Abstract
Though the knee experiences three-dimensional loading during everyday tasks, assessment of proprioceptive acuity has typically been limited to the primary direction of movement, knee flexion and extension. While loading in the constrained directions (varus/valgus and internal/external rotation) may contribute to injury and joint disease, little information is available regarding proprioceptive acuity in these planes of movement. The primary aim of this study was to characterize proprioceptive acuity in the frontal plane (varus/valgus) and to compare it with sagittal plane (flexion/extension) proprioceptive acuity in healthy subjects. Proprioception was assessed in 17 young, healthy subjects (11 females, 6 males, ages 21–33 years) using the threshold to detection of passive movement (TDPM). TDPM was found to be significantly (P < 0.001) lower in the frontal plane [valgus: mean (SD) 0.60 (0.20)° and varus: 0.58 (0.23)°] compared with the sagittal plane [extension: 0.78 (0.34)°, flexion: 0.82 (0.48)°]; however, no significant differences were noted within the same plane of movement. Results from this preliminary study may suggest more accurate proprioceptive acuity in the frontal plane compared with the sagittal plane. While further examination is necessary to confirm this relationship, more accurate frontal plane acuity may reflect a protective neural mechanism which enables more precise neuromuscular control of the joint in this constrained plane of movement.
Keywords: Knee, Propriocepion, Frontal plane, Sagittal plane
Introduction
The central nervous system continuously uses sensory input from mechanoreceptors in muscles, joints, and skin to update information about joint configuration during movement. At the conscious level, these somatosensory representations constitute proprioception, or the awareness of joint movement and position (Riemann and Lephart 2002a). Proprioceptive feedback has been demonstrated to be a key component of motor control and functional joint stability (Dietz et al. 1987; Riemann and Lephart 2002b; Sainburg et al. 1995). In this context, proprioceptive and neuromuscular training programs have been advocated for the rehabilitation and prevention of musculoskeletal disorders of the knee (Hewett et al. 2002, 2006; Lephart et al. 1997). One of the aims of these training paradigms is to enhance the awareness of joint movement and position, while adopting appropriate motor control strategies which maintain joint stability and protect the joint’s connective tissues. As loading in constrained movement directions (varus/valgus and internal/external rotation) has been associated with increased risk of injury and disease (Hewett et al. 2005; Jackson et al. 2004; Lewek et al. 2004; McLean et al. 2004; Sharma et al. 2003; Weidow et al. 2006), training paradigms often utilize a variety of movements designed to challenge knee stability in both the primary plane of movement (flexion/extension) and these constrained movement directions (Hewett et al. 2006).
Such multi-dimensional demands pose a dual task to the neuromuscular system: produce movement in the primary direction and maintain stabilizing forces in the constrained directions. This dual task would necessitate proprioceptive feedback on joint kinematics and kinetics in all three planes of movement. However, while numerous studies have characterized knee proprioception in the sagittal plane in healthy and pathological populations (Ageberg et al. 2007; Hurkmans et al. 2007; Koralewicz and Engh 2000; Rozzi et al. 1999), relatively few studies have examined proprioceptive acuity in the constrained planes of movements (frontal and transverse planes). Recently, Muaidi and colleagues examined proprioception during active internal and external rotations of the knee in both healthy (Muaidi et al. 2008) and anterior cruciate ligament (ACL) injured groups (Muaidi et al. 2009). Given that transverse plane rotations result in tension on the ACL, it was argued that this testing paradigm enables a more targeted evaluation of the contribution of the ACL and the detrimental effects of ligament injury on proprioception (Muaidi et al. 2008). Indeed, results from these studies indicated that transverse plane proprioceptive acuity is impaired following ACL injury, but can be restored with ACL reconstruction (Muaidi et al. 2009). Furthermore, results from these studies provide insights into the stabilization of the joint to loading in a direction which contributes to ACL injury risk (Bahr and Krosshaug 2005). Recent evidence has also implicated abnormal frontal plane knee joint kinetics as a risk factor in joint injury and degenerative disease (Astephen et al. 2008; Hewett et al. 2005; Jackson et al. 2004; Khan et al. 2008; Lewek et al. 2004; McLean et al. 2004; Sharma et al. 2003; Weidow et al. 2006). However, to our knowledge, there have been no investigations of proprioceptive acuity in this plane.
