Abstract
Although research continues to demonstrate that HIV stigma is associated with decreased HIV testing, the psychological processes implicated in this association remain unclear. The authors address this gap by differentiating between the HIV stigma mechanisms of stereotypes, prejudice, and discrimination. They hypothesize that HIV stereotypes specifically, more so than prejudice or discrimination, are associated with HIV testing among at-risk populations. Ninety-three HIV-negative people receiving methadone maintenance therapy at a clinic in the northeastern United States participated by completing a survey. Results demonstrated that HIV stereotypes are associated with HIV testing via the mediator of perceived HIV risk. As hypothesized, prejudice, discrimination, and objective HIV risk were not associated with perceived HIV risk. Differentiating between HIV stigma mechanisms in future work can provide critical insight into how to intervene in HIV stigma to increase HIV testing and improve HIV prevention among at-risk populations.
Evidence from Project Accept (Genberg et al., 2009; Young et al., 2001) and other studies throughout the world (Hamra, Ross, Orrs, & D'Agostino, 2006; Kalichman & Simbayi, 2003; Pitpitan et al., 2012) demonstrate that endorsement of greater HIV stigma is associated with decreased HIV testing. This robust association is even found with at-risk groups, including men who have sex with men (Li et al., 2012) and injection drug users (Ford, Wirawan, Sumantera, Sawitri, & Stahre, 2004), for whom regular HIV testing is critical for early detection and treatment (Branson et al., 2006). Despite this accumulating evidence, why this association exists remains unclear. Why might people who endorse greater HIV stigma, or social discrediting and devaluation of people living with HIV (PLWH; Earnshaw & Chaudoir, 2009), be less likely to test for HIV? A stronger understanding of the psychological processes underlying the association between HIV stigma and HIV testing has the potential to inform interventions targeting HIV stigma to increase HIV testing among at-risk populations. In the current work, we differentiate between the HIV stigma mechanisms of stereotypes, prejudice, and discrimination and hypothesize that HIV stereotypes specifically drive the association between HIV stigma and HIV testing. We further hypothesize that HIV stereotypes influence HIV testing via the mediator of perceived HIV risk. We evaluate these hypotheses among a sample of people at risk for HIV infection: patients enrolled in methadone maintenance therapy who have a history of drug addiction (e.g., heroin).
In a recent application of stigma theory to HIV, the HIV Stigma Framework suggests that HIV stigma is manifested among people at risk for HIV via three distinct stigma mechanisms: stereotypes, prejudice, and discrimination (Earnshaw & Chaudoir, 2009). The HIV Stigma Framework emphasizes the importance of differentiating between these mechanisms to enhance our understanding of how HIV stigma is associated with HIV-related behavior such as HIV testing. Stereotypes are group-based beliefs about PLWH that are often applied to individuals (e.g., PLWH are gay men, prostitutes, drug users). Prejudice represents negative emotions felt toward PLWH (e.g., disgust). Discrimination reflects behavioral expressions of prejudice directed toward PLWH (e.g., social rejection). Stereotypes, prejudice, and discrimination represent cognitive, affective, and behavioral manifestations of HIV stigma. Research on the association between HIV stigma and HIV testing has yet to differentiate among these three stigma mechanisms.
HIV stereotypes, rather than prejudice or discrimination, may play a key role in HIV testing. Past work demonstrates that people who endorse greater stereotypes perceive that they are less at risk of experiencing relevant negative events, including diseases (Weinstein, 1980). This cognitive manifestation of HIV stigma, more so than its affective and behavioral manifestations, represents a heuristic that people use to define who is at risk for HIV (e.g., gay men, prostitutes, drug users). People rely on such heuristics to evaluate their own risk of experiencing negative outcomes such as HIV (Slovic, 1987). For example, if an individual believes that gay men are most at risk for HIV and he does not identify as a gay man, then he may perceive that he is at low risk for HIV. Heuristics shape risk perceptions regardless of objective levels of risk (Slovic, 1987). Therefore, HIV stereotypes may shape people's perceived HIV risk despite their objective engagement in HIV risk behaviors. This same individual who endorses the stereotype about gay men and HIV may perceive that he is at low risk for HIV despite engaging in drug use and unprotected sex.
