Abstract
Background
The benefits of endoscopic testing for colorectal-cancer screening are uncertain. We evaluated the effect of screening with flexible sigmoidoscopy on colorectal-cancer incidence and mortality.
Methods
From 1993 through 2001, we randomly assigned 154,900 men and women 55 to 74 years of age either to screening with flexible sigmoidoscopy, with a repeat screening at 3 or 5 years, or to usual care. Cases of colorectal cancer and deaths from the disease were ascertained.
Results
Of the 77,445 participants randomly assigned to screening (intervention group), 83.5% underwent baseline flexible sigmoidoscopy and 54.0% were screened at 3 or 5 years. The incidence of colorectal cancer after a median follow-up of 11.9 years was 11.9 cases per 10,000 person-years in the intervention group (1012 cases), as compared with 15.2 cases per 10,000 person-years in the usual-care group (1287 cases), which represents a 21% reduction (relative risk, 0.79; 95% confidence interval [CI], 0.72 to 0.85; P<0.001). Significant reductions were observed in the incidence of both distal colorectal cancer (479 cases in the intervention group vs. 669 cases in the usual-care group; relative risk, 0.71; 95% CI, 0.64 to 0.80; P<0.001) and proximal colorectal cancer (512 cases vs. 595 cases; relative risk, 0.86; 95% CI, 0.76 to 0.97; P = 0.01). There were 2.9 deaths from colorectal cancer per 10,000 person-years in the intervention group (252 deaths), as compared with 3.9 per 10,000 person-years in the usual-care group (341 deaths), which represents a 26% reduction (relative risk, 0.74; 95% CI, 0.63 to 0.87; P<0.001). Mortality from distal colorectal cancer was reduced by 50% (87 deaths in the intervention group vs. 175 in the usual-care group; relative risk, 0.50; 95% CI, 0.38 to 0.64; P<0.001); mortality from proximal colorectal cancer was unaffected (143 and 147 deaths, respectively; relative risk, 0.97; 95% CI, 0.77 to 1.22; P = 0.81).
Conclusions
Screening with flexible sigmoidoscopy was associated with a significant decrease in colorectal-cancer incidence (in both the distal and proximal colon) and mortality (distal colon only). (Funded by the National Cancer Institute; PLCO ClinicalTrials.gov number, NCT00002540.)
Colorectal cancer is the second leading cause of cancer-related deaths in the United States.1 Colorectal-cancer mortality2-4 and incidence5,6 are reduced with screening by means of fecal occult-blood testing. Endoscopic screening with flexible sigmoidoscopy or colonoscopy is more sensitive than fecal testing for the detection of adenomatous polyps, the precursor lesions of colorectal cancer.7-9 Three European randomized trials of flexible sigmoidoscopy have been performed.10 In the United Kingdom, one time screening with flexible sigmoidoscopy significantly reduced the incidence of colorectal cancer (by 23%) and associated mortality (by 31%).11 In Italy, an 18% reduction in incidence and a nonsignificant 22% reduction in mortality were observed,12 whereas in Norway, no benefit was observed after 7 years of follow-up.13
In the United States, the multicenter, randomized Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial evaluated flexible sigmoidoscopy in comparison with usual care. Two screenings with flexible sigmoidoscopy were offered, 3 or 5 years apart. Previous reports have described the outcome from the first screening10 and the yield from both screenings.14 We report here on the effect of screening flexible sigmoidoscopy on the incidence of distal and proximal colorectal cancer and related mortality.
Methods
Study Design
A total of 154,900 men and women 55 to 74 years of age were enrolled from 1993 through 2001; they provided written informed consent and completed baseline questionnaires. The primary exclusion criteria were a history of prostate, lung, colorectal, or ovarian cancer; ongoing treatment for any type of cancer except basal-cell or squamous-cell skin cancer; and, beginning in 1995, assessment by means of a lower endoscopic procedure (flexible sigmoidoscopy, colonoscopy, or barium enema examination) in the previous 3 years. Further details, including data on recruitment through mass mailing, have been reported previously.15,16 Randomization was performed in blocks stratified according to screening center, age, and sex. The study was sponsored by the National Cancer Institute. All the authors vouch for the accuracy of the data and the fidelity of the study to the protocol. The protocol and statistical analysis plan are available with the full text of this article at NEJM.org.
Participants in the intervention group were offered flexible sigmoidoscopy at baseline and at 3 years (for those who underwent randomization before April 1995) or at 5 years. Repeat screening in persons who received a diagnosis of colorectal cancer or adenoma after the initial screening was discouraged but did occur14 (see Fig. S1 in the Supplementary Appendix, available at NEJM.org). Physicians and nurse examiners followed standardized procedures for flexible sigmoidoscopic examinations. An examination was considered to be positive if a polyp or mass was detected. Biopsies were not routinely performed. Participants were referred to their primary care physicians for decisions regarding diagnostic follow-up. Medical records related to follow-up, a diagnosis of cancer, and cancer complications were collected.
Death from colorectal cancer was the primary end point. Secondary end points included colorectal-cancer incidence, cancer stage, survival, harms of screening, and all-cause mortality. All cancers and deaths were ascertained primarily by means of a mailed Annual Study Update questionnaire. Participants who did not return questionnaires were contacted by repeat mailing or telephone. Cancer incidence, stage, and location were verified from medical records.17 Information on vital status was supplemented by periodic linkage to the National Death Index. Deaths that were potentially related to prostate, lung, colorectal, or ovarian cancer were reviewed in a blinded fashion, in an end-point adjudication process.18 Colorectal-cancer deaths included deaths due to colorectal cancer and those due to its treatment. Carcinoid tumors were included as colorectal-cancer cases. Cancers located in the rectum through the splenic flexure were defined as distal, and those in the transverse colon through the cecum were defined as proximal. A screening-detected cancer was defined as a colorectal cancer diagnosed within 1 year after a positive flexible sigmoidoscopic examination.