Accordingly, the primary aim of this study was to examine proprioceptive acuity in the frontal plane of the knee in healthy subjects using the threshold to detection of passive movement (TDPM). As detection thresholds are contingent upon the specific experimental conditions in which they are gathered, we also measured TDPM in the sagittal plane to provide a comparison between the primary and constrained planes of movement at the knee. Due to the differences in range of motion between the two movement directions, we hypothesized that detection thresholds will be lower in the frontal plane. Furthermore, as this was the first examination of proprioceptive acuity in the frontal plane, an additional aim of the study was to determine the test–retest reliability of the TDPM metric in this movement direction. Knowledge gained from this study may provide new insights into the mechanisms contributing to multidimensional joint stability which may be especially significant in the context of the prevention and management of joint injury and disease.
Methods
All experimental procedures were approved by the Institutional Review Board of Northwestern University and complied with the principles of the Declaration of Helsinki. Seventeen healthy subjects (11 females and 6 males, ages 21–33 years) with no history of neurological or musculoskeletal disorders participated in the study after providing informed consent. Subject demographics are presented in Table 1. The experiment was conducted over two testing sessions on separate days, with one session testing proprioception in the sagittal plane and the other in the frontal plane of the knee. Each testing session lasted approximately 1.5–2 h and the order of the testing sessions was randomized.
Table 1.
Subject demographics. Reported as mean (SD)
| Age (years) | Height (m) | Weight (kg) | BMI (kg/m2) | |
|---|---|---|---|---|
| All subjects (N = 17) | 25 (3) | 1.67 (0.06) | 66 (12) | 24 (4) |
| Females (N = 11) | 24 (3) | 1.64 (0.05) | 61 (12) | 23 (4) |
| Males (N = 6) | 25 (3) | 1.71 (0.06) | 74 (6) | 25 (3) |
The experimental apparatus used for proprioceptive testing has been described previously (Dhaher et al. 2003). For testing in the frontal plane, subjects were seated in an experimental chair with the right knee at neutral flexion/extension (0° knee flexion) (Fig. 1a). The subject’s right ankle was placed in a modified, inflated, aircast (Aircast, DJO Inc. Vista, CA, USA) and then secured within a coupling ring, which fixed the limb to a servomotor actuator, via a rigid cantilever beam. The beam was visually aligned with the subject’s lower leg and the subject was allowed to assume their natural frontal plane knee joint alignment. Brackets were securely fastened around the knee joint at the femoral epicondyles to prevent medial/lateral translation of the femur during testing, and a strap was placed over the right thigh to prevent movement of the proximal limb.
Fig. 1.
Schematic of the experimental configuration for proprioceptive testing in a the frontal plane and b the sagittal plane
For testing in the sagittal plane, the servomotor assembly was rotated 90° so that the cantilever beam was initially vertical and the servomotor center of rotation was aligned with the femoral epicondyles. Similar to testing in the frontal plane, subjects were seated and a modified air-cast was placed around the subject’s right ankle and then secured within the coupling ring attached to the servomotor (Fig. 1b).
Proprioceptive testing
To characterize proprioceptive acuity in a functionally relevant posture, the targeted test posture was chosen to be consistent with a knee posture observed during the stance phase of gait (30° of knee flexion and neutral varus/valgus) (Lafortune et al. 1992). While this knee flexion angle was easily attained for sagittal plane testing, isolating varus and valgus motions of the knee in this flexed knee posture is technically difficult (Dhaher and Francis 2006). Therefore, frontal plane proprioceptive testing was performed with the knee at 0° of knee flexion. Previous work from our laboratory has demonstrated that production of knee varus and valgus movements in this posture is consistent and reliable (Dhaher and Francis 2006).
During proprioceptive testing procedures, subjects wore headphones with white noise playing and an eye mask to minimize auditory and visual cues associated with the servomotor. Subjects were instructed to remain relaxed throughout the experimental procedures and to not volitionally contract their leg muscles. Surface EMG electrodes (Delsys Bagnoli 3.1, Boston, MA, USA) recorded muscle activity in the quadriceps and hamstring muscles throughout the testing protocol to ensure that subjects maintained a relaxed state. Unacceptable EMG activity was identified when the mean EMG activity during the testing protocol was greater than two standard deviations above the mean baseline activity, collected 200 ms prior to the onset of joint movement. Trials that showed unacceptable EMG activity were rejected.
TDPM was assessed in four movement directions: towards varus, valgus, flexion, and extension, following a protocol similar to previously published reports (Boerboom et al. 2008; Hurkmans et al. 2007; van der Esch et al. 2007). From the initial postures described above, the servomotor rotated the knee at a velocity of 1°/s and subjects were instructed to press a handheld button as soon as movement of the limb was detected. The slow velocity was chosen to minimize subjects’ detection of a sudden onset of movement and is within the range of angular velocities (0.5–2°/s) suggested for assessing proprioceptive acuity (Riemann et al. 2002). Though slower testing velocities, such as 0.5°/s or less, are often used in TDPM tests (Boerboom et al. 2008; Hurkmans et al. 2007; van der Esch et al. 2007), a velocity of 1°/s was used due to practical limitations related to the software controlling the servomotor.
