DOI] [PubMed] [Google Scholar]
- (6).Ten Have-Opbroek AAW Lung development in the mouse embryo. Exp Lung Res. 1991;17:111–30. doi: 10.3109/01902149109064406. [DOI] [PubMed] [Google Scholar]
- (7).Maeda Y, Dave V, Whitsett JA. Transcriptional control of lung morphogenesis. Physiol Rev. 2007 Jan;87(1):219–44. doi: 10.1152/physrev.00028.2006. [DOI] [PubMed] [Google Scholar]
- (8).Sasaki T, Kusafuka T, Okada A. Analysis of the development of normal foregut and tracheoesophageal fistula in an adriamycin rat model using three-dimensional image reconstruction. Surg Today. 2001;31(2):133–9. doi: 10.1007/s005950170197. [DOI] [PubMed] [Google Scholar]
- (9).Arey LB. Developmental Anatomy. ed 7 Saunders; Philadelphia, PA: 1966. pp. 263–265. [Google Scholar]
- (10).Gray SW, Scandalakis JE. Embryology for surgeons. Saunders; Philadelphia, PA: 1972. pp. 63–100. [Google Scholar]
- (11).Zaw-Tun HA. The tracheo-esophageal septum--fact or fantasy? Origin and development of the respiratory primordium and esophagus. Acta Anat. 1982;114(1):1–21. [PubMed] [Google Scholar]
- (12).O’Rahilly R, Muller F. Chevalier Jackson lecture. Respiratory and alimentary relations in staged human embryos. New embryological data and congenital anomalies. Ann Otol Rhinol Laryngol. 1984 Sep;93(5 Pt 1):421–9. doi: 10.1177/000348948409300501. [DOI] [PubMed] [Google Scholar]
- (13).Kluth D, Steding G, Seidl W. The embryology of foregut malformations. J Pediatr Surg. 1987 May;22(5):389–93. doi: 10.1016/s0022-3468(87)80254-3. [DOI] [PubMed] [Google Scholar]
- (14).Qi BQ, Beasley SW. Stages of normal tracheo-bronchial development in rat embryos: Resolution of a controversy. Dev Growth Diff. 2000;42(2):145–53. doi: 10.1046/j.1440-169x.2000.00488.x. [DOI] [PubMed] [Google Scholar]
- (15).Kluth D, Fiegel H. The embryology of the foregut. Semin Pediatr Surg. 2003 Feb;12(1):3–9. doi: 10.1053/spsu.2003.50003. [DOI] [PubMed] [Google Scholar]
- (16).Williams AK, Quan QB, Beasley SW. Three-dimensional imaging clarifies the process of tracheoesophageal separation in the rat. J Pediatr Surg. 2003 Feb;38(2):173–7. doi: 10.1053/jpsu.2003.50037. [DOI] [PubMed] [Google Scholar]
- (17).Sakiyama J, Yamagishi A, Kuroiwa A. Tbx4-Fgf10 system controls lung bud formation during chicken embryonic development. Development. 2003 Apr;130(7):1225–34. doi: 10.1242/dev.00345. [DOI] [PubMed] [Google Scholar]
- (18).Sekine K, Ohuchi H, Fujiwara M, Yamasaki M, Yoshizawa T, Sato T, Yagishita N, Matsui D, Koga Y, Itoh N, Kato S. Fgf10 is essential for limb and lung formation. Nature Genet. 1999 Jan;21(1):138–41. doi: 10.1038/5096. [DOI] [PubMed] [Google Scholar]
- (19).Motoyama J, Liu J, Mo R, Ding Q, Post M, Hui CC. Essential function of Gli2 and Gli3 in the formation of lung, trachea and oesophagus. Nature Genet. 1998;20(1):54–7. doi: 10.1038/1711. [DOI] [PubMed] [Google Scholar]
- (20).Ioannides AS, Henderson DJ, Spitz L, Copp AJ. Role of Sonic hedgehog in the development of the trachea and oesophagus. J Pediatr Surg. 2003 Jan;38(1):29–36. doi: 10.1053/jpsu.2003.50005. [DOI] [PubMed] [Google Scholar]
- (21).Minoo P, Su G, Drum H, Bringas P, Kimura S. Defects in tracheoesophageal and lung morphogenesis in Nkx2.1(−/− ) mouse embryos. Dev Biol. 1999;209(1):60–71. doi: 10.1006/dbio.1999.9234. [DOI] [PubMed] [Google Scholar]