Assessment of Study-Group Contamination
Colorectal screening with flexible sigmoidoscopy or colonoscopy outside the study protocol, performed for routine care (contamination), was assessed with the use of biennially and, later, annually administered health-status questionnaires. In total, 13,788 randomly selected participants (10,077 in the usual-care group and 3711 in the intervention group) were included in the analysis. Verification of reported procedures was not obtained. To estimate contamination in the usual-care group during the screening phase (study years 0 through 5), we determined the proportion of participants at study years 5 and 6 who reported having undergone routine endoscopic testing in the previous 5 years. Contamination by colonoscopy in the intervention group during the screening phase was defined as routine colonoscopy in participants without a positive flexible sigmoidoscopic examination and was estimated from reports on colonoscopy in a subgroup of 1392 participants in the intervention group.19,20 To estimate use of colonoscopy after the screening phase, we determined the proportion of participants in each group in study years 11 through 13 who reported having undergone routine colonoscopic testing in the previous 5 years.
Statistical Analysis
The primary analysis was an intention-to-screen comparison of colorectal-cancer mortality between the study groups. Event rates were defined as the number of events (cancers or deaths) divided by person-years. For mortality, person-years were measured from randomization to the date of death or the date of last follow-up (censoring date), and for incidence, person-years were measured from randomization to the date of diagnosis, death, or censoring, whichever came first. Data were censored on December 31, 2009, or at 13 years from randomization, whichever came first.
The trial was designed to have 90% power to detect a 15% or greater relative reduction in colorectal-cancer mortality in the intervention group, as compared with the usual-care group, on the assumption of at least 85% compliance with screening in the intervention group and no more than 15% contamination among participants in the usual-care group.15
We calculated the pointwise confidence intervals for incidence-rate and mortality ratios assuming a Poisson distribution for the number of events and, through asymptotic methods, a normal distribution for the logarithm of the ratio.21 The number needed to invite for screening to prevent one colorectal-cancer death or case was defined as the number of intervention-group participants divided by the difference in colorectal-cancer deaths or cases between groups. The adjusted, sequential P value and confidence interval for the colorectal-cancer mortality ratio were derived in accordance with the sequential design and the weighted method used to monitor the trial, which allows for a varying rate ratio.22 An interim analysis plan was used to monitor the primary end point for efficacy and futility. We assessed the between-group difference in mortality with the use of a weighted log-rank test, incorporating increasing weights that were proportional to the pooled mortality. The weighted statistic was chosen because of the presumed delay in the effect of screening on colorectal-cancer mortality. The monitoring design stipulated a one-sided efficacy boundary, constructed by means of the Lan–DeMets procedure with an O'Brien–Fleming spending function,23 and a nonbinding futility boundary was constructed with the use of stochastic curtailment24 (see the Supplementary Appendix). All analyses were performed with SAS/STAT software, version 9 (SAS Institute),25 or R software, version 2.12.0 (R Development Core Team).26
Results
Characteristics of the Participants and Use of Screening
A total of 77,445 participants were randomly assigned to flexible sigmoidoscopy, and 77,455 to usual care. The baseline characteristics of the participants were similar in the two study groups (Table 1); the median follow-up time was 11.9 years, and the mean follow-up time was 11.0 years. Vital status within a year after the data-cutoff date was known for 99.9% of participants, and compliance with the Annual Study Update questionnaire was 93.8%. Randomization and follow-up are shown in Figure S1 in the Supplementary Appendix.
Table 1.
Characteristics of the Study Participants.*
| Characteristic | Flexible-Sigmoidoscopy Group (N = 77,445) | Usual-Care Group (N = 77,455) |
| no. of participants (%) | ||
| Sex | ||
| Female | 39,105 (50.5) | 39,111 (50.5) |
| Male | 38,340 (49.5) | 38,344 (49.5) |
| Age | ||
| 55–59 yr | 25,851 (33.4) | 25,839 (33.4) |
| 60–64 yr | 23,783 (30.7) | 23,771 (30.7) |
| 65–69 yr | 17,457 (22.5) | 17,473 (22.6) |
| 70–74 yr | 10,354 (13.4) | 10,372 (13.4) |
| Race or ethnic group† | ||
| White (non-Hispanic) | 66,874 (86.4) | 65,708 (84.8) |
| Black (non-Hispanic) | 3,883 (5.0) | 3,825 (4.9) |
| Hispanic | 1,421 (1.8) | 1,397 (1.8) |
| Asian | 2,791 (3.6) | 2,785 (3.6) |
| Other or unknown | 2,476 (3.2) | 3,740 (4.8) |
| Educational level | ||
| High-school graduate or less | 22,892 (29.6) | 22,583 (29.2) |
| Some college | 25,935 (33.5) | 25,585 (33.0) |
| College graduate | 26,659 (34.4) | 25,915 (33.5) |
| Unknown | 1,959 (2.5) | 3,372 (4.4) |
| Prior FOBT‡ | ||
| Yes | 29,244 (37.8) | 29,890 (38.6)§ |
| No | 43,858 (56.6) | 42,223 (54.5) |
| Unknown | 4,343 (5.6) | 5,342 (6.9) |
| Prior lower GI endoscopy¶ | ||
| Yes | 9,736 (12.6) | 10,113 (13.1)§ |
| No | 64,653 (83.5) | 62,997 (81.3) |
| Unknown | 3,056 (3.9) | 4,345 (5.6) |
| Either prior FOBT or prior lower GI endoscopy | ||
| Yes | 31,511 (40.7) | 31,990 (41.3)§ |
| No | 40,648 (52.5) | 39,161 (50.6) |
| Unknown | 5,286 (6.8) | 6,304 (8.1) |
| First-degree relative with colorectal cancer | ||
| Yes | 7,643 (9.9) | 7,322 (9.5) |
| No | 65,299 (84.3) | 64,506 (83.3) |
| Unknown | 4,503 (5.8) | 5,627 (7.3) |
| Daily use of aspirin or ibuprofen in past 12 mo | ||
| Yes | 24,822 (32.1) | 23,949 (30.9)‖ |
| No | 50,368 (65.0) | 49,766 (64.3) |
| Unknown | 2,255 (2.9) | 3,740 (4.8) |
| Aspirin or ibuprofen use ≥3–4 times per wk in past 12 mo | ||
| Yes | 33,248 (42.9) | 32,087 (41.4)** |
| No | 41,971 (54.2) | 41,658 (53.8) |
| Unknown | 2,226 (2.9) | 3,710 (4.8) |
There were no significant differences between the groups except as noted. FOBT denotes fecal occult-blood test, and GI gastrointestinal.
Race or ethnic group was determined by self-report.
Prior FOBT indicates a test within 3 years before study entry.
