Abstract
Background
Race and socioeconomic disparities are pervasive and persist throughout our health care system. Inequities have also been identified in outcomes after trauma despite its immediate nature and the perceived equal access to emergent care.
Objectives
Our objective was to systematically evaluate the current literature on the association between trauma mortality and race, insurance status, and socioeconomic status. Our secondary objective was to assess data investigating potential mechanisms underlying these outcome disparities.
Methods
We performed a systematic review and random effects meta-analysis to examine the relationship between trauma and race, insurance, and socioeconomic disparities published between April 1990 and October 2011. The Cochrane Review Handbook and the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) statement were used as guides.
Results
Thirty-five studies were included in the final review. The current body of literature indicates that uninsured status is an independent negative predictor of trauma outcomes. Our meta-analysis corroborated this by demonstrating that uninsured patients were more likely to die than privately insured patients (OR 2.17 95% CI 1.51–3.11). Racial disparities in trauma outcomes are shown to be present and independent for black patients compared to whites. Our meta-analysis demonstrated that black race was associated with higher odds of death when compared with white race (OR 1.19 95% CI 1.09 – 1.31). Studies comparing Hispanic and white non-Hispanic patients’ post-trauma mortality outcomes, however, have provided conflicting results. Our meta-analysis found no significant difference in mortality comparing Hispanic patients with white patients (OR 1.08 95% CI 0.99–1.18)
Conclusions
Both race/ethnicity and insurance are clearly associated with disparate outcomes following trauma. These disparities are likely due to myriad factors across the trauma continuum of care: host factors, prehospital factors, hospital/provider factors, and factors associated with postacute care and rehabilitation. While there are many proposed mechanisms, we believe that there are several interventions that could be particularly effective in combatting trauma disparities. These include trauma prevention programs targeting vulnerable populations, expansion of healthcare coverage, relocation of trauma centers to better provide for vulnerable populations, and restructuring clinical training to address implicit biases. While much work still remains to fully elucidate the mechanisms underlying trauma disparities, we can and should now act to begin to reduce or eliminate these disparities that still plague our healthcare system.
Level of Evidence
Two.
BACKGROUND
Disparities in health outcomes have been uncovered for many conditions. Data indicate that black patients currently have higher mortality than white patients for nine of the leading 15 causes of death. The life expectancy gap between black patients and white patients persists, though it has gradually improved from 7.1 years in 1989 to less than 5.0 years in 2009.1
Recent research suggests patients from minority groups have higher mortality than white patients following trauma. This was surprising to some, as trauma was thought to be immune to disparities given its emergent nature and apparent universal access to care for it. Therefore, an in-depth review of currently published literature on this topic is warranted. Studies have also shown that disparities in trauma are associated with insurance coverage and socioeconomic status (SES). Understanding the relationship between disparities based on race, insurance status, and SES may help to elucidate the mechanisms leading to these disparities. Moreover, by assessing the literature regarding disparities in the context of the continuum of care, a better understanding of possible interventions addressing these mechanisms can be obtained.
OBJECTIVES
The objective of this review is to critically assess and summarize trauma outcome disparities by race, insurance, and SES and to determine if racial disparities are independent of insurance and SES. The objective of the meta-analysis is to determine whether mortality amongst trauma patients in the United States is associated with differences in patients’ race and/or insurance coverage.
METHODS
Search Strategy
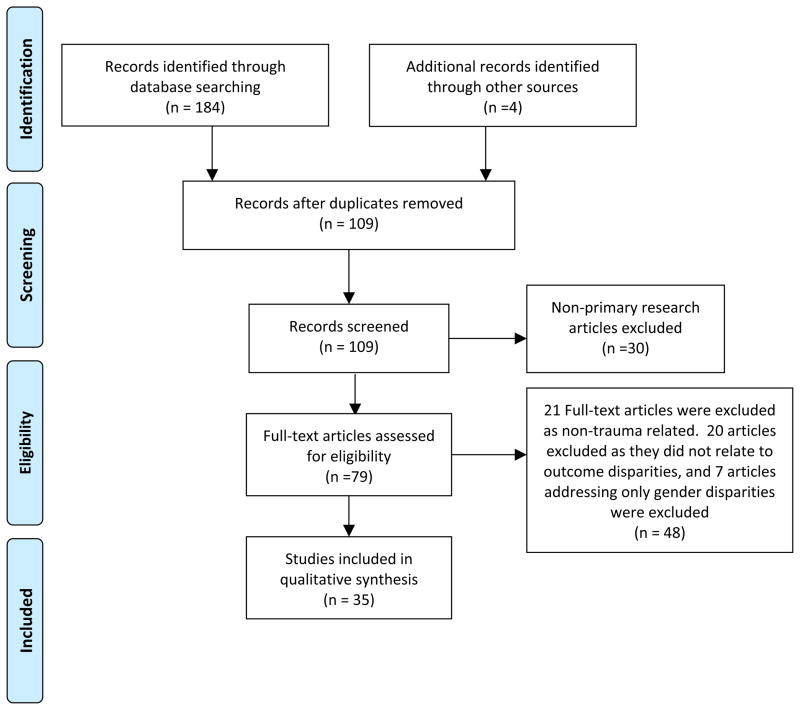
Using the Cochrane Handbook, the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) statement, and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement as guides, we created a study protocol (see Supplement A). Accordingly, we searched PubMed and Embase for articles published between April 1990 and October 2011. Our search strategy is detailed in our study protocol, and the search process and study selection are detailed in Figure 1.
Figure 1.
Flow diagram of search process and study selection as suggested by the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA).5
Analyses
We performed double data extraction and risk of bias assessment for all studies included in the meta-analysis. Articles were evaluated for variables tested, data quality, and statistical compatibility. Meta-analyses were carried out only on those studies that provided information on race or insurance. Sttudies with the same effect measure can be combined; therefore, only studies providing odds ratios and confidence intervals or standard errors were included. In cases where study populations were likely to be overlapping, larger or higher-quality studies were selected for inclusion in meta-analysis. Studies were evaluated using a random-effects model to account for heterogeneity between the studies, which was evaluated using I2. Forest plots were generated to evaluate relevant subgroups and sensitivity analyses. A p-value of <0.05 was chosen a priori as indication of statistical significance. Statistical analysis was performed using Stata 12.1 (Statacorp, College Station, TX)
RESULTS
We identified 35 articles that qualified for inclusion in the systematic review (see Table 1 for characteristics). Ten studies were eliminated from the meta-analysis due to insufficient mortality data.2–11 We also eliminated eight studies for statistical incompatibility.12–19
Table 1.