The maximum angular excursion during proprioceptive testing was 5° in the frontal plane and 7° in the sagittal plane. To ensure that subjects were comfortable with movements in the frontal plane, several smaller stretches were applied at the beginning of the experimental session. Starting at 3°, the stretches were incrementally increased by 1° to a maximum of 5° and subjects were asked to report any discomfort with the movements. All study participants were comfortable with this range of movement in the frontal plane.
TDPM was defined as the position difference between the onset of movement and the subjects’ detection of movement, with smaller TDPM values indicating greater proprioceptive acuity. Following familiarization with the protocol, at least five trials were performed in each testing direction in a randomized order.
Test–retest reliability
A test–retest reliability study was performed on a separate study population to determine consistency of measurements between testing sessions. Fifteen young, female subjects [mean (SD) age: 22.3 (1.9) years, height: 1.65 (0.05) m, weight: 60.2 (11.5) kg] participated in two frontal plane testing sessions that were on average 12.5 (SD 2.4) days apart (range 8–15 days). Similar to previous studies (Ageberg et al. 2007; Rankin and Stokes 1998), the reliability of the proprioceptive testing procedure was assessed using the intraclass correlation coefficient [ICC(1,2)] (Shrout and Fleiss 1979) and Bland and Altman tests for agreement between test sessions (Bland and Altman 1986). The Bland and Altman tests include (1) a graphical representation (Bland–Altman plot) of the difference between test measures plotted against the mean of the two measures; (2) calculation of the mean of the difference between test measures (d̄) and 95% confidence intervals (CI) of d̄; and (3) a measure of the limits of agreement (LOA) between the two measures, which is defined as d̄ ± 2 × SDdiff, where SDdiff is the standard deviation of the differences.
Statistical analysis
All statistical analyses were performed using the NCSS software suite (NCSS, Kaysville, UT, USA) with significance set a priori to α = 0.05. A preliminary analysis indicated no significant differences in genders, so male and female data were analyzed together. A repeated measures analysis of variance (ANOVA) using one within-subjects factor (movement direction) was performed to examine differences between varus, valgus, flexion, and extension TDPM. Post hoc Tukey–Kramer multiple comparisons were used when a significant effect was found.
Results
TDPM results
TDPM values were found to be lower in the frontal plane compared with the sagittal plane [Mean (SD) TDPM for valgus: 0.60 (0.20), varus: 0.58 (0.23), extension: 0.78 (0.34), and flexion: 0.82 (0.48)]. Repeated measures ANOVA revealed a significant main effect of movement direction (P <0.001). Post hoc Tukey–Kramer multiple comparison analysis showed that varus and valgus TDPM values were each significantly less than those for flexion and extension. No significant differences were found between TDPM values within the same plane of movement (i.e. valgus vs. varus and flexion vs. extension).
Reliability of TDPM in the frontal plane
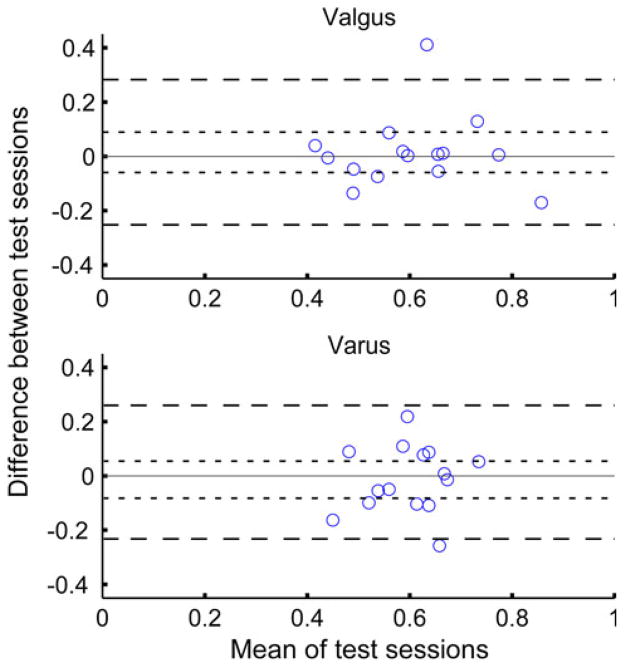
No significant differences were found between varus and valgus TDPM results from the first and second test sessions (P = 0.67 for varus and 0.68 for valgus by repeated measures ANOVA). Frontal plane TDPM measures demonstrated good reliability in valgus [with ICC(1,2) = 0.72] and fair reliability in varus [ICC(1,2) = 0.40], according to the classifications of Fleiss (1986). Results from the Bland and Altman procedures indicated no systematic bias between test sessions, as the mean difference, d̄; between test sessions was small and the 95% CI for d̄ included 0 [d̄ (95% CI): 0.015 (−0.059,0.089) for valgus and 0.014 (−0.082,0.054) for varus] (Fig. 2). The LOA were narrow at (−0.25,0.28) for valgus and (−0.23,0.26) for varus. Furthermore, the mean absolute difference between measurements was small as well, at 0.08 for valgus and 0.10 for varus.