- (22).Que J, Okubo T, Goldenring JR, Nam KT, Kurotani R, Morrisey EE, Taranova O, Pevny LH, Hogan BL. Multiple dose-dependent roles for Sox2 in the patterning and differentiation of anterior foregut endoderm. Development. 2007 Jul;134(13):2521–31. doi: 10.1242/dev.003855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Que J, Choi M, Ziel JW, Klingensmith J, Hogan BL. Morphogenesis of the trachea and esophagus: current players and new roles for noggin and Bmps. Diff. 2006 Sep;74(7):422–37. doi: 10.1111/j.1432-0436.2006.00096.x. [DOI] [PubMed] [Google Scholar]
- (24).Li Y, Litingtung Y, Ten DP, Chiang C. Aberrant Bmp signaling and notochord delamination in the pathogenesis of esophageal atresia. Dev Dyn. 2007 Mar;236(3):746–54. doi: 10.1002/dvdy.21075. [DOI] [PubMed] [Google Scholar]
- (25).Qi BQ, Beasley SW. Preliminary evidence that cell death may contribute to separation of the trachea from the primitive foregut in the rat embryo. J Pediatr Surg. 1998 Nov;33(11):1660–5. doi: 10.1016/s0022-3468(98)90604-2. [DOI] [PubMed] [Google Scholar]
- (26).Zhou BY, Hutson JM, Farmer PJ, Hasthorpe S, Myers NA, Liu M. Apoptosis in tracheoesophageal embryogenesis in rat embryos with or without adriamycin treatment. J Pediatr Surg. 1999;34(5):872–5. doi: 10.1016/s0022-3468(99)90390-1. [DOI] [PubMed] [Google Scholar]
- (27).Williams AK, Qi BQ, Beasley SW. Temporospatial aberrations of apoptosis in the rat embryo developing esophageal atresia. J Pediatr Surg. 2000 Nov;35(11):1617–20. doi: 10.1053/jpsu.2000.18331. [DOI] [PubMed] [Google Scholar]
- (28).Orford J, Manglick P, Cass DT, Tam PP. Mechanisms for the development of esophageal atresia. J Pediatr Surg. 2001 Jul;36(7):985–94. doi: 10.1053/jpsu.2001.24722. [DOI] [PubMed] [Google Scholar]
- (29).Trahair JF, Wing SJ, Horn JL. Failure of short-term luminal IGF-I to protect against atrophy in a model of fetal esophageal atresia. J Pediatr Surg. 1995 Nov;30(11):1564–70. doi: 10.1016/0022-3468(95)90158-2. [DOI] [PubMed] [Google Scholar]
- (30).Wesson DE, Muraji T, Kent G, Filler RM, Almalchi T. The effect of intrauterine esophageal ligation on growth of fetal rabbits. J Pediatr Surg. 1984 Aug;19(4):398–9. doi: 10.1016/s0022-3468(84)80261-4. [DOI] [PubMed] [Google Scholar]
- (31).Kleckner SC, Pringle KC, Clark EB. The effect of chick embryo hyperflexion on tracheoesophageal development. J Pediatr Surg. 1984 Aug;19(4):340–4. doi: 10.1016/s0022-3468(84)80249-3. [DOI] [PubMed] [Google Scholar]
- (32).Wilson JG, ROTH CB, Warkany J. An analysis of the syndrome of malformations induced by maternal vitamin A deficiency. Effects of restoration of vitamin A at various times during gestation. Am J Anat. 1953 Mar;92(2):189–217. doi: 10.1002/aja.1000920202. [DOI] [PubMed] [Google Scholar]
- (33).Kalter H, Warkany J. Congenital malformations in inbred strains of mice induced by riboflavin-deficient, galactoflavin-containing diets. J Exp Zool. 1957 Dec;136(3):531–65. doi: 10.1002/jez.1401360308. [DOI] [PubMed] [Google Scholar]
- (34).Thompson DJ, Molello JA, Strebing RJ, Dyke IL. Teratogenicity of adriamycin and daunomycin in the rat and rabbit. Teratology. 1978 Apr;17(2):151–7. doi: 10.1002/tera.1420170207. [DOI] [PubMed] [Google Scholar]
- (35).Ioannides AS, Chaudhry B, Henderson DJ, Spitz L, Copp AJ. Dorso-ventral patterning in oesophageal atresia with tracheo-oesophageal fistula: evidence from a new mouse model. J Pediatr Surg. 2002;37:185–91. doi: 10.1053/jpsu.2002.30252. [DOI] [PubMed] [Google Scholar]
- (36).Dawrant MJ, Giles S, Bannigan J, Puri P. Adriamycin mouse model: a variable but reproducible model of tracheo-oesophageal malformations. Pediatr Surg Int. 2007 May;23(5):469–72. doi: 10.1007/s00383-006-1847-9. [DOI] [PubMed] [Google Scholar]