Annotated Bibliography of Trauma Outcome Disparity Research
| Lead Author | Title | Study Design | Study Characteristics |
|---|---|---|---|
| Arango- Lasprilla 2007 | Traumatic brain injury and functional outcomes: does minority status matter? | Retrospective Cross- sectional | Outcome of interest: rehabilitation characteristics and functional outcomes Years: 1989–2004 Data source: TBI Model Systems database Age requirements: none Adjusted variables: ethnicity, age, level of education, injury severity, functional status at rehab admission, functional status 1 year later, Community integration, and GOS-E |
| Arango- Lasprilla 2007 | Functional outcomes from inpatient rehabilitation after traumatic brain injury: how do Hispanics fare? | Retrospective Cross- sectional | Outcome of interest: Rehabilitation placement Years: 1989–2003 Data source: TBI Model Systems database Age requirements: >16 Adjusted variables: ethnicity, age, length of posttraumatic amnesia, injury severity, functional outcome scores, and preinjury education |
| Arthur 2008 | Racial disparities in mortality among adults hospitalized after injury | Retrospective Cross- sectional | Outcome of interest: in-hospital mortality Years: 1998–2002 Data source: HCUP Age requirements: 18–64 Adjusted variables: age, race, gender, comorbid conditions, injury severity, primary payer, median income of zip code of residence, hospital type |
| Bowman 2007 | Racial disparities in outcomes of persons with moderate to severe traumatic brain injury | Retrospective Cross- sectional | Outcome of interest: TBI mortality Years: 2000–2003 Data source: NTDB Age requirements: none Adjusted variables: payer type, spinal cord injury, hypotension, comorbidities, age, gender, GCS, injury type, injury intent, injury severity, hospital volume of TBI, trauma designation |
| Crompton 2010 | Racial disparities in motorcycle-related mortality: an analysis of the National Trauma Data Bank | Retrospective Cross- sectional | Outcome of interest: Motorcycle crash in- hospital mortality Years: 2002–2006 Data source: NTDB Age requirements: >18 Adjusted variables: age, sex, insurance status, year, helmet use, injury severity characteristics |
| Downing 2011 | The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? | Retrospective Cross- sectional | Outcome of interest: mortality Years: 2002–2006 Data source: NTDB Age requirements: 19–30 Adjusted variables: age, ethnicity, gender, history of substance abuse, mechanism of injury, injury severity, shock, complications, teaching status of hospital |
| Englum 2011 | Racial, Ethnic, and Insurance Status Disparities in Use of Posthospitalization Care after Trauma | Retrospective Cross- sectional | Outcome of interest: Discharge to posthospitalization facilities by race and insurance status Years: 2007 Data source: NTDB Age requirements: 18–64 Adjusted variables: age, sex, ISS, presence of shock, GCS-motor, mechanism of injury, type of injury, intention of injury, presence of severe head/extremity injury, trauma level designation, and length of hospital stay. |
| Falcone 2007 | Disparities in child abuse mortality are not explained by injury severity | Retrospective Cross- sectional | Outcome of interest: child abuse mortality Years: 1995–2004 Data source: Cincinnati Children’s Hospital Database Age requirements: <16 Adjusted variables: Race, age, GCS, injury severity, pulse, blood pressure, respiratory rate, insurance |
| Falcone 2008 | Despite overall low pediatric head injury mortality, disparities exist between races | Retrospective Cross- sectional | Outcome of interest: mortality Years: 2000–2004 Data source: NTDB and Cincinnati Children’s Hospital Database Age requirements: <16 Adjusted variables: sex, ethnicity, ISS, pulse, blood pressure, respiratory rate, GCS, number of injuries, insurance status, disposition, LOS |
| Gannon 2002 | A statewide population-based study of gender differences in trauma: validation of a prior single- institution study | Prospective Cohort | Outcome of interest: hospital mortality Years: 1996–1997 Data source: Pennsylvania trauma centers database Age requirements: 18–64 Adjusted variables: sex, ethnicity, respiratory rate, blood pressure, RTS, injury type, history of cardiac disease, cancer, immune diseases, or DM |
| Greene 2010 | Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma | Retrospective Cross- sectional | Outcome of interest: Blunt trauma mortality Years: 2002–2006 Data source: NTDB Age requirements: <65 Adjusted variables: insurance status, mechanism of injury, age, race, sex, injury severity, shock head injury, extremity injury, hospital teaching status, year |
| Haas 1994 | Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status | Retrospective Cross- sectional | Outcome of interest: resource use and mortality Years: 1990 Data source: Institutional data results Age requirements: 15–64 Adjusted variables: age, sex, race, injury severity, comorbidity |
| Haider 2011 | Association Between Hospitals Caring for a Disproportionately High Percentage of Minority Trauma Patients and Increased Mortality | Retrospective Cohort | Outcome of interest: mortality Years: 2007–2008 Data source: NTDB Age requirements: 18–64 Adjusted variables: age, sex, insurance status, injury severity score, presence of hypotension, presence of severe head and/or extremity injury, mechanism of injury. |
| Haider 2008 | Race and insurance status as risk factors for trauma mortality | Retrospective Cross- sectional | Outcome of interest: in hospital mortality Years: 2001–2005 Data source: NTDB Age requirements: 18–64 Adjusted variables: age, sex, injury severity, RTS, severe extremity injury, type of injury, mechanism of injury |
| Haider 2007 | Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry | Retrospective Cross- sectional | Outcome of interest: TBI mortality Years: 1996–2001 Data source: NTDB Age requirements: 2–16 Adjusted variables: severity of head injury, anatomic injury, and physiologic injury, intent of injury, type of injury, mechanism of injury, age, sex, comorbidities, severe extremity injury |
| Hakmeh 2010 | Effect of race and insurance on outcome of pediatric trauma | Retrospective Cross- sectional | Outcome of interest: moderate to severe injury mortality Years: 2000–2005 Data source: NTDB Age requirements: ≤17 Adjusted variables: race, insurance status, injury type, injury severity |
| Krause 2006 | Racial disparities in health outcomes after spinal cord injury: mediating effects of education and income | Retrospective Cross- sectional | Outcome of interest: spinal cord injury outcomes disparities Years: not stated Data source: hospital records Age requirements: >18 Adjusted variables: race, gender, quality of life variables, utilization of services |