People who perceive themselves to be at lower risk for HIV may engage in less HIV testing. Longitudinal research demonstrates that people who perceive themselves to be at lower risk of disease subsequently engage in fewer behaviors to protect themselves from disease (Brewer, Weinstein, Cuite, & Herrington, 2004). This phenomenon extends to HIV testing as people who perceive themselves to be at lower HIV risk are less likely to test for HIV (Stein & Nyamathi, 2010). This association also occurs regardless of one's engagement in HIV risk behaviors (e.g., illicit drug use and/or unsafe sex; Fichtner, Wolitski, Johnson, Rabins, & Fishbein, 1996). That is, associations are shown controlling for objective HIV risk.
As shown in our theoretical model (see Figure 1), we hypothesized that HIV stereotypes are associated with HIV testing through the mediator of perceived HIV risk. That is, people who endorse greater stereotypes about PLWH are hypothesized to perceive themselves to be at lower risk for HIV, and people who perceive themselves to be at lower risk for HIV are hypothesized to engage in less frequent HIV testing. Because individuals use cognitive appraisals (i.e., stereotypes) to assess their perceived HIV risk, we hypothesized that the affective and behavioral aspects of HIV stigma (i.e., prejudice and discrimination) would not be associated with perceived HIV risk. Furthermore, we anticipated that the associations among HIV stereotypes, perceived HIV risk, and HIV testing occur controlling for objective HIV risk behaviors (i.e., recent illicit drug use and unprotected sex). We evaluated these hypotheses among a sample of patients receiving methadone maintenance therapy. Meta-analytic evidence suggests that methadone maintenance therapy reduces illicit drug use and other HIV risk behaviors, but only at small to moderate effect sizes (Marsch, 1998). Therefore, methadone maintenance therapy patients often continue to engage in HIV risk behaviors such as drug use and unprotected sex. Frequent HIV testing is important for early detection and treatment among this at-risk population (Branson et al., 2006).
FIGURE 1.
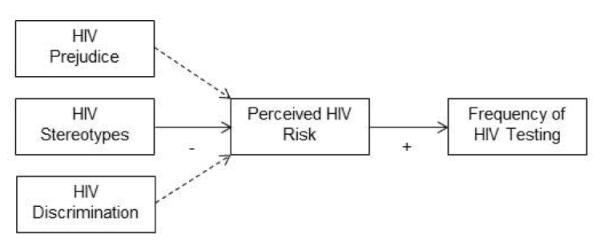
Theoretical model of HIV stigma mechanisms and HIV testing among at-risk populations. Dashed lines represent a hypothesized nonassociation between variables.
METHODS
PARTICIPANTS AND PROCEDURE
Participants were enrolled in methadone maintenance therapy in the northeastern United States and were recruited from an ongoing HIV risk reduction randomized control trial. Of the 304 participants in the randomized control trial, 93 (30.6%) agreed to participate in this substudy by completing a supplemental cross-sectional survey at a follow-up to the randomized control trial for an additional small incentive. Most nonsubsample participants did not complete the survey because they had no further scheduled follow-ups for the randomized control trial. All demographic and self-report risk characteristics were collected as part of the randomized control trial using audio computer-assisted self-interview technology (ACASI). Methadone dose was abstracted from medical charts. Urine screens for cocaine, opiates, and oxycodone use were conducted as part of the randomized control trial. The supplemental survey completed by the subsample included the HIV stigma mechanisms, perceived HIV risk, and frequency of HIV testing items and was administered using paper and pencil. All self-report items were pretested to ensure comprehensibility by participants.
The mean age of the subsample was 37.10 (SD = 10.21); 50.5% were male; 67.7% were White, 14.0% Black, and 14.0% Latino; 65.6% reported an annual income below $11,000; and the average daily methadone dose was 84.80 mg/day (SD = 28.39). Most subsample participants (78.5%) reported a history of injection drug use; 42.9% had recently tested positive for cocaine, opiate, and/or oxycodone use via a urine screen; and 65.5% reported recent unprotected vaginal, anal, and/or oral sex. Subsample participants did not differ from nonsubsample participants on gender, income, randomized control trial condition, methadone dose, history of injection drug use, recent drug use, or recent unprotected sex. The subsample was slightly older than the nonsubsample participants [nonsubsample: M = 32.21, SD = 8.78; t(302) = −4.66, p < .001], and were less likely to be White and more likely to be Black [nonsubsample: 78.5% White, 5.7% Black; χ2 (3) = 10.92, p = .01]. This study had Institutional Review Board approval from the University of Connecticut, and participants provided informed consent.