- (37).Possogel AK, Diez-Pardo JA, Morales C, Navarro C, Tovar JA. Embryology of esophageal atresia in the adriamycin rat model. J Pediatr Surg. 1998 Apr;33(4):606–12. doi: 10.1016/s0022-3468(98)90326-8. [DOI] [PubMed] [Google Scholar]
- (38).Merei J, Hasthorpe S, Farmer P, Hutson JM. Relationship between esophageal atresia with tracheoesophageal fistula and vertebral anomalies in mammalian embryos. J Pediatr Surg. 1998;33(1):58–63. doi: 10.1016/s0022-3468(98)90362-1. [DOI] [PubMed] [Google Scholar]
- (39).Crisera CA, Connelly PR, Marmureanu AR, Colen KL, Rose MI, Li M, Longaker MT, Gittes GK. Esophageal atresia with tracheoesophageal fistula: suggested mechanism in faulty organogenesis. J Pediatr Surg. 1999;34(1):204–8. doi: 10.1016/s0022-3468(99)90258-0. [DOI] [PubMed] [Google Scholar]
- (40).Crisera CA, Maldonado TS, Longaker MT, Gittes GK. Defective fibroblast growth factor signaling allows for nonbranching growth of the respiratory-derived fistula tract in esophageal atresia with tracheoesophageal fistula. J Pediatr Surg. 2000;35(10):1421–5. doi: 10.1053/jpsu.2000.16404. [DOI] [PubMed] [Google Scholar]
- (41).Crisera CA, Connelly PR, Marmureanu AR, Li M, Rose MI, Longaker MT, Gittes GK. TTF-1 and HNF-3beta in the developing tracheoesophageal fistula: further evidence for the respiratory origin of the distal esophagus’. J Pediatr Surg. 1999;34(9):1322–6. doi: 10.1016/s0022-3468(99)90003-9. [DOI] [PubMed] [Google Scholar]
- (42).Spilde TL, Bhatia AM, Marosky JK, Preuett B, Kobayashi H, Hembree MJ, Prasadan K, Daume E, Snyder CL, Gittes GK. Fibroblast growth factor signaling in the developing tracheoesophageal fistula. J Pediatr Surg. 2003 Mar;38(3):474–7. doi: 10.1053/jpsu.2003.50082. [DOI] [PubMed] [Google Scholar]
- (43).Crisera CA, Grau JB, Maldonado TS, Kadison AS, Longaker MT, Gittes GK. Defective epithelial-mesenchymal interactions dictate the organogenesis of tracheoesophageal fistula. Pediatric Surg Int. 2000;16(4):256–61. doi: 10.1007/s003830050740. [DOI] [PubMed] [Google Scholar]
- (44).Arsic D, Keenan J, Quan QB, Beasley S. Differences in the levels of Sonic hedgehog protein during early foregut development caused by exposure to Adriamycin give clues to the role of the Shh gene in oesophageal atresia. Pediatr Surg Int. 2003 Aug;19(6):463–6. doi: 10.1007/s00383-003-0959-8. [DOI] [PubMed] [Google Scholar]
- (45).Spilde TL, Bhatia AM, Mehta S, Ostlie DJ, Hembree MJ, Preuett BL, Prasadan K, Li ZX, Snyder CL, Gittes GK. Defective sonic hedgehog signaling in esophageal atresia with tracheoesophageal fistula. Surgery. 2003 Aug;134:345–50. doi: 10.1067/msy.2003.243. [DOI] [PubMed] [Google Scholar]
- (46).Spilde T, Bhatia A, Ostlie D, Marosky J, Holcomb G, III, Snyder C, Gittes G. A role for sonic hedgehog signaling in the pathogenesis of human tracheoesophageal fistula. J Pediatr Surg. 2003 Mar;38:465–8. doi: 10.1053/jpsu.2003.50080. [DOI] [PubMed] [Google Scholar]
- (47).Possoegel AK, Diez-Pardo JA, Morales C, Tovar JA. Notochord involvement in experimental esophageal atresia. Pediatr Surg Int. 1999;15(3-4):201–5. doi: 10.1007/s003830050555. [DOI] [PubMed] [Google Scholar]
- (48).Gillick J, Mooney E, Giles S, Bannigan J, Puri P. Notochord anomalies in the adriamycin rat model: A morphologic and molecular basis for the VACTERL association. J Pediatr Surg. 2003 Mar;38:469–73. doi: 10.1053/jpsu.2003.50081. [DOI] [PubMed] [Google Scholar]