| Leukhardt 2010 | Follow-up disparities after trauma: a real problem for outcomes research | Retrospective Cross- sectional | Outcome of interest: follow-up after trauma Years: 2000–2005 Data source: Institutional records, trauma registry, NDI, census Age requirements: none Adjusted variables: age, sex, race, disposition, discharge zip code, length of stay, penetrating trauma, ISS, spinal cord injury, head ISS>3, death after discharge. |
| Martin 2010 | Severity of head computed tomography scan findings fail to explain racial differences in mortality following child abuse | Retrospective Cross- sectional | Outcome of interest: non-accidental trauma mortality Years: 1994–2004 Data source: Institutional database Age requirements: ≤16 Adjusted variables: race, injury severity, others not specified. |
| Maybury 2010 | Pedestrians struck by motor vehicles further worsen race-and insurance-based disparities in trauma outcomes: the case for inner- city pedestrian injury prevention programs | Retrospective Cross- sectional | Outcome of interest: Pedestrian accident mortality Years: 2002–2006 Data source: NTDB Age requirements: 16–64 Adjusted variables: sex, age, injury severity, shock, severe head injury, severe extremity injury, hospital teaching status, year of admission |
| Millham 2009 | Are there racial disparities in trauma care? | Retrospective Cross- sectional | Outcome of interest: Gun shot wound, MVC mortality Years: 2001–2005 Data source: NTDB Age requirements:>14 Adjusted variables: age, gender, blood pressure, geographic region, hospital teaching status, trauma center status |
| Nirula 2009 | Inequity of rehabilitation services after trauma injury | Retrospective Cohort | Outcome of interest: discharge to rehabilitation facility Years: 2000–2004 Data source: NTDB Age requirements: none (subgroup analysis for <65) Adjusted variables: age, sex, race, payer, comorbidities, drug or alcohol use, ISS, systolic blood pressure, GCS, AIS |
| Oyetunji 2010 | Multiple imputation in Trauma Disparity Research | Retrospective Cross- sectional | Outcome of interest: multiple imputation analysis in trauma Years: 2002–2006 Data source: NTDB Age requirements: Age ≥18 Adjusted variables: age, gender, anatomic and physiologic injury severity, severe head and extremity injury |
| Rangel 2010 | Socioeconomic disparities in infant mortalityafter nonaccidental trauma: a multicenter study | Retrospective Cross- sectional | Outcome of interest: non-accidental trauma mortality Years: 2000–2004 Data source: multiple institutional databases Age requirements:<1 Adjusted variables: race, insurance status, injury severity, head injury severity |
| Rosen 2009 | Downwardly mobile: the accidental cost of being uninsured | Retrospective Cross- sectional | Outcome of interest: mortality Years: 2002–2006 Data source: NTDB Age requirements: ≥18 Adjusted variables: sex, race, age, injury severity, RTS, trauma center level, mechanism of injury |
| Rosen 2009 | Lack of insurance negatively affects trauma mortality in US children | Retrospective Cross- sectional | Outcome of interest: mortality Years: 2002–2006 Data source: NTDB Age requirements: ≥16 Adjusted variables: race, injury severity, sex, injury type |
| Sacks 2011 | Insurance status and hospital discharge disposition after trauma: inequities in access to postacute care | Retrospective Cohort | Outcome of interest: disposition to a specialized postacute care facility Years: 2002–2006 Data source: NTDB Age requirements: ≥18 Adjusted variables: Age, sex, ISS, race/ethnicity, mechanism of injury. |
| Salim 2010 | Does insurance status matter at a public, level I trauma center? | Retrospective Cross- sectional | Outcome of interest: trauma mortality Years: 1998–2005 Data source: Institutional database Age requirements: ≥18 Adjusted variables: sex, age, injury type, blood pressure, GCS, toxicology, injury severity, AIS |
| Shafi 2007 | Ethnic disparities exist in trauma care | Retrospective Cross- sectional | Outcome of interest: TBI mortality Years: 2004 Data source: NTDB Age requirements: none Adjusted variables: age, sex, injury severity, AIS, GCS, associate injuries, insurance status |
| Shafi 2008 | Ethnic disparities in initial management of trauma patients in a nationwide sample of emergency department visits | Retrospective Cross- sectional | Outcome of interest: intensity of ED assessment and management and discharge disposition Years: 2003 Data source: National Hospital Ambulatory Medical Care Survey Age requirements: ≤15 Adjusted variables: not explicitly stated |
| Shafi 2007 | Racial disparities in long-term functional outcome after traumatic brain injury | Retrospective Cross- sectional | Outcome of interest: functional outcomes among TBI patients Years: 1998–2005 Data source: Institutional data Age requirements: ≤14 Adjusted variables: age, sex, injury severity, AIS, GCS, disposition, insurance status |
| Staudenmayer 2007 | Ethnic disparities in long-term functional outcomesafter traumatic brain injury | Prospective Cohort | Outcome of interest: functional outcomes among TBI patients Years: 1998–2005 Data source: Institutional data Age requirements: ≤14 Adjusted variables: age, sex, GCS, AIS, injury severity |
| Tepas 2011 | Insurance status, not race, is a determinant of outcomes from vehicular injury | Retrospective Cross- sectional | Outcome of interest: MVC victim mortality Years: 2008–2009 Data source: Florida Healthcare Administration Database Age requirements: none Adjusted variables: age, sex, ethnicity, insurance status, ICISS, comorbidities, severity, TBI, spinal cord injury, torso injury, vascular injury |
| Vettukattil 2011 | Do trauma safety- net hospitals deliver truly safe trauma care? A multilevel analysis of the national trauma data bank | Retrospective Cross- sectional | Outcome of interest: mortality Years: 2001–2005 Data source: NTDB Age requirements: 18–64 Adjusted variables: age, sex, insurance, injury severity, shock, type and mechanism of injury |
| Wood 2010 | Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury | Retrospective Cross- sectional | Outcome of interest: diagnosis of abuse in TBI infants Years: 2004–2008 Data source: Pediatric Health Information System Age requirements:<1 Adjusted variables: unclear |
Disparities by Insurance Status
Of fourteen studies that assessed the impact of insurance status on trauma outcomes, thirteen12,14,15,20–29 conclude that uninsured trauma patients had higher mortality rates than insured patients while one study8 found they had worse long-term functional outcomes. This finding was consistent among studies of the National Trauma Data Bank (NTDB), in regional studies, and in single-institution studies.20–22,28,29 The finding also held across studies of both adults and pediatric patients,15,23 independent of injury type.28 Vettukattil et al suggest that patients treated at safety-net hospitals do not suffer an increased burden of mortality, despite the fact that they treat a higher burden of uninsured patients.19 While the definition of insurance differed among studies, consistency in conclusions suggests this variation is unlikely to affect overall results.