P<0.001
Prior lower GI endoscopy indicates sigmoidoscopy, colonoscopy, or barium enema examination within 3 years before randomization.
P = 0.03
P = 0.01
In the intervention group, 83.5% of the participants (64,653) underwent baseline screening and 54.0% (41,858) underwent subsequent screening. A total of 86.6% of participants (67,071) underwent at least one flexible sigmoidoscopic screening, and 50.9% (39,440) underwent two screenings; in 28.5% of participants (22,083), at least one screening was positive for a polyp or mass. Of participants with abnormal screening results, 80.5% underwent a diagnostic intervention within 1 year, 95.6% of whom underwent colonoscopy; the rate of colonoscopy performed as a direct effect of screening with flexible sigmoidoscopy was 21.9%.
Colorectal-Cancer Incidence and Mortality According to Study Group
Table 2 shows colorectal-cancer incidence and mortality in the intervention group as compared with the usual-care group. The incidence of colorectal cancer was 11.9 cases per 10,000 person-years in the intervention group (1012 cases), as compared with 15.2 cases per 10,000 person-years in the usual-care group (1287 cases), which represents a 21% reduction (relative risk, 0.79; 95% confidence interval [CI], 0.72 to 0.85; P<0.001). Significant reductions were observed in the incidence of both distal colorectal cancer (479 cases in the intervention group vs. 669 cases in the usual-care group; relative risk, 0.71; 95% CI, 0.64 to 0.80; P<0.001) and proximal colorectal cancer (512 cases vs. 595 cases; relative risk, 0.86; 95% CI, 0.76 to 0.97; P = 0.01). The relative risk of colorectal cancer among men was 0.73 (95% CI, 0.66 to 0.82) and among women 0.86 (95% CI, 0.76 to 0.98), with a borderline significant interaction between sex and study-group assignment (P = 0.052). The reduction in the incidence of colorectal cancer was similar for participants 55 to 64 years of age (518 cases vs. 662 cases; relative risk, 0.78; 95% CI, 0.69 to 0.87) and for those 65 to 74 years of age (494 cases vs. 625 cases, relative risk, 0.79; 95% CI, 0.71 to 0.89). The number needed to invite for screening in order to prevent 1 case of colorectal cancer was 282 (95% CI, 210 to 427).
Table 2.
Colorectal-Cancer Incidence and Mortality.*
| Variable | Flexible-Sig moidoscopy Group (N = 77,445) | Usual-Care Group (N = 77,455) | Relative Risk (95% CI) | P Value | ||
|---|---|---|---|---|---|---|
| no. of participants | rate per 10,000 person-yr (95% CI) | no. of participants | rate per 10,000 person-yr (95% CI) | |||
| Incidence | ||||||
| All colorectal cancers | 1012 | 11.9 (11.2–12.7) | 1287 | 15.2 (14.4–16.0) | 0.79 (0.72–0.85) | <0.001 |
| Location of cancer† | ||||||
| Distal | 479 | 5.6 (5.1–6.2) | 669 | 7.9 (7.3–8.5) | 0.71 (0.64–0.80) | <0.001 |
| Proximal | 512 | 6.0 (5.5–6.6) | 595 | 7.0 (6.5–7.6) | 0.86 (0.76–0.97) | 0.01 |
| Sex | ||||||
| Male | 567 | 13.6 (12.4–14.7) | 768 | 18.5 (17.2–19.9) | 0.73 (0.66–0.82) | <0.001 |
| Female | 445 | 10.3 (9.4–11.3) | 519 | 12.0 (11.0–13.0) | 0.86 (0.76–0.98) | 0.02 |
| Age at randomization | ||||||
| 55–64 yr | 518 | 9.4 (8.6–10.2) | 662 | 12.1 (11.2–13.0) | 0.78 (0.69–0.87) | <0.001 |
| 65–74 yr | 494 | 16.6 (15.1–18.1) | 625 | 20.9 (19.3–22.5) | 0.79 (0.71–0.89) | <0.001 |
| Mortality | ||||||
| All colorectal-cancer deaths | 252 | 2.9 (2.5–3.2) | 341 | 3.9 (3.5–4.3) | 0.74 (0.63–0.87) | <0.001 |
| Location of cancer† | ||||||
| Distal | 87 | 1.0 (0.8–1.2) | 175 | 2.0 (1.7–2.3) | 0.50 (0.38–0.64) | <0.001 |
| Proximal | 143 | 1.6 (1.4–1.9) | 147 | 1.7 (1.4–2.0) | 0.97 (0.77–1.22) | 0.81 |
| Sex | ||||||
| Male | 139 | 3.2 (2.7–3.8) | 211 | 4.9 (4.3–5.6) | 0.66 (0.53–0.81) | <0.001 |
| Female | 113 | 2.6 (2.1–3.0) | 130 | 2.9 (2.4–3.4) | 0.87 (0.68–1.12) | 0.28 |
| Age at randomization | ||||||
| 55–64 yr | 133 | 2.4 (2.0–2.8) | 157 | 2.8 (2.3–3.2) | 0.84 (0.67–1.06) | 0.16 |
| 65–74 yr | 119 | 3.9 (3.2–4.6) | 184 | 6.0 (5.1–6.9) | 0.65 (0.52–0.82) | <0.001 |
The median follow-up time for incidence was 11.9 years (interquartile range, 10.2 to 13.0) and for mortality was 12.1 years (interquartile range, 10.4 to 13.0).
Distal location was defined as the rectum through the splenic flexure, and proximal as the transverse colon through the cecum. For incidence, the location was unknown for 21 cases in the flexible-sigmoidoscopy group and 23 cases in the usual-care group. For mortality, the location was unknown for 22 deaths in the flexible-sigmoidoscopy group and 19 deaths in the usual-care group.