Fig. 2.
Bland–Altman plot for agreement between test measures for valgus (top) and varus (bottom). The difference between the two test measures (TDPM on day 1–TDPM on day 2) is plotted versus the mean TDPM across test days. The 95% confidence intervals (CI) of the mean difference between test days (d̄) is shown as dotted lines. The 95% limits of agreement (LOA) are shown as dashed lines
Discussion
Knowledge of proprioceptive acuity in the constrained planes of movement (frontal and transverse) at the human knee is lacking. This study provides the first measures of proprioceptive acuity in the frontal plane of the healthy knee and demonstrates that TDPM is a reliable assessment of frontal plane proprioception. TDPM values were similar between the varus and valgus directions; however, results indicated lower TDPM values in the frontal plane compared with the sagittal plane. Specifically, average detection thresholds were 0.58° and 0.60° in varus/valgus and 0.78° and 0.82° in flexion/extension. This apparent difference in TDPM may be attributed to the difference in range of motion between planes of movement. Previous reports have demonstrated lower detection thresholds near the end range of movement, which has been attributed to a protective neural mechanism (Ageberg et al. 2007; Friden et al. 2001; Friden et al. 1996). Thus, lower TDPM values in the frontal plane may reflect the constrained range of motion in this movement direction. In this context, knowledge of proprioceptive acuity in this direction may have direct clinical implications in understanding knee joint pathologies, such as OA and ACL injury, which may be aggravated by frontal plane loading (Astephen et al. 2008; Hewett et al. 2005; Jackson et al. 2004; Khan et al. 2008; Lewek et al. 2004; McLean et al. 2004; Sharma et al. 2003; Weidow et al. 2006). The results of this study can be used as baseline data for the evaluation of frontal plane proprioceptive acuity in various pathological populations.
The conscious perception of joint movement and position involves the central processing of sensory feedback arising from muscle, skin, and joint (periarticular) mechanoreceptors (Riemann and Lephart 2002a). While the exact degree to which each receptor type contributes to joint proprioception remains unknown, we believe that frontal and sagittal plane rotations primarily target different tissues. Movement in the frontal plane stretches the capsule-ligamentous structures of the joint, which would presumably engage periarticular receptors. Conversely, it is unlikely that periarticular mechanoreceptors were engaged during sagittal plane movements, as testing was performed in the mid-range of movement (30° knee flexion) under a relaxed state (Grigg and Greenspan 1977). On the other hand, muscle spindles were likely active during knee flexion and extension movements. While spindles may have also been engaged during varus and valgus rotations, a previous geometric analysis using musculoskeletal modeling software (SIMM, MusculoGraphics, Inc. Santa Rosa, CA, USA) indicated insignificant changes in musculotendon length (Dhaher et al. 2003), suggesting that the role of muscle spindles in this plane may be limited. Thus, though the exact contribution of various mechanoreceptors cannot be discerned in the present study, we believe that the primary sources of afferent feedback in the frontal and sagittal planes were periarticular mechanoreceptors and muscle spindles, respectively.
The differences in TDPM between the frontal and sagittal plane observed in this study may potentially be attributed to differences in receptor type as well as other peripheral and central neural mechanisms. Evidence from microstimulation experiments in awake humans indicates a more direct cortical connection from periarticular afferents than muscle spindles (Macefield et al. 1990; Macefield 2005), which may imply an increased central sensitivity to the activity of periarticular receptors. Further, as the frontal plane of the knee is highly constrained, the applied rotations constituted a larger proportion of the range of motion than rotations in the sagittal plane. This may have resulted in a comparatively more intense mechanical stimulus, which could lead to increased afferent outflow.
In addition to afferent feedback, cognitive processes also play a large role in the conscious perception of joint movement. Tests of perception, like TDPM, require subjects to pay attention and focus on the sensation at their joint (Fagius and Wahren 1981). As joint rotations in the frontal plane are relatively novel, subjects may have focused more intently on their knees. Even if afferent feedback from mechanoreceptors was similar between planes of movement, it is possible that enhanced cognitive (central) processing may have contributed to the lower TDPM values in the frontal plane.