MEASURES
Given that previously developed scales conflate the HIV stigma mechanisms of stereotypes, prejudice, and discrimination (Earnshaw & Chaudoir, 2009), several measures were created and pilot tested for the current study. Items were measured on 1-to-5-point Likert scales and averaged such that higher means indicate greater endorsement of stigma. HIV stereotypes were assessed with four items, including: “Most people who are HIV positive are … gay men, prostitutes, drug users” (M = 2.13, SD = 0.84; α = .76). HIV prejudice was assessed with five items, including: “People who are HIV positive make me feel … nervous, afraid, uncomfortable” (M = 2.42, SD = 0.77; α = .81). HIV discrimination was assessed with five items, including: “People who are HIV positive should be treated the same as everyone else” (reverse scored) (M = 1.67, SD = 0.57; α = .73). The three stigma mechanisms were moderately to strongly correlated (rs = .31~.46, ps < .01), providing evidence for their theorized association. However, all correlations were below .80, supporting discriminant validity between the constructs (i.e., measuring separate, yet related, constructs; Brown, 2006).
Perceived HIV risk and HIV testing frequency were also measured on 1-to-5-point Likert scales with higher means indicating greater perceptions of risk or frequency of testing. Perceived HIV risk was assessed with one item, tailored for the study population: “Currently, how at risk are you for getting HIV from using drugs?” (M = 1.48, SD = 0.94). Frequency of HIV testing was assessed with one item: “How frequently do you test for HIV?” (M = 3.71, SD = 1.50). Participants reported testing for HIV an average of every 2 to 3 years. This average falls below the Centers for Disease Control and Prevention's recommendation of annual HIV testing for high-risk populations (Branson et al., 2006).
RESULTS
All analyses controlled for demographics, trial condition, methadone dose, and objective HIV risk (history of injection drug use, recent drug use, recent unprotected sex). First, HIV stereotypes, prejudice, and discrimination were entered into a linear regression analysis predicting perceived HIV risk. As shown in Table 1, HIV stereotypes were associated with perceived HIV risk: Participants who endorsed HIV stereotypes to a greater extent perceived themselves to be at lower risk of acquiring HIV. As hypothesized, neither HIV prejudice nor discrimination was associated with perceived HIV risk. Objective HIV risk behaviors were also not associated with perceived HIV risk.
TABLE 1.
Linear Regression Predicting Perceived HIV Risk
| Predictor | B (SE) | β | t |
|---|---|---|---|
| Demographics | |||
| Age | −0.01 (0.01) | −0.16 | −1.15 |
| Male gender | 0.29 (0.20) | 0.17 | 1.46 |
| White ethnicity | −0.36 (0.24) | −0.19 | −1.49 |
| Income | −0.23 (0.13) | −0.20 | −1.76† |
| RCT Trial Condition | −0.10 (0.20) | −0.06 | −0.51 |
| Methadone Dose | −0.01 (0.01) | −0.17 | −1.35 |
| Objective HIV Risk | |||
| History of IDU | −0.18 (0.28) | −0.08 | −0.64 |
| Recent drug use | −0.12 (0.20) | −0.07 | −0.59 |
| Recent unprotected sex | −0.15 (0.23) | −0.08 | −0.66 |
| HFV Stigma Mechanisms | |||
| HIV stereotypes | −0.34 (0.13) | −0.32 | −2.67** |
| HIV prejudice | −0.21 (0.16) | −0.18 | −1.33 |
| HIV discrimination | 0.26 (0.20) | 0.17 | 1.29 |
Note.
p ≤ .10.
p ≤ .01.
Second, HIV stereotypes and perceived HIV risk were entered into a bootstrap analysis predicting frequency of HIV testing (Hayes, in press; Shrout & Bolger, 2002). Bootstrapping is a statistical resampling method that estimates the indirect effect of an independent variable on a dependent variable via a mediating variable and has been recommended for mediation analyses with small sample sizes (Shrout & Bolger, 2002). Table 2 includes the direct effects of all variables, including HIV stereotypes and perceived HIV risk, on frequency of HIV testing. Although there was no direct effect of HIV stereotypes on frequency of HIV testing, there was an effect of perceived HIV risk on frequency of HIV testing: Participants who perceived greater HIV risk engaged in more frequent HIV testing. The bootstrap analysis further demonstrated that HIV stereotypes had an indirect effect on frequency of HIV testing via the mediator of perceived HIV risk (B = −0.15, SE = 0.09; CI [−0.36, 0.01]). Additional analyses demonstrated that the effect was not moderated by recent drug use.
TABLE 2.