Mortality related to colorectal cancer was 2.9 per 10,000 person-years in the intervention group (252 deaths), as compared with 3.9 per 10,000 person-years in the usual-care group (341 deaths), which represents a 26% reduction (relative risk, 0.74; 95% CI, 0.63 to 0.87; P<0.001). Mortality related to distal colorectal cancer was reduced by 50% (87 deaths in the intervention group vs. 175 in the usual-care group; relative risk, 0.50; 95% CI, 0.38 to 0.64; P<0.001), but mortality related to proximal colorectal cancer (143 vs. 147 deaths, respectively; relative risk, 0.97; 95% CI, 0.77 to 1.22; P = 0.81) was unaffected. Men had a 34% reduction in colorectal cancer mortality (139 vs. 211 deaths; relative risk, 0.66; 95% CI, 0.53 to 0.81) and women a 13% reduction (113 vs. 130 deaths; relative risk, 0.87; 95% CI, 0.68 to 1.12); the interaction between sex and study-group assignment was not significant (P = 0.10). The relative risks for colorectal-cancer mortality among participants 55 to 64 years of age and 65 to 74 years of age were 0.84 (95% CI, 0.67 to 1.06) and 0.65 (95% CI, 0.52 to 0.82), respectively (P = 0.11 for the interaction between age and study-group assignment). The number needed to invite for screening in order to prevent 1 colorectal-cancer death was 871 (95% CI, 567 to 1874).
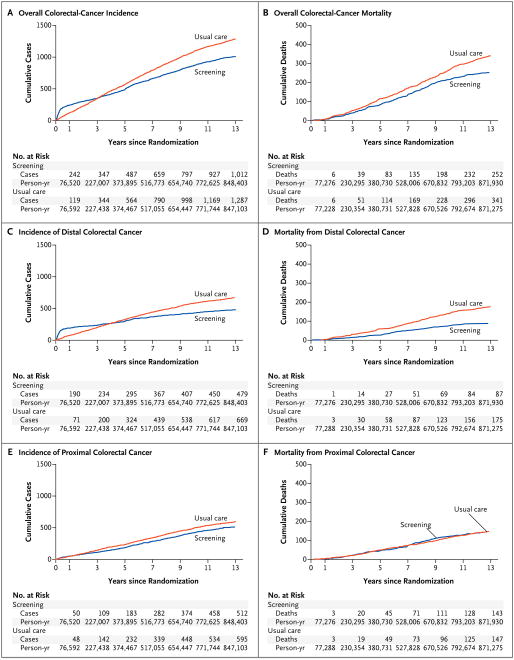
The cumulative incidences of overall and distal colorectal cancer were higher in the intervention group through approximately 3 years, after which cumulative incidences became lower in the intervention group (Fig. 1A and 1C). The cumulative incidences of proximal colorectal cancer (Fig. 1E) were similar for the first few years but became and remained lower after year 3 in the intervention group. Overall colorectal-cancer mortality and mortality related to distal and to proximal colorectal cancer are shown in Figure 1B, 1D, and 1F. Between-group differences in mortality emerged within a few years and persist for total and distal colorectal cancer, but no difference in mortality related to proximal colorectal cancer was observed.
Figure 1.
Overall, Distal, and Proximal Colorectal-Cancer Incidence and Mortality.
Incidence and Stage of Cancer According to Means of Detection
Table 3 shows colorectal-cancer incidence and stage according to the means of detection. Screening-detected cancers accounted for 24.1% of colorectal cancers (244 of 1012) in the intervention group. Among participants with screening-detected cancers, 82.8% of the cancers were distal, whereas among participants who were never screened, 52.8% were distal, and among participants with cancers not detected by screening, 31.6% were distal (P<0.001). Participants with screening-detected cancers were more likely to have early-stage cancer (stage I or II) than participants who were never screened or those whose tumors were not detected by screening (75.4% vs. 50.9% and 50.7%, respectively; P<0.001 for both comparisons).
Table 3.
Colorectal-Cancer Incidence and Stage According to Means of Detection.
| Flexible Sigmoidoscopy Group (N = 77,445) | Usual-Care Group (N = 77,455) | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Screening-Detected Cancer | Non–Screening -Detected Cancer | Total | Total | |||
| In Screened Participants* | In Unscreened Participants† | ||||||
| no. at baseline | no. at yr 3 or 5 | total no. (%) | number (percent) | ||||
| All colorectal cancers | 192 | 52 | 244 (100.0) | 607 (100.0) | 161 (100.0) | 1012 (100.0) | 1287 (100.0) |
| Location | |||||||
| Distal | 165 | 37 | 202 (82.8) | 192 (31.6) | 85 (52.8) | 479 (47.3) | 669 (52.0) |
| Proximal | 26 | 15 | 41 (16.8) | 403 (66.4) | 68 (42.2) | 512 (50.6) | 595 (46.2) |
| Unknown | 1 | 0 | 1 (0.4) | 12 (2.0) | 8 (5.0) | 21 (2.1) | 23 (1.8) |
| Sex | |||||||
| Male | 136 | 33 | 169 (69.3) | 324 (53.4) | 74 (46.0) | 567 (56.0) | 768 (59.7) |
| Female | 56 | 19 | 75 (30.7) | 283 (46.6) | 87 (54.0) | 445 (44.0) | 519 (40.3) |
| Stage | |||||||
| I | 113 | 33 | 146 (59.8) | 148 (24.4) | 40 (24.8) | 334 (33.0) | 407 (31.6) |
| II | 31 | 7 | 38 (15.6) | 160 (26.4) | 42 (26.1) | 240 (23.7) | 309 (24.0) |
| III | 24 | 6 | 30 (12.3) | 168 (27.7) | 43 (26.7) | 241 (23.8) | 328 (25.5) |
| IV | 5 | 3 | 8 (3.3) | 107 (17.6) | 25 (15.5) | 140 (13.8) | 209 (16.2) |
| Carcinoid | 17 | 3 | 20 (8.2) | 10 (1.6) | 2 (1.2) | 32 (3.2) | 9 (0.7) |
| Unknown | 2 | 0 | 2 (0.8) | 14 (2.3) | 9 (5.6) | 25 (2.5) | 25 (1.9) |
This category includes participants who underwent at least one screening flexible sigmoidoscopic examination and who had cancers that were detected because of symptoms, detected by screening performed outside the study protocol, or detected more than 1 year after a positive screening examination.
This category includes participants who did not undergo a screening flexible sigmoidoscopic examination and who had cancers that were detected because of symptoms or detected by screening performed outside the study protocol.