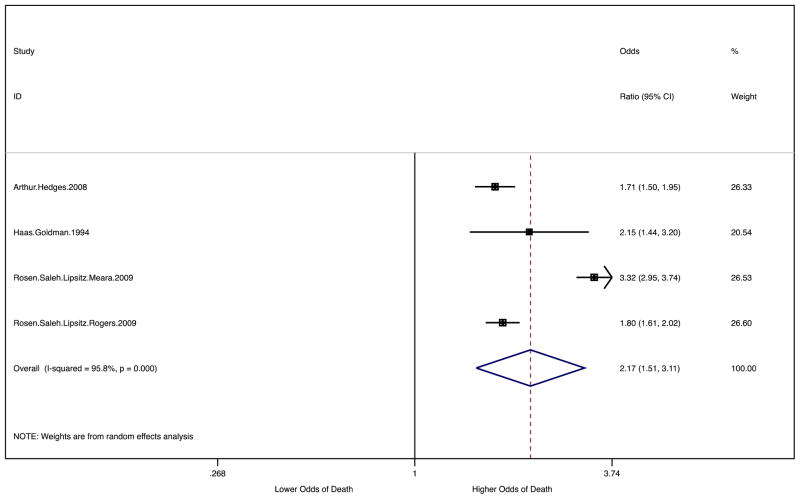
For the meta-analysis, only those studies that were statistically compatible and which provided mortality data were eligible.20–29 These studies categorized insurance in various ways; however, the majority of comparisons analyzed insured versus uninsured patients and private versus uninsured patients. There were insufficient non-overlapping studies to allow for meta-analysis comparing insured and uninsured patients. Of the ten eligible studies, two20,22 did not compare privately insured patients to uninsured patients, four studies24–26,28 overlapped with larger studies,27,29. Our meta-analysis demonstrates that uninsured patients were more likely than privately insured patients to die after trauma (OR 2.17 95% CI 1.51– 3.11) (Figure 2).
Figure 2.
Random effects meta-analysis of mortality for uninsured and privately insured patients. Pooled odds ratio 2.17 (95% CI 1.51, 3.11) for uninsured patients compared to privately insured patients.
Differences in interventions may be related to disparities in trauma outcomes. In a statewide study in Massachusetts, uninsured trauma patients were less likely than the privately insured to undergo an operative procedure (OR 0.68, 95% CI 0.63–0.74) or physical therapy (OR 0.61, 95% CI 0.57–0.67).21 Wood et al17 showed that uninsured more likely than the insured patients to receive skeletal surveys to uncover suspected child abuse, though, child abuse or positive skeletal surveys were more common among whites in this study.
Disparities by Socioeconomic Status
Two studies15,23 assess outcome disparities by SES, both of which conclude that median income of the patient’s home address is a predictor of higher trauma mortality rates. In a small study on infant mortality following non-accidental trauma by Rangel and colleagues,15 median income was divided into quartiles and compared to the highest earning quartile (Q4). Each of the lower three quartiles were found to have significantly higher odds of mortality (Q1 OR: 6.75, p= 0.0008; Q2 OR: 5.58, p=0.003; Q3 OR: 5.64, p=0.007). Similarly, a large retrospective study of adults hospitalized after injury by Arthur et al23 showed that a median income of patient’s home zip code below $45,000 was a predictor of higher mortality rates. This was highest for a median income below $25,000, the lowest income bracket (OR 1.32, 95% CI 1.14–1.53).
Disparities by Race
Overall, data show that minority patients have worse trauma outcomes than white patients. Twenty-four studies2,3,8,9,12,14–16,20,22–36 assess outcome disparities between racial groups; the majority focus on mortality as the outcome, and five focus on post-trauma functional outcomes. Of those, four2,3,9,30 show that minority patients have worse functional outcomes and one8 found no significant difference by race. Another study went beyond comparing outcomes between racial groups and found that patients treated in hospitals with higher percentages of minority patients had significantly increased odds of mortality compared with hospitals treating primarily white patients. 13
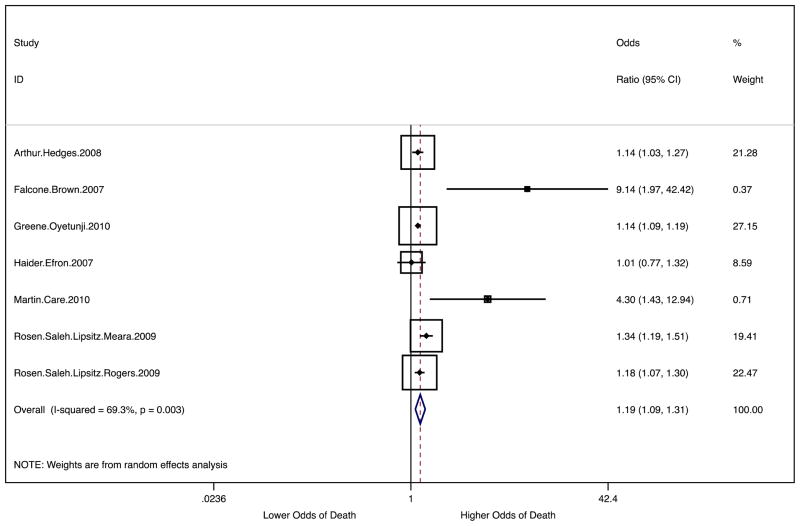
Similar to our qualitative review, our meta-analysis demonstrates that black patients have worse trauma mortality rates than white patients. Of the 24 studies in the qualitative analysis, 14 were eligible for meta-analysis,20,22–25,27–32,34–36 one study was eliminated from the analysis because it did not provide data for specific races.31 Another study was eliminated because it did not provide ORs comparing minority races to the reference group.22 Five studies24,25,28,32,36 were eliminated because they overlapped with larger studies.27,29 Our meta-analysis showed that black patients have worse trauma mortality rates than white patients (OR 1.19 95% CI 1.09–1.31) (Figure 3).