The finding of lower TDPM values in the frontal plane may potentially suggest more accurate proprioceptive acuity in the frontal plane compared with the sagittal plane. However, it is important to note that differences in the experimental testing protocol across planes of movement may have also contributed to the observed results, and therefore limit our interpretation. First, testing was performed in two different knee postures. As stated in the methods section, the targeted testing posture in this study was 30° of knee flexion and neutral varus/valgus, a posture commonly seen during the stance phase of gait (Lafortune et al. 1992). However, in a flexed knee posture, it is technically difficult to isolate varus and valgus rotations at the knee from proximal rotation of the femur (Dhaher and Francis 2006). Therefore, frontal plane testing was performed at 0° of knee flexion, while sagittal plane testing was performed at 30° of knee flexion. The disparate knee flexion angles used during testing may have confounded our interpretation of the differential proprioceptive acuity across planes of movement. If sagittal plane testing had been performed at a more extended knee angle, it is possible that the differences in TDPM across planes may have diminished. Indeed, previous studies have demonstrated that knee extension TDPM improves as the knee is extended (Ageberg et al. 2007; Boerboom et al. 2008). However, the same investigations report the opposite relationship for knee flexion TDPM, as proprioceptive acuity became less accurate at more extended knee postures. Consistent with these prior observations, a preliminary examination on three subjects indicated that TDPM in knee extension and flexion improved by an average of 0.10° and 0.01°, respectively, from 30° of flexion to 10°. Thus, though these results are not conclusive, it is possible that the difference between TDPM in the frontal plane and extension observed in the current study may be in part attributed to the difference in testing posture. However, even at a more extended knee posture, the significant difference between TDPM in the frontal plane and knee flexion likely would have remained.
An additional experimental factor which may confound the interpretation of our results was the use of brackets at the knee during frontal plane testing. As described in the “Methods” section and depicted in Fig. 1, brackets were positioned just proximal to the femoral epicondyles, in order to isolate varus and valgus rotations at the knee. These brackets, which were not present during testing in the sagittal plane, may have provided additional sensory information from cutaneous afferents, which could have increased proprioceptive acuity in the frontal plane. In an attempt to examine the potential effect of this additional cutaneous sensation in the sagittal plane, three subjects were tested with and without a thick padded strap across the thigh during the sagittal plane paradigm. TDPM was found to improve by 0.03° on average, which is less than the difference in TDPM between planes of movement. Therefore, these preliminary observations may suggest that proprioceptive differences across planes cannot be primarily attributed to variations in cutaneous cues across paradigms. Nonetheless, future investigations, utilizing anesthetics on the skin, may be necessary to fully describe the contribution of cutaneous afferents to proprioception in each plane of movement.
The assessment of proprioceptive acuity using TDPM has been demonstrated as a reliable measurement in the sagittal plane of the knee (Ageberg et al. 2007). Similarly, results from our test–retest reliability study indicated fair to good repeatability (Fleiss 1986). However, ICC values for varus movement were lower than for valgus movement. This may be due to the relatively small inter-subject variability observed for this metric (see Fig. 2). Indeed, one of the limitations of the ICC is its sensitivity to the variability between subjects (Rankin and Stokes 1998). Despite differences in ICC between varus and valgus, the Bland and Altman methods reveal similar results for both directions and indicate minor differences between test sessions. Taken together, these tests indicate that the TDPM procedure used in the frontal plane has good reliability, which is comparable to previous studies of TDPM in the sagittal plane (Ageberg et al. 2007).
The TDPM testing protocol used in the current study was based on those described previously. However, one divergence from prior reports is the use of a faster testing velocity: 1°/s in the current study compared with the commonly used 0.5°/s (Boerboom et al. 2008; Hurkmans et al. 2007; van der Esch et al. 2007). While one could argue that this may have affected our results, a previous investigation reported insignificant variations in TDPM for velocities ranging from 0.1 to 0.85°/s (Pap et al. 1999). Furthermore, given that the same angular velocity was used in all testing sessions, we assume that proprioceptive comparisons across movement directions were unaffected by our choice of testing velocity.
While this investigation was not designed to examine the effect of gender on proprioceptive acuity, our preliminary analysis of the current results revealed no significant differences between males and females in any direction of movement. However, previous investigators have reported gender differences in proprioceptive acuity at the knee (Boerboom et al. 2008; Rozzi et al. 1999). It is possible that the lack of difference observed in the current study was the result of inadequate statistical power due to the small sample size. Given the observed differences in frontal plane loading across genders and its association with the risk of ACL injury (Griffin et al. 2006; Hewett et al. 2005), an extensive examination of potential gender effects on the observed proprioceptive acuity is warranted.