Incidence and Mortality According to Location and Stage of Cancer
Table 4 shows colorectal-cancer incidence and mortality according to the location in the colon and the stage at diagnosis. Case fatality rates for stage I, II, III, and IV cancers were similar in the intervention and usual-care groups and were approximately 6%, 11%, 30%, and 79%, respectively. There was a reduction in the incidence of distal colorectal cancer in the intervention group for each cancer stage, ranging from 19.8% for stage I cancers (50 fewer cases) to 61.7% for stage IV cancers (66 fewer cases). Mortality related to distal colorectal cancer was also reduced for each stage, by 21.4% for stage I cancers (3 fewer deaths) to 60.7% for stage IV cancers (51 fewer deaths). The incidence of cancer in the proximal colon was reduced by 14.4 to 20.7% in the intervention group for stage I, II, and III cancers (22, 34, and 25 fewer cases, respectively) but by only 2.0% (2 fewer cases) for stage IV disease. The number of deaths from proximal colorectal cancer was similar in the two groups. Overall, there were only 4 fewer deaths from proximal colorectal cancer in the intervention group. Because of the relative paucity of cancers in the descending colon and splenic flexure (Table S2 in the Supplementary Appendix), limiting the definition of distal cancer to cancers in the rectum and sigmoid had little effect on the incidence or mortality results.
Table 4.
Colorectal-Cancer Incidence and Mortality According to Location and Stage.
| Variable | Cancer Stage | Total | |||||
|---|---|---|---|---|---|---|---|
| I | II | III | IV | Carcinoid | Unknown | ||
| Flexible-sigmoidoscopy group | |||||||
| Cases of colorectal cancer — no. | 334 | 240 | 241 | 140 | 32 | 25 | 1012 |
| Deaths from colorectal cancer — no. (%) | 20 (6.0) | 26 (10.8) | 70 (29.0) | 113 (80.7) | 3 (9.4) | 20 (80.0) | 252 (24.9) |
| Cases of distal colorectal cancer — no. | 202 | 110 | 96 | 41 | 24 | 6 | 479 |
| Deaths from distal colorectal cancer — no. (%) | 11 (5.4) | 15 (13.6) | 28 (29.2) | 33 (80.5) | 0 | 0 | 87 (18.2) |
| Cases of proximal colorectal cancer — no. | 131 | 130 | 145 | 96 | 8 | 2 | 512 |
| Deaths from proximal colorectal cancer — no. (%) | 9 (6.9) | 11 (8.5) | 42 (29.0) | 78 (81.2) | 3 (37.5) | 0 | 143 (27.9) |
| Usual-care group | |||||||
| Cases of colorectal cancer — no. | 407 | 309 | 328 | 209 | 9 | 25 | 1287 |
| Deaths from colorectal cancer — no. (%) | 21 (5.2) | 33 (10.7) | 102 (31.1) | 163 (78.0) | 4 (44.4) | 18 (72.0) | 341 (26.5) |
| Cases of distal colorectal cancer — no. | 252 | 144 | 157 | 107 | 3 | 6 | 669 |
| Deaths from distal colorectal cancer — no. (%) | 14 (5.6) | 25 (17.4) | 50 (31.8) | 84 (78.5) | 1 (33.3) | 1 (16.7) | 175 (26.2) |
| Cases of proximal colorectal cancer — no. | 153 | 164 | 170 | 98 | 6 | 4 | 595 |
| Deaths from proximal colorectal cancer — no. (%) | 7 (4.6) | 8 (4.9) | 52 (30.6) | 77 (78.6) | 3 (50.0) | 0 | 147 (24.7) |
| Between-group differences* | |||||||
| Distal colorectal cancer | |||||||
| Cases — no. (% reduction in incidence) | 50 (19.8) | 34 (23.6) | 61 (38.9) | 66 (61.7) | -21 (-700.0) | 0 | 190 |
| Deaths — no. (% reduction in mortality) | 3 (21.4) | 10 (40.0) | 22 (44.0) | 51 (60.7) | 1 (100.0) | 1 (100.0) | 88 |
| Proximal colorectal cancer | |||||||
| Cases — no. (% reduction in incidence) | 22 (14.4) | 34 (20.7) | 25 (14.7) | 2 (2.0) | −2 (−33.3) | 2 (50.0) | 83 |
| Deaths — no. (% reduction in mortality) | −2 (−8.6) | −3 (−37.5) | 10 (19.2) | −1 (−1.3) | 0 | 0 | 4 |
Differences in cases and deaths were calculated as the number in the usual-care group minus the number in the flexible-sigmoidoscopy group. The percentage difference was calculated as 100 – [(flexible-sigmoidoscopy rate ÷ usual-care rate) × 100]. The flexible-sigmoidoscopy rate was defined as cases in the flexible-sigmoidoscopy group divided by the flexible-sigmoidoscopy population, and the usual-care rate as cases in the usual-care group divided by the usual-care population.
Cancer Treatment, Screening Complications and False Positive Results, and Deaths from Other Causes
The rates of administered treatment for colorectal cancer with surgery, chemotherapy, or radiation therapy were similar overall and according to cancer stage in the two groups (Table S1 in the Supplementary Appendix).
There were 3 bowel perforations, 2 by the same operator, in 107,236 flexible sigmoidoscopic examinations (2.8 per 100,000). Among participants with a positive flexible sigmoidoscopic examination and no cancer detected on follow-up, there were 19 perforations during 17,672 subsequent diagnostic or therapeutic colonoscopic examinations (107.5 per 100,000). False positive results of sigmoidoscopy, with no neoplasia identified at subsequent diagnostic testing, were observed among 20% of men and 13% of women.27 Some of the false positive sigmoidoscopic examinations may have been due to false negative results of colonoscopy. Deaths from other causes, excluding prostate, lung, colorectal, and ovarian cancers, totaled 9138 (11.8%) in the intervention group and 9286 (12.0%) in the usual-care group (relative risk, 0.98; 95% CI, 0.96 to 1.01; P = 0.28) (Table S3 in the Supplementary Appendix).
Endoscopic Contamination
The estimated rate of endoscopic contamination in the usual-care group during the screening phase was 25.8% (95% CI, 23.6 to 28.0) for flexible sigmoidoscopy, 34.4% (95% CI, 32.0 to 36.8) for colonoscopy, and 46.5% (95% CI, 43.9 to 49.1) for either flexible sigmoidoscopy or colonoscopy. The rate of colonoscopy in the intervention group during the screening phase by participants without a positive screening examination was 5.5% (95% CI, 4.5 to 6.5). The rate of routine colonoscopy after the screening phase was 47.7% (95% CI, 44.7 to 50.7) in the intervention group and 48.0% (95% CI, 45.2 to 50.8) in the usual-care group.