- (49).Merei JM. Notochord-gut failure of detachment and intestinal atresia. Pediatr Surg Int. 2004 Jun;20(6):439–43. doi: 10.1007/s00383-004-1172-0. [DOI] [PubMed] [Google Scholar]
- (50).Williams AK, Qi BQ, Beasley SW. Demonstration of abnormal notochord development by three-dimensional reconstructive imaging in the rat model of esophageal atresia. Pediatr Surg Int. 2001;17(1):21–4. doi: 10.1007/s003830000440. [DOI] [PubMed] [Google Scholar]
- (51).Vleesch D,V, Quan QB, Beasley SW, Williams A. Abnormal branching and regression of the notochord and its relationship to foregut abnormalities. Eur J Pediatr Surg. 2002 Apr;12(2):83–9. doi: 10.1055/s-2002-30168. [DOI] [PubMed] [Google Scholar]
- (52).Kim SK, Hebrok M, Melton DA. Pancreas development in the chick embryo. Cold Spring Harbor Symp Quant Biol. 1997;62:377–83. [PubMed] [Google Scholar]
- (53).Dawrant MJ, Giles S, Bannigan J, Puri P. Abnormal separation of the respiratory primordium in the adriamycin mouse model of tracheoesophageal malformations. J Pediatr Surg. 2007 Feb;42(2):375–80. doi: 10.1016/j.jpedsurg.2006.10.011. [DOI] [PubMed] [Google Scholar]
- (54).Litingtung Y, Lei L, Westphal H, Chiang C. Sonic hedgehog is essential to foregut development. Nature Genet. 1998;20(1):58–61. doi: 10.1038/1717. [DOI] [PubMed] [Google Scholar]
- (55).Pepicelli CV, Lewis PM, McMahon AP. Sonic hedgehog regulates branching morphogenesis in the mammalian lung. Curr Biol. 1998 Sep 24;8(19):1083–6. doi: 10.1016/s0960-9822(98)70446-4. [DOI] [PubMed] [Google Scholar]
- (56).Kim PC, Mo R, Hui CC. Murine models of VACTERL syndrome: Role of sonic hedgehog signaling pathway. J Pediatr Surg. 2001 Feb;36(2):381–4. doi: 10.1053/jpsu.2001.20722. [DOI] [PubMed] [Google Scholar]
- (57).Mahlapuu M, Enerbäck S, Carlsson P. Haploinsufficiency of the forkhead gene Foxf1, a target for sonic hedgehog signaling, causes lung and foregut malformations. Development. 2001;128(12):2397–406. doi: 10.1242/dev.128.12.2397. [DOI] [PubMed] [Google Scholar]
- (58).Yuan BB, Li CG, Kimura S, Engelhardt RT, Smith BR, Minoo P. Inhibition of distal lung morphogenesis in Nkx2.1 (−/−) embryos. Dev Dyn. 2000;217(2):180–90. doi: 10.1002/(SICI)1097-0177(200002)217:2<180::AID-DVDY5>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- (59).Johnston JJ, Olivos-Glander I, Killoran C, Elson E, Turner JT, Peters KF, Abbott MH, Aughton DJ, Aylsworth AS, Bamshad MJ, Booth C, Curry CJ, David A, Dinulos MB, Flannery DB, Fox MA, Graham JM, Grange DK, Guttmacher AE, Hannibal MC, Henn W, Hennekam RC, Holmes LB, Hoyme HE, Leppig KA, Lin AE, Macleod P, Manchester DK, Marcelis C, Mazzanti L, McCann E, McDonald MT, Mendelsohn NJ, Moeschler JB, Moghaddam B, Neri G, Newbury-Ecob R, Pagon RA, Phillips JA, Sadler LS, Stoler JM, Tilstra D, Walsh Vockley CM, Zackai EH, Zadeh TM, Brueton L, Black GC, Biesecker LG. Molecular and clinical analyses of Greig cephalopolysyndactyly and Pallister-Hall syndromes: robust phenotype prediction from the type and position of GLI3 mutations. Am J Hum Genet. 2005 Apr;76(4):609–22. doi: 10.1086/429346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (60).Boulet AM, Capecchi MR. Targeted disruption of hoxc-4 causes esophageal defects and vertebral transformations. Dev Biol. 1996;177:232–49. doi: 10.1006/dbio.1996.0159. [DOI] [PubMed] [Google Scholar]