Results from this study indicate a statistically significant difference in detection thresholds between the frontal and sagittal planes of movement in favor of the frontal plane. Though results are preliminary and subject to the limitations described above, it could be hypothesized that they reflect more accurate proprioceptive acuity in the frontal plane, potentially suggesting that the neuromuscular system has more precise control of the joint in this constrained plane of movement in order to maintain joint stability. However, exactly whether more accurate proprioceptive acuity may have clinical impact is unknown. This is largely due to limited and inconsistent data regarding the relationship between proprioceptive acuity, as measured in isolated testing conditions, and neuromuscular control or functional performance (Friden et al. 2001). While some investigators have demonstrated a positive association between proprioceptive acuity and measures of functional ability (Fu and Hui-Chan 2007; Lin et al. 2009; Muaidi et al. 2009; van der Esch et al. 2007), others have not (Courtney and Rine 2006). Thus, though we observe a statistical difference in TDPM between planes, it is unknown whether this constitutes a functionally or clinically significant difference, especially considering the experimental limitations described above.
Functional neuromuscular control is a complex process involving the confluence of descending motor commands and sensory feedback. As described by Ashton-Miller et al. (2001) (Ashton-Miller et al. 2001), the contribution of proprioceptive processes to the improved performance of a functional task following training is often difficult to distinguish. Studies which assess the efficacy of proprioceptive training paradigms on function often do not evaluate proprioception before and after training (Hewett et al. 2006). Those that have measured proprioception before and after training have reported both improvements (Diracoglu et al. 2005) and no change (Risberg et al. 2007), indicating that this issue still requires further evaluation. Future studies which associate proprioceptive acuity to functional tasks (i.e. 3D gait kinematics and kinetics) are necessary to delineate the relative contribution of peripheral sensory feedback and may provide an indirect assessment of the clinical significance of the proprioceptive metric, particularly in pathological populations. Such examinations may guide the refinement of proprioceptive therapies and training programs aimed at managing musculoskeletal disorders.
Conclusions
To our knowledge this is the first examination of joint proprioception in the frontal plane of the knee. Understanding the three-dimensional proprioceptive capabilities of the knee joint may be useful in developing proprioceptive training protocols which are designed to improve joint stability in the constrained planes of movement as well as knee flexion/extension. Our results indicate lower TDPM values in the frontal plane compared with the sagittal plane of the knee. Though results are preliminary, they may suggest more accurate awareness of frontal plane movements, which may functionally relate to the limited range of motion in this direction compared with the sagittal plane and contribute to a protective neural mechanism designed to prevent injury. Future examinations are necessary to more fully characterize the differential proprioceptive acuity in the constrained planes of movement (both frontal and transverse planes) compared with the primary plane of movement at the knee.
From a clinical perspective, frontal plane knee joint proprioception may have implications in understanding the development of pathologies, such as knee osteoarthritis (OA) and ACL injury, which may be exacerbated by frontal plane loading (Astephen et al. 2008; Hewett et al. 2005; Jackson et al. 2004; Khan et al. 2008; Lewek et al. 2004; McLean et al. 2004; Sharma et al. 2003; Weidow et al. 2006). Our initial findings in young, healthy subjects provide baseline data of proprioceptive acuity in the frontal plane and can serve as the basis for future examination of three-dimensional proprioceptive acuity in patients with musculoskeletal disease or injury.
Acknowledgments
The authors would like to thank Charles David Stanford for his help with data collection and analysis. This work was supported by funding from the National Institutes of Health (R01 AR049837 and T32 HD007418), the Arthritis Foundation, and the Alpha Omicron Pi Foundation.
Footnotes
Communicated by Fausto Baldissera.