Discussion
In this randomized study, flexible sigmoidoscopy, as compared with usual care, was associated with a 26% reduction in overall colorectal-cancer mortality and a 21% reduction in the incidence of colorectal cancer. Mortality related to distal colorectal cancer was reduced by 50%, and the incidence was reduced by 29%. A significant 14% reduction in the incidence of proximal colorectal cancer was observed, but there was no significant reduction in mortality related to proximal cancer. The baseline characteristics, rate and time of follow-up, treatment, and deaths according to cancer stage were similar in the two study groups, findings that suggest similarities in the underlying risk, biologic features of the cancers, and treatment outcome. These results provide strong support for the observed benefit as being directly attributable to sigmoidoscopic screening.
The observed reductions in incidence and mortality are similar to the results of the United King-dom11 and Italian12 studies of flexible sigmoidoscopy. Although the end results of these trials are similar, there are notable differences among the studies in enrollment criteria, compliance, screening frequency, and the use of endoscopic screening outside the protocol. In the United Kingdom study, a single flexible sigmoidoscopic screening for participants 55 to 64 years of age was performed. In the PLCO trial, two screenings were offered, and participants ranged from 55 to 74 years of age. In the United Kingdom study, 71.2% of participants underwent a screening examination, whereas in the PLCO trial, 86.6% underwent at least one screening. In the PLCO trial, the second screening increased the cumulative diagnostic yield of cancer or advanced adenoma by 26% among women and 34% among men.14 However, we cannot measure the incremental benefit of the second examination on colorectal-cancer incidence or mortality.
In the United States, endoscopic screening has been widely endorsed,28,29 and population-based data show an increase in use.30 We identified substantial use of flexible sigmoidoscopy and colonoscopy in the usual-care group during the time that the intervention group was undergoing screening and in both groups during follow-up after screening. This testing probably reduced the difference in mortality and incidence between the two groups. However, screening in the PLCO trial was performed primarily in the first study year, when 83.5% of participants were screened, whereas in the usual-care group, testing accumulated over time. In conjunction with the European trials,11,12 our study confirms that flexible sigmoidoscopy substantially reduces colorectal-cancer incidence and mortality, especially with regard to distal colorectal cancer.
Observational studies have raised doubts about the benefit of endoscopic screening in reducing mortality31,32 from and the incidence33,34 of proximal colorectal cancer. There is a lesser degree of protection against cancer in the proximal colon than in the distal colon.31-36 In the United Kingdom trial of flexible sigmoidoscopy, the benefit with regard to colorectal-cancer incidence and mortality was limited to the distal colon, but only 5% of participants underwent colonoscopy.11 In the Italian study, 8.4% of participants were referred for colonoscopy,12 and the reductions in the incidence of proximal colorectal cancer (9%) and related mortality (15%) were not significant. In the PLCO trial, we found a significant reduction in the incidence of proximal colorectal cancer. This effect was achieved with a colonoscopy rate of 21.9% as a direct effect of abnormal screening results of flexible sigmoidoscopy, in addition to colonoscopy occurring outside the screening protocol and after the screening period. We did not observe a reduction in mortality related to proximal colorectal cancer. Much of the benefit in reducing colorectal-cancer mortality from screening derives from a reduction in stage IV disease,4 which has a much higher mortality than lower stages. In the PLCO trial, 79.1% of participants with stage IV disease died of colorectal cancer. For cancers in the distal colon, reductions of more than 60% in the incidence of stage IV disease and related mortality were observed. In contrast, for cancers in the proximal colon, no significant reductions in the incidence of stage IV disease or related mortality were identified. Furthermore, in the intervention group, tumors that were not detected by screening were more likely to be proximal and at a later stage than screening-detected tumors (Table 3).37
As compared with the distal colon, the proximal colon poses a more difficult challenge for colorectal-cancer control because of limitations in bowel preparation, a greater prevalence of advanced serrated adenomas, which are harder to detect than conventional adenomas,38,39 and biologic differences, including a greater incidence of BRAF mutation,39 microsatellite instability,38,40 and CpG island methylator phenotype (CIMP).40 Although our protocol was associated with a reduction in the incidence of proximal colorectal cancer, presumably because of the detection and removal of precursor adenomas that would otherwise have progressed to cancer, it apparently did not succeed in identifying and successfully removing a proportionally greater number of precursor lesions destined to develop into fatal colorectal cancers. We have estimated that using colonoscopy rather than flexible sigmoidoscopy as the screening method in the PLCO trial would have increased the number of screening-detected cancers by approximately 16 percentage points (from <25% to approximately 40% of colorectal cancers diagnosed in participants assigned to flexible sigmoidoscopy) and that two thirds of that increase would have been attributable to increased detection of proximal colorectal cancer.37 The effect on the incidence of proximal colorectal cancer and related mortality of the additional polyp removal with universal colonoscopy is not known.
The effectiveness of flexible sigmoidoscopy in reducing mortality related to distal colorectal cancer reflects the reduction in cancer incidence, or the reduced number of tumors that could have resulted in death, and the identification of earlier-stage tumors, which are less likely to cause death than later-stage tumors. Screening-detected cancers, though accounting for less than 25% of tumors in the intervention group, were distinctly and predominantly at an early stage (Table 3).37
Although the trial was not powered to detect the effect of sigmoidoscopic screening on colorectal-cancer mortality and incidence in subgroups, the results are suggestive of a stronger effect among men than among women. This finding may be due to the fact that women had a lower proportion of screening-detected cancers (Table 3) and a higher proportion of proximal colorectal cancers than men.37 A significant differential effect between the screening of participants 55 to 64 years of age and those 65 to 74 years of age was not observed.
Our results can be compared with those of the Minnesota trial of fecal occult-blood testing. After 13 years of follow-up, with six rounds of fecal occult-blood testing and a 38% rate of colonoscopy in the annually screened group, colorectal-cancer incidence was reduced by 12% (a nonsignificant difference) and mortality by 33% (a significant difference).41 In the PLCO trial, after a median follow-up of 11.9 years with up to two flexible sigmoidoscopic screenings in addition to screenings outside the protocol in both groups, incidence was reduced by 21% and mortality by 26%. Endoscopic testing appears to have a more potent protective effect than fecal occult-blood testing in reducing the incidence of colorectal cancer and requires fewer rounds of testing, presumably because endoscopic testing detects more precursor adenomas.7-9 However, whether endoscopic evaluation is a better screening test depends on the population and available resources.