Figure 3.
Random effects meta-analysis of mortality for black and white patients. Pooled odds ratio 1.19 (95% CI 1.09, 1.31) for black patients compared to white patients.
Findings vary when all non-white patients are combined into a single group. Of those, Downing et al12 and Gannon et al31 found that non-white race was a significant predictor of mortality while three other studies15,16,22 found no significant difference. However, there were insufficient non-overlapping studies to perform a meta-analysis of non-white patients compared with white patients.
These conflicting results become clearer when considering each non-white cohort independently. Ten studies14,23–27,32–35 found that black patients have significantly higher post-trauma mortality than white patients, while only three studies22,24,30 found no significant difference between groups. In a retrospective cross-sectional analysis of the NTDB, Rosen et al27 found that black trauma patients had higher odds of death than white trauma patients after controlling for severity and patient characteristics including insurance status (OR 1.18 95% CI 1.07–1.29). Oyetunji and colleagues14 obtained similar results (OR 1.31, 95% CI 1.20–1.44). However, a retrospective single institution study of 29,829 trauma patients controlled for similar factors and found that no single race or ethnicity was a significant predictor of mortality.22
Outcome disparities for black patients held across several types of trauma as well. Most prominent are well-documented racial disparities in pediatric TBI patients.34,35 In a retrospective study comparing 3,111 pediatric head injury patients from the trauma database of Cincinnati Children’s Hospital Medical Center (CCHMC) to 13,363 patients in the National Trauma Database, Falcone et al34 found that, even after controlling for insurance, injury severity, and other factors, African-American children had a mortality odds ratio 3.1 times higher than that of white children (95% CI 1.2–7.8). In moderately and severely injured pediatric trauma patients in the NTDB, blacks had higher mortality rates than whites (OR 1.37, 95% CI 1.22–1.52), even after controlling for insurance status, injury severity, and other factors.26 While one study found no significant difference for in-hospital mortality; black pediatric TBI patients had significantly worse functional outcomes at discharge than white patients.30
In both of the studies that assessed Asian trauma outcomes, mortality rates were higher than whites. In a 2008 study of adults hospitalized after injury, using data from the Healthcare Cost and Utilization Project, odds of death were higher for Asian patients (OR 1.39 95% CI 1.06–183) and black patients (OR 1.14 1.03–1.27) compared to whites.24 Amongst patients with moderate to severe TBI, blacks and Asians each had higher odds of mortality than whites with odds ratios of (1.19 95% CI 1.02–1.39) and (1.41 95% CI 1.11–1.79) respectively. In addition to controlling for patient characteristics and injury severity, this study also used two proxies to control for SES: insurance status and median income by patient zip code.23
In the seven studies comparing Hispanic and white post-trauma mortality outcomes, the results are less clear. Three studies found that Hispanic patients have worse post-trauma mortality outcomes than whites,25,26,28 one found worse outcomes only associated with blunt mechanism,36 and three found no significant difference between groups.22,24,27 Using the NTDB, Rosen et al27 found no significant mortality difference between Hispanic and white trauma patients after controlling for severity and patient characteristics such as insurance status. By contrast, an analysis of 429,751 patients in the NTDB showed that Hispanic patients had higher adjusted odds of mortality than white patients (OR 1.47 95% CI 1.39–1.57).28 Milham et al36 found that Hispanic drivers in MVCs suffered higher mortality than white patients (OR 1.72, 95% CI 1.36–2.19) even after controlling for patient characteristics, presence of shock and treatment facility characteristics. Two additional studies showed that Hispanic patients fare worse as pedestrians in motor vehicle accidents as well as in moderately and severely injured pediatric trauma.25,26 Our meta-analysis, however, only demonstrated a trend toward a difference in mortality between Hispanic and white patients (OR 1.08 95% CI 0.99–1.18).
An additional concern considered by this review was initial treatment upon presentation to the Emergency Department. Some might suggest that differential initial assessment and management of minority patients might lead to the aforementioned disparities, yet Shafi et all found these factors do not differ between racial groups.10
Independence of Race Outcome Disparities
Because race and SES are correlated, it is important to decipher whether racial disparities are independent of socioeconomic disparities. The overwhelming majority of data show that black race is a predictor of higher trauma mortality independent of SES. Of the eight studies that compared black and white trauma patients while controlling for insurance status, seven14,25–27,32–34 showed that black race is an independent predictor of mortality while one study5 found no significant difference. Arthur et al23 conclude that black patients have higher mortality rates independent of both proxies for SES (insurance status and median income of patient zip code).