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Martha L. Cammarata, Email: m-cammarata@u.northwestern.edu, Department of Biomedical Engineering, Northwestern University, Evanston, IL, USA. Sensory Motor Performance Program, Rehabilitation Institute of Chicago, 345 E. Superior St. Rm 1406, Chicago, IL 60611, USA
Yasin Y. Dhaher, Department of Biomedical Engineering, Northwestern University, Evanston, IL, USA. Sensory Motor Performance Program, Rehabilitation Institute of Chicago, 345 E. Superior St. Rm 1406, Chicago, IL 60611, USA. Department of Physical Medicine and Rehabilitation, Northwestern University, Chicago, IL, USA
References
- Ageberg E, Flenhagen J, Ljung J. Test–retest reliability of knee kinesthesia in healthy adults. BMC Musculoskelet Disord. 2007;8:57. doi: 10.1186/1471-2474-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton-Miller JA, Wojtys EM, Huston LJ, Fry-Welch D. Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc. 2001;9:128–136. doi: 10.1007/s001670100208. [DOI] [PubMed] [Google Scholar]
- Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ, Hubley-Kozey CL. Gait and neuromuscular pattern changes are associated with differences in knee osteoarthritis severity levels. J Biomech. 2008;41:868–876. doi: 10.1016/j.jbiomech.2007.10.016. [DOI] [PubMed] [Google Scholar]
- Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med. 2005;39:324–329. doi: 10.1136/bjsm.2005.018341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- Boerboom AL, Huizinga MR, Kaan WA, Stewart RE, Hof AL, Bulstra SK, Diercks RL. Validation of a method to measure the proprioception of the knee. Gait Posture. 2008;28:610–614. doi: 10.1016/j.gaitpost.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Courtney CA, Rine RM. Central somatosensory changes associated with improved dynamic balance in subjects with anterior cruciate ligament deficiency. Gait Posture. 2006;24:190–195. doi: 10.1016/j.gaitpost.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Dhaher YY, Francis MJ. Determination of the abduction-adduction axis of rotation at the human knee: helical axis representation. J Orthop Res. 2006;24:2187–2200. doi: 10.1002/jor.20281. [DOI] [PubMed] [Google Scholar]
- Dhaher YY, Tsoumanis AD, Rymer WZ. Reflex muscle contractions can be elicited by valgus positional perturbations of the human knee. J Biomech. 2003;36:199–209. doi: 10.1016/s0021-9290(02)00334-2. [DOI] [PubMed] [Google Scholar]
- Dietz V, Quintern J, Sillem M. Stumbling reactions in man: significance of proprioceptive and preprogrammed mechanisms. J Physiol. 1987;386:149–163. doi: 10.1113/jphysiol.1987.sp016527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol. 2005;11:303–310. doi: 10.1097/01.rhu.0000191213.37853.3d. [DOI] [PubMed] [Google Scholar]
- Fagius J, Wahren LK. Variability of sensory threshold determination in clinical use. J Neurol Sci. 1981;51:11–27. doi: 10.1016/0022-510x(81)90056-3. [DOI] [PubMed] [Google Scholar]
- Fleiss JL. The design and analysis of clinical experiments. Wiley; New York: 1986. [Google Scholar]
- Friden T, Roberts D, Zatterstrom R, Lindstrand A, Moritz U. Proprioception in the nearly extended knee. Measurements of position and movement in healthy individuals and in symptomatic anterior cruciate ligament injured patients. Knee Surg Sports Traumatol Arthrosc. 1996;4:217–224. doi: 10.1007/BF01567966. [DOI] [PubMed] [Google Scholar]
- Friden T, Roberts D, Ageberg E, Walden M, Zatterstrom R. Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther. 2001;31:567–576. doi: 10.2519/jospt.2001.31.10.567. [DOI] [PubMed] [Google Scholar]
- Fu SN, Hui-Chan CW. Are there any relationships among ankle proprioception acuity, pre-landing ankle muscle responses, and landing impact in man? Neurosci Lett. 2007;417:123–127. doi: 10.1016/j.neulet.2007.01.068. [DOI] [PubMed] [Google Scholar]
- Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE, Jr, Hannafin JA, Hewett TE, Huston LJ, Ireland ML, Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, Myklebust G, Noyes FR, Powers C, Shields C, Jr, Shultz SJ, Silvers H, Slauterbeck J, Taylor DC, Teitz CC, Wojtys EM, Yu B. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34:1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- Grigg P, Greenspan BJ. Response of primate joint afferent neurons to mechanical stimulation of knee joint. J Neurophysiol. 1977;40:1–8. doi: 10.1152/jn.1977.40.1.1. [DOI] [PubMed] [Google Scholar]
- Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop Relat Res. 2002;402:76–94. doi: 10.1097/00003086-200209000-00008. [DOI] [PubMed] [Google Scholar]