In conclusion, screening with flexible sigmoidoscopy, in conjunction with colonoscopy (predominantly) for diagnosis and management after abnormal test results, was associated with a significant and clinically important decrease in colorectal-cancer incidence and mortality. The incidence of colorectal cancer was reduced in both the distal and proximal colon. A significant reduction in mortality was observed only for cancer in the distal colon.
Supplementary Material
Acknowledgments
Supported by contracts from the Division of Cancer Prevention, National Cancer Institute, to the 10 screening centers and to the coordinating center (N01-CN-25476, to Westat; N01-CN-25511, to the University of Pittsburgh Cancer Institute; N01-CN-25512, to Henry Ford Health System; N01-CN-25513, to the University of Minnesota School of Public Health; N01-CN-25514, to the University of Colorado; N01-CN-25515, to Pacific Health Research and Education Institute; N01-CN-25516, to Washington University; N01-CN-25518, to Marshfield Clinic Research Foundation; N01-CN-25522, to Georgetown University Medical Center; N01-CN-25524, to the University of Utah; and N01-CN-75022, to the University of Alabama at Birmingham).
Dr. Andriole reports receiving consulting fees, payment for the development of presentations, and payment for travel, accommodation, and meeting expenses from Amgen; consulting fees, stock options, and payment for travel, accommodation, and meeting expenses from Augmenix; consulting fees and payment for travel, accommodation, and meeting expenses from Bayer; consulting fees and payment for travel, accommodation, and meeting expenses from Bristol-Myers Squibb; consulting fees, stock options, and payment for travel, accommodation, and meeting expenses from Cambridge Endo; consulting fees and payment for travel, accommodation, and meeting expenses from Caris; consulting fees and payment for travel, accommodation, and meeting expenses from GlaxoSmithKline; consulting fees and payment for travel, accommodation, and meeting expenses from Janssen Biotech; consulting fees and payment for travel, accommodation, and meeting expenses from Myriad Genetics; consulting fees and payment for travel, accommodation, and meeting expenses from Steba Biotech; consulting fees and payment for travel, accommodation, and meeting expenses from Ortho Clinical Diagnostics; consulting fees and stock options from Viking Medical; royalties from UpToDate and Year Book of Urology; stock options from Envisioneering Medical; and grant support to his institution from Johnson & Johnson, Medivation, and Wilex; and being a member of an independent data monitoring committee for Amarex. Dr. Schoen reports receiving stock options from Onconome.
Appendix
The authors' affiliations are as follows: the Departments of Medicine (R.E.S.) and Epidemiology (R.E.S., J.L.W.), University of Pittsburgh, and the University of Pittsburgh Cancer Institute (R.E.S., J.L.W.), Pittsburgh; the Divisions of Cancer Prevention (P.F.P., G.I., B.S.K., P.C.P., C.D.B.) and Cancer Epidemiology and Genetics (M.P.P.), National Cancer Institute, and the Office of Disease Prevention (J.K.G.), National Institutes of Health, Bethesda; and Westat (B.O., D.M.C.) and Information Management Services (P.W., T.L.R.), Rockville — all in Maryland; Pacific Health Research and Education Institute, Honolulu (L.A.Y.); the Department of Health Studies and Environmental Health Sciences, University of Minnesota, Minneapolis (T.C.); the Department of Medicine, Howard University (A.O.L.), and Georgetown University (C.I.) — both in Washington, DC; M.D. Anderson Cancer Center, Houston (R.B.); Washington University, St. Louis (G.L.A.); Huntsman Cancer Institute, University of Utah, Salt Lake City (S.S.B.); Anschutz Cancer Pavilion, University of Colorado, Denver (E.D.C.); the School of Medicine, University of Alabama at Birmingham, Birmingham (M.N.F.); Henry Ford Health System, Detroit (C.C.J.); Marshfield Clinic Research Foundation, Marshfield, WI (D.J.R.); and the Dalla Lana School of Public Health, University of Toronto, Toronto (A.B.M.).
Footnotes
No other potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–36. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 2.Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–7. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 3.Kronborg O, Jorgensen OD, Fenger C, Rasmussen M. Randomized study of biennial screening with a faecal occult blood test: results after nine screening rounds. Scand J Gastroenterol. 2004;39:846–51. doi: 10.1080/00365520410003182. [DOI] [PubMed] [Google Scholar]
- 4.Mandel JS, Church TR, Ederer F, Bond JH. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999;91:434–7. doi: 10.1093/jnci/91.5.434. [DOI] [PubMed] [Google Scholar]
- 5.Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343:1603–7. doi: 10.1056/NEJM200011303432203. [DOI] [PubMed] [Google Scholar]
- 6.Hewitson P, Glasziou P, Watson E, Towler B, Irwig L. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (Hemoccult): an update. Am J Gastroenterol. 2008;103:1541–9. doi: 10.1111/j.1572-0241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- 7.Hol L, van Leerdam ME, van Ballegooijen M, et al. Screening for colorectal cancer: randomised trial comparing guaiac-based and immunochemical faecal occult blood testing and flexible sigmoidoscopy. Gut. 2010;59:62–8. doi: 10.1136/gut.2009.177089. [DOI] [PubMed] [Google Scholar]
- 8.Segnan N, Senore C, Andreoni B, et al. Comparing attendance and detection rate of colonoscopy with sigmoidoscopy and FIT for colorectal cancer screening. Gastroenterology. 2007;132:2304–12. doi: 10.1053/j.gastro.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Quintero E, Castells A, Bujanda L, et al. Colonoscopy vs. fecal immunochemi-cal testing in colorectal-cancer screening. N Engl J Med. 2012;366:697–706. doi: 10.1056/NEJMoa1108895. [DOI] [PubMed] [Google Scholar]
- 10.Weissfeld JL, Schoen RE, Pinsky PF, et al. Flexible sigmoidoscopy in the PLCO cancer screening trial: results from the baseline screening examination of a randomized trial. J Natl Cancer Inst. 2005;97:989–97. doi: 10.1093/jnci/dji175. [DOI] [PubMed] [Google Scholar]