For Hispanic trauma outcomes, controlling for SES does not significantly add to the mixed results presented above. Of the studies that control for insurance status, two25,26 found that Hispanic patients had worse outcomes while two22,27 found no difference. Likewise, only one23 of the two studies24 assessing Asian trauma outcomes controlled for SES. While Asian race was an independent predictor of higher mortality rates using both proxies, further studies are needed to validate this finding. Though black race appears to be an independent predictor of mortality and results regarding other racial disparities are not clear, one study showed that insurance has a stronger predictive value on mortality than race,28 a finding echoed by two other recent studies.14,26
Disparities in Post-Acute Trauma Care and Rehabilitation
Disparities in post-acute care have also been well demonstrated.4,6,11,18 Millham and Jain36 found that black and Hispanic patients surviving gun shot wounds and motor vehicle accidents had a shorter length of stay than white patients (p<0.001). The study controlled for insurance, injury severity, and other patient and hospital characteristics. A large study of the NTDB found that black and Hispanic patients were less likely to be discharged to a rehabilitation center than white patients following moderate or severe traumatic brain injury with relative odds of 0.68, (95% CI 0.55–0.83) and 0.67 (95% CI 0.52–0.86).24 Despite some conflicting evidence,8 these results are confirmed by a comparable study of traumatic brain injury patients in the NTDB by Shafi and colleagues,7 as well as a study by Nirula et al,5 which showed evidence that race and insurance status are independent negative predictors in the likelihood of being transferred to a rehabilitation facility upon discharge. In a more recent study of the NTDB, Englum et al18 found that black and Hispanic patients were much less likely to be discharged to rehabilitation centers (RRR 0.61, 95% CI 0.56–0.66; RRR 0.44, 95% CI 0.40–0.49 respectively), which persisted when controlling for insurance status.
DISCUSSION
Trauma is considered an important frontier in disparities research because of apparent universal access and well-validated means of severity adjustment that allow for reasonable comparisons between groups.36 Despite these advantages, refining study variables and developing comparison groups that uncover existing disparities is still a work in progress. This review demonstrates the progress that has been made in refining the measurement of SES and addressing the heterogeneity of minority populations. Both of the studies that assessed SES outcome disparities using median income of the patient’s home address found clear evidence that SES is a predictor of higher trauma mortality rates. The apparent significance of this variable should encourage health disparities researchers to incorporate additional SES indicators. At the same time, researchers should continually push for more accurate and sensitive data, such as income, wealth and education data at the census tract level and occupation data on the individual patient level. Overall, studies that combine all minority patients into one cohort did not find evidence of inequalities. Departing from this binary approach, evidence of disparities becomes immediately evident for black and Asian trauma patients. While outcome disparities were less clear for Hispanic patients, the large heterogeneity in length of years in the U.S. and English proficiency of the U.S. Hispanic population may mask inequalities suffered by segments of this population. Disparities in Hispanic patient outcomes may be ambiguous at a national level, but should be able to be unmasked through additional regional and subgroup studies.
Mechanisms of Disparities and Opportunities for Intervention
While trauma may provide universal access to some level of care, clear outcome disparities based on race, SES, and insurance status suggest that these inequalities are likely to have a systemic component. By assessing mechanisms of disparities within the context of the continuum of care (Figure 4), we can begin to understand the interplay of factors that contribute to disparate health outcomes. See Supplement B for an in-depth discussion of mechanisms of disparities within the continuum of trauma care as well as interventions we believe to be most prudent for reducing or eliminating those disparities. Firm elucidation of mechanisms underlying disparities is timely, as policy-makers have begun to seek and support interventions.
Figure 4.
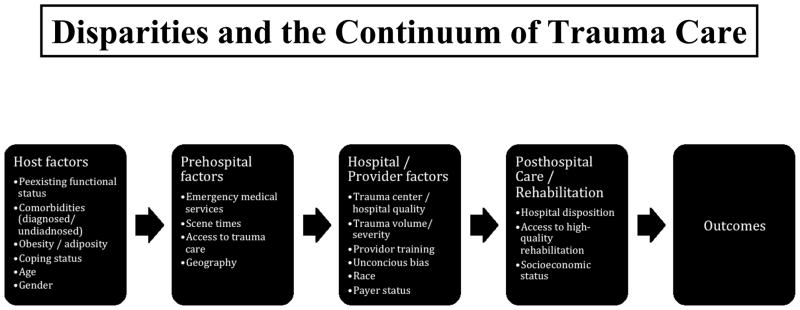
The continuum of trauma care: Factors identified in literature that are thought to impact outcome and lead to Disparities in Trauma Outcomes.
Limitations
This study is limited by the observational nature of the included articles and the inherent risks of selection bias and confounding associated with such studies. Many of the included articles assessed mortality following trauma, though it has been suggested that adjusted mortality may not be the best indicator of quality of trauma care.37 Future studies should assess quality of care using quality indicators, such as those proposed by the American College of Surgeons Committee on Trauma (ASCOT), which have been shown to correlate with outcomes.38 Moreover, it has been suggested that when assessing outcomes it is important to determine subtler measures of quality not currently included in the ASCOT quality indicators by assessing metrics such as failure to rescue, cost-effectiveness, and functional outcomes en lieu of “blunt,” measures such as mortality.39 Databases such as the NTDB represent convenience samples, leading to a risk of selection bias. However, the vast majority of trauma centers are now reporting to the NTDB and this database is thus becoming more representative of the general US population. Administrative databases are also limited in that they lack patient-level information necessary to employ ASCOT audit filters, or other metrics of quality.38 To address confounding, we performed an assessment of risk of bias and included effect measures from the most adjusted models in the meta-analysis. Even still, not all studies adjusted for the same variables, which likely led to increased inter-study heterogeneity. One limitation of the meta-analysis is that studies reported outcomes by different groups, thus limiting the numbers of comparisons we could make. Also many of the studies were published using the NTDB and because study populations overlapped, we were forced to eliminate many studies from the meta-analysis thus reducing our sample size. Future systematic reviews and meta-analysis should take care to assess risk of bias in included studies, attempt to reduce sources of bias and confounding, and avoid analyzing studies that investigate overlapping populations.
Conclusion
This study finds consistent evidence that disparities in trauma care and outcomes exist between privately insured patients and uninsured patients, with the bulk of the literature showing uninsured patients have worse outcomes regardless of the reference group. This study also finds significant disparities in outcomes between black and white patients, but we identified inconsistent evidence that these disparities in trauma care and outcomes also exist for Hispanic and Asian patients. Finally, we suggest that interventions should focus upon injury prevention, increasing access to care, encouraging growth in number of trauma centers serving vulnerable populations, and improvements in resident training.