- Hewett TE, Myer GD, Ford KR, Heidt RS, Jr, Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- Hurkmans EJ, van der Esch M, Ostelo RW, Knol D, Dekker J, Steultjens MP. Reproducibility of the measurement of knee joint proprioception in patients with osteoarthritis of the knee. Arthritis Rheum. 2007;57:1398–1403. doi: 10.1002/art.23082. [DOI] [PubMed] [Google Scholar]
- Jackson BD, Wluka AE, Teichtahl AJ, Morris ME, Cicuttini FM. Reviewing knee osteoarthritis—a biomechanical perspective. J Sci Med Sport. 2004;7:347–357. doi: 10.1016/s1440-2440(04)80030-6. [DOI] [PubMed] [Google Scholar]
- Khan FA, Koff MF, Noiseux NO, Bernhardt KA, O’Byrne MM, Larson DR, Amrami KK, Kaufman KR. Effect of local alignment on compartmental patterns of knee osteoarthritis. J Bone Joint Surg Am. 2008;90:1961–1969. doi: 10.2106/JBJS.G.00633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koralewicz LM, Engh GA. Comparison of proprioception in arthritic and age-matched normal knees. J Bone Joint Surg Am. 2000;82-A:1582–1588. doi: 10.2106/00004623-200011000-00011. [DOI] [PubMed] [Google Scholar]
- Lafortune MA, Cavanagh PR, Sommer HJ, 3rd, Kalenak A. Three-dimensional kinematics of the human knee during walking. J Biomech. 1992;25:347–357. doi: 10.1016/0021-9290(92)90254-x. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage. 2004;12:745–751. doi: 10.1016/j.joca.2004.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin DH, Lin CH, Lin YF, Jan MH. Efficacy of 2 non-weight-bearing interventions, proprioception training versus strength training, for patients with knee osteoarthritis: a randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:450–457. doi: 10.2519/jospt.2009.2923. [DOI] [PubMed] [Google Scholar]
- Macefield VG. Physiological characteristics of low-threshold mechanoreceptors in joints, muscle and skin in human subjects. Clin Exp Pharmacol Physiol. 2005;32:135–144. doi: 10.1111/j.1440-1681.2005.04143.x. [DOI] [PubMed] [Google Scholar]
- Macefield G, Gandevia SC, Burke D. Perceptual responses to microstimulation of single afferents innervating joints, muscles and skin of the human hand. J Physiol. 1990;429:113–129. doi: 10.1113/jphysiol.1990.sp018247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean SG, Huang X, Su A, Van Den Bogert AJ. Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech (Bristol, Avon) 2004;19:828–838. doi: 10.1016/j.clinbiomech.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Muaidi QI, Nicholson LL, Refshauge KM. Proprioceptive acuity in active rotation movements in healthy knees. Arch Phys Med Rehabil. 2008;89:371–376. doi: 10.1016/j.apmr.2007.08.154. [DOI] [PubMed] [Google Scholar]
- Muaidi QI, Nicholson LL, Refshauge KM, Adams RD, Roe JP. Effect of anterior cruciate ligament injury and reconstruction on proprioceptive acuity of knee rotation in the transverse plane. Am J Sports Med. 2009;37:1618–1626. doi: 10.1177/0363546509332429. [DOI] [PubMed] [Google Scholar]
- Pap G, Machner A, Nebelung W, Awiszus F. Detailed analysis of proprioception in normal and ACL-deficient knees. J Bone Joint Surg Br. 1999;81:764–768. doi: 10.1302/0301-620x.81b5.9352. [DOI] [PubMed] [Google Scholar]
- Rankin G, Stokes M. Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehabil. 1998;12:187–199. doi: 10.1191/026921598672178340. [DOI] [PubMed] [Google Scholar]
- Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002a;37:71–79. [PMC free article] [PubMed] [Google Scholar]
- Riemann BL, Lephart SM. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. J Athl Train. 2002b;37:80–84. [PMC free article] [PubMed] [Google Scholar]
- Riemann BL, Myers JB, Lephart SM. Sensorimotor system measurement techniques. J Athl Train. 2002;37:85–98. [PMC free article] [PubMed] [Google Scholar]
- Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87:737–750. doi: 10.2522/ptj.20060041. [DOI] [PubMed] [Google Scholar]
- Rozzi SL, Lephart SM, Gear WS, Fu FH. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med. 1999;27:312–319. doi: 10.1177/03635465990270030801. [DOI] [PubMed] [Google Scholar]
- Sainburg RL, Ghilardi MF, Poizner H, Ghez C. Control of limb dynamics in normal subjects and patients without proprioception. J Neurophysiol. 1995;73:820–835. doi: 10.1152/jn.1995.73.2.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48:3359–3370. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- van der Esch M, Steultjens M, Harlaar J, Knol D, Lems W, Dekker J. Joint proprioception, muscle strength, and functional ability in patients with osteoarthritis of the knee. Arthritis Rheum. 2007;57:787–793. doi: 10.1002/art.22779. [DOI] [PubMed] [Google Scholar]
- Weidow J, Tranberg R, Saari T, Karrholm J. Hip and knee joint rotations differ between patients with medial and lateral knee osteoarthritis: gait analysis of 30 patients and 15 controls. J Orthop Res. 2006;24:1890–1899. doi: 10.1002/jor.20194. [DOI] [PubMed] [Google Scholar]