- (61).Mendelsohn C, Lohnes D, Décimo D, Lufkin T, LeMeur M, Chambon P, Mark M. Function of the retinoic acid receptors (RARs) during development. (II) Multiple abnormalities at various stages of organogenesis in RAR double mutants. Development. 1994;120:2749–71. doi: 10.1242/dev.120.10.2749. [DOI] [PubMed] [Google Scholar]
- (62).Vissers LE, van Ravenswaaij CM, Admiraal R, Hurst JA, de Vries BB, Janssen IM, van der Vliet WA, Huys EH, De Jong PJ, Hamel BC, Schoenmakers EF, Brunner HG, Veltman JA, Van Kessel AG. Mutations in a new member of the chromodomain gene family cause CHARGE syndrome. Nature Genet. 2004 Sep;36(9):955–7. doi: 10.1038/ng1407. [DOI] [PubMed] [Google Scholar]
- (63).Van Bokhoven H, Celli J, van Reeuwijk J, Rinne T, Glaudemans B, van Beusekom E, Rieu P, Newbury-Ecob RA, Chiang C, Brunner HG. MYCN haploinsufficiency is associated with reduced brain size and intestinal atresias in Feingold syndrome. Nature Genet. 2005 May;37(5):465–7. doi: 10.1038/ng1546. [DOI] [PubMed] [Google Scholar]
- (64).Cox PM, Gibson RA, Morgan N, Brueton LA. VACTERL with hydrocephalus in twins due to Fanconi anemia (FA): mutation in the FAC gene. Am J Med Genet. 1997 Jan 10;68(1):86–90. [PubMed] [Google Scholar]
- (65).Williamson KA, Hever AM, Rainger J, Rogers RC, Magee A, Fiedler Z, Keng WT, Sharkey FH, McGill N, Hill CJ, Schneider A, Messina M, Turnpenny PD, Fantes JA, van H,V, Fitzpatrick DR. Mutations in SOX2 cause anophthalmia-esophageal-genital (AEG) syndrome. Hum Mol Genet. 2006 May 1;15(9):1413–22. doi: 10.1093/hmg/ddl064. [DOI] [PubMed] [Google Scholar]
- (66).De FF, Cainarca S, Andolfi G, Ferrentino R, Berti C, Rodriguez CG, Rittinger O, Dennis N, Odent S, Rastogi A, Liebelt J, Chitayat D, Winter R, Jawanda H, Ballabio A, Franco B, Meroni G. X-linked Opitz syndrome: novel mutations in the MID1 gene and redefinition of the clinical spectrum. Am J Med Genet A. 2003 Jul 15;120(2):222–8. doi: 10.1002/ajmg.a.10265. [DOI] [PubMed] [Google Scholar]
- (67).Depaepe A, Dolk H, Lechat MF. The epidemiology of tracheo-oesophageal fistula and oesophageal atresia in Europe. EUROCAT Working Group. Arch Dis Child. 1993 Jun;68(6):743–8. doi: 10.1136/adc.68.6.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (68).Entezami M, Coumbos A, Runkel S, Vogel M, Wegner R. Combined partial trisomy 3p/monosomy 5p resulting in sonographic abnormalities. Clin Genet. 1997 Aug;52(2):96–9. doi: 10.1111/j.1399-0004.1997.tb02525.x. [DOI] [PubMed] [Google Scholar]
- (69).Schroeder HW, Jr., Forbes S, Mack L, Davis S, Norwood TH. Recombination aneusomy of chromosome 5 associated with multiple severe congenital malformations. Clin Genet. 1986 Oct;30(4):285–92. doi: 10.1111/j.1399-0004.1986.tb00608.x. [DOI] [PubMed] [Google Scholar]
- (70).Walsh LE, Vance GH, Weaver DD. Distal 13q Deletion Syndrome and the VACTERL association: case report, literature review, and possible implications. Am J Med Genet. 2001 Jan 15;98(2):137–44. doi: 10.1002/1096-8628(20010115)98:2<137::aid-ajmg1022>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- (71).Marsh AJ, Wellesley D, Burge D, Ashton M, Browne CE, Dennis NR, Temple IK. Interstitial deletion of chromosome 17 (del(17)(q22q23.3)) confirms a link with oesophageal atresia. J Med Genet. 2000;37(9):701–4. doi: 10.1136/jmg.37.9.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (72).Digilio MC, Marino B, Bagolan P, Giannotti A, Dallapiccola B. Microdeletion 22q11 and oesophageal atresia. J Med Genet. 1999 Feb;36(2):137–9. [PMC free article] [PubMed] [Google Scholar]