Supplementary Material
Acknowledgments
SOURCES OF FUNDING
L. Cooper is supported by NHLBI grants K24HL083113 and P50HL0105187. A. Haider MD MPH received support from National Institutes of Health/NIGMS K23GM093112-01; American College of Surgeons C. James Carrico Fellowship for the study of Trauma and Critical Care and Hopkins Center for Health Disparities Solutions. P. Weygandt MPH received support from grant number 5TL1RR025007 from the National Center Research Resources to the Johns Hopkins University School of Medicine, which funds the Predoctoral Clinical Research Training Program.
The authors would like to thank Ariel Bowman for providing important input regarding issues of access in trauma care.
Footnotes
CONFLICTS OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Adil Haider: Study Design, Data Analysis, Data Interpretation, and Writing of the Manuscript
Jessica Bentley: Study Design, Data Interpretation, and Writing of the Manuscript
P Logan Weygandt: Study Design, Data Analysis, Data Interpretation, and Writing of the Manuscript
M Francesca Monn: Study Design, Data Analysis, Data Interpretation, Critical Review
Karim A Rehman: Study Design, Data Interpretation, and Writing of the Manuscript
Benjamin Zarzaur: Study Design, Data Interpretation, and Critical Review
Marie Crandall: Study Design, Data Interpretation, and Critical Review
Edward E Cornwell: Study Design, Data Interpretation, and Critical Review
Lisa A Cooper: Study Design, Data Interpretation, and Critical Review
References
- 1.Kochanek KD, Xu J, Murphy SL, Minino AM, Kung HC. Deaths: final data for 2009. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System. 2011;60(3):1–166. [PubMed] [Google Scholar]
- 2.Arango-Lasprilla JC, Rosenthal M, Deluca J, Cifu DX, Hanks R, Komaroff E. Functional outcomes from inpatient rehabilitation after traumatic brain injury: how do Hispanics fare? Archives of physical medicine and rehabilitation. 2007 Jan;88(1):11–18. doi: 10.1016/j.apmr.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Arango-Lasprilla JC, Rosenthal M, Deluca J, et al. Traumatic brain injury and functional outcomes: does minority status matter? Brain injury: [BI] 2007 Jun;21(7):701–708. doi: 10.1080/02699050701481597. [DOI] [PubMed] [Google Scholar]
- 4.Krause JS, Broderick LE, Saladin LK, Broyles J. Racial disparities in health outcomes after spinal cord injury: mediating effects of education and income. The journal of spinal cord medicine. 2006;29(1):17–25. doi: 10.1080/10790268.2006.11753852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nirula R, Nirula G, Gentilello LM. Inequity of rehabilitation services after traumatic injury. The Journal of trauma. 2009 Jan;66(1):255–259. doi: 10.1097/TA.0b013e31815ede46. [DOI] [PubMed] [Google Scholar]
- 6.Sacks GD, Hill C, Rogers SO., Jr Insurance status and hospital discharge disposition after trauma: inequities in access to postacute care. The Journal of trauma. 2011 Oct;71(4):1011–1015. doi: 10.1097/TA.0b013e3182092c27. [DOI] [PubMed] [Google Scholar]
- 7.Shafi S, de la Plata CM, Diaz-Arrastia R, et al. Ethnic disparities exist in trauma care. The Journal of trauma. 2007 Nov;63(5):1138–1142. doi: 10.1097/TA.0b013e3181568cd4. [DOI] [PubMed] [Google Scholar]
- 8.Shafi S, Marquez de la Plata C, Diaz-Arrastia R, et al. Racial disparities in long-term functional outcome after traumatic brain injury. The Journal of trauma. 2007 Dec;63(6):1263–1268. doi: 10.1097/TA.0b013e31815b8f00. discussion 1268–1270. [DOI] [PubMed] [Google Scholar]
- 9.Staudenmayer KL, Diaz-Arrastia R, de Oliveira A, Gentilello LM, Shafi S. Ethnic disparities in long-term functional outcomes after traumatic brain injury. The Journal of trauma. 2007 Dec;63(6):1364–1369. doi: 10.1097/TA.0b013e31815b897b. [DOI] [PubMed] [Google Scholar]
- 10.Shafi S, Gentilello LM. Ethnic disparities in initial management of trauma patients in a nationwide sample of emergency department visits. Archives of surgery (Chicago, Ill: 1960) 2008 Nov;143(11):1057–1061. doi: 10.1001/archsurg.143.11.1057. discussion 1061. [DOI] [PubMed] [Google Scholar]
- 11.Leukhardt WH, Golob JF, McCoy AM, Fadlalla AM, Malangoni MA, Claridge JA. Follow-up disparities after trauma: a real problem for outcomes research. American journal of surgery. 2010 Mar;199(3):348–352. doi: 10.1016/j.amjsurg.2009.09.021. discussion 353. [DOI] [PubMed] [Google Scholar]
- 12.Downing SR, Oyetunji TA, Greene WR, et al. The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? The Journal of trauma. 2011 Jan;70(1):130–134. doi: 10.1097/TA.0b013e3182032b34. discussion 134–135. [DOI] [PubMed] [Google Scholar]
- 13.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Archives of surgery (Chicago, Ill: 1960) 2012 Jan;147(1):63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oyetunji TA, Crompton JG, Ehanire ID, et al. Multiple imputation in trauma disparity research. The Journal of surgical research. 2011 Jan;165(1):e37–41. doi: 10.1016/j.jss.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 15.Rangel EL, Burd RS, Falcone RA., Jr Socioeconomic disparities in infant mortality after nonaccidental trauma: a multicenter study. The Journal of trauma. 2010 Jul;69(1):20–25. doi: 10.1097/TA.0b013e3181bbd7c3. [DOI] [PubMed] [Google Scholar]
- 16.Tepas JJ, 3rd, Pracht EE, Orban BL, Flint LM. Insurance status, not race, is a determinant of outcomes from vehicular injury. Journal of the American College of Surgeons. 2011 Apr;212(4):722–727. doi: 10.1016/j.jamcollsurg.2010.12.016. discussion 727–729. [DOI] [PubMed] [Google Scholar]