- 11.Atkin WS, Edwards R, Kralj-Hans I, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375:1624–33. doi: 10.1016/S0140-6736(10)60551-X. [DOI] [PubMed] [Google Scholar]
- 12.Segnan N, Armaroli P, Bonelli L, et al. Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian randomized controlled trial — SCORE. J Natl Cancer Inst. 2011;103:1310–22. doi: 10.1093/jnci/djr284. [DOI] [PubMed] [Google Scholar]
- 13.Hoff G, Grotmol T, Skovlund E, Bretthauer M. Risk of colorectal cancer seven years after flexible sigmoidoscopy screening: randomised controlled trial. BMJ. 2009;338:b1846. doi: 10.1136/bmj.b1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weissfeld JL, Schoen RE, Pinsky PF, et al. Flexible sigmoidoscopy in the randomized Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial: added yield from a second screening examination. J Natl Cancer Inst. 2012;104:280–9. doi: 10.1093/jnci/djr549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prorok PC, Andriole GL, Bresalier RS, et al. Design of the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. Control Clin Trials. 2000;21(Suppl):273S–309S. doi: 10.1016/s0197-2456(00)00098-2. [DOI] [PubMed] [Google Scholar]
- 16.Simpson NK, Johnson CC, Ogden SL, et al. Recruitment strategies in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial: the first six years. Control Clin Trials. 2000;21(Suppl):356S–378S. doi: 10.1016/s0197-2456(00)00102-1. [DOI] [PubMed] [Google Scholar]
- 17.Fleming ID, Cooper JS, Henson DE, et al. AJCC cancer staging manual. 5th. Philadelphia: Lippincott-Raven; 1997. [Google Scholar]
- 18.Miller AB, Yurgalevitch S, Weissfeld JL. Death review process in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. Control Clin Trials. 2000;21(Suppl):400S–406S. doi: 10.1016/s0197-2456(00)00095-7. [DOI] [PubMed] [Google Scholar]
- 19.Schoen RE, Pinsky PF, Weissfeld JL, et al. Utilization of surveillance colonoscopy in community practice. Gastroenterology. 2010;138:73–81. doi: 10.1053/j.gastro.2009.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinsky PF, Schoen RE, Weissfeld JL, et al. The yield of surveillance colonoscopy by adenoma history and time to examination. Clin Gastroenterol Hepatol. 2009;7:86–92. doi: 10.1016/j.cgh.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Ahlbom A. Biostatistics for epidemiologists. Boca Raton, FL: Lewis; 1993. [Google Scholar]
- 22.Izmirlian G. Estimation of the relative risk following group sequential procedure based upon the weighted log-rank statistic. Ithaca, NY: Cornell University, Library; Feb, 2011. ( http://arxiv.org/abs/1102.5088) [Google Scholar]
- 23.DeMets DL, Lan G. The alpha spending function approach to interim data analyses. Cancer Treat Res. 1995;75:1–27. doi: 10.1007/978-1-4615-2009-2_1. [DOI] [PubMed] [Google Scholar]
- 24.Lin DY, Yao Q, Ying ZL. A general theory on stochastic curtailment for censored survival data. J Am Stat Assoc. 1999;94:510–21. [Google Scholar]
- 25.SAS/STAT, version 9. Cary, NC: SAS Institute; 2010. [Google Scholar]
- 26.R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2010. [Google Scholar]
- 27.Croswell JM, Kramer BS, Kreimer AR, et al. Cumulative incidence of false-positive results in repeated, multimodal cancer screening. Ann Fam Med. 2009;7:212–22. doi: 10.1370/afm.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Preventive Services Task Force. Screening for colorectal cancer. U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149:627–37. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 30.Vital signs: colorectal cancer screening, incidence, and mortality — United States, 2002–2010. MMWR Morb Mortal Wkly Rep. 2011;60:884–9. [PubMed] [Google Scholar]
- 31.Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1–8. doi: 10.7326/0003-4819-150-1-200901060-00306. [DOI] [PubMed] [Google Scholar]
- 32.Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139:1128–37. doi: 10.1053/j.gastro.2010.06.052. [DOI] [PubMed] [Google Scholar]
- 33.Singh H, Nugent Z, Mahmud SM, Demers AA, Bernstein CN. Predictors of colorectal cancer after negative colonoscopy: a population-based study. Am J Gastroenterol. 2010;105:663–73. doi: 10.1038/ajg.2009.650. [DOI] [PubMed] [Google Scholar]
- 34.Lakoff J, Paszat LF, Saskin R, Rabeneck L. Risk of developing proximal vs. distal colorectal cancer after a negative colonoscopy: a population-based study. Clin Gastroenterol Hepatol. 2008;6:1117–21. doi: 10.1016/j.cgh.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 35.Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154:22–30. doi: 10.7326/0003-4819-154-1-201101040-00004. [DOI] [PubMed] [Google Scholar]
- 36.Baxter NN, Warren J, Barrett MJ, Stukel T, Doria-Rose VR. The association between colonoscopy and colorectal cancer mortality in a US cohort according to site of cancer and colonoscopist specialty. Gastroenterology. 2011;140(Suppl):S74–S75. doi: 10.1200/JCO.2011.40.4772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schoen RE, Pinsky PF, Weissfeld JL, et al. Colorectal cancers not detected by screening flexible sigmoidoscopy in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Gastrointest Endosc. 2012;75:612–20. doi: 10.1016/j.gie.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 38.Minoo P, Zlobec I, Peterson M, Terracciano L, Lugli A. Characterization of rectal, proximal and distal colon cancers based on clinicopathological, molecular and protein profiles. Int J Oncol. 2010;37:707–18. doi: 10.3892/ijo_00000720. [DOI] [PubMed] [Google Scholar]
- 39.Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088–100. doi: 10.1053/j.gastro.2009.12.066. [DOI] [PubMed] [Google Scholar]
- 40.Deng G, Kakar S, Tanaka H, et al. Proximal and distal colorectal cancers show distinct gene-specific methylation profiles and clinical and molecular characteristics. Eur J Cancer. 2008;44:1290–301. doi: 10.1016/j.ejca.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 41.Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. N Engl J Med. 1993;328:1365–71. doi: 10.1056/NEJM199305133281901. Erratum, N Engl J Med 1993;329:672. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.