Linear Regression Predicting Frequency of HIV Testing
| Predictor | B (SE) | β | t |
|---|---|---|---|
| Demographics | |||
| Age | 0.03 (0.02) | 0.20 | 1.49 |
| Male gender | 0.01 (0.34) | 0.01 | 0.04 |
| White ethnicity | 0.29 (0.42) | 0.09 | 0.69 |
| Income | −0.03 (0.22) | −0.02 | −0.14 |
| RCT Trial Condition | −0.35 (0.34) | −0.12 | −1.06 |
| Methadone Dose | 0.01 (0.01) | 0.06 | 0.47 |
| Objective HIV Risk | |||
| History of IDU | 1.73 (0.46) | 0.47 | 3.77** |
| Recent drug use | 0.33 (0.33) | 0.11 | 0.99 |
| Recent unprotected sex | 0.28 (0.40) | 0.09 | 0.69 |
| HIV Stereotypes | 0.08 (0.21) | 0.05 | 0.40 |
| Perceived HIV Risk | 0.45 (0.20) | 0.26 | 2.23* |
Note.
p ≤ .05.
p ≤ .01.
Given that the sample consisted of people with a history of drug use, additional analyses were conducted to ensure that including the item on drug users in the stereotypes measure (i.e., “Most people who are HIV positive are drug users”) did not skew the results. Analyses were replicated, including the measure of HIV stereotypes with the item on drug users removed (M = 2.18, SD = 0.90; α = .54). Results were consistent with original findings.
DISCUSSION
This is the first known study to differentiate between the HIV stigma mechanisms of stereotypes, prejudice, and discrimination in relation to HIV testing. Results suggest that HIV stereotypes may be the specific HIV stigma mechanism driving the association between HIV stigma and HIV testing found in previous work. HIV stereotypes influenced HIV testing frequency via the mediator of perceived HIV risk. That is, people who endorsed greater HIV stereotypes perceived themselves to be at lower risk of acquiring HIV. In turn, people who perceived themselves to be at lower risk of acquiring HIV tested less frequently for HIV. These associations occurred despite objective engagement in HIV risk behaviors, including drug use and unprotected sex. Results suggest that HIV stereotypes play a powerful role in at-risk people's assessment of their HIV risk, perhaps more so than their actual engagement in HIV risk behavior. Additionally, this is the first known study to provide evidence for discriminant validity among HIV stigma mechanisms proposed by the HIV Stigma Framework (Earnshaw & Chaudoir, 2009). Although these cognitive, affective, and behavioral manifestations of HIV stigma were correlated, only the cognitive manifestation was associated with HIV testing.
This study is limited by its cross-sectional methodology. Consistent with past work (Ford et al., 2004; Genberg et al., 2009; Hamra et al., 2006; Kalichman & Simbayi, 2003; Li et al., 2012; Pitpitan et al., 2012; Young et al., 2010), we theorize that endorsing greater HIV stigma influences HIV testing. Results of longitudinal research support this theory by demonstrating that perceived risk is associated with subsequent engagement in preventive health behaviors (Brewer et al., 2004). However, it is also possible that engaging in HIV testing influences endorsement of HIV stigma, including HIV stereotypes. Future research should examine these associations using longitudinal and experimental methodologies to determine whether greater endorsement of HIV stereotypes leads to decreased HIV testing. Additionally, the current study measured perceived HIV risk due to drug use only. Although this item was tailored for the study population (i.e., patients enrolled in methadone maintenance therapy who have a history of drug addiction), it does not capture perceived HIV risk due to other behaviors such as sex. Future research should use more comprehensive measures of perceived HIV risk. Future research might also replicate these results among other samples. Although our sample size was small, a post-hoc power analysis demonstrated that we had adequate power (0.98) to detect statistically significant effects. Nonetheless, future research might test whether these processes replicate among larger samples, including other at-risk populations.
CONCLUSIONS
These results have implications for researchers and clinicians working with populations at risk for HIV. First, interventions such as Project Accept that seek to increase HIV testing might explicitly focus on reducing HIV stereotypes rather than HIV stigma in general. For example, interventions may explicitly aim to eliminate stereotypes that all PLWH are gay men, prostitutes, and/or drug users while emphasizing that HIV risk is determined by HIV risk behaviors. In doing so, at-risk individuals may perceive their own HIV risk more accurately and in turn test for HIV more frequently. This strategy is consistent with prevention work that has long aimed to increase accurate knowledge of or information regarding the importance of behaviors, rather than group membership, in determining HIV risk (e.g., Fisher & Fisher, 1992). Second, these results suggest that work that continues to differentiate between the HIV stigma mechanisms proposed by the HIV Stigma Framework (Earnshaw & Chaudoir, 2009) can provide critical insight into why and how HIV stigma is associated with other HIV-related behaviors, including those relevant to HIV prevention efforts. It is likely that stereotypes, prejudice, and discrimination play differing roles in HIV-related behaviors beyond HIV testing, such as HIV risk behavior and treatment of PLWH. It is only through more nuanced and sophisticated understandings of HIV stigma that we will be able to intervene in HIV stigma to improve outcomes for people at risk of and living with HIV.
Acknowledgments
A grant from the National Institute on Drug Abuse (RO1 DA022122) awarded to Copenhaver funded the randomized controlled trial from which participants were drawn for the current study. A seed grant from the University of Connecticut Center for Health Intervention and Prevention funded work on the HIV stigma survey. Training grants from the National Institute of Mental Health funded Earnshaw's (T32 MH020031) and Smith's (F31 MH093264) efforts.
The authors thank the participants, as well as Ruth Arnold, Denese Bellinger, Marla Genova, and Brian Sibilio for their assistance with data collection.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Center for Health Intervention and Prevention.
REFERENCES
- Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Morbidity and Mortality Weekly Report. 2006;55(RR14):1–17. [PubMed] [Google Scholar]
- Brewer NT, Weinstein ND, Cuite CL, Herrington JE. Risk perceptions and their relation to risk behavior. Annals of Behavioral Medicine. 2004;27(2):125–130. doi: 10.1207/s15324796abm2702_7. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. Guilford Press; New York: 2006. [Google Scholar]
- Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fichtner RR, Wolitski RJ, Johnson WD, Rabins CB, Fishbein M. Influence of perceived and assessed risk on STD clinic clients' acceptance of HIV testing, return for test results, and HIV serostatus. Psychology, Health, & Medicine. 1996;1(1):83–98. [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111(3):455–476. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Ford K, Wirawan DN, Sumantera GM, Sawitri AA, Stahre M. Voluntary HIV testing, disclosure, and stigma among injection drug users in Bali, Indonesia. AIDS Education and Prevention. 2004;16(6):487–498. doi: 10.1521/aeap.16.6.487.53789. [DOI] [PubMed] [Google Scholar]
- Genberg BL, Hlavka Z, Konda KA, Maman S, Chariyalertsak S, Chingono A, et al. A comparison of HIV/AIDS-related stigma in four countries: Negative attitudes and perceived acts of discrimination towards people living with HIV/AIDS. Social Science & Medicine. 2009;68(12):2279–2287. doi: 10.1016/j.socscimed.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamra M, Ross MW, Orrs M, D'Agostino A. Relationship between expressed HIV/AIDS-related stigma and HIV-beliefs/knowledge and behaviour in families of HIV infected children in Kenya. Tropical Medicine and International Health. 2006;11(4):513–527. doi: 10.1111/j.1365-3156.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- Hayes AF. An introduction to mediation, moderation, and conditional process analysis: A regression based approach. Guilford Press; New York: in press. [Google Scholar]
- Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counseling and testing in a black township in Cape Town, South Africa. Sexually Transmitted Infections. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Lu H, Ma X, Sun Y, He X, Li C, et al. HIV/AIDS-related stigmatizing and discriminatory attitudes and recent HIV testing among men who have sex with men in Beijing. AIDS & Behavior. 2012;16(3):499–507. doi: 10.1007/s10461-012-0161-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: A meta-analysis. Addiction. 1998;93(4):515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Skinner D, et al. AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape Town, South Africa. Annals of Behavioral Medicine. 2012;43(3):362–371. doi: 10.1007/s12160-012-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7(4):422–445. [PubMed] [Google Scholar]
- Slovic P. Perception of risk. Science. 1987;236:280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- Stein JA, Nyamathi A. Psychological and socio-medical aspects of AIDS/HIV. AIDS Care. 2010;12(3):343–356. doi: 10.1080/09540120050043007. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Unrealistic optimism about future life events. Journal of Personality and Social Psychology. 1980;39(5):806–820. [Google Scholar]
- Young SD, Hlavka Z, Modiba P, Gray G, Van Rooyen H, Richter L, et al. HIV-related stigma, social norms, and HIV testing in Soweto and Vulindlela, South Africa: National Institutes of Mental Health Project Accept (HPTN 043) Journal of Acquired Immune Deficiency Syndrome. 2010;55(5):620–624. doi: 10.1097/QAI.0b013e3181fc6429. [DOI] [PMC free article] [PubMed] [Google Scholar]