- 17.Wood JN, Hall M, Schilling S, Keren R, Mitra N, Rubin DM. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics. 2010 Sep;126(3):408–414. doi: 10.1542/peds.2010-0031. [DOI] [PubMed] [Google Scholar]
- 18.Englum BR, Villegas C, Bolorunduro O, et al. Racial, ethnic, and insurance status disparities in use of posthospitalization care after trauma. Journal of the American College of Surgeons. 2011 Dec;213(6):699–708. doi: 10.1016/j.jamcollsurg.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vettukattil AS, Haider AH, Haut ER, et al. Do trauma safety-net hospitals deliver truly safe trauma care? A multilevel analysis of the national trauma data bank. The Journal of trauma. 2011 Apr;70(4):978–984. doi: 10.1097/TA.0b013e31820b5d0c. [DOI] [PubMed] [Google Scholar]
- 20.Greene WR, Oyetunji TA, Bowers U, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. American journal of surgery. 2010 Apr;199(4):554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. American journal of public health. 1994 Oct;84(10):1605–1608. doi: 10.2105/ajph.84.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salim A, Ottochian M, DuBose J, et al. Does insurance status matter at a public, level I trauma center? The Journal of trauma. 2010 Jan;68(1):211–216. doi: 10.1097/TA.0b013e3181a0e659. [DOI] [PubMed] [Google Scholar]
- 23.Arthur M, Hedges JR, Newgard CD, Diggs BS, Mullins RJ. Racial disparities in mortality among adults hospitalized after injury. Medical care. 2008 Feb;46(2):192–199. doi: 10.1097/MLR.0b013e31815b9d8e. [DOI] [PubMed] [Google Scholar]
- 24.Bowman SM, Martin DP, Sharar SR, Zimmerman FJ. Racial disparities in outcomes of persons with moderate to severe traumatic brain injury. Medical care. 2007 Jul;45(7):686–690. doi: 10.1097/MLR.0b013e31803dcdf3. [DOI] [PubMed] [Google Scholar]
- 25.Maybury RS, Bolorunduro OB, Villegas C, et al. Pedestrians struck by motor vehicles further worsen race- and insurance-based disparities in trauma outcomes: the case for inner-city pedestrian injury prevention programs. Surgery. 2010 Aug;148(2):202–208. doi: 10.1016/j.surg.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 26.Hakmeh W, Barker J, Szpunar SM, Fox JM, Irvin CB. Effect of race and insurance on outcome of pediatric trauma. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine. 2010 Aug;17(8):809–812. doi: 10.1111/j.1553-2712.2010.00819.x. [DOI] [PubMed] [Google Scholar]
- 27.Rosen H, Saleh F, Lipsitz S, Rogers SO, Jr, Gawande AA. Downwardly mobile: the accidental cost of being uninsured. Archives of surgery (Chicago, Ill: 1960) 2009 Nov;144(11):1006–1011. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 28.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., 3rd Race and insurance status as risk factors for trauma mortality. Archives of surgery (Chicago, Ill: 1960) 2008 Oct;143(10):945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 29.Rosen H, Saleh F, Lipsitz SR, Meara JG, Rogers SO., Jr Lack of insurance negatively affects trauma mortality in US children. Journal of pediatric surgery. 2009 Oct;44(10):1952–1957. doi: 10.1016/j.jpedsurg.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 30.Haider AH, Efron DT, Haut ER, DiRusso SM, Sullivan T, Cornwell EE., 3rd Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry. The Journal of trauma. 2007 May;62(5):1259–1262. doi: 10.1097/TA.0b013e31803c760e. discussion 1262–1253. [DOI] [PubMed] [Google Scholar]
- 31.Gannon CJ, Napolitano LM, Pasquale M, Tracy JK, McCarter RJ. A statewide population-based study of gender differences in trauma: validation of a prior single-institution study. Journal of the American College of Surgeons. 2002 Jul;195(1):11–18. doi: 10.1016/s1072-7515(02)01187-0. [DOI] [PubMed] [Google Scholar]
- 32.Crompton JG, Pollack KM, Oyetunji T, et al. Racial disparities in motorcycle-related mortality: an analysis of the National Trauma Data Bank. American journal of surgery. 2010 Aug;200(2):191–196. doi: 10.1016/j.amjsurg.2009.07.047. [DOI] [PubMed] [Google Scholar]
- 33.Falcone RA, Jr, Martin C, Brown RL, Garcia VF. Despite overall low pediatric head injury mortality, disparities exist between races. Journal of pediatric surgery. 2008 Oct;43(10):1858–1864. doi: 10.1016/j.jpedsurg.2008.01.058. [DOI] [PubMed] [Google Scholar]
- 34.Falcone RA, Jr, Brown RL, Garcia VF. Disparities in child abuse mortality are not explained by injury severity. Journal of pediatric surgery. 2007 Jun;42(6):1031–1036. doi: 10.1016/j.jpedsurg.2007.01.038. discussion 1036–1037. [DOI] [PubMed] [Google Scholar]
- 35.Martin CA, Care M, Rangel EL, Brown RL, Garcia VF, Falcone RA., Jr Severity of head computed tomography scan findings fail to explain racial differences in mortality following child abuse. American journal of surgery. 2010 Feb;199(2):210–215. doi: 10.1016/j.amjsurg.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 36.Millham F, Jain NB. Are there racial disparities in trauma care? World journal of surgery. 2009 Jan;33(1):23–33. doi: 10.1007/s00268-008-9745-z. [DOI] [PubMed] [Google Scholar]
- 37.Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE. Quality indicators for evaluating trauma care: a scoping review. Archives of surgery (Chicago, Ill: 1960) 2010 Mar;145(3):286–295. doi: 10.1001/archsurg.2009.289. [DOI] [PubMed] [Google Scholar]
- 38.Glance LG, Dick AW, Mukamel DB, Osler TM. Association between trauma quality indicators and outcomes for injured patients. Archives of surgery (Chicago, Ill : 1960) 2012 Apr;147(4):308–315. doi: 10.1001/archsurg.2011.1327. [DOI] [PubMed] [Google Scholar]
- 39.Mabry CD. Time to turn the page: moving on to write new chapters for trauma care. 20120417 DCOM-20120531 (1538-3644 (Electronic)